Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Anesthesia
2.3. Follow-Up
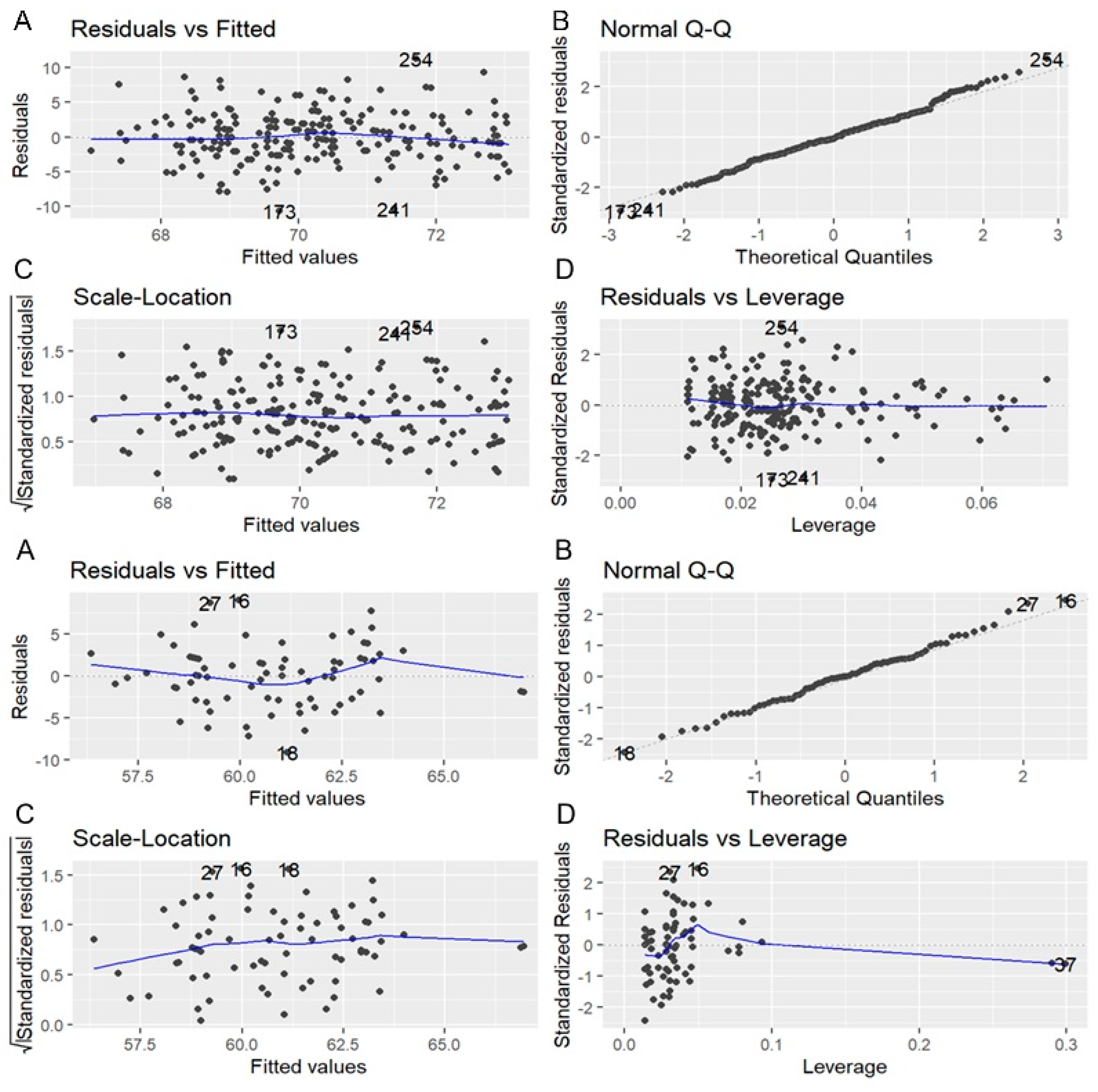
3. Statistical Analysis
4. Results
4.1. Quality of Life and Symptom Improvement
4.2. Influence of Anesthesia and Anesthetic Drugs
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Peigh, G.; Zhou, J.; Rosemas, S.C.; Roberts, A.I.; Longacre, C.; Nayak, T.; Schwab, G.; Soderlund, D.; Passman, R.S. Impact of Atrial Fibrillation Burden on Health Care Costs and Utilization. JACC Clin. Electrophysiol. 2024, 10, 718–730. [Google Scholar] [CrossRef] [PubMed]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the Management of Atrial Fibrillation Developed in Collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414. [Google Scholar] [PubMed]
- Tzeis, S.; Gerstenfeld, E.P.; Kalman, J.; Saad, E.B.; Sepehri Shamloo, A.; Andrade, J.G.; Barbhaiya, C.R.; Baykaner, T.; Boveda, S.; Calkins, H.; et al. 2024 European Heart Rhythm Association/Heart Rhythm Society/Asia Pacific Heart Rhythm Society/Latin American Heart Rhythm Society Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation. Europace 2024, 26, euae043. [Google Scholar] [CrossRef]
- Mark, D.B.; Anstrom, K.J.; Sheng, S.; Piccini, J.P.; Baloch, K.N.; Monahan, K.H.; Daniels, M.R.; Bahnson, T.D.; Poole, J.E.; Rosenberg, Y.; et al. Effect of Catheter Ablation vs Antiarrhythmic Drug Therapy on Quality of Life Among Patients with Atrial Fibrillation: The CABANA Randomized Clinical Trial. JAMA 2019, 321, 1059–1068. [Google Scholar] [CrossRef]
- Blomström-Lundqvist, C.; Gizurarson, S.; Schwieler, J.; Jensen, S.M.; Bergfeldt, L.; Kennebäck, G.; Rubulis, A.; Malmborg, H.; Raatikainen, P.; Lönnerholm, S.; et al. Effect of Catheter Ablation vs Antiarrhythmic Medication on Quality of Life in Patients with Atrial Fibrillation: The CAPTAF Randomized Clinical Trial. JAMA 2019, 321, 1061–1071. [Google Scholar] [CrossRef]
- Allan, K.S.; Aves, T.; Henry, S.; Banfield, L.; Victor, J.C.; Dorian, P.; Healey, J.S.; Andrade, J.G.; Carroll, S.L.; McGillion, M.H. Health-Related Quality of Life in Patients with Atrial Fibrillation Treated with Catheter Ablation or Antiarrhythmic Drug Therapy: A Systematic Review and Meta-analysis. CJC Open 2020, 2, 286–295. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wokhlu, A.; Monahan, K.H.; Hodge, D.O.; Asirvatham, S.J.; Friedman, P.A.; Munger, T.M.; Bradley, D.J.; Bluhm, C.M.; Haroldson, J.M.; Packer, D.L. Long-Term Quality of Life After Atrial Fibrillation Ablation: Results from a Large Multicenter Prospective Cohort. Health Qual. Life Outcomes 2023, 21, 98. [Google Scholar]
