Patient Satisfaction with IBD Undergoing Colonoscopy: A Multicenter Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Outcomes
- To examine how stress levels influence patient satisfaction, the expertise of endoscopists and nurses, disease activity, and various clinical factors (e.g., pathology type, surgical history, preparation methods, and sedation type).
- To evaluate the determinants of patient satisfaction undergoing an endoscopic examination.
2.2. Design
2.3. Participants
2.4. Instruments
2.4.1. Pre-Exam Patient Assessment
2.4.2. Post-Exam Patient Assessment
2.5. Endoscopy Customer Satisfaction Questionnaire (ECSQ)
2.6. Perceived Stress Scale (PSS-10)
2.7. Disease Activity Assessment
2.8. Data Analysis
2.9. Ethical Considerations
3. Results
3.1. Relationship Between Patient Satisfaction and Stress Levels, Endoscopist and Nurse Expertise, Disease Activity, and Clinical Variables
3.2. Relationship Between Patient Satisfaction and Healthcare Workers Competence
3.3. Relationship Between Patient Satisfaction and Clinical Variables
3.4. Determinants and Predictors of Patient Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Friedman, S.; Cheifetz, A.S.; Farraye, F.A.; Banks, P.A.; Makrauer, F.L.; Burakoff, R.; Farmer, B.; Torgersen, L.N.; Wahl, K.E. Factors That Affect Adherence to Surveillance Colonoscopy in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2013, 19, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Sturm, A.; Maaser, C.; Calabrese, E.; Annese, V.; Fiorino, G.; Kucharzik, T.; Vavricka, S.R.; Verstockt, B.; van Rheenen, P.; Tolan, D.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD Scores and General Principles and Technical Aspects. J. Crohns Colitis 2019, 13, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Gönczi, L.; Lakatos, P.L.; Burisch, J. The Burden of Inflammatory Bowel Disease in Europe in 2020. J Crohns Colitis 2021, 15, 1573–1587. [Google Scholar] [CrossRef] [PubMed]
- Crocetti, E.; Bergamaschi, W.; Russo, A.G. Population-Based Incidence and Prevalence of Inflammatory Bowel Diseases in Milan (Northern Italy), and Estimates for Italy. Eur. J. Gastroenterol. Hepatol. 2021, 33, e383–e389. [Google Scholar] [CrossRef]
- Bessissow, T.; Van Keerberghen, C.-A.; Van Oudenhove, L.; Ferrante, M.; Vermeire, S.; Rutgeerts, P.; Van Assche, G. Anxiety Is Associated with Impaired Tolerance of Colonoscopy Preparation in Inflammatory Bowel Disease and Controls. J. Crohns Colitis 2013, 7, e580–e587. [Google Scholar] [CrossRef]
- Narula, N.; Pinto-Sanchez, M.I.; Calo, N.C.; Ford, A.C.; Bercik, P.; Reinisch, W.; Moayyedi, P. Anxiety But Not Depression Predicts Poor Outcomes in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2019, 25, 1255–1261. [Google Scholar] [CrossRef]
- Sint Nicolaas, J.; de Jonge, V.; Korfage, I.J.; Ter Borg, F.; Brouwer, J.T.; Cahen, D.L.; Lesterhuis, W.; Ouwendijk, R.J.T.; Kuipers, E.J.; van Leerdam, M.E. Benchmarking Patient Experiences in Colonoscopy Using the Global Rating Scale. Endoscopy 2012, 44, 462–472. [Google Scholar] [CrossRef]
- Harewood, G.C.; Wiersema, M.J.; Melton, L.J. A Prospective, Controlled Assessment of Factors Influencing Acceptance of Screening Colonoscopy. Am. J. Gastroenterol. 2002, 97, 3186–3194. [Google Scholar] [CrossRef]
- Mirza, R.M.; MacKean, G.; Shaffer, S.R.; Sewitch, M.J.; Heisler, C.; McLeod, J.; Habashi, P.; MacDonald, K.V.; Barker, K.; Nguyen, G.C.; et al. Patient Experiences in the Management of Inflammatory Bowel Disease: A Qualitative Study. J. Can. Assoc. Gastroenterol. 2022, 5, 261–270. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.; Pittet, V.; Rossel, J.-B.; von Känel, R.; Swiss IBD Cohort Study Group. Symptoms of Depression and Anxiety Are Independently Associated With Clinical Recurrence of Inflammatory Bowel Disease. Clin. Gastroenterol. Hepatol. 2016, 14, 829–835.e1. [Google Scholar] [CrossRef]
