Redefining Knee Arthroplasty: Does Robotic Assistance Improve Outcomes Beyond Alignment? An Evidence-Based Umbrella Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Structure of the Umbrella Review
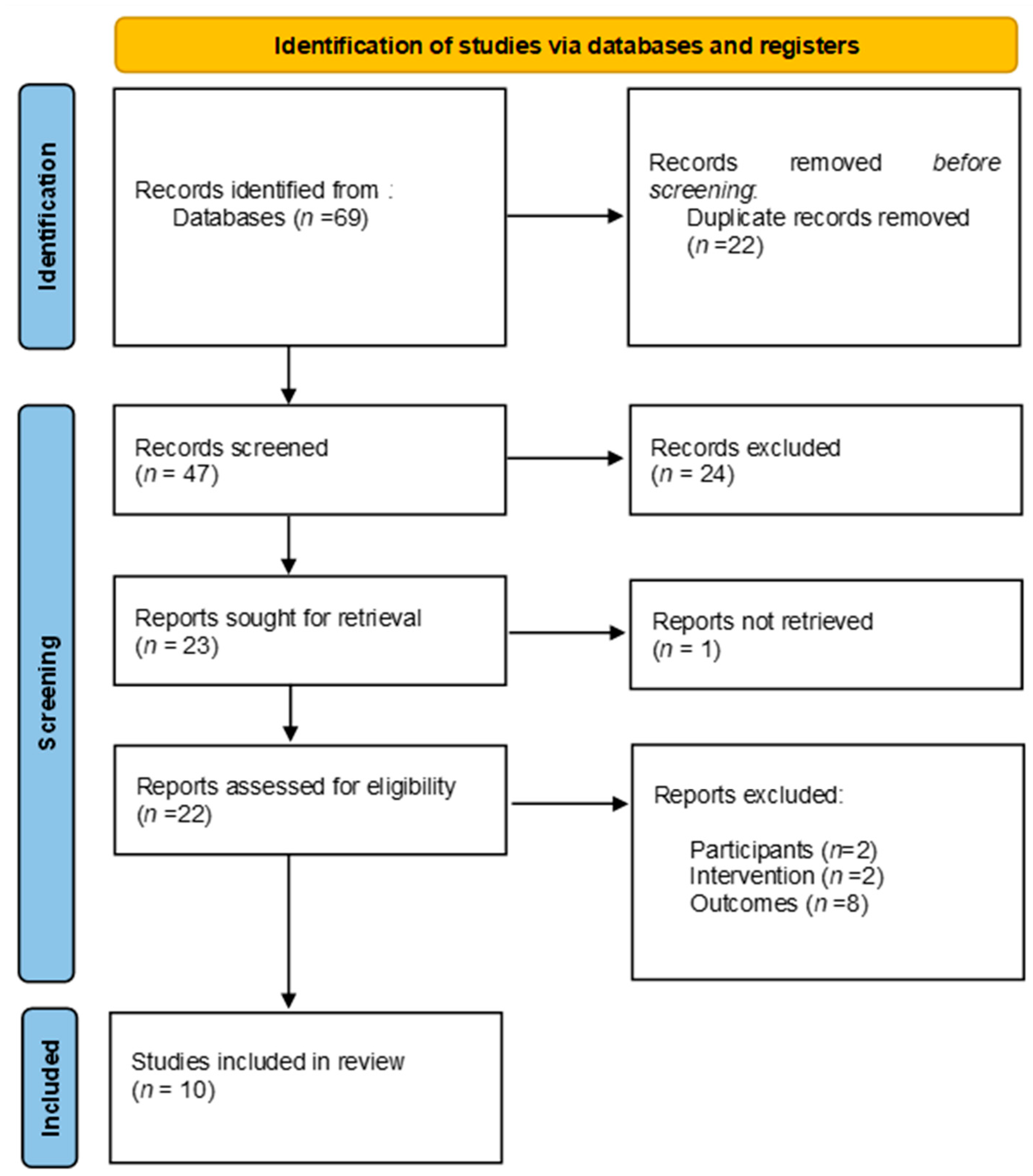
2.2. Search Strategy
2.3. Selection and Screening of Systematic Reviews
- Study characteristics (author, year, population, sample size, type of robot-assisted system).