- Sharma, E.; Varley, A.; Osorio, J.; Thorne, C.; Varosy, P.; Metzl, M.; Rajendra, A.; Oza, S.; Morales, G.; Magnano, A.; et al. Procedural Trends in Catheter Ablation of Persistent Atrial Fibrillation: Insights from the Real-AF Registry. Circ. Arrhythm Electrophysiol. 2023, 16, e011828. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dada, R.S.; Hayanga, J.W.A.; Woods, K.; Schwartzman, D.; Thibault, D.; Ellison, M.; Schmidt, S.; Siddoway, D.; Badhwar, V.; Hayanga, H.K. Anesthetic Choice for Atrial Fibrillation Ablation: A National Anesthesia Clinical Outcomes Registry Analysis. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2600–2606. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Mansour, M.; Calkins, H.; d’Avila, A.; Chinitz, L.; Woods, C.; Gupta, S.K.; Kim, J.; Eldadah, Z.A.; Pickett, R.A.; et al. Pulsed-Field Ablation vs Conventional Thermal Ablation for Treatment of Atrial Fibrillation: A Multicenter Randomized Clinical Trial. JACC Clin. Electrophysiol. 2024, 10, 512–523. [Google Scholar]
- Steinberg, B.A.; Dorian, P.; Anstrom, K.J.; Hess, R.; Mark, D.B.; Noseworthy, P.A.; Spertus, J.A.; Piccini, J.P. Patient-Reported Outcomes in Atrial Fibrillation Research: Results of a ClinicalTrials.gov Analysis. JACC Clin. Electrophysiol. 2019, 5, 599. [Google Scholar] [CrossRef] [PubMed]
- Hussein, A.A.; Lindsay, B.; Madden, R.; Martin, D.; Saliba, W.I.; Tarakji, K.G.; Rausch, D.J.; Dresing, T.; Callahan, T.; Wazni, O.; et al. New Model of Automated Patient-Reported Outcomes Applied in Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2019, 12, e006986. [Google Scholar] [CrossRef] [PubMed]
- Baumhauer, J.F. Patient-Reported Outcomes—Are They Living Up to Their Potential? N. Engl. J. Med. 2017, 377, 6–9. [Google Scholar] [CrossRef]
- Jones, J.; Stanbury, M.; Haynes, S.; Bunting, K.V.; Lobban, T.; Camm, A.J.; Kotecha, D. Importance and Assessment of Quality of Life in Symptomatic Permanent Atrial Fibrillation: Patient Focus Groups from the RATE-AF Trial. Cardiology 2020, 145, 666–675. [Google Scholar] [CrossRef]
- Heidt, S.T.; Kratz, A.; Najarian, K.; Hassett, A.L.; Oral, H.; Gonzalez, R.; Ghanbari, H. Symptoms in Atrial Fibrillation: A Contemporary Review and Future Directions. J. Atr. Fibrillation 2016, 9, 1422. [Google Scholar]
- Björkenheim, A.; Brandes, A.; Magnuson, A.; Chemnitz, A.; Svedberg, L.; Edvardsson, N.; Poçi, D. Assessment of Atrial Fibrillation–Specific Symptoms before and 2 Years after Atrial Fibrillation Ablation: Do Patients and Physicians Differ in Their Perception of Symptom Relief? JACC Clin. Electrophysiol. 2017, 3, 1168–1176. [Google Scholar] [CrossRef]
- Schmidt, B.; Bordignon, S.; Neven, K.; Reichlin, T.; Blaauw, Y.; Hansen, J.; Adelino, R.; Ouss, A.; Füting, A.; Son, Y.-J.; et al. Health-Related Quality of Life and Associated Factors in Patients with Atrial Fibrillation: An Integrative Literature Review. Int. J. Environ. Res. Public Health 2019, 16, 3042. [Google Scholar] [CrossRef]