- Lontai, L.; Elek, L.P.; Balogh, F.; Angyal, D.; Pajkossy, P.; Gonczi, L.; Lakatos, P.L.; Iliás, Á. Burden of Mental Health among Patients with Inflammatory Bowel Disease-A Cross-Sectional Study from a Tertiary IBD Center in Hungary. J. Clin. Med. 2024, 13, 2002. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, D.; Settanni, C.R.; Parisio, L.; Orgiana, N.; Poscia, A.; Schiavoni, E.; Turchini, L.; Cascio, A.L.; Germini, F.; Sblendorio, E.; et al. Transition from Intravenous to Subcutaneous Biological Therapies in Inflammatory Bowel Disease: An Online Survey of Patients. Indian J. Gastroenterol. 2024, 43, 215–225. [Google Scholar] [CrossRef]
- Volpato, E.; Bosio, C.; Previtali, E.; Leone, S.; Armuzzi, A.; Pagnini, F.; Graffigna, G. The Evolution of IBD Perceived Engagement and Care Needs across the Life-Cycle: A Scoping Review. BMC Gastroenterol. 2021, 21, 293. [Google Scholar] [CrossRef]
- Introduction of the Nurse Endoscopist Role in One Australian Health Service—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/28957967/ (accessed on 10 March 2025).
- Nurse-Performed Endoscopy: Implications for the Nursing Profession in Australia—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/28558517/ (accessed on 10 March 2025).
- Mahawongkajit, P.; Techagumpuch, A.; Auksornchat, K. Effects of Basic Endoscopic Handling and Care Training on Gastrointestinal Endoscopy Logistics. Endosc. Int. Open 2022, 10, E56–E61. [Google Scholar] [CrossRef]
- Spier, B.J.; Benson, M.; Pfau, P.R.; Nelligan, G.; Lucey, M.R.; Gaumnitz, E.A. Colonoscopy Training in Gastroenterology Fellowships: Determining Competence. Gastrointest. Endosc. 2010, 71, 319–324. [Google Scholar] [CrossRef]
- Testoni, P.A.; Notaristefano, C.; Soncini, M.; Hassan, C.; Monica, F.; Radaelli, F.; Triossi, O.; Pasquale, L.; Neri, M.; Cannizzaro, R.; et al. An Italian Prospective Multicenter Study on Colonoscopy Practice and Quality: What Has Changed in the Last 10 Years. Dig. Liver Dis. 2023, 55, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Lai, E.J.; Calderwood, A.H.; Doros, G.; Fix, O.K.; Jacobson, B.C. The Boston Bowel Preparation Scale: A Valid and Reliable Instrument for Colonoscopy-Oriented Research. Gastrointest. Endosc. 2009, 69, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Minciullo, A.; Tartaglini, D.; Colombo, B.; Filomeno, L.; Di Muzio, M. Assessing Validity and Reliability of a New Tool: The ECSQ (Endoscopy Customer Satisfaction Question-Naire) in Italian for Customer Satisfaction in Digestive Endoscopy. Ann. Ig. 2022, 34, 166–176. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Sewitch, M.J.; Gong, S.; Dube, C.; Barkun, A.; Hilsden, R.; Armstrong, D. A Literature Review of Quality in Lower Gastrointestinal Endoscopy from the Patient Perspective. Can. J. Gastroenterol. 2011, 25, 681–685. [Google Scholar] [CrossRef]
- Sargin, M.; Uluer, M.S.; Aydogan, E.; Hanedan, B.; Tepe, M.İ.; Eryılmaz, M.A.; Ebem, E.; Özmen, S. Anxiety Levels in Patients Undergoing Sedation for Elective Upper Gastrointestinal Endoscopy and Colonoscopy. Med. Arch. 2016, 70, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.D.; Chuai, S.; Nessel, L.; Lichtenstein, G.R.; Aberra, F.N.; Ellenberg, J.H. Use of the Noninvasive Components of the Mayo Score to Assess Clinical Response in Ulcerative Colitis. Inflamm. Bowel Dis. 2008, 14, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Daperno, M.; D’Haens, G.; Van Assche, G.; Baert, F.; Bulois, P.; Maunoury, V.; Sostegni, R.; Rocca, R.; Pera, A.; Gevers, A.; et al. Development and Validation of a New, Simplified Endoscopic Activity Score for Crohn’s Disease: The SES-CD. Gastrointest. Endosc. 2004, 60, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.F.; Bradshaw, J.M. A Simple Index of Crohn’s-Disease Activity. Lancet 1980, 1, 514. [Google Scholar] [CrossRef]
- Denters, M.J.; Schreuder, M.; Depla, A.C.T.M.; Mallant-Hent, R.C.; van Kouwen, M.C.A.; Deutekom, M.; Bossuyt, P.M.; Fockens, P.; Dekker, E. Patients’ Perception of Colonoscopy: Patients with Inflammatory Bowel Disease and Irritable Bowel Syndrome Experience the Largest Burden. Eur. J. Gastroenterol. Hepatol. 2013, 25, 964–972. [Google Scholar] [CrossRef]
- Tolerability of Bowel Preparation and Colonoscopy in IBD Patients: Results From a Prospective, Single-Center, Case-Control Study—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/36777747/ (accessed on 10 March 2025).
