Efficacy of Ergonomic Interventions on Work-Related Musculoskeletal Pain: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
- Studies with non-occupational populations (e.g., general public, student populations).
- Studies lacking a control group.
- Studies with insufficient data for effect size estimation.
- Conference abstracts, case reports, and unpublished dissertations.
2.3. Literature Search
2.4. Study Selection
2.5. Data Extraction
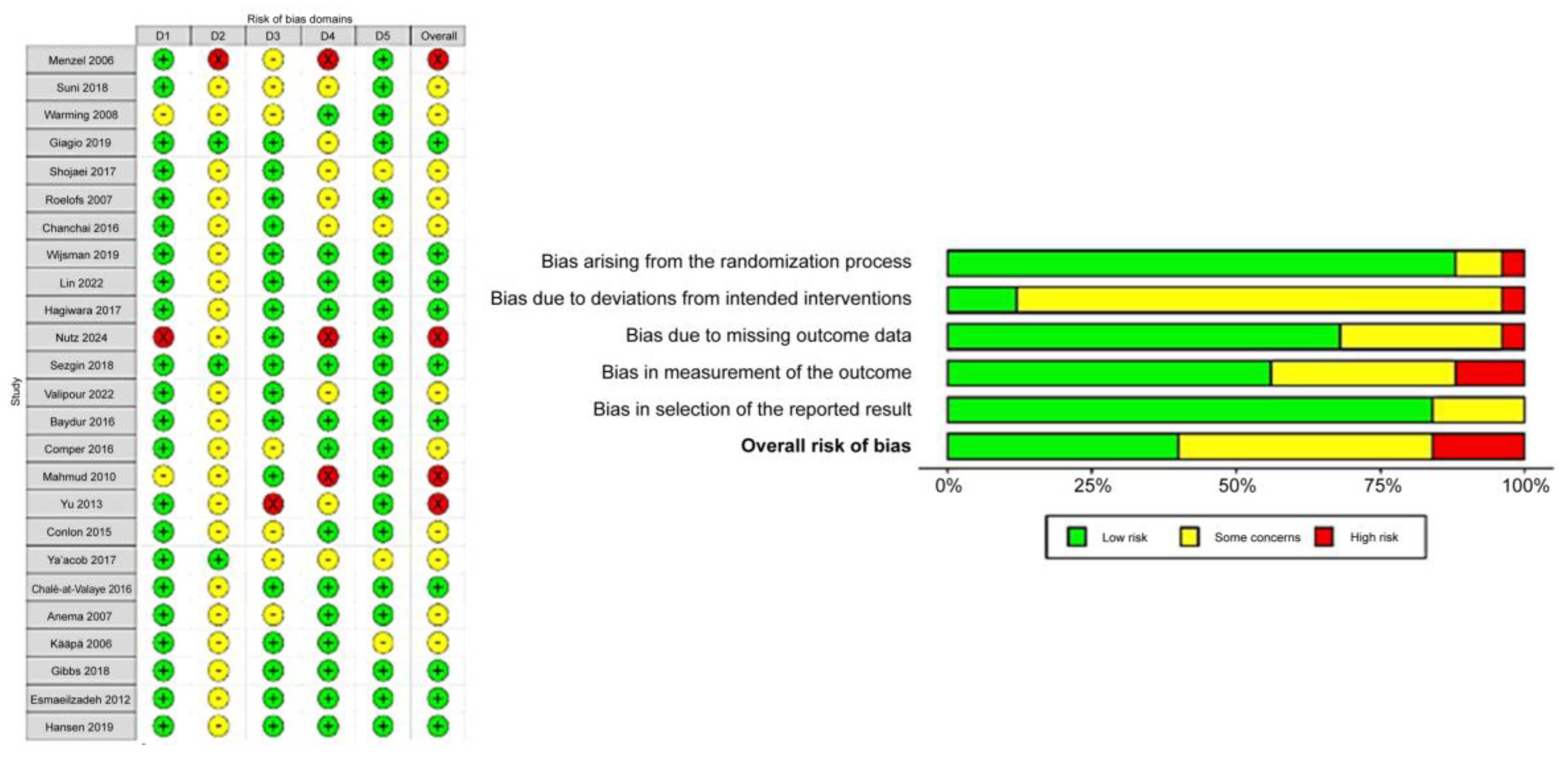
2.6. Assessment of Risk of Bias
2.7. Assessment of Results
2.8. Risk of Bias Across the Studies
2.9. Additional Analyses
3. Results
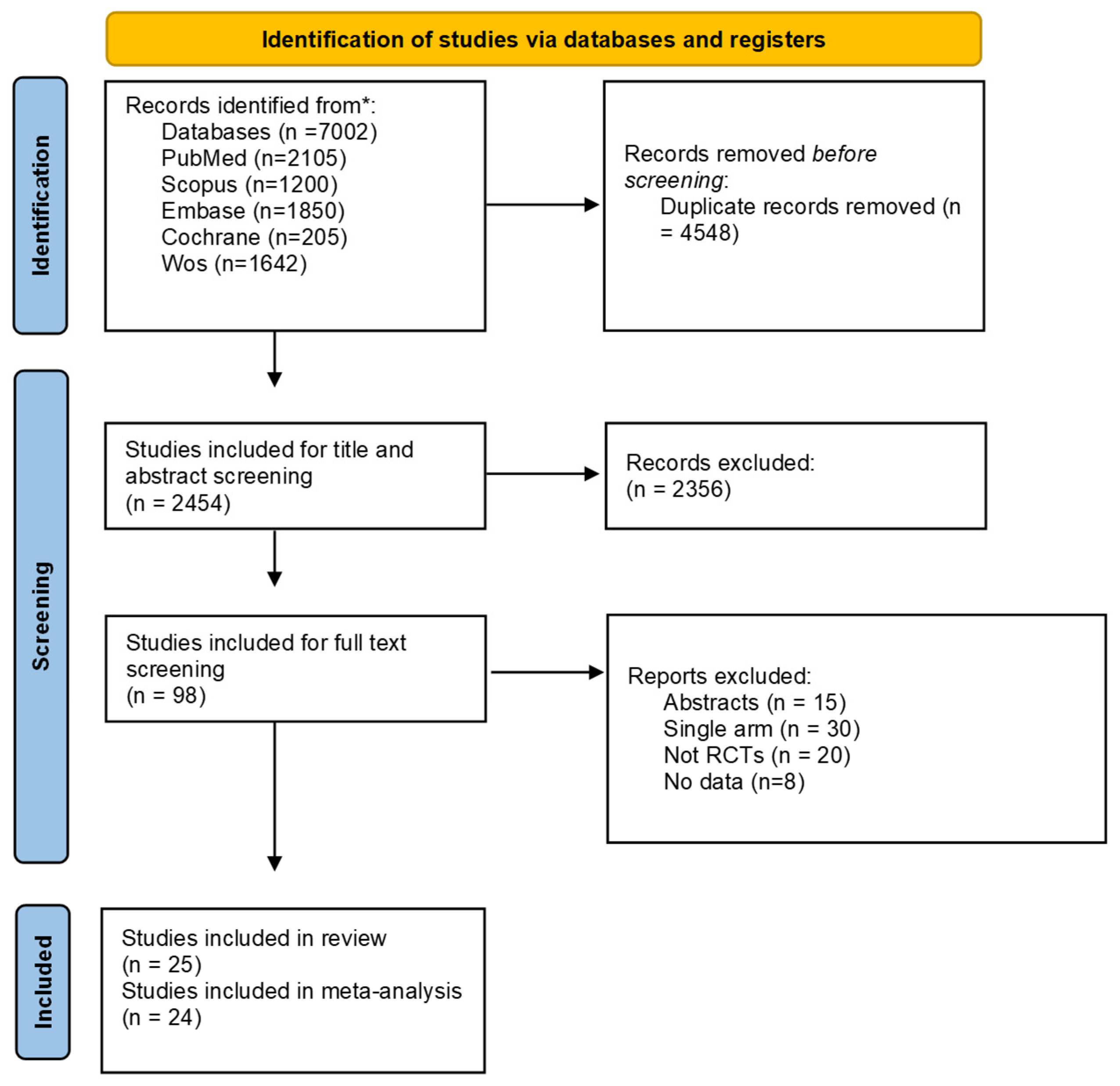
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias Assessment
3.4. Reported Pain Reduction in Different Body Parts
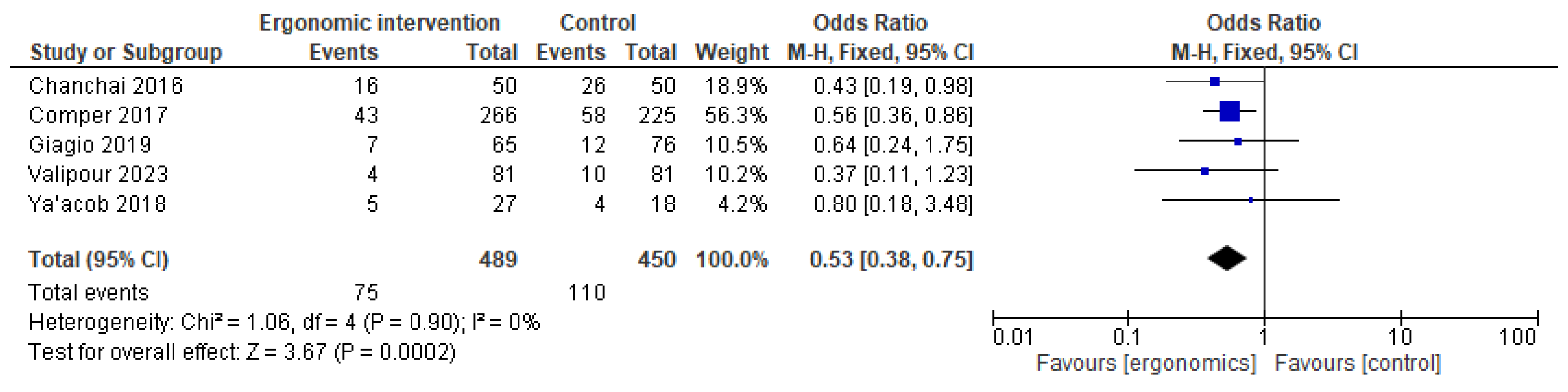
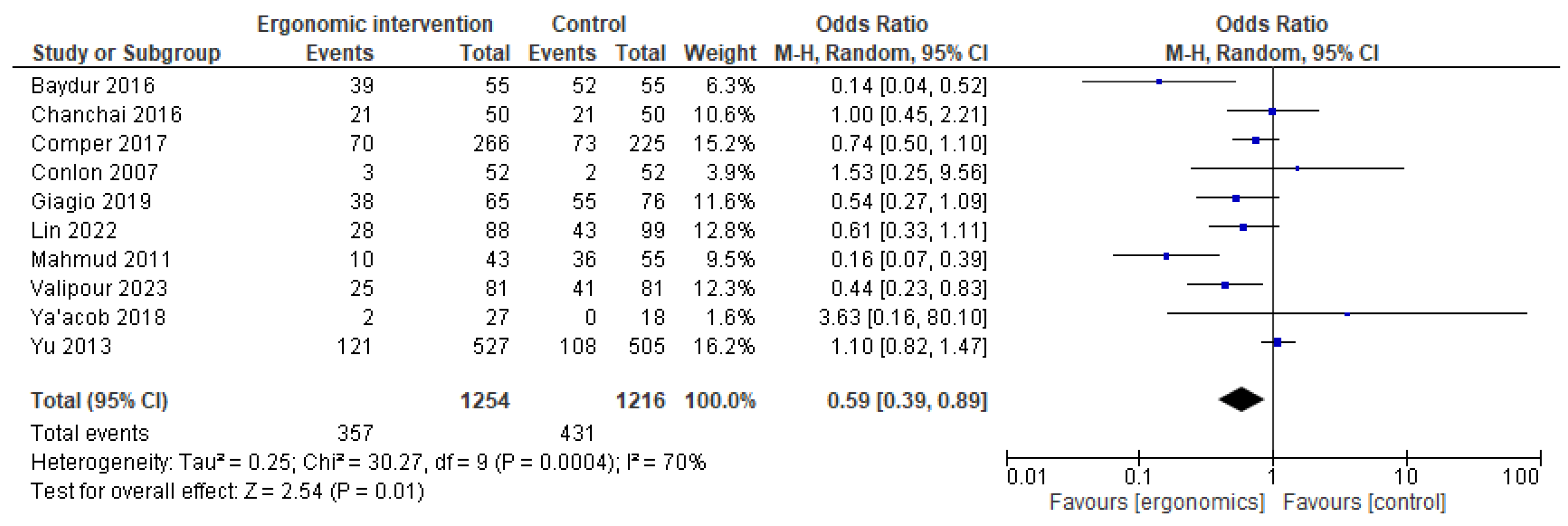
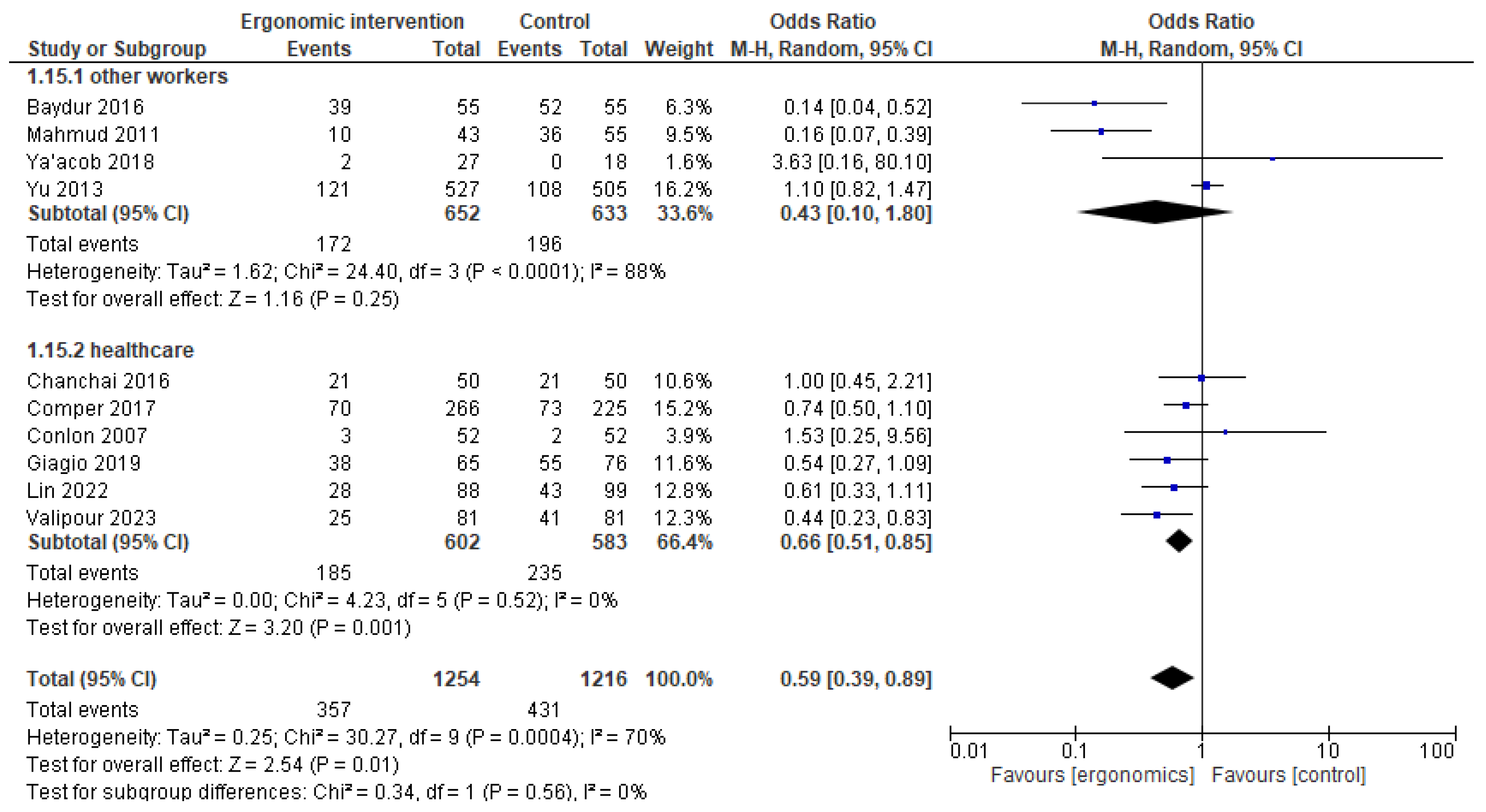
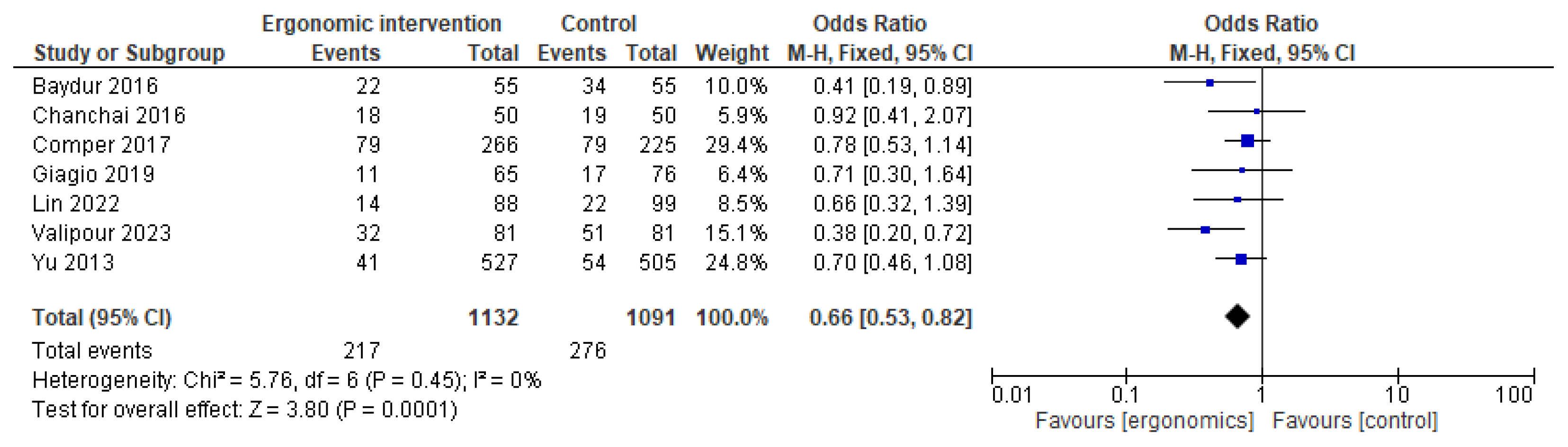
3.5. Back Pain
3.6. Neck Pain
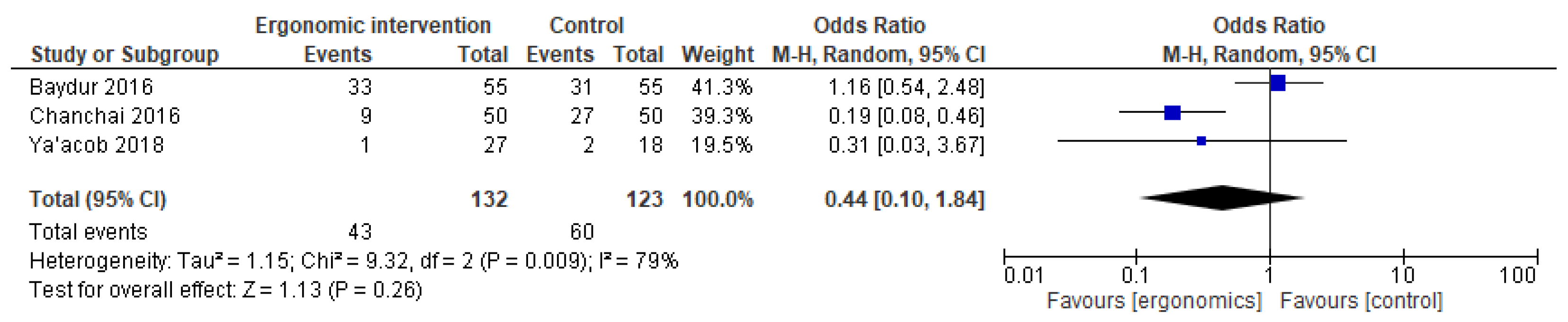
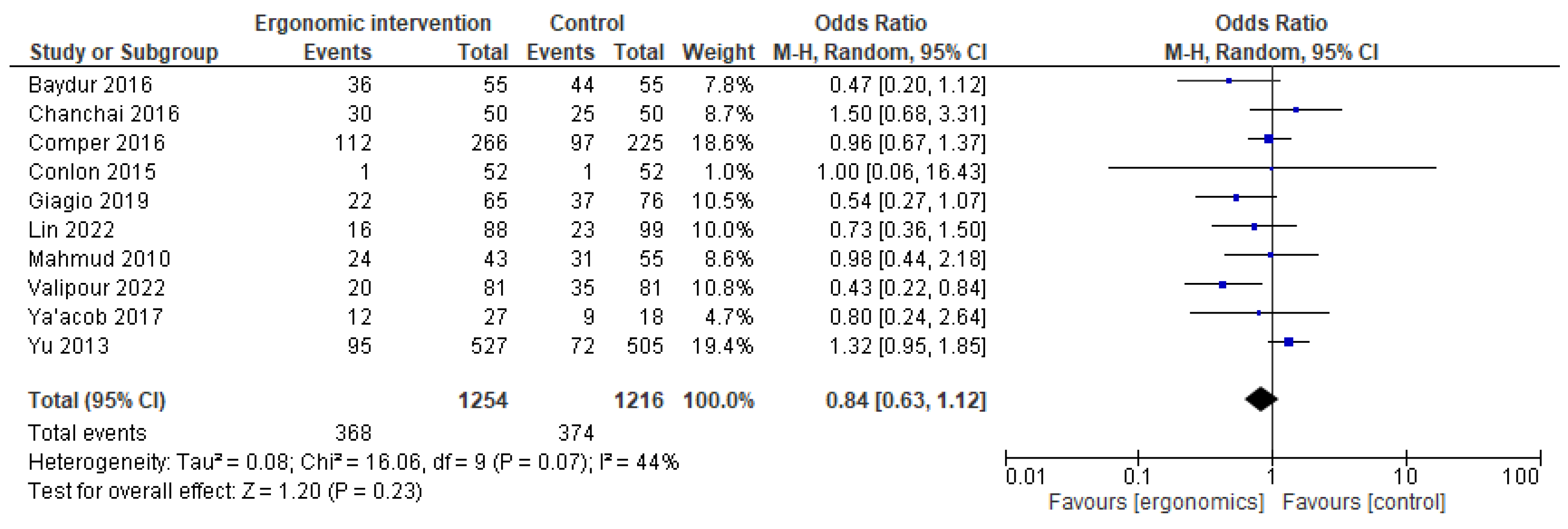
3.7. Shoulder and Upper Limb Pain
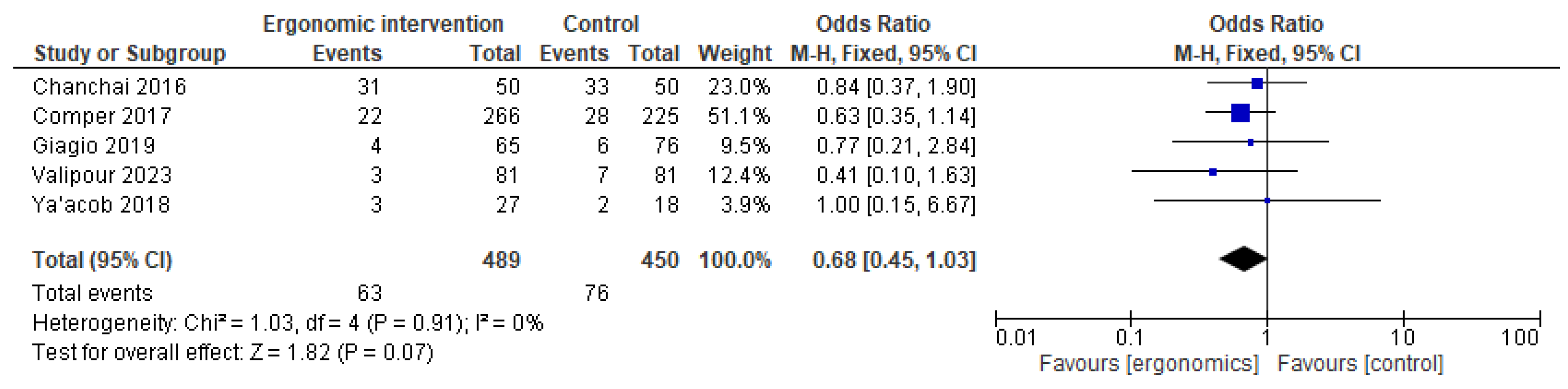
3.8. Knee and Lower Limb Pain
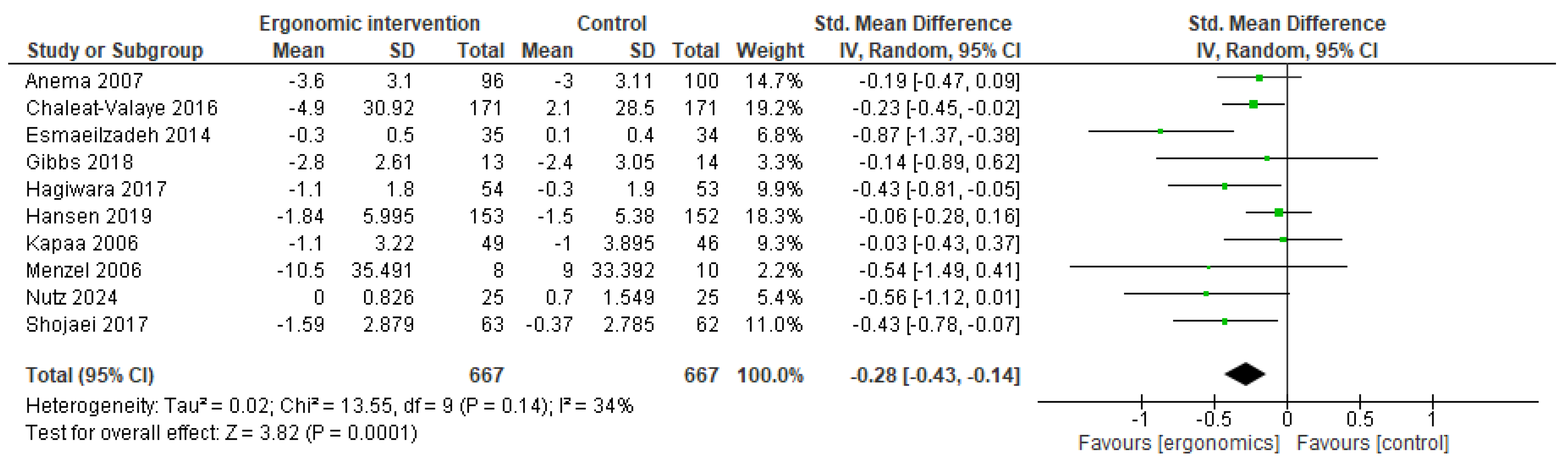
3.9. Pain Intensity
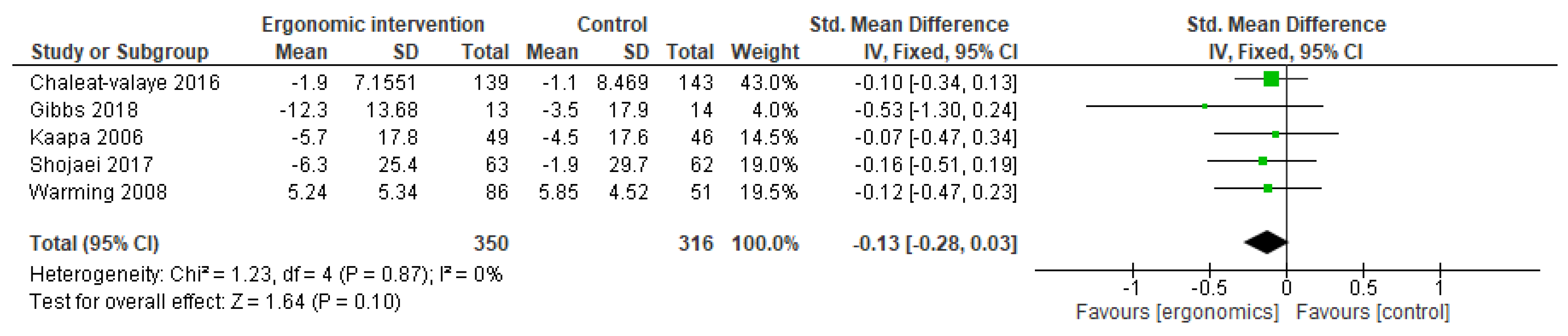
3.10. Disability Scores
3.11. Publication Bias and GRADE Assessment
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MSDs | musculoskeletal diseases |
| BMI | body mass index |
| CI | confidence interval |
| GRADE | Grading of Recommendations, Assessment, Development, and Evaluation |
| LD | linear dichroism |
| ORs | odds ratios |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCTs | randomized controlled trials |
| SMD | standardized mean difference |
References
- da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Punnett, L.; Wegman, D.H. Work-related musculoskeletal disorders: The epidemiologic evidence and the debate. J. Electromyogr. Kinesiol. 2004, 14, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.O.; Pereira, B.F.; Pereira Gomes, M.V.; Marcondes, L.P.; De Campos Gomes, F.; De Melo-Neto, J.S. Preventive factors against work-related musculoskeletal disorders: Narrative review. Rev. Bras. Med. Trab. 2020, 17, 415–430. [Google Scholar] [CrossRef]
