Proximal Hip Fracture: Does Canal Width Matter?
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Study Design and Population
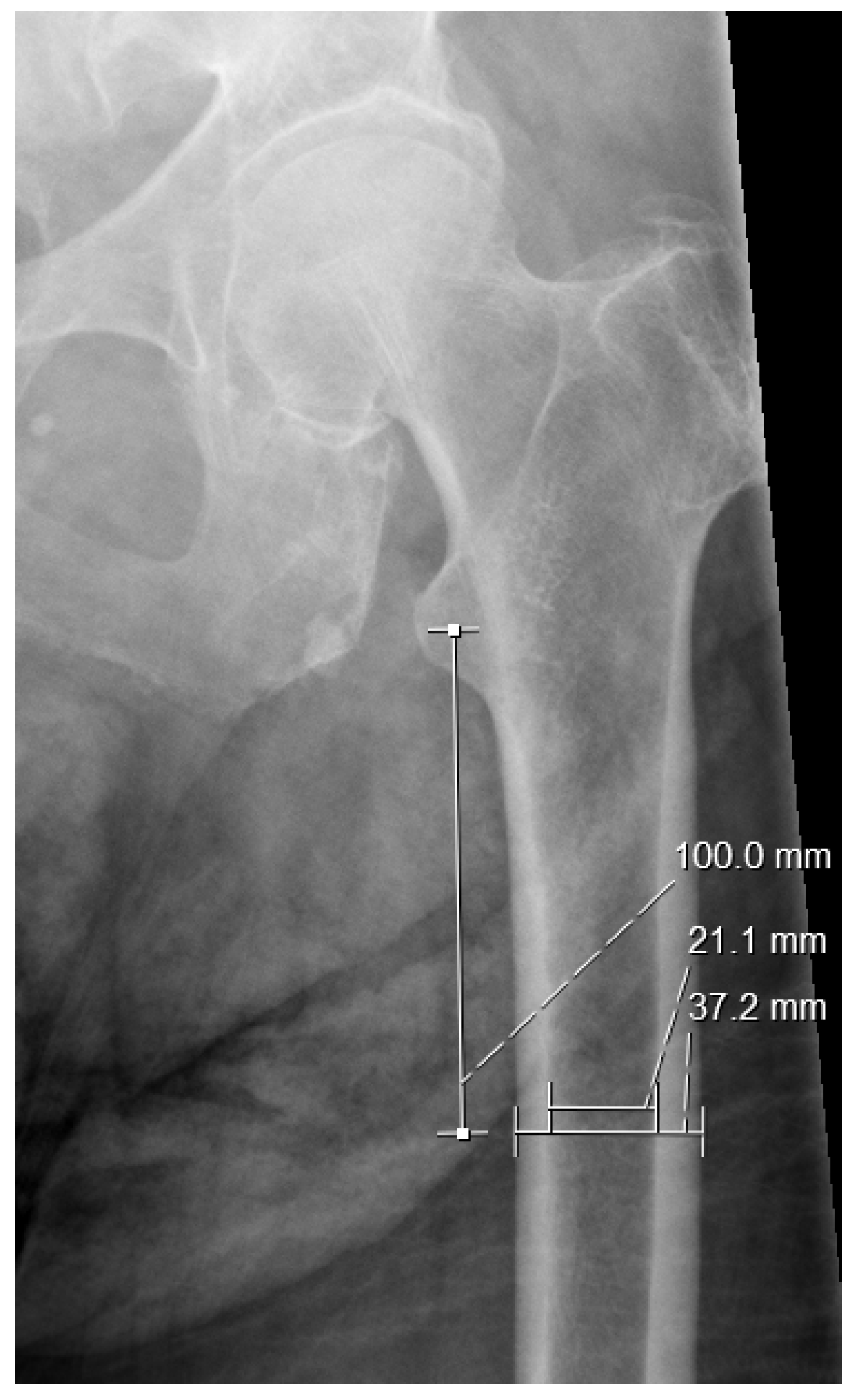
2.3. Measurements
2.4. Statistical Analysis
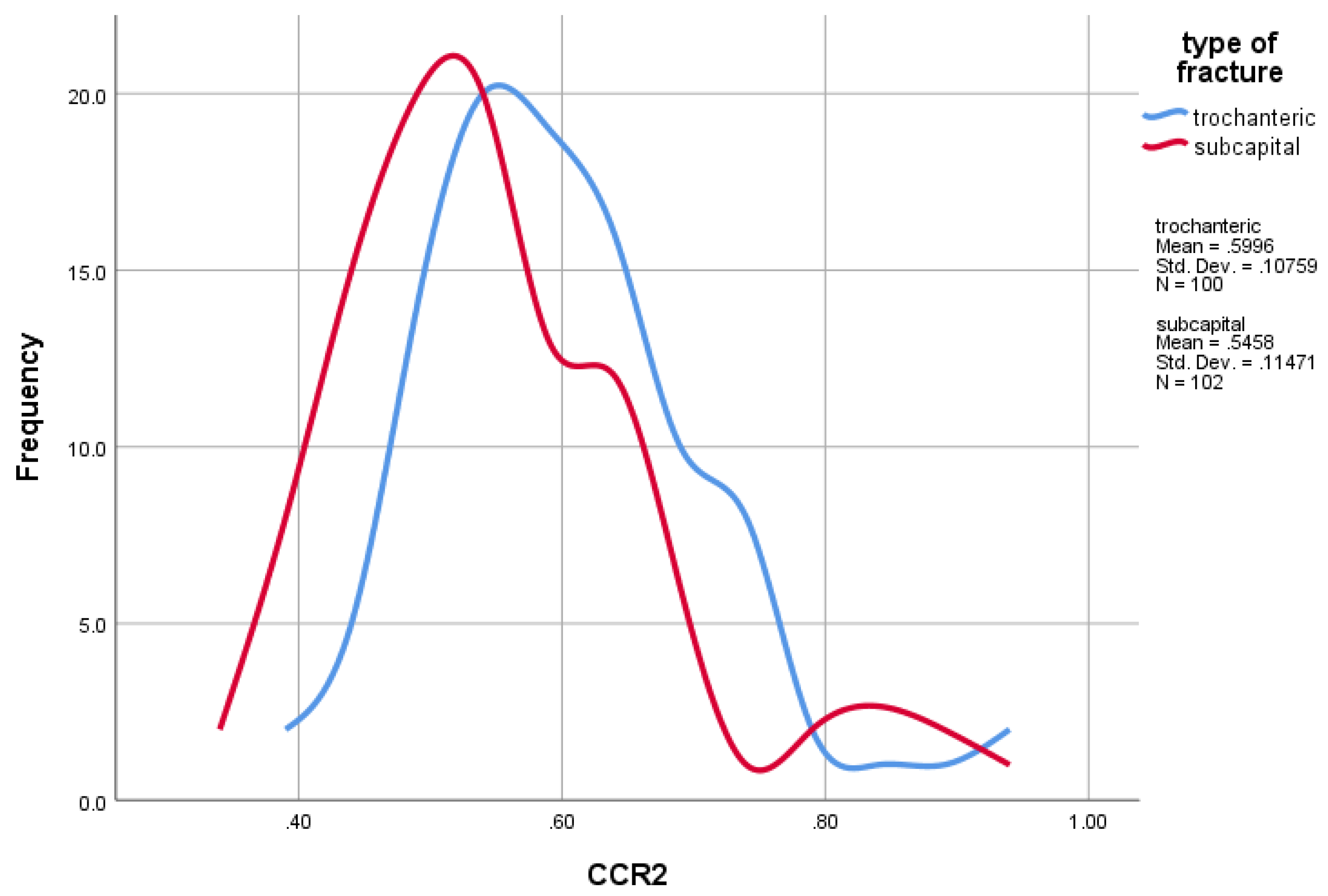
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnell, O.; Kanis, J.A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Nieves, J.W.; Bilezikian, J.P.; Lane, J.M.; Einhorn, T.A.; Wang, Y.; Steinbuch, M.; Cosman, F. Fragility fractures of the hip and femur: Incidence and patient characteristics. Osteoporos. Int. 2010, 21, 399–408. [Google Scholar] [CrossRef]
- Borgström, F.; Karlsson, L.; Ortsäter, G.; Norton, N.; Halbout, P.; Cooper, C.; Lorentzon, M.; McCloskey, E.V.; Harvey, N.C.; Javaid, M.K.; et al. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 2020, 15, 59. [Google Scholar] [CrossRef]
- Aprato, A.; Bechis, M.; Buzzone, M.; Bistolfi, A.; Daghino, W.; Massè, A. No rest for elderly femur fracture patients: Early surgery and early ambulation decrease mortality. J. Orthop. Traumatol. Off. J. Ital. Soc. Orthop. Traumatol. 2020, 21, 12. [Google Scholar] [CrossRef] [PubMed]
- Kemmler, W.; Bebenek, M.; Kohl, M.; von Stengel, S. Exercise and fractures in postmenopausal women. Final results of the controlled Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). Osteoporos. Int. 2015, 26, 2491–2499. [Google Scholar] [CrossRef] [PubMed]
- Uusi-Rasi, K.; Karinkanta, S.; Tokola, K.; Kannus, P.; Sievänen, H. Bone Mass and Strength and Fall-Related Fractures in Older Age. J. Osteoporos. 2019, 2019, 5134690. [Google Scholar] [CrossRef]
- Taylor, A.J.; Gary, L.C.; Arora, T.; Becker, D.J.; Curtis, J.R.; Kilgore, M.L.; Morrisey, M.A.; Saag, K.G.; Matthews, R.; Yun, H.; et al. Clinical and demographic factors associated with fractures among older Americans. Osteoporos. Int. 2011, 22, 1263–1274. [Google Scholar] [CrossRef]
- Guerado, E.; Cruz, E.; Cano, J.R.; Crespo, P.V.; Alaminos, M.; Sánchez-Quevedo, M.d.C.; Campos, A. Bone mineral density aspects in the femoral neck of hip fracture patients. Injury 2016, 47 (Suppl. S1), S21–S24. [Google Scholar] [CrossRef]