- Shahini, E.; Sinagra, E.; Vitello, A.; Ranaldo, R.; Contaldo, A.; Facciorusso, A.; Maida, M. Factors Affecting the Quality of Bowel Preparation for Colonoscopy in Hard-to-Prepare Patients: Evidence from the Literature. World J. Gastroenterol. 2023, 29, 1685–1707. [Google Scholar] [CrossRef]
- Wang, C.; Sheng, Y.; Yu, L.; Tian, F.; Xue, Y.; Zhai, Q. Effects of Cognitive Behavioral Therapy on Mental Health and Quality of Life in Inflammatory Bowel Disease Patients: A Meta-Analysis of Randomized Controlled Trials. Behav. Brain Res. 2023, 454, 114653. [Google Scholar] [CrossRef]
- Chen, J.; Chen, X.; Sun, Y.; Xie, Y.; Wang, X.; Li, R.; Hesketh, T. The Physiological and Psychological Effects of Cognitive Behavior Therapy on Patients with Inflammatory Bowel Disease before COVID-19: A Systematic Review. BMC Gastroenterol. 2021, 21, 469. [Google Scholar] [CrossRef]
- Effective Communication Enhances the Patients’ Endoscopy Experience—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/25690478/ (accessed on 10 March 2025).
- Spadaccini, M.; Frazzoni, L.; Vanella, G.; East, J.; Radaelli, F.; Spada, C.; Fuccio, L.; Benamouzig, R.; Bisschops, R.; Bretthauer, M.; et al. Efficacy and Tolerability of High- vs Low-Volume Split-Dose Bowel Cleansing Regimens for Colonoscopy: A Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2020, 18, 1454–1465.e14. [Google Scholar] [CrossRef]
- Beran, A.; Aboursheid, T.; Ali, A.H.; Albunni, H.; Mohamed, M.F.; Vargas, A.; Hadaki, N.; Alsakarneh, S.; Rex, D.K.; Guardiola, J.J. Risk Factors for Inadequate Bowel Preparation in Colonoscopy: A Comprehensive Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2024, 119, 2389–2397. [Google Scholar] [CrossRef]
- Dubian, S.; Yzet, C.; Brazier, F.; Yzet, T.; Hautefeuille, V.; Decrombecque, C.; Bocquillon, Q.; Richard, N.; Buisson, A.; Meynier, J.; et al. Fecal Calprotectin, Intestinal Ultrasound, and Their Combination for the Diagnosis of Inflammatory Bowel Disease. Clin. Res. Hepatol. Gastroenterol. 2025, 49, 102549. [Google Scholar] [CrossRef]
- Correia, J.C.; Waqas, A.; Assal, J.-P.; Davies, M.J.; Somers, F.; Golay, A.; Pataky, Z. Effectiveness of Therapeutic Patient Education Interventions for Chronic Diseases: A Systematic Review and Meta-Analyses of Randomized Controlled Trials. Front. Med. 2022, 9, 996528. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.-H.; Peng, Y.-C.; Lin, Y.-T.; Chang, C.-S.; Ou, M.-C. Aromatherapy for Reducing Colonoscopy Related Procedural Anxiety and Physiological Parameters: A Randomized Controlled Study. Hepatogastroenterology 2010, 57, 1082–1086. [Google Scholar] [PubMed]