- Demissie, B.; Bayih, E.T.; Demmelash, A.A. A systematic review of work-related musculoskeletal disorders and risk factors among computer users. Heliyon 2024, 10, e25075. [Google Scholar] [CrossRef]
- Hoe, V.C.W.; Urquhart, D.M.; Kelsall, H.L.; Zamri, E.N.; Sim, M.R. Ergonomic interventions for preventing work-related musculoskeletal disorders of the upper limb and neck among office workers. Cochrane Database Syst. Rev. 2018, 10, CD008570. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, J.H.; Martimo, K.P.; Karppinen, J.; Kuijer, P.P.F.M.; Viikari-Juntura, E.; Takala, E.P. Manual material handling advice and assistive devices for preventing and treating back pain in workers. Cochrane Database Syst. Rev. 2011, CD005958. [Google Scholar] [CrossRef]
- Adiga, U. Enhancing Occupational Health and Ergonomics for Optimal Workplace Well-being: A Review. Int. J. Chem. Biochem. Sci. 2023, 24, 157–164. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123-30. [Google Scholar]
- Menzel, N.N.; Robinson, M.E. Back Pain in Direct Patient Care Providers: Early Intervention with Cognitive Behavioral Therapy. Pain Manag. Nurs. 2006, 7, 53–63. [Google Scholar] [CrossRef]
- Suni, J.H.; Kolu, P.; Tokola, K.; Raitanen, J.; Rinne, M.; Taulaniemi, A.; Parkkari, J.; Kankaanpää, M. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: A blinded four-arm randomized controlled trial. BMC Public Health 2018, 18, 1376. [Google Scholar] [CrossRef]
- Warming, S.; Ebbehøj, N.E.; Wiese, N.; Larsen, L.H.; Duckert, J.; Tønnesen, H. Little effect of transfer technique instruction and physical fitness training in reducing low back pain among nurses: A cluster randomised intervention study. Ergonomics 2008, 51, 1530–1548. [Google Scholar] [CrossRef] [PubMed]
- Giagio, S.; Volpe, G.; Pillastrini, P.; Gasparre, G.; Frizziero, A.; Squizzato, F. A preventive program for work-related musculoskeletal disorders among surgeons: Outcomes of a randomized controlled clinical trial. Ann. Surg. 2019, 270, 969–975. [Google Scholar] [CrossRef]