- Outcomes of interest (hospital stay, physical outcomes).
- Risk of bias assessment (as reported in the review or meta-analysis).
- Effect sizes (e.g., mean difference, standardized mean difference) for hospital stay and physical outcomes.
2.4. Methodological Quality Assessment
3. Results
3.1. Description of the Included Systematic Reviews
3.2. Methodological Quality of the Included Systematic Reviews
3.3. Risk of Bias in the Included Systematic Reviews
3.4. Summary and Consistency of the Evidence
3.4.1. Hospital Stay
3.4.2. Postoperative Alignment
3.4.3. Range of Motion
3.4.4. Postoperative Pain
3.4.5. Functional Performance
4. Discussion
5. Limitations
6. Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.K.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Dalury, D.F.; Pomeroy, D.L.; Gorab, R.S.; Adams, M.J. Why are Total Knee Arthroplasties Being Revised? J. Arthroplast. 2013, 28, 120–121. [Google Scholar] [CrossRef]
- Deckey, D.G.; Rosenow, C.S.; Verhey, J.T.; Brinkman, J.C.; Mayfield, C.K.; Clarke, H.D.; Bingham, J.S. Robotic-assisted total knee arthroplasty improves accuracy and precision compared to conventional techniques. Bone Jt. J. 2021, 103, 74–80. [Google Scholar] [CrossRef]
- Antonios, J.K.; Korber, S.; Sivasundaram, L.; Mayfield, C.; Kang, H.P.; Oakes, D.A.; Heckmann, N.D. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: An analysis of patient and hospital factors. Arthroplast. Today 2019, 5, 88–95. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Valdes, K.; Pedersini, P.; Berjano, P. Osteoarthritis: A call for research on central pain mechanism and personalized pre-vention strategies. Clin. Rheumatol. 2019, 38, 583–584. [Google Scholar] [CrossRef]
- Fozo, Z.A.; Ghazal, A.H.; Hesham Gamal, M.; Matar, S.G.; Kamal, I.; Ragab, K.M. A Systematic Review and Meta-Analysis of Conventional Versus Robotic-Assisted Total Knee Arthroplasty. Cureus 2023, 15, e46845. [Google Scholar] [CrossRef]
- Pedersini, P.; Turroni, S.; Villafañe, J.H. Gut microbiota and physical activity: Is there an evidence-based link? Sci. Total Environ. 2020, 727, 138648. [Google Scholar] [CrossRef]
- Ioannidis, J.P.A. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Can. Med. Assoc. J. 2009, 181, 488–493. [Google Scholar] [CrossRef]
- Smith, V.; Devane, D.; Begley, C.M.; Clarke, M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 2011, 11, 15. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R.; ROBIS Group. A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Mannan, A.; Vun, J.; Lodge, C.; Eyre-Brook, A.; Jones, S. Increased precision of coronal plane outcomes in robotic-assisted total knee arthroplasty: A systematic review and meta-analysis. Surgeon 2018, 16, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Batailler, C.; Fernandez, A.; Swan, J.; Servien, E.; Haddad, F.S.; Catani, F.; Lustig, S. MAKO CT-based robotic arm-assisted system is a reliable procedure for total knee arthroplasty: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3585–3598. [Google Scholar] [CrossRef]
- Fu, X.; She, Y.; Jin, G.; Liu, C.; Liu, Z.; Li, W.; Jin, R. Comparison of robotic-assisted total knee arthroplasty: An updated systematic review and meta-analysis. J. Robot. Surg. 2024, 18, 292. [Google Scholar] [CrossRef]
- Mancino, F.; Cacciola, G.; Malahias, M.-A.; De Filippis, R.; De Marco, D.; Di Matteo, V.; Gu, A.; Sculco, P.K.; Maccauro, G.; De Martino, I. What are the benefits of robotic-assisted total knee arthroplasty over conventional manual total knee arthroplasty? A systematic review of comparative studies. Orthop. Rev. 2020, 12, 15–22. [Google Scholar] [CrossRef]