- Lazar Barzegar, S.; Mohammadi, S.; Shamsalinia, A.; Saberifar, M. The Effects of White Noise on Preprocedural Anxiety and Vital Signs Among Older Adults Undergoing Colonoscopy. J. Perianesth Nurs. 2024, 39, 386–390. [Google Scholar] [CrossRef]
- Shipley, R.H.; Butt, J.H.; Farbry, J.E.; Horwitz, B. Psychological Preparation for Endoscopy. Physiological and Behavioral Changes in Patients with Differing Coping Styles for Stress. Gastrointest. Endosc. 1977, 24, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Behrouzian, F.; Sadrizadeh, N.; Nematpour, S.; Seyedian, S.S.; Nassiryan, M.; Zadeh, A.J.F. The Effect of Psychological Preparation on the Level of Anxiety before Upper Gastrointestinal Endoscopy. J. Clin. Diagn. Res. 2017, 11, VC01–VC04. [Google Scholar] [CrossRef]
- Sulosaari, V.; Unal, E.; Cinar, F.I. The Effectiveness of Mindfulness-Based Interventions on the Psychological Well-Being of Nurses: A Systematic Review. Appl. Nurs. Res. 2022, 64, 151565. [Google Scholar] [CrossRef]
- Broder, E.; Davies, A.; Alrubaiy, L. Using Information Videos to Improve Patient Satisfaction in Endoscopy: A Prospective Service Improvement Project. Cureus 2022, 14, e24108. [Google Scholar] [CrossRef]
- Peña, L.R.; Mardini, H.E.; Nickl, N.J. Development of an Instrument to Assess and Predict Satisfaction and Poor Tolerance among Patients Undergoing Endoscopic Procedures. Dig. Dis. Sci. 2005, 50, 1860–1871. [Google Scholar] [CrossRef]
- Lin, O.S. Less Stick, More Carrot: Measuring and Improving Patient Satisfaction with Endoscopic Procedures. Gastrointest. Endosc. 2009, 69, 892–895. [Google Scholar] [CrossRef]
- Yacavone, R.F.; Locke, G.R.; Gostout, C.J.; Rockwood, T.H.; Thieling, S.; Zinsmeister, A.R. Factors Influencing Patient Satisfaction with GI Endoscopy. Gastrointest. Endosc. 2001, 53, 703–710. [Google Scholar] [CrossRef] [PubMed]
| Variables | Entire Sample (n = 444) |
|---|---|
| Smoker | |
| Yes | 94 (21.2%) |
| No | 350 (78.8%) |
| First Colonscopy | |
| Yes | 92 (20.7%) |
| No | 352 (79.3%) |
| Symptoms | |
| Yes | 322 (72.5%) |