- Shojaei, S.; Tavafian, S.S.; Jamshidi, A.R.; Wagner, J. A multidisciplinary workplace intervention for chronic low back pain among nursing assistants in Iran. Asian Spine J. 2017, 11, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, P.D.; Bierma-Zeinstra, S.M.; van Poppel, M.N.; Jellema, P.; Willemsen, S.P.; van Tulder, M.W.; van Mechelen, W.; Koes, B.W. Lumbar supports to prevent recurrent low back pain among home care workers: A randomized trial. Ann. Intern. Med. 2007, 147, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Chanchai, W.; Songkham, W.; Ketsomporn, P.; Sappakitchanchai, P.; Siriwong, W.; Robson, M.G. The impact of an ergonomics intervention on psychosocial factors and musculoskeletal symptoms among Thai hospital orderlies. Int. J. Environ. Res. Public Health 2016, 13, 464. [Google Scholar] [CrossRef]
- Wijsman, P.J.M.; Molenaar, L.; van‘t Hullenaar, C.D.P.; van Vugt, B.S.T.; Bleeker, W.A.; Draaisma, W.A.; Broeders, I.A.M.J. Ergonomics in handheld and robot-assisted camera control: A randomized controlled trial. Surg. Endosc. 2019, 33, 3919–3925. [Google Scholar] [CrossRef]
- Lin, S.; Tsai, C.C.; Liu, X.; Wu, Z.; Zeng, X. Effectiveness of participatory ergonomic interventions on musculoskeletal disorders and work ability among young dental professionals: A cluster-randomized controlled trail. J. Occup. Health 2022, 64, e12330. [Google Scholar] [CrossRef]
- Hagiwara, Y.; Yabe, Y.; Yamada, H.; Watanabe, T.; Kanazawa, K.; Koide, M.; Sekiguchi, T.; Hatano, H.; Itoi, E. Effects of a wearable type lumbosacral support for low back pain among hospital workers: A randomized controlled trial. J. Occup. Health 2017, 59, 201–209. [Google Scholar] [CrossRef]
- Nutz, E.; Jarvers, J.S.; Theopold, J.; Kleber, C.; Osterhoff, G. Effect of an upper body exoskeleton for surgeons on postoperative neck, back, and shoulder complaints. J. Occup. Health 2024, 66, uiae020. [Google Scholar] [CrossRef]
- Sezgin, D.; Esin, M.N. Effects of a PRECEDE-PROCEED model based ergonomic risk management programme to reduce musculoskeletal symptoms of ICU nurses. Intensive Crit. Care Nurs. 2018, 47, 89–97. [Google Scholar] [CrossRef]
- Valipour, F.; Mirzahosseini, S.A.H.; Saffari, M.; Jafari, E.; Lin, C.Y.; Al Zaben, F.; Koenig, H.G. Health education using the theory of planned behavior to modify ergonomic posture in hospital computer users: A randomized controlled trial. Int. Arch. Occup. Environ. Health 2023, 96, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Baydur, H.; Ergör, A.; Demiral, Y.; Akalin, E. Effects of