- Deleanu, B.; Prejbeanu, R.; Tsiridis, E.; Vermesan, D.; Crisan, D.; Haragus, H.; Predescu, V.; Birsasteanu, F. Occult fractures of the proximal femur: Imaging diagnosis and management of 82 cases in a regional trauma center. World J. Emerg. Surg. 2015, 10, 55. [Google Scholar] [CrossRef]
- de Sire, A.; Invernizzi, M.; Baricich, A.; Lippi, L.; Ammendolia, A.; Grassi, F.A.; Leigheb, M. Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation. World J. Orthop. 2021, 12, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Vidán, M.T.; Sánchez, E.; Gracia, Y.; Marañón, E.; Vaquero, J.; Serra, J.A. Causes and effects of surgical delay in patients with hip fracture: A cohort study. Ann. Intern. Med. 2011, 155, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.G.; D’Antoni, A.V.; Loukas, M.; Oskouian, R.J.; Tubbs, R.S. Hip fractures in the elderly-: A Clinical Anatomy Review. Clin. Anat. 2017, 30, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, L.; Hao, Y.; Wang, Z.; Wang, M.; Ge, S. Analysis of trabecular distribution of the proximal femur in patients with fragility fractures. BMC Musculoskelet. Disord. 2013, 14, 130. [Google Scholar] [CrossRef]
- Hopley, C.; Stengel, D.; Ekkernkamp, A.; Wich, M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ 2010, 340, c2332. [Google Scholar] [CrossRef]
- Miller, B.J.; Callaghan, J.J.; Cram, P.; Karam, M.; Marsh, J.L.; Noiseux, N.O. Changing trends in the treatment of femoral neck fractures: A review of the american board of orthopaedic surgery database. J. Bone Joint Surg. Am. 2014, 96, e149. [Google Scholar] [CrossRef]
- Rotem, G.; Sharfman, Z.T.; Rath, E.; Gold, A.; Rachevsky, G.; Steinberg, E.; Drexler, M.; Haviv, B.; Amar, E. Does hip morphology correlate with proximal femoral fracture type? Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2020, 30, 629–634. [Google Scholar] [CrossRef]