| No | 122 (27.5%) |
| Previous Pathologies | |
| Yes | 344 (77.5%) |
| No | 100 (22.6%) |
| Previous Surgeries | |
| Yes | 224 (50.5%) |
| No | 219 (49.4%) |
| Stoma | |
| Yes | 16 (3.6%) |
| No | 428 (96.4%) |
| Type of Preparation | |
| High volume | 60 (13.5%) |
| Low volume | 384 (86.5%) |
| Preparation Timing | |
| Day before | 288 (64.8%) |
| Split | 151 (34.1%) |
| Same day | 5 (1.1%) |
| Exam Completed | |
| Yes | 367 (82.6%) |
| No | 77 (17.3%) |
| Feeling of Cleanliness | |
| Low | 36 (8.1%) |
| Medium | 162 (36.5%) |
| High | 246 (55.4%) |
| Sedation | |
| No | 46 (10.4%) |
| Conscious sedation | 320 (72.1%) |
| Deep sedation | 78 (17.6%) |
| Nurse Experience | |
| Novice | 56 (12.6%) |
| Competent | 113 (25.5%) |
| Expert | 274 (61.7%) |
| Endoscopist Experience | |
| Novice | 61 (13.74%) |
| Competent | 179 (40.32%) |
| Expert | 204 (45.95%) |
| Completed Exam | 444 (100%) |
| Disease Activity | |
| Remission | 140 (31.53%) |
| Mild | 104 (23.42%) |
| Moderate | 102 (22.97%) |
| Severe | 98 (22.07%) |
| Biological Therapy | |
| Yes | 289 (65.09%) |
| No | 155 (34.91%) |
| Medical Therapy | |
| Yes | 185 (41.67%) |
| No | 259 (58.33%) |
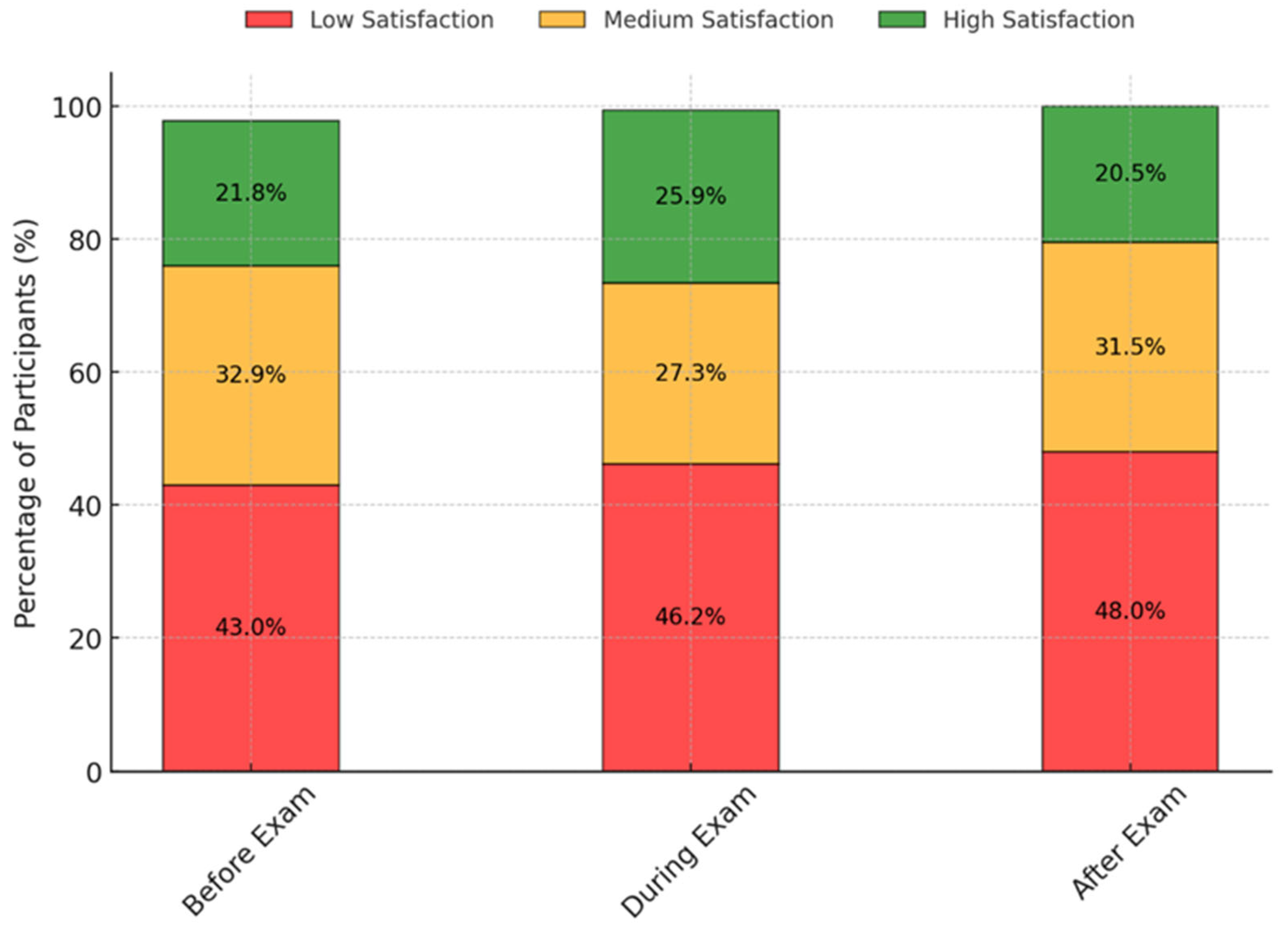
| ECSQ | |
| ECSQ Before [median, IQR] | 15 [11.00] |
| ECSQ Exam [median, IQR] | 11 [10.00] |
| ECSQ After [median, IQR] | 14 [8.25] |
| ECSQ Total [median, IQR] | 57.5 [67.50] |
| Preceived Stress | |
| PSS [median, IQR] | 38 [4.00] |
| Low stress [n, %] | 10 [2.25] |
| Medium stress | 54 [12.2] |
| High stress | 380 [85.6] |
| ECSQ Before Exam | ECSQ During Exam | ECSQ After Exam | ECSQ Total Score | PSS | |
|---|---|---|---|---|---|
| Median [IQR] | Median [IQR] | Median [IQR] | Median [IQR] | Median [IQR] | |
| Sex | |||||
| Man | 15 [11] | 11 [10] | 12 [8] | 72 [45] | 38 [4] |
| Women | 15.5 [11] | 10.5 [10] | 14 [10] | 69 [44.5] | 38 [4] |
| Sign. | 0.645 | 0.740 | 0.487 | 0.976 | 0.454 |
| Educational Level | |||||
| Did not complete school | 11 [5.5] | 5 [5.5] | 12 [4] | 90 [25] | 36 [6] |
| Middle school | 15 [10.75] | 9 [10] | 12 [9.5] | 86 [47] | 38 [4] |
| High school | 16 [11] | 12 [10] | 14 [10] | 71 [46] | 38 [4] |
| Bachelor’s degree | 15 [10] | 11 [9] | 13 [8] | 67 [42.5] | 38 [4] |
| Sign. | 0.584 | 0.826 | 0.927 | 0.590 | 0.130 |
| Smoke | |||||
| Yes | 15.5 [10] | 12 [9.75] | 14 [11] | 76 [42] | 38 [4] |