participatory ergonomic intervention on developing upper extremity musculoskeletal disorders and disability in office employees using a computer. J. Occup. Health 2016, 58, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Comper, M.L.C.; Dennerlein, J.T.; Evangelista, G.D.S.; Rodrigues Da Silva, P.; Padula, R.S. Effectiveness of job rotation for preventing work-related musculoskeletal diseases: A cluster randomised controlled trial. Occup. Environ. Med. 2017, 74, 545–552. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, N.; Kenny, D.; Md Zein, R.; Hassan, S.N. Ergonomic Training Reduces Musculoskeletal Disorders among Office Workers: Results from the 6-Month Follow-Up. Malays. J. Med. Sci. 2011, 18, 16–26. [Google Scholar]
- Yu, W.; Yu, I.T.; Wang, X.; Li, Z.; Wan, S.; Qiu, H.; Lin, H.; Xie, S.; Sun, T. Effectiveness of participatory training for prevention of musculoskeletal disorders: A randomized controlled trial. Int. Arch. Occup. Environ. Health 2013, 86, 431–440. [Google Scholar] [CrossRef]
- Conlon, C.F.; Krause, N.; Rempel, D.M. A randomised controlled trial evaluating an alternative mouse and forearm support on upper body discomfort and musculoskeletal disorders among engineers. Occup. Environ. Med. 2008, 65, 311–318. [Google Scholar] [CrossRef]
- Ya’Acob, N.A.; Abidin, E.Z.; Rasdi, I.; Rahman, A.A.; Ismail, S. Reducing work-related musculoskeletal symptoms through implementation of Kiken Yochi training intervention approach. Work 2018, 60, 143–152. [Google Scholar] [CrossRef]
- Anema, J.R.; Steenstra, I.A.; Bongers, P.M.; de Vet, H.C.; Knol, D.L.; Loisel, P.; van Mechelen, W. Multidisciplinary rehabilitation for subacute low back pain: Graded activity or workplace intervention or both? A randomized controlled trial. Spine 2007, 32, 291–298, discussion 299–300. [Google Scholar] [CrossRef]
- Kääpä, E.H.; Frantsi, K.; Sarna, S.; Malmivaara, A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: A randomized trial. Spine 2006, 31, 371–376. [Google Scholar] [CrossRef]
- Gibbs, B.; Hergenroeder, A.L.; Perdomo, S.J.; Kowalsky, R.J.; Delitto, A.; Jakicic, J.M. Reducing sedentary behavior to decrease chronic low back pain: The stand back randomized trial. Occup. Environ. Med. 2018, 75, 321–327. [Google Scholar] [CrossRef]