- Migliorini, F.; Pilone, M.; Schäfer, L.; Simeone, F.; Bell, A.; Maffulli, N. Functional alignment in robotic-assisted total knee arthroplasty: A systematic review. Arch. Orthop. Trauma. Surg. 2024, 144, 1741–1749. [Google Scholar] [CrossRef]
- Nogalo, C.; Meena, A.; Abermann, E.; Fink, C. Complications and downsides of the robotic total knee arthroplasty: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 736–750. [Google Scholar] [CrossRef]
- Onggo, J.R.; Onggo, J.D.; De Steiger, R.; Hau, R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: A meta-analysis and systematic review. Arch. Orthop. Trauma. Surg. 2020, 140, 1533–1549. [Google Scholar] [CrossRef]
- Thienpont, E.; Fennema, P.; Price, A. Can technology improve alignment during knee arthroplasty. Knee 2013, 20, S21–S28. [Google Scholar] [CrossRef]
- Mullaji, A.B.; Khalifa, A.A. Is it prime time for robotic-assisted TKAs? A systematic review of current studies. J. Orthop. 2022, 34, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Cao, S.; Wu, J.; Weng, X.; Feng, B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2019, 95, 125–133. [Google Scholar] [CrossRef] [PubMed]
- van de Graaf, V.A.; Clark, G.W.; Collopy, D.; Wood, J.A.; Chen, D.B.; MacDessi, S.J. Functional alignment minimizes changes to joint line obliquity in robotic-assisted total knee arthroplasty: A CT analysis of functional versus kinematic alignment in 2,116 knees using the Coronal Plane Alignment of the Knee (CPAK) classification. Bone Jt. Open 2024, 5, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, T.; Igarashi, T.; Takada, K.; Yoshizawa, S.; Ikegami, H.; Musha, Y. Robotic-assisted total knee arthroplasty improves the outlier of rotational alignment of the tibial prosthesis using 3DCT measurements. Knee 2021, 31, 64–76. [Google Scholar] [CrossRef]
- Song, E.-K.; Seon, J.-K.; Yim, J.-H.; Netravali, N.A.; Bargar, W.L. Robotic-assisted TKA Reduces Postoperative Alignment Outliers and Improves Gap Balance Compared to Conventional TKA. Clin. Orthop. Relat. Res. 2013, 471, 118–126. [Google Scholar] [CrossRef]
- Maman, D.; Laver, L.; Becker, R.; Mahamid, A.; Berkovich, Y. Robotic-assisted total knee arthroplasty reduces postoperative complications and length of stay without increased cost compared to navigation-guided techniques: A national analysis. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 336–342. [Google Scholar] [CrossRef]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Pietrzak, J.R.T.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Jt. J. 2018, 100, 930–937. [Google Scholar] [CrossRef]
- Hua, Y.; Salcedo, J. Cost-effectiveness analysis of robotic-arm assisted total knee arthroplasty. PLoS ONE 2022, 17, e0277980. [Google Scholar] [CrossRef]
- Zhang, J.J.Y.; Chen, J.Y.; Tay, D.K.J.; Pang, H.N.; Yeo, S.J.; Liow, M.H.L. Cost-Effectiveness of Robot-Assisted Total Knee Arthroplasty: A Markov Decision Analysis. J. Arthroplast. 2023, 38, 1434–1437. [Google Scholar] [CrossRef]
- Yang, H.-Y.; Seon, J.-K.; Yim, J.-H.; Lee, D.-H.; Song, E.-K. Functional Alignment Achieved a More Balanced Knee After Robotic Arm-Assisted Total Knee Arthroplasty than Modified Kinematic Alignment. J. Clin. Med. 2025, 14, 820. [Google Scholar] [CrossRef]
- Fary, C.; Cholewa, J.; Ren, A.N.; Abshagen, S.; Anderson, M.B.; Tripuraneni, K. Multicenter, prospective cohort study: Immediate postoperative gains in active range of motion following robotic-assisted total knee replacement compared to a propensity-matched control using manual instrumentation. Arthroplast. 2023, 5, 62. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.-J.; Ra, H.J. Patient Satisfaction after Total Knee Arthroplasty. Knee Surg. Relat. Res. 2016, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Hoveidaei, A.H.; Esmaeili, S.; Ghaseminejad-Raeini, A.; Pirahesh, K.; Fallahi, M.S.; Sandiford, N.A.; Citak, M. Robotic assisted Total Knee Arthroplasty (TKA) is not associated with increased patient satisfaction: A systematic review and meta-analysis. Int. Orthop. 2024, 48, 1771–1784. [Google Scholar] [CrossRef] [PubMed]