| No | 15 [11] | 10 [10] | 13.5 [8] | 69 [45.5] | 38 [4] |
| Sign. | 0.343 | 0.410 | 0.659 | 0.926 | 0.467 |
| First Colonscopy | |||||
| Yes | 12 [9] | 8 [8] | 11 [8.25] | 55 [43.5] | 38 [2.5] |
| No | 16 [11] | 12 [10] | 15 [9] | 75 [46] | 38 [4] |
| Sign. | 0.007 ** | 0.005 ** | 0.002 ** | 0.001 *** | 0.100 |
| Symptoms | |||||
| Yes | 16 [11.75] | 12 [10] | 15 [9] | 58 [42.5] | 38 [4] |
| No | 12 [8] | 8 [7.75] | 12 [7.75] | 72 [46] | 38 [4] |
| Sign. | 0.001 *** | 0.005 ** | 0.009 ** | 0.002 ** | 0.791 |
| Previous Pathologies | |||||
| Yes | 15.5 [11] | 12 [10] | 14 [9] | 69 [41.5] | 38 [4] |
| No | 15 [10] | 8 [9] | 12 [8] | 64 [42.5] | 38 [4] |
| Sign. | 0.236 | 0.033 * | 0.007 ** | 0.126 | 0.321 |
| Pathology | |||||
| Chron | 15 [10] | 9 [9] | 12 [9] | 75 [41] | 38 [4] |
| Colitis | 16 [11] | 12 [9] | 15 [9] | 65 [42.5] | 38 [4] |
| Sign. | 0.075 | 0.032 * | 0.002 ** | 0.030 * | 0.284 |
| Previous Surgeries | |||||
| Yes | 15 [11] | 9 [9] | 12 [8] | 75 [45] | 38 [4] |
| No | 16 [11] | 12 [9] | 14 [9.5] | 85 [40] | 38 [4] |
| Sign. | 0.296 | 0.035 | 0.642 | 0.149 | 0.027 * |
| Stoma | |||||
| Yes | 18.5 [10.25] | 12 [8] | 17.5 [9.25] | 69 [44.5] | 38 [2] |
| No | 15 [11] | 10.5 [10] | 13 [9] | 51 [43] | 38 [4] |
| Sign. | 0.403 | 0.097 | 0.122 | 0.264 | 0.038 * |
| Type of Preparation | |||||
| High volume | 12 [7] | 6.5 [6.25] | 11 [8] | 75 [46] | 38 [4] |
| Low volume | 16 [11] | 12 [10] | 14 [9] | 53 [51] | 38 [4] |
| Sign. | 0.001 *** | 0.000 *** | 0.004 ** | 0.011 * | 0.591 |
| Preparation Timing | |||||
| Day before | 15 [10] | 10 [9] | 13 [9] | 69 [46] | 38 [4] |
| Split | 16 [11.5] | 12 [10] | 14 [9] | 75 [42.5] | 38 [4] |
| Same day | 13 [10] | 9 [9] | 11 [7] | 73 [51.5] | 38 [0] |
| Sign. | 0.332 | 0.673 | 0.450 | 0.484 | 0.638 |
| Exam Completed | |||||
| Yes | 15 [11] | 10 [10] | 13 [9.5] | 64 [46] | 38 [4] |
| No | 17 [11] | 12 [8] | 15 [8] | 55 [42.75] | 38 [4] |
| Sign. | 0.738 | 0.111 | 0.510 | 0.873 | 0.028 * |
| Feeling of Cleanliness | |||||
| Low | 15 [12] | 12 [10] | 16 [7.25] | 73 [51.5] | 38 [2] |
| Medium | 16 [10.75] | 12 [8] | 15 [9] | 75 [27] | 38 [4] |
| High | 15 [10.75] | 9 [9] | 12 [10] | 69 [46] § | 38 [4] |
| Sign. | 0.601 | 0.089 | 0.108 | 0.04 * | 0.214 |
| Sedation | |||||
| No | 14 [10.75] | 11.5 [10] | 13.5 [7.75] | 75 [51.5] | 38 [4] |