- Chaléat-Valayer, E.; Denis, A.; Abelin-Genevois, K.; Zelmar, A.; Siani-Trebern, F.; Touzet, S.; Bergeret, A.; Colin, C.; Fassier, J.B. Long-term effectiveness of an educational and physical intervention for preventing low-back pain recurrence: A randomized controlled trial. Scand. J. Work. Environ. Health. 2016, 42, 510–519. [Google Scholar] [CrossRef]
- Hansen, B.B.; Kirkeskov, L.; Begtrup, L.M.; Boesen, M.; Bliddal, H.; Christensen, R.; Andreasen, D.L.; Kristensen, L.E.; Flachs, E.M.; Kryger, A.I. Early occupational intervention for people with low back pain in physically demanding jobs: A randomized clinical trial. PLoS Med. 2019, 16, e1002898. [Google Scholar] [CrossRef]
- Esmaeilzadeh, S.; Ozcan, E.; Capan, N. Effects of ergonomic intervention on work-related upper extremity musculoskeletal disorders among computer workers: A randomized controlled trial. Int. Arch. Occup. Environ. Health 2014 87, 73–83. [CrossRef]
- Stucky, C.H.; Cromwell, K.D.; Voss, R.K.; Chiang, Y.J.; Woodman, K.; Lee, J.E.; Cormier, J.N. Surgeon symptoms, strain, and selections: Systematic review and meta-analysis of surgical ergonomics. Ann. Med. Surg. 2018, 27, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Doğan, O. Assessment of employees’ ergonomic issues in the workplace in terms of occupational health and safety practices: A meta-analysis study. Elektron. Sos. Bilim. Dergisi. 2024, 23, 1640–1654. [Google Scholar] [CrossRef]
- Van Niekerk, S.M.; Louw, Q.A.; Hillier, S. The effectiveness of a chair intervention in the workplace to reduce musculoskeletal symptoms. A systematic review. BMC Musculoskelet. Disord. 2012, 13, 145. [Google Scholar] [CrossRef] [PubMed]
- Ezzatvar, Y.; Dueñas, L.; Balasch-Bernat, M.; Lluch-Girbés, E.; Rossettini, G. Which Portion of Physiotherapy Treatments’ Effect Is Not Attributable to the Specific Effects in People With Musculoskeletal Pain? A Meta-Analysis of Randomized Placebo-Controlled Trials. J. Orthop. Sports Phys. Ther. 2024, 54, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Russo, F.; Papalia, G.F.; Vadalà, G.; Fontana, L.; Iavicoli, S.; Papalia, R.; Denaro, V. The Effects of Workplace Interventions on Low Back Pain in Workers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 12614. [Google Scholar] [CrossRef]