- Nasiri Sarvi, M.; Luo, Y. Sideways fall-induced impact force and its effect on hip fracture risk: A review. Osteoporos. Int. 2017, 28, 2759–2780. [Google Scholar] [CrossRef]
- Yamauchi, K.; Naofumi, M.; Sumida, H.; Fukuta, S.; Hori, H. Comparison of morphological features in the femur between femoral neck fractures and femoral intertrochanteric fractures. Surg. Radiol. Anat. 2016, 38, 775–780. [Google Scholar] [CrossRef]
- Bouxsein, M.L.; Szulc, P.; Munoz, F.; Thrall, E.; Sornay-Rendu, E.; Delmas, P.D. Contribution of trochanteric soft tissues to fall force estimates, the factor of risk, and prediction of hip fracture risk. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2007, 22, 825–831. [Google Scholar] [CrossRef]
- Greenspan, S.L.; Myers, E.R.; Maitland, L.A.; Kido, T.H.; Krasnow, M.B.; Hayes, W.C. Trochanteric bone mineral density is associated with type of hip fracture in the elderly. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 1994, 9, 1889–1894. [Google Scholar] [CrossRef]
- Napoli, N.; Schwartz, A.V.; Palermo, L.; Jin, J.J.; Wustrack, R.; Cauley, J.A.; Ensrud, K.E.; Kelly, M.; Black, D.M. Risk factors for subtrochanteric and diaphyseal fractures: The study of osteoporotic fractures. J. Clin. Endocrinol. Metab. 2013, 98, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Doblaré, M.; García, J.M.; Gómez, M.J. Modelling bone tissue fracture and healing: A review. Eng. Fract. Mech. 2004, 71, 1809–1840. [Google Scholar] [CrossRef]
- Gnudi, S.; Ripamonti, C.; Lisi, L.; Fini, M.; Giardino, R.; Giavaresi, G. Proximal femur geometry to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. Osteoporos. Int. 2002, 13, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Pande, I.; O’Neill, T.W.; Pritchard, C.; Scott, D.L.; Woolf, A.D. Bone mineral density, hip axis length and risk of hip fracture in men: Results from the Cornwall Hip Fracture Study. Osteoporos. Int. 2000, 11, 866–870. [Google Scholar] [CrossRef]