| Conscious sedation | 16 [11] | 12 [10] | 14.5 [9] | 75 [48.5] | 38 [4] |
| Deep sedation | 13 [10] | 8 [9] | 12 [8] | 64 [38] § | 38 [4] |
| Sign. | 0.918 | 0.326 | 0.101 | 0.025 * | 0.187 |
| Seniority of Nurse | |||||
| Novice | 14 [11.25] | 9.5 [10] | 12.5 [9.5] | 66 [49.5] | 38 [4] |
| Competent | 15 [11] | 9 [9] | 12 [8] | 65 [40] | 38 [4] |
| Expert | 16 [11] | 12 [10] | 15 [9] | 75 [46] | 38 [4] |
| Sign. | 0.381 | 0.521 | 0.192 | 0.101 | 0.125 |
| Endoscopist Experience | |||||
| Novice | 12 [8] | 9 [8] § | 12 [10] | 65 [42.5] | 38 [4] § |
| Competent | 16 [11] | 10 [10] | 14 [9] | 72 [46] | 38 [4] |
| Expert | 16 [11.25] | 12 [10] | 14 [8] | 75 [46] | 38 [4] |
| Sign. | 0.056 | 0.024 * | 0.295 | 0.373 | 0.009 ** |
| Disease Activity | |||||
| Remission | 20 [8.25] | 14 [5.25] | 17 [8] | 90 [30] | 38 [4] |
| Mild | 19 [11.25] | 13 [10] | 16 [8] | 93 [33.25] | 38 [4] |
| Moderate | 13.5 [10] | 9 [8] | 12 [10] | 69 [45] | 38 [4] |
| Severe | 11 [3] | 6 [3] | 9 [4] | 44 [16.5] | 38 [2] |
| Sign. | 0.005 ** | 0.000 *** | 0.000 *** | 0.000 *** | 0.000 *** |
| Biological Therapy | |||||
| Yes | 15 [10] | 9 [9] | 12 [9] | 64 [45] | 38 [4] |
| No | 17 [11] | 12 [10] | 15 [9] | 77 [42.5] | 38 [4] |
| Sign. | 0.037 * | 0.159 | 0.060 | 0.007 ** | 0.470 |
| Medical Therapy | |||||
| Yes | 15 [11] | 10 [9] | 14 [8] | 72 [45] | 38 [4] |
| No | 16 [11] | 12 [10] | 14 [9.5] | 69 [46] | 38 [4] |
| Sign. | 0.686 | 0.368 | 0.765 | 0.823 | 0.325 |
| Age | BMI | Years Diagnosis | Exam Duration (min) | ECSQ Before | ECSQ During | ECSQ After | ECSQ Total | PSS | Test Performed Last 24 Months (n) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | NA | |||||||||
| BMI | 0.23 *** | NA | ||||||||
| Time from diagnosis (y) | 0.2 *** | −0.02 | NA | |||||||
| Exam duration (min) | 0.1 * | 0.02 | 0.07 | NA | ||||||
| ECSQ before exam | −0.02 | −0.04 | 0.1 * | −0.02 | NA | |||||
| ECSQ intra exam | −0.05 | −0.02 | 0.05 | −0.04 | 0.79 *** | NA | ||||
| ECSQ after exam | −0.01 | 0.01 | 0.02 | 0.02 | 0.70 *** | 0.78 *** | NA | |||
| ECSQ total | −0.02 | 0 | 0.09 | −0.01 | 0.84 *** | 0.81 *** | 0.82 *** | NA | ||
| PSS | 0.01 | −0.01 | 0 | −0.01 | −0.18 *** | −0.24 *** | −0.24 *** | −0.27 *** | NA | |
| Test performed last 24 months (n) | −0.07 | −0.04 | −0.11 * | −0.24 *** | −0.02 | −0.01 | −0.02 | −0.01 | −0.02 | NA |