- Farrell, S.F.; Edmunds, D.; Fletcher, J.; Martine, H.; Mohamed, H.; Liimatainen, J.; Sterling, M. Effectiveness of psychological interventions delivered by physiotherapists in the management of neck pain: A systematic review with meta-analysis. Pain Rep. 2023, 8, e1076. [Google Scholar] [CrossRef]
- Boocock, M.G.; McNair, P.J.; Larmer, P.J.; Armstrong, B.; Collier, J.; Simmonds, M.; Garrett, N. Interventions for the prevention and management of neck/upper extremity musculoskeletal conditions: A systematic review. Occup. Environ. Med. 2007, 64, 291–303. [Google Scholar] [CrossRef]
- Kennedy, C.A.; Amick, B.C., 3rd; Dennerlein, J.T.; Brewer, S.; Catli, S.; Williams, R.; Serra, C.; Gerr, F.; Irvin, E.; Mahood, Q.; et al. Systematic review of the role of occupational health and safety interventions in the prevention of upper extremity musculoskeletal symptoms, signs, disorders, injuries, claims and lost time. J. Occup. Rehabil. 2010, 20, 127–162. [Google Scholar] [CrossRef] [PubMed]
- Van Eerd, D.; Munhall, C.; Irvin, E.; Rempel, D.; Brewer, S.; van der Beek, A.J.; Dennerlein, J.T.; Tullar, J.; Skivington, K.; Pinion, C.; et al. Effectiveness of workplace interventions in the prevention of upper extremity musculoskeletal disorders and symptoms: An update of the evidence. Occup. Environ. Med. 2016, 73, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.F.; Ansari, S.; Zaki, S.; Sharma, S.; Nuhmani, S.; Alnagmoosh, A.; Alsubaiei, M.E. Effects of physical interventions on pain and disability in chronic low back pain with pronated feet: A systematic review and meta-analysis. Physiother. Theory Pract. 2025, 41, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Bäckryd, E.; Ghafouri, N.; Gerdle, B.; Dragioti, E. Rehabilitation interventions for neuropathic pain: A systematic review and meta-analysis of randomized controlled trials. J. Rehabil. Med. 2024, 56, jrm40188. [Google Scholar] [CrossRef]
- Shetty, A.; Delanerolle, G.; Cavalini, H.; Qui, Y.; Boyd, A.; Bouchareb, Y.; Thillainathan, A.; Kim, S.; Phiri, P.; Shi, J. A Systematic Review and Network Meta-Analysis of Minimally Invasive Intervention Use in Pain Management. Preprints.org [Internet]. 2023. Available online: http://europepmc.org/abstract/PPR/PPR669467 (accessed on 10 January 2025).