- Pagani, N.R.; Menendez, M.E.; Moverman, M.A.; Puzzitiello, R.N.; Gordon, M.R. Adverse Events Associated With Robotic-Assisted Joint Arthroplasty: An Analysis of the US Food and Drug Administration MAUDE Database. J. Arthroplast. 2022, 37, 1526–1533. [Google Scholar] [CrossRef]

| Study | Included Studies | Participants | Intervention | Comparison | Outcomes | Conclusions/Results |
|---|---|---|---|---|---|---|
| Batailler et al., 2020 [14] | 14 | 9084 (3090 RA-TKAs, 5994 conventional TKA) | MAKO CT-based robotic arm-assisted TKA | Conventional manual TKA | Accuracy of alignment, pain, hospital stay, soft tissue injury | RA-TKA improves alignment accuracy and reduces soft tissue injuries but is costlier and time-intensive. |
| Fu et al., 2024 [15] | 12 | 2863 (1449 RA-TKAs and 1414 M-TKAs) | Robotic-assisted total knee arthroplasty (RA-TKA) | Manual total knee arthroplasty (M-TKA) | KSS, WOMAC, OKS, ROM, HKA angle, component angles, satisfaction | RA-TKA yields better alignment accuracy but no superior clinical outcomes compared to M-TKA over time. |
| Mancino et al., 2020 [16] | 9 | 1199 (614 RA, 585 CM) | Robotic (RA) TKA | Conventional (CM) TKA | Implant survivorship, complications, clinical outcomes, radiographic outcomes | Improved radiographic outcomes (fewer radiolucent lines and deviations in RA); no significant differences in operative time and complications. |
| Mannan et al., 2018 [13] | 5 | 402 | Robotic-assisted TKA | Conventional TKA | Mechanical axis alignment, tibial and femoral alignment, operative time, blood loss | Robotic-assisted TKA achieved significantly more accurate alignment with fewer mechanical axis deviations (>3°) compared to conventional TKA. Additionally, reduced blood loss and longer operative times were observed. |
| Migliorini et al., 2024 [17] | 7 | 1198 (100 conventional TKA, 1098 RA-TKAs or computer-assisted) | Robotic (RA) TKA | Conventional (CM) TKA or computer assisted | Resection accuracy, implant alignment, gap balancing | FA shows better results in precision and alignment, but more long-term evidence is needed. |
| Nogalo et al., 2023 [18] | 21 | Not specified | Robotic TKA | Conventional TKA | Complications, operative duration, costs, infection rates | Robotic TKA associated with complications such as pin-hole fractures, iatrogenic injuries, excessive blood loss, and pin-site infections. Longer surgical duration and higher intraoperative costs were also reported. |
| Onggo et al., 2020 [19] | 18 | 6534 (2234 RA, 4300 CM) | Robotic (rTKA) | Conventional (cTKA) | Clinical outcomes, radiographic outcomes, complications, perioperative parameters, and costs | rTKA reduces blood loss and improves alignment, but the long-term clinical impact is marginal. |
| Thienpont et al., 2013 [20] | 30 | Not specified | Computer-assisted navigation, Patient-Matched Instrumentation (PMI), Robotic-assisted implantation | Conventional instrumentation | Mechanical alignment, operative time, malalignment | Computer-assisted navigation reduced the number of alignment deviations (>2° and >3°) compared to conventional instrumentation. Patient-Matched Instrumentation (PMI) and robotic implantation showed mixed results, with some improvements in alignment but limited demonstrated clinical benefits |