| Predictors | Estimate | SE | t-Value | p-Value | Sign. |
|---|---|---|---|---|---|
| Intercept | 55.451 | 7.323 | 10.316 | 0.000 | *** |
| Middle school | −4.348 | 3.372 | −1.290 | 0.197 | |
| High school | −6.356 | 3.323 | −1.913 | 0.056 | . |
| Bachelor’s degree | −6.389 | 3.324 | −1.922 | 0.055 | . |
| Competent level endoscopist | 0.995 | 0.859 | 1.158 | 0.247 | |
| Expert level endoscopist | 2.111 | 0.843 | 2.504 | 0.012 | * |
| Mild disease activity | 1.705 | 0.735 | 2.318 | 0.020 | * |
| Moderate disease activity | −0.267 | 0.764 | −0.349 | 0.727 | |
| Severe disease activity | −3.872 | 0.862 | −4.492 | 0.000 | *** |
| Tests performed in the last 24 months (n) | 0.459 | 0.224 | 2.046 | 0.041 | * |
| Sedation | −4.203 | 2.917 | −1.441 | 0.150 | |
| Medical therapy | 3.053 | 3.118 | 0.979 | 0.328 | |
| Biological therapy | 4.641 | 3.355 | 1.383 | 0.167 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Napolitano, D.; Lo Cascio, A.; Bozzetti, M.; Povoli, A.; Grubissa, S.; Molino, L.; Marino, M.; Berretti, D.; Puca, P.; Lavigna, D.I.R.; et al. Patient Satisfaction with IBD Undergoing Colonoscopy: A Multicenter Cross-Sectional Study. J. Clin. Med. 2025, 14, 2562. https://doi.org/10.3390/jcm14082562
Napolitano D, Lo Cascio A, Bozzetti M, Povoli A, Grubissa S, Molino L, Marino M, Berretti D, Puca P, Lavigna DIR, et al. Patient Satisfaction with IBD Undergoing Colonoscopy: A Multicenter Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(8):2562. https://doi.org/10.3390/jcm14082562
Chicago/Turabian StyleNapolitano, Daniele, Alessio Lo Cascio, Mattia Bozzetti, Arianna Povoli, Simonetta Grubissa, Luca Molino, Marco Marino, Debora Berretti, Pierluigi Puca, Diletta Immacolata Rita Lavigna, and et al. 2025. "Patient Satisfaction with IBD Undergoing Colonoscopy: A Multicenter Cross-Sectional Study" Journal of Clinical Medicine 14, no. 8: 2562. https://doi.org/10.3390/jcm14082562
APA StyleNapolitano, D., Lo Cascio, A., Bozzetti, M., Povoli, A., Grubissa, S., Molino, L., Marino, M., Berretti, D., Puca, P., Lavigna, D. I. R., Grilli, F., Antonelli, G., Calvez, V., Di Petrillo, A., Onali, S., Gasbarrini, A., Fiorino, G., & Scaldaferri, F. (2025). Patient Satisfaction with IBD Undergoing Colonoscopy: A Multicenter Cross-Sectional Study. Journal of Clinical Medicine, 14(8), 2562. https://doi.org/10.3390/jcm14082562