| Study ID | Country | Type of Ergonomic (Education/Training/Device) | Study Arms | Age (Mean +SD) | M/F | Main Outcomes |
|---|---|---|---|---|---|---|
| Menzel 2006 [9] | USA | Education and training | Cognitive behavioral therapy (CBT) | 40.3 | 5/27 | The intervention group experienced a notable reduction in pain intensity, suggesting a substantial effect of the intervention. Nonetheless, levels of stress increased during the same period. Additionally, depressive symptoms emerged as a significant predictor, explaining a considerable proportion of the variance in work absenteeism due to back pain. |
| Waitlist control group | ||||||
| Suni 2018 [10] | Finland | Education and training | Combined neuromuscular exercise + back care counseling | 45.1 (6.2) | 53F | Combined-arm showed reduced intensity of LBP (p = 0.006) and pain interfering with work (p = 0.011) compared with the Control-arm. Work-related fear of pain was reduced in both the Combined- (p = 0.003) and Exercise-arm (p = 0.002). Physical activity-related fear was reduced only in the Exercise-arm (p = 0.008). |
| Exercise alone (neuromuscular exercise) | 47.2 (7.4) | 57F | ||||
| Counseling alone (back care counseling) | 46.4 (6.4) | 55F | ||||
| Control (no intervention) | 46.7 (7.2) | 54F | ||||
| Warming 2008 [11] | Denmark | Education and training | Transfer technique education (TT) alone | - | - | The individual randomized intervention subgroup (transfer technique/physical training) significantly improved the LBP-disability (p = 0.001). |
| Combined with physical fitness training (TTPT). | - | - | ||||
| Control (nurses followed usual patient handling routine) | - | - | ||||
| Giagio 2019 [12] | Italy | Education, training, and devices | Preventive program (PP) | 35.5 (10.9) | 37/28 | Among the surgeons included, physical activity was identified as the only modifiable risk factor for work-related musculoskeletal disorders (p = 0.05). The preventive program group showed significant improvements in general health at 3 and 6 months (p = 0.04), along with reductions in low back pain (p = 0.04) and analgesic use (p = 0.03). |
| No-preventive program (NPP) | 37.7 (12.1) | 50/26 | ||||
| Shojaei 2017 [13] | Iran | Education and training | Educational program and ergonomic posture training | - | 52/11 | Comparative analyses revealed a statistically significant decrease in the intensity of work-related low back pain from baseline in the group that participated in the multidisciplinary program (p < 0.001), while no meaningful changes were observed in the control groups. However, differences in disability scores between the intervention and control groups did not reach statistical significance (p = 0.07). |
| Control (no intervention) | - | 47/15 | ||||
| Roelofs 2007 [14] | Netherlands | Device-based and education | Lumbar support + short course on healthy working methods. | 41.8 (9.7) | 3/180 | Over the course of a year, participants who used lumbar support reported fewer days with low back pain compared to those who only received a brief educational intervention. However, this reduction in pain did not translate into a noticeable decrease in total sick leave days. The lumbar support group also showed slight but statistically significant improvements in pain intensity and functional capacity. |
| Short course on healthy working methods only | 41.5 (9.8) | 5/172 | ||||
| Chanchai 2016 [15] | Thailand | Education and training | Ergonomic training sessions | 34.9 (9.5) | - | The study identified statistically significant variations in the prevalence of self-reported musculoskeletal disorders in the arm, upper back, and lower back regions when comparing data collected before and after the intervention. The results further indicated that the intervention had a measurable impact on certain psychosocial risk factors. |
| Control (no intervention) | 34.3 (7.3) | - | ||||
| Wijsman 2019 [16] | Netherlands | Device-based ergonomic intervention | AutoLap™ robotic camera holder was used during laparoscopic procedures. | 60.7 | - | Implementation of the AutoLap™ system leads to enhanced ergonomic conditions and postural benefits for the first assistant, while the surgeon’s ergonomic experience remains unchanged. Additionally, the use of a robotic camera holder is associated with a significant reduction in perceived workload. |
| Standard laparoscopic procedures without a robotic camera holder. | 59.6 | - | ||||
| Lin 2022 [17] | China | Education and training | Participatory ergonomic (PE) training | 27.12 (5.33) | 31/57 | Work ability scores showed improvement following the nine-month intervention. Compared to the control group, participants in the ergonomic program reported significantly fewer musculoskeletal issues in the neck and wrists/hands, along with a marginal increase in their work ability index, suggesting a positive—though limited—effect of the intervention. |
| Single 45 min ergonomic education session (sham intervention). | 28.25 (6.04) | 31/68 | ||||
| Hagiwara 2017 [18] | Japan | Device-based ergonomic intervention | (Wearable lumbar support—“spinal underwear”). | 44.7 (10.0) | 2/52 | VAS and Somatosensory Amplification Scale scores as well as lumbar spinal ROM in the experimental group significantly decreased. Low back pain and neck pain in the experimental group significantly decreased. |
| Waiting list control | 44.7 (9.6) | 1/52 | ||||
| Nutz 2024 [19] | Germany | Device-based ergonomic intervention | Surgeons performed two surgeries of the same type—one without and one with the exoskeleton (Paexo Shoulder, Ottobock) | 39 (7) | 20/5 | An upper body exoskeleton can significantly reduce the discomfort in the neck, shoulder, and back caused to surgeons by surgery. |
| The first surgery was performed without the exoskeleton. | ||||||
| Sezgin 2018 [20] | Turkey | Education and training | Ergonomic Risk Management Program (ERMP) | 27 (5.21) | 20/52 | Six months post-intervention, nurses showed an average RULA score of 4.39 ± 1.49 during patient repositioning, suggesting the need for prompt ergonomic review. Pain levels, related medication use, and ergonomic risks significantly declined, while exercise frequency rose. |
| Continued with regular ICU nursing duties without specific ergonomic training | ||||||
| Valipour 2023 [21] | Iran | Education-based ergonomic intervention following the Theory of Planned Behavior (TPB). | Six weekly educational sessions (each ~1 h) covering ergonomic principles using TPB constructs. | 32.2 (5.6) | 18/63 | At follow-up, % classified as high risk by ROSA dropped to 21% in the intervention group but rose to 65% in the control group. The intervention group reported significant symptom relief in the wrists/hands, lower back, neck, shoulders, and upper back (all p < 0.05), along with a notable reduction in the number of affected areas after three months. |
| Control (No intervention) | 14/67 | |||||
| Baydur 2016 [22] | Turkey | Education and training | Training in office ergonomics and individual risk assessment. | 36.0 (8.4) | 47/69 | Multivariate analysis showed a significantly lower likelihood of symptoms in the right neck and right wrist/hand in the intervention group (p < 0.05). Neck-related disability and symptom scores were also consistently lower over time compared to the control group (p < 0.05). |
| Received an educational brochure at the end of the study. | ||||||
| Comper 2017 [23] | Brazil | Education and training | Job rotation program | 28.4 (7.8) | 72/194 | At 12 months, both groups reported increased sick leave hours due to musculoskeletal issues, with no significant difference between the job rotation group and controls. Secondary outcomes also showed no significant group differences (p > 0.05). |
| Ergonomic training | 32.5 (9.0) | 30/195 | ||||