- Matteucci, A.; Bonanni, M.; Versaci, F.; Frati, G.; Peruzzi, M.; Sangiorgi, G.; Biondi-Zoccai, G.; Massaro, G. Cardiovascular Medicine: A Year in Review. Minerva Cardiol. Angiol. 2022, 70, 40–55. [Google Scholar] [CrossRef]
- Wang, J.; Wang, Q.; Bao, Z.; Peng, Y.; Liu, S.; Yu, T.; Wang, L.; Yang, G.; Gao, M.; Sun, G. The Combined Effects of Patient Activation and Relational Aspects on the Quality of Life in Atrial Fibrillation Patients. Front. Psychol. 2021, 12, 761149. [Google Scholar] [CrossRef]
- Schmidt, B.; Bordignon, S.; Neven, K.; Reichlin, T.; Blaauw, Y.; Hansen, J.; Adelino, R.; Ouss, A.; Füting, A.; Roten, L.; et al. European Real-World Outcomes with Pulsed Field Ablation in Patients with Symptomatic Atrial Fibrillation: Lessons from the Multi-Center EU-PORIA Registry. Europace 2023, 25, euad185. [Google Scholar] [CrossRef] [PubMed]
- Li, K.H.C.; Sang, T.; Chan, C.; Gong, M.; Liu, Y.; Jesuthasan, A.; Li, G.; Liu, T.; Lam, M.H.; Wu, W.K.; et al. Anaesthesia use in catheter ablation for atrial fibrillation: A systematic review and meta-analysis of observational studies. Heart Asia 2019, 11, e011155. [Google Scholar] [CrossRef] [PubMed]
- Mahmoodi, E.; Leitch, J.; Davies, A.; Leigh, L.; Oldmeadow, C.; Dwivedi, J.; Boyle, A.; Jackson, N. The importance of anaesthesia in atrial fibrillation ablation: Comparing conscious sedation with general anaesthesia. Indian Pacing Electrophysiol. J. 2023, 23, 47–52. [Google Scholar] [CrossRef]
- Pavlicek, V.; Wedegärtner, S.M.; Millenaar, D.; Wintrich, J.; Böhm, M.; Kindermann, I.; Ukena, C. Heart-Focused Anxiety, General Anxiety, Depression and Health-Related Quality of Life in Patients with Atrial Fibrillation Undergoing Pulmonary Vein Isolation. J. Clin. Med. 2022, 11, 1751. [Google Scholar] [CrossRef] [PubMed]
- Linde, M.; Jubele, K.; Kupics, K.; Nikitina, A.; Erglis, A. Quality of Life in Patients with Atrial Fibrillation Undergoing Pulmonary Vein Isolation: Short-Term Follow-Up Study. Medicina 2024, 60, 1594. [Google Scholar] [CrossRef]
- Al-Bashaireh, A.M.; Alkouri, O.; Alharbi, A.; Khader, Y.; Hammoudeh, A.; Aljawarneh, Y.; Alotaibi, N.E.; Qaladi, O.; Ababneh, A.; Schultz, T. Factors Associated with Quality of Life among People with Atrial Fibrillation: Jordan Atrial Fibrillation Registry Study. Medicina 2024, 60, 1262. [Google Scholar] [CrossRef]
- Di Fusco, S.A.; Aquilani, S.; Spinelli, A.; Alonzo, A.; Matteucci, A.; Castello, L.; Imperoli, G.; Colivicchi, F. The polypill strategy in cardiovascular disease prevention: It’s time for its implementation. Prog. Cardiovasc. Dis. 2023, 79, 37–40. [Google Scholar] [CrossRef]

| Category | Questions |
|---|---|
| Quality of Life | How would you rate the overall improvement in your quality of life? |
| How much has your physical activity improved since the procedure? | |