| Mullaji et al., 2022 [21] | 13 | 2112 knees | Robotic-Assisted Total Knee Arthroplasty (RATKA) | Conventional Total Knee Arthroplasty (CTKA) | Operative time, Length of stay, Functional outcomes, Alignment, Complications | Robotic-assisted TKA provides better component alignment and early functional outcomes. However, there is limited evidence of its superiority over CTKA in terms of long-term outcomes. Operative times are generally longer for RATKA, but hospital stays may be shorter. Complication rates are similar between RATKA and CTKA. |
| Ren et al., 2018 [22] | 7 studies (6 RCTs and 1 retrospective) | 486 patients, 517 knees | Robot-assisted TKA (ROBODOC, CASPAR) | Conventional TKA | Accuracy of mechanical alignment and implant positioning; Functional scores (WOMAC, KSS, HSS); Complications (blood loss, surgical time, ROM) | Improved mechanical alignment and implant positioning accuracy; Better functional scores (WOMAC, KSS); Reduced blood loss; No significant differences in surgical time, ROM, or complication rates; Further studies are needed. |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | Overall |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Batailler et al., 2020 [14] | Yes | Partial Yes | Yes | Yes | No | No | No | Partial Yes | Yes | No | NA | NA | No | Yes | NA | Yes | Critically low |
| Fu et al., 2024 [15] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Mancino et al., 2020 [16] | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Partial Yes | No | NA | NA | Yes | No | NA | Yes | Critically low |
| Mannan et al., 2018 [13] | Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
| Migliorini et al., 2024 [17] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | NA | NA | Yes | No | NA | Yes | Low |
| Mullaji et al., 2022 [21] | Yes | No | Yes | Yes | Yes | No | No | Yes | No | No | NA | NA | No | No | NA | Yes | Critically low |
| Nogalo et al., 2023 [18] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | NA | NA | Yes | Yes | NA | Yes | High |
| Onggo et al., 2020 [19] | Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Moderate |
| Ren et al., 2018 [22] | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | High |
| Thienpont et al., 2013 [20] | Yes | Partial Yes | Yes | Yes | Yes | Yes | No | Yes | No | No | NA | NA | No | No | NA | Yes | Critically low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Sanz, F.; Sosa-Reina, M.D.; Jaén-Crespo, G.; González-de-la-Flor, Á.; Villafañe, J.H.; Romero-Morales, C. Redefining Knee Arthroplasty: Does Robotic Assistance Improve Outcomes Beyond Alignment? An Evidence-Based Umbrella Review. J. Clin. Med. 2025, 14, 2588. https://doi.org/10.3390/jcm14082588
García-Sanz F, Sosa-Reina MD, Jaén-Crespo G, González-de-la-Flor Á, Villafañe JH, Romero-Morales C. Redefining Knee Arthroplasty: Does Robotic Assistance Improve Outcomes Beyond Alignment? An Evidence-Based Umbrella Review. Journal of Clinical Medicine. 2025; 14(8):2588. https://doi.org/10.3390/jcm14082588
Chicago/Turabian StyleGarcía-Sanz, Fernando, María Dolores Sosa-Reina, Gonzalo Jaén-Crespo, Ángel González-de-la-Flor, Jorge Hugo Villafañe, and Carlos Romero-Morales. 2025. "Redefining Knee Arthroplasty: Does Robotic Assistance Improve Outcomes Beyond Alignment? An Evidence-Based Umbrella Review" Journal of Clinical Medicine 14, no. 8: 2588. https://doi.org/10.3390/jcm14082588
APA StyleGarcía-Sanz, F., Sosa-Reina, M. D., Jaén-Crespo, G., González-de-la-Flor, Á., Villafañe, J. H., & Romero-Morales, C. (2025). Redefining Knee Arthroplasty: Does Robotic Assistance Improve Outcomes Beyond Alignment? An Evidence-Based Umbrella Review. Journal of Clinical Medicine, 14(8), 2588. https://doi.org/10.3390/jcm14082588