- Szulc, P.; Duboeuf, F.; Schott, A.M.; Dargent-Molina, P.; Meunier, P.J.; Delmas, P.D. Structural determinants of hip fracture in elderly women: Re-analysis of the data from the EPIDOS study. Osteoporos. Int. 2006, 17, 231–236. [Google Scholar] [CrossRef]
- Dorr, L.D.; Faugere, M.C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Noble, P.C.; Alexander, J.W.; Lindahl, L.J.; Yew, D.T.; Granberry, W.M.; Tullos, H.S. The anatomic basis of femoral component design. Clin. Orthop. Relat. Res. 1988, 235, 148–165. [Google Scholar] [CrossRef]
- Dossick, P.H.; Dorr, L.D.; Gruen, T.; Saberi, M.T. Techniques for preoperative planning and postoperative evaluation of noncemented hip arthroplasty. Tech. Orthop. 1991, 6, 1–6. [Google Scholar] [CrossRef]
- Nakaya, R.; Takao, M.; Hamada, H.; Sakai, T.; Sugano, N. Reproducibility of the Dorr classification and its quantitative indices on plain radiographs. Orthop. Traumatol. Surg. Res. 2019, 105, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Reeve, J. Role of cortical bone in hip fracture. Bonekey Rep. 2017, 6, 867. [Google Scholar] [CrossRef]
- Jordan, G.R.; Loveridge, N.; Bell, K.L.; Power, J.; Rushton, N.; Reeve, J. Spatial clustering of remodeling osteons in the femoral neck cortex: A cause of weakness in hip fracture? Bone 2000, 26, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Baudoin, C.; Fardellone, P.; Sebert, J.L. Effect of sex and age on the ratio of cervical to trochanteric hip fracture. A meta-analysis of 16 reports on 36,451 cases. Acta Orthop. Scand. 1993, 64, 647–653. [Google Scholar] [CrossRef]
- Tanner, D.A.; Kloseck, M.; Crilly, R.G.; Chesworth, B.; Gilliland, J. Hip fracture types in men and women change differently with age. BMC Geriatr. 2010, 10, 12. [Google Scholar] [CrossRef] [PubMed]
- Karagas, M.R.; Lu-Yao, G.L.; Barrett, J.A.; Beach, M.L.; Baron, J.A. Heterogeneity of Hip Fracture: Age, Race, Sex, and Geographic Patterns of Femoral Neck and Trochanteric Fractures among the US Elderly. Am. J. Epidemiol. 1996, 143, 677–682. [Google Scholar] [CrossRef]