| How would you rate your mental well-being after the ablation? | |
| How much has the procedure impacted your social life? | |
| Resumption of Daily Activities | How easy was it to resume your usual daily activities post-ablation? |
| How much has the ablation improved your ability to perform household tasks? | |
| How would you rate your return to work or professional activities? | |
| How well can you tolerate physical exertion compared to before the procedure? | |
| Recovery After the Procedure | How would you describe your recovery process after the ablation? |
| How would you rate the recovery experience following anesthesia? | |
| How much pain or discomfort did you experience in the days following the procedure? | |
| How satisfied are you with the information provided regarding post-procedure care? | |
| Symptoms and Recurrences | How relieved do you feel from atrial fibrillation symptoms after the ablation? |
| How much do you notice a reduction in the frequency of AF episodes? | |
| How confident are you in the procedure’s ability to prevent recurrences? | |
| How much have palpitations or irregular heartbeats decreased after the procedure? | |
| Satisfaction | How satisfied are you with the ablation procedure overall? |
| How confident are you in the long-term benefits of the procedure? | |
| How would you rate the communication and support from the medical team? | |
| How well has the procedure met your expectations for symptom relief? |
| Total | PFA | HPSD RF | RF | Cryo | p Value | |
|---|---|---|---|---|---|---|
| Characteristics | N = 148 | N = 52 | N = 45 | N = 42 | N = 10 | |
| Age | 63.4 (7.9) | 63.9 (7.8) | 62.5 (8.3) | 63.2 (7.5) | 64.5 (7.7) | 0.57 |
| Gender (Male) | 100 (68%) | 37 (71%) | 30 (66%) | 28 (68%) | 6 (60%) | 0.53 |
| BMI | 28.4 (3.7) | 28.4 (3.8) | 28.1 (3.6) | 28.5 (3.7) | 28.8 (4.3) | 0.83 |
| Diabetes | 49 (32%) | 14 (27%) | 13 (30%) | 18 (43%) | 2 (20%) | 0.15 |
| Dyslipidemia | 82 (55%) | 30 (56%) | 20 (45%) | 23 (55%) | 4 (40%) | 0.39 |
| Hypertension | 92 (62%) | 28 (53%) | 25 (56%) | 26 (63%) | 6 (60%) | 0.46 |
| Anesthesia | 111 (75%) | 40 (77%) | 33 (73%) | 31 (72%) | 7 (70%) | 0.65 |
| AF | 0.34 | |||||
| Parossistic | 115 (77%) | 41 (78%) | 33 (73%) | 35 (83%) | 6 (60%) | |
| Persistant | 33 (23%) | 11 (21%) | 12 (26%) | 7 (16%) | 3 (30%) | |
| Questionnaire | ||||||
| Activity | 13.4 (2.4) | 15.9 (1.8) | 12 (1.4) | 11.9 (1.6) | 12.1 (1.2) | <0.001 |
| Recovery | 15.8 (2.8) | 16.3 (2.3) | 15.5 (3.1) | 15.4 (2.8) | 15.5 (3.4) | 0.39 |
| QoL | 16.1 (2.8) | 18.2 (1.7) | 15 (2.3) | 14.5 (2.7) | 13.7 (2.5) | <0.001 |
| Satisfaction | 11.9 (1.7) | 11.9 (1.8) | 11.9 (1.79) | 12 (1.6) | 11.6 (1.7) | 0.94 |
| Syntoms | 10.7 (2.9) | 7.8 (1.6) | 12.3 (2) | 12.2 (2.5) | 12.2 (1) | <0.001 |