| Mahmud 2011 [24] | Malaysia | Education and training | Office ergonomics training by NIOSH. | 34.6 (10.4) | 13/30 | Workstation habits improved significantly and remained so at follow-up, particularly in keyboard, mouse, chair, and desk use. The greatest reduction in musculoskeletal disorders was in the neck (−42.2%, 95% CI −60.0 to −24.4). Significant improvements were also observed in the neck, right shoulder, upper and lower limbs, and lower back. |
| Received a leaflet with ergonomic office tips | 34.2 (8.4) | 11/44 | ||||
| Yu 2013 [25] | China | Education and training | Participatory training (POHSI model) | 29.1 (7.3) | 541/377 | One year post-training, in the intervention group, MSD prevalence significantly declined in the lower extremities (p < 0.001) and in the wrist/fingers (p = 0.002). No significant changes were found in other body regions or in the control groups. |
| Control_1 group was the control group in the intervention factory | 28.9 (7.4) | 516/391 | ||||
| Control_2 group was the control group in the control factory | 28.3 (7.1) | 914/740 | ||||
| Conlon 2007 [26] | USA | Device-based ergonomic intervention | Alternative mouse | 43.3 (10.8) | 39/13 | During the study, 42 participants developed new musculoskeletal disorders. Those using a forearm support board reported a significant reduction in right upper extremity discomfort. The alternative mouse showed a protective, but non-significant (p = 0.20) effect on right upper extremity disorders and neck/shoulder discomfort. |
| Forearm support board | 42.6 (10.3) | 39/12 | ||||
| Alternative mouse + Forearm support board | 44.4 (9.66) | 36/15 | ||||
| Conventional mouse | 41.2 (8.43) | 35/17 | ||||
| Ya’acob 2018 [27] | Malaysia | Education and training | MSS education and training and Kiken Yochi Training | 34.94 (10.37) | 27M | Postural assessment showed that 68.5% of participants had high-risk working postures for musculoskeletal symptoms. Tasks such as cultivation, manual weeding, and pineapple harvesting posed the greatest ergonomic risks. The most reported musculoskeletal symptoms were in the knees, lower back, and shoulders. Two months post-intervention, the intervention group showed a significant reduction in MSS prevalence in the ankles and feet. |
| Received only MSS education and training | 32.0 (9.07) | 18M | ||||
| Anema 2007 [28] | Netherlands | Education and training | Workplace intervention, Yes | 44.0 (8.6) | 51/45 | Median return-to-work time was shorter with workplace intervention (77 vs. 104 days, p = 0.02), which significantly improved return rates (p = 0.002). Graded activity negatively affected return to work (p < 0.001) and functional status. The combined intervention showed no effect. |
| Workplace intervention, No | 41.2 (10.7) | 33/67 | ||||
| Graded activity, Yes | 41.3 (9.2) | 19/36 | ||||
| Graded activity, No | 43.4 (8.3) | 26/31 | ||||
| Kääpä 2006 [29] | Finland | Education and training | Multidisciplinary rehabilitation | 46 (7.9) | 59F | No significant differences were found between the two treatment groups at post-rehabilitation, 6-, 12-, or 24-month follow-up. However, both intervention groups showed favorable effects in before-and-after comparisons, which were sustained at the 2-year follow-up. |
| Individual physiotherapy | 46.5 (7.0) | 61F | ||||
| Gibbs 2018 [30] | USA | Education, training, and device-based ergonomic intervention | Behavioral counseling, sit-stand desk attachment, activity prompter, and pain self-management | 52 (9) | 2/11 | Over six months, the intervention group sat 1.5 h/day less than controls (p < 0.001) and showed an average ODI reduction of 8 points (p = 0.001). At 6 months, ODI decreased by 50% in the intervention group vs. 14% in controls (p = 0.042). Although LBP reduction was not significant. |
| No intervention (offered a 60 min lesson at the end of the study) | 51 (13) | 4/10 | ||||
| Chaléat-Valaye 2016 [31] | France | Education and training | Education session + workplace training + home exercise program | 47.1 (8.5) | 39/132 | At two-year follow-up, LBP recurrence with sick leave occurred in 24% of the intervention group and 21% of controls, with no significant difference (p = 0.516). The intervention significantly reduced fear-avoidance beliefs (p < 0.05) and improved muscle endurance (p < 0.05). It also reduced use of painkillers, medical visits, imaging, and physiotherapy. |
| Usual care | 47.3 (8.5) | 38/133 | ||||
| Hansen 2019 [32] | Denmark | Education and training | Occupational intervention + usual care | 45.3 (10.1) | 104/49 | At 6 months, intention-to-treat analysis showed no significant difference in sick leave between groups (p = 0.42). Both groups improved significantly in pain (NRS), disability (RMDQ), fear-avoidance beliefs (FABQ), and physical HRQoL (SF-36), with no significant differences in secondary outcomes between them. |
| Usual care only | 45.7 (10.5) | 102/50F | ||||
| Esmaeilzadeh 2014 [33] | Turkey | Education, training, and device-based ergonomic intervention | Ergonomic training and workstation adjustments | 35.8 (6.5) | 9/26 | Over six months, the intervention group showed significant improvements in body posture (p < 0.001) and workstation layout (p = 0.002). WUEMSS intensity, duration, and frequency decreased significantly (all p < 0.01), alongside improvements in functional status and both physical (p < 0.001) and mental (p = 0.035) health-related quality of life. No significant change was observed in workday loss due to WUEMSS (p > 0.05). |
| Control (no intervention) | 35.0 (7.8) | 11/23 |
| Outcome | Excluded Study | Effect Size (95% CI) | p-Value | IÂ2 After Exclusion (%) |
|---|---|---|---|---|
| Lower back | Yu 2013 [32] | OR 0.53 (0.40, 0.70) | <0.00001 | 24% |
| Shoulder | Yu 2013 [32] | OR 0.76 (0.58, 1) | 0.05 | 17% |
| Arms | Baydur 2016 [14] | OR 0.20 (0.08, 0.47) | 0.0002 | 0 |
| Elbow | Comper 2017 [26] | OR 1 (0.69, 1.44) | 0.99 | 0 |
| Knees | Chanchai 2016 [21] | OR 0.69 (0.49, 0.99) | 0.04 | 0 |
| Pain intensity | Esmaeilzadeh 2014 [15] | SMD −0.22 (−0.33, −0.11) | 0.0001 | 0 |
| Certainty Assessment | № of Patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| № of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Ergonomic Intervention | Control | Relative (95% CI) | Absolute (95% CI) | ||
| Pain intensity | ||||||||||||
| 10 | randomized trials | serious a | not serious | not serious | not serious | none | 667 | 667 | - | SMD 0.28 SD lower (0.43 lower to 0.14 lower) | ⨁⨁⨁◯ Moderate a | CRITICAL |
| Disability score | ||||||||||||
| 5 | randomized trials | serious a | not serious | not serious | not serious | none | 350 | 316 | - | SMD 0.13 SD lower (0.28 lower to 0.03 higher) | ⨁⨁⨁◯ Moderate a | IMPORTANT |
| Reported pain reduced | ||||||||||||
| 11 | randomized trials | serious a | not serious | not serious | not serious | none | 1409/6771 (20.8%) | 1730/6405 (27.0%) | OR 0.64 (0.56 to 0.73) | 79 fewer per 1000 (from 98 fewer to 57 fewer) | ⨁⨁⨁◯ Moderate a | IMPORTANT |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, W.; Rojas, C.; Isidoro, R.; Lorente, A.; Dias, A.; Mariscal, G.; Benlloch, M.; Lorente, R. Efficacy of Ergonomic Interventions on Work-Related Musculoskeletal Pain: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 3034. https://doi.org/10.3390/jcm14093034
Santos W, Rojas C, Isidoro R, Lorente A, Dias A, Mariscal G, Benlloch M, Lorente R. Efficacy of Ergonomic Interventions on Work-Related Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(9):3034. https://doi.org/10.3390/jcm14093034
Chicago/Turabian StyleSantos, Weiner, Carmen Rojas, Rui Isidoro, Alejandro Lorente, Ana Dias, Gonzalo Mariscal, María Benlloch, and Rafael Lorente. 2025. "Efficacy of Ergonomic Interventions on Work-Related Musculoskeletal Pain: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 9: 3034. https://doi.org/10.3390/jcm14093034
APA StyleSantos, W., Rojas, C., Isidoro, R., Lorente, A., Dias, A., Mariscal, G., Benlloch, M., & Lorente, R. (2025). Efficacy of Ergonomic Interventions on Work-Related Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(9), 3034. https://doi.org/10.3390/jcm14093034