- Johnell, O.; Kanis, J.A.; Oden, A.; Johansson, H.; De Laet, C.; Delmas, P.; Eisman, J.A.; Fujiwara, S.; Kroger, H.; Mellstrom, D.; et al. Predictive value of BMD for hip and other fractures. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2005, 20, 1185–1194. [Google Scholar] [CrossRef]
- De Laet, C.; Kanis, J.A.; Odén, A.; Johanson, H.; Johnell, O.; Delmas, P.; Eisman, J.A.; Kroger, H.; Fujiwara, S.; Garnero, P.; et al. Body mass index as a predictor of fracture risk: A meta-analysis. Osteoporos. Int. 2005, 16, 1330–1338. [Google Scholar] [CrossRef]


| Trochanteric Group (n = 100) | Sub-Capital Group (n = 102) | |
|---|---|---|
| Age (SD) | 82.84 (6.87) | 79.99 (7.41) |
| Gender: Female (n) | 64.00% (64) | 73.53% (75) |
| Charlson comorbidity score (SD) | 5.9 (2.00) | 5.3 (1.63) |
| Dorr type A | 19 | 19 |
| Dorr type B | 72 | 73 |
| Dorr type C | 9 | 10 |
| Trochanteric, Mean (SD) | Sub-Capital, Mean (SD) | p-Value | |
|---|---|---|---|
| CW10 | 32.78 (2.94) | 31.30 (3.11) | 0.001 |
| EW10 | 16.15 (2.74) | 15.51 (3.02) | 0.117 |
| EWlt | 27.22 (3.61) | 28.85 (4.60) | 0.006 |
| CTI | 0.51 (0.07) | 0.50 (0.09) | 0.778 |
| CCR | 0.60 (0.11) | 0.55 (0.11) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oulianski, M.; Sagi, A.; Rosinsky, P.; Bilenko, G.; Avraham, D.; Lubovsky, O. Proximal Hip Fracture: Does Canal Width Matter? J. Clin. Med. 2025, 14, 2768. https://doi.org/10.3390/jcm14082768
Oulianski M, Sagi A, Rosinsky P, Bilenko G, Avraham D, Lubovsky O. Proximal Hip Fracture: Does Canal Width Matter? Journal of Clinical Medicine. 2025; 14(8):2768. https://doi.org/10.3390/jcm14082768
Chicago/Turabian StyleOulianski, Maria, Amit Sagi, Philip Rosinsky, Garrik Bilenko, Dana Avraham, and Omri Lubovsky. 2025. "Proximal Hip Fracture: Does Canal Width Matter?" Journal of Clinical Medicine 14, no. 8: 2768. https://doi.org/10.3390/jcm14082768
APA StyleOulianski, M., Sagi, A., Rosinsky, P., Bilenko, G., Avraham, D., & Lubovsky, O. (2025). Proximal Hip Fracture: Does Canal Width Matter? Journal of Clinical Medicine, 14(8), 2768. https://doi.org/10.3390/jcm14082768