| Total Score | 67.9 (5.6) | 69.7 (4.5) | 66.7 (6.1) | 67.1 (6) | 67.4 (5.6) | 0.001 |
| Total | Deep Sedation | General Anesthesia | p Value | Propofol | Remifentanil | p Value | |
|---|---|---|---|---|---|---|---|
| N = 148 | N = 37 | N = 111 | N = 69 | N = 42 | |||
| Activity | 13.4 (2.5) | 13.2(2.5) | 13.4 (2.5) | 0.64 | 13.4 (2.4) | 13.5 (2.6) | 0.83 |
| Recovery | 15.8 (2.8) | 11.8 (1.5) | 17 (1.7) | <0.001 | 16.1 (1.7) | 18.3 (.9) | <0.001 |
| QoL | 16 (2.8) | 12.5 (2.5) | 17.1 (2) | <0.001 | 17 (1.8) | 17 (2.1) | 0.90 |
| Satisfaction | 11.9 (1.7) | 11.8 (1.5) | 11.9 (1.8) | 0.79 | 11.8 (1.9) | 12.1 (1.6) | 0.38 |
| Syntoms | 10.7 (2.9) | 10.7 (1.8) | 10.7 (3.1) | 0.93 | 10.6 (2.9) | 10.7 (3.5) | 0.87 |
| Total Score | 67.9 (5.6) | 60.8 (4.2) | 70.2 (3.9) | <0.001 | 69.3 (3.7) | 71.7 (3.7) | <0.001 |
| Coeffient | Standard Error | p Value | Confidence Interval | ||
|---|---|---|---|---|---|
| Deep Sedation | |||||
| Age | −0.04 | 0.07 | 0.579 | −0.173 | 0.0958 |
| Gender | −0.96 | 1.2 | 0.426 | −3.35 | 1.432 |
| BMI | −0.27 | 0.13 | 0.041 | −0.537 | −0.0113 |
| AF | −0.9 | 1.37 | 0.513 | −3.64 | 1.836 |
| Energy | −1.98 | 0.49 | 0.0 | −2.953 | 1.001 |
| General Anesthesia | |||||
| Age | 0.02 | 0.03 | 0.535 | −0.0437 | 0.0839 |
| Gender | 0.21 | 0.54 | 0.704 | −0.859 | 1.271 |
| BMI | −0.08 | 0.06 | 0.21 | −0.198 | 0.0439 |
| AF | −0.44 | 0.65 | 0.497 | −1.719 | 0.837 |
| Anesthetic Drug | 2.51 | 0.51 | 0.001 | 1.505 | 3.504 |
| Energy | −0.75 | 0.24 | 0.002 | −1.226 | −0.265 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matteucci, A.; Russo, M.; Galeazzi, M.; Pandozi, C.; Bonanni, M.; Mariani, M.V.; Pierucci, N.; La Fazia, V.M.; Di Fusco, S.A.; Nardi, F.; et al. Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study. J. Clin. Med. 2025, 14, 2741. https://doi.org/10.3390/jcm14082741
Matteucci A, Russo M, Galeazzi M, Pandozi C, Bonanni M, Mariani MV, Pierucci N, La Fazia VM, Di Fusco SA, Nardi F, et al. Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study. Journal of Clinical Medicine. 2025; 14(8):2741. https://doi.org/10.3390/jcm14082741
Chicago/Turabian StyleMatteucci, Andrea, Maurizio Russo, Marco Galeazzi, Claudio Pandozi, Michela Bonanni, Marco Valerio Mariani, Nicola Pierucci, Vincenzo Mirco La Fazia, Stefania Angela Di Fusco, Federico Nardi, and et al. 2025. "Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study" Journal of Clinical Medicine 14, no. 8: 2741. https://doi.org/10.3390/jcm14082741
APA StyleMatteucci, A., Russo, M., Galeazzi, M., Pandozi, C., Bonanni, M., Mariani, M. V., Pierucci, N., La Fazia, V. M., Di Fusco, S. A., Nardi, F., & Colivicchi, F. (2025). Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study. Journal of Clinical Medicine, 14(8), 2741. https://doi.org/10.3390/jcm14082741






