Systemic Lupus Erythematosus Features in Elderly Patients: Case-Based Review
Abstract
1. Introduction
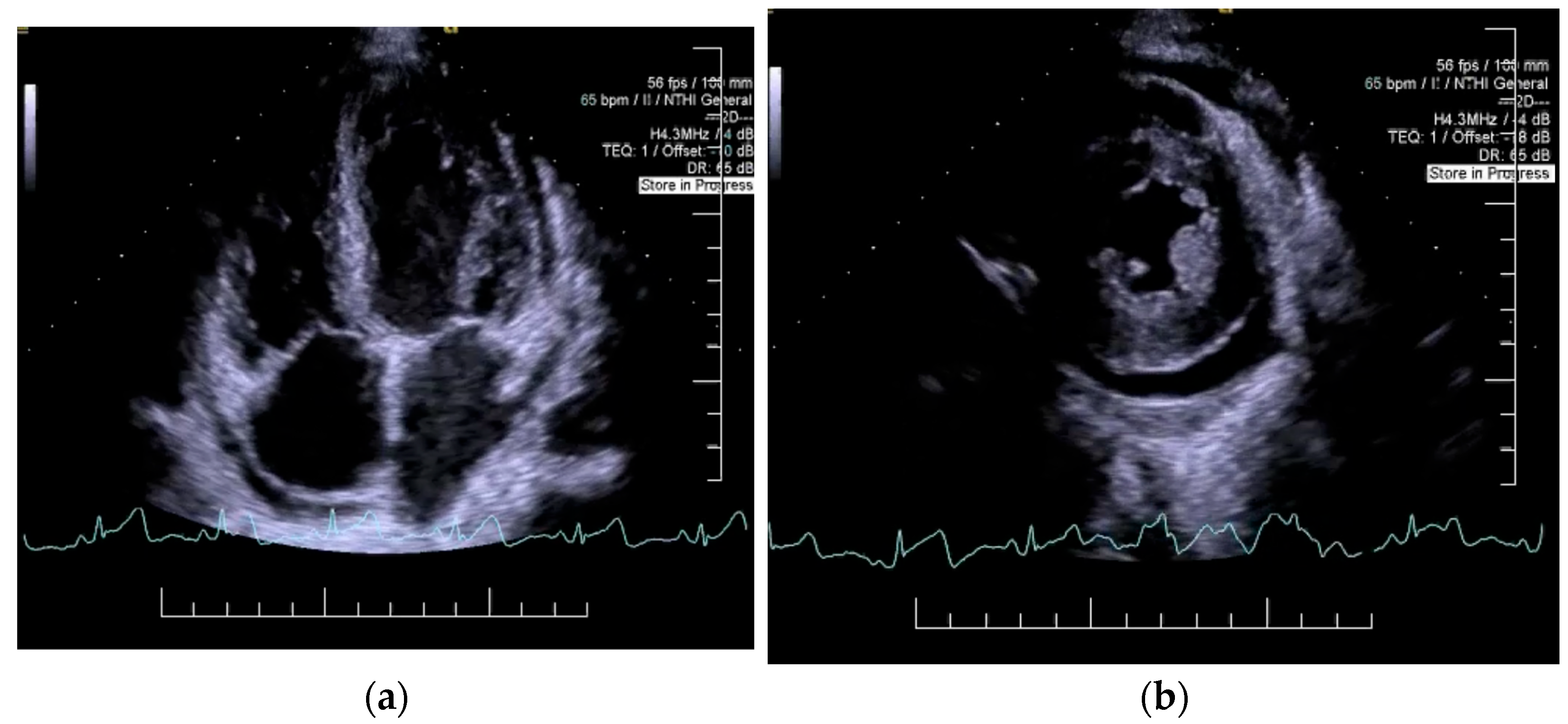
2. Case Presentation
3. Discussions
3.1. Epidemiology
3.2. Pathophysiology
3.2.1. Apoptosis and Toll-like Receptors (TLRs)
3.2.2. Innate Immune System
3.2.3. Adaptive Immune System
3.2.4. Complement System
3.2.5. Steroid Hormones
3.2.6. Physiopathology Particularities in Elderly Patients
3.3. Diagnosis
3.3.1. Diagnosis Criteria
3.3.2. Characteristics of SLE in the Elderly Patient
3.4. Management
3.5. Prognosis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Aringer, M.; Costenbader, K.; Daikh, D.; Brinks, R.; Mosca, M.; Ramsey-Goldman, R.; Smolen, J.S.; Wofsy, D.; Boumpas, D.T.; Kamen, D.L.; et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 1151–1159. [Google Scholar] [CrossRef]
- Arnaud, L.; Chasset, F.; Martin, T. Immunopathogenesis of systemic lupus erythematosus: An update. Autoimmun. Rev. 2024, 23, 103648. [Google Scholar] [CrossRef] [PubMed]
- So, C.; Imai, R.; Tomishima, Y.; Nishimura, N. Bilateral Pleuritis as the Initial Symptom of Systemic Lupus Erythematosus: A Case Series and Literature Review. Intern. Med. 2019, 58, 1617–1620. [Google Scholar] [CrossRef] [PubMed]
- Ikushima, H.; Mitsutake, A.; Hideyama, T.; Sato, T.; Katsumata, J.; Seki, T.; Maekawa, R.; Kishida, Y.; Shiio, Y. Severe pleuritis and pericarditis associated with very-late-onset systemic lupus erythematosus. J. Gen. Fam. Med. 2018, 19, 53–56. [Google Scholar] [CrossRef]
- Frutos, A.R.; Holgado, S.; Bergé, A.S.; Casas, I.; Olivé, A.; López-Longo, F.J.; Calvo-Alén, J.; Galindo, M.; Fernández-Nebro, A.; Pego-Reigosa, J.M.; et al. Late-onset versus early-onset systemic lupus: Characteristics and outcome in a national multicentre register (RELESSER). Rheumatology 2021, 60, 1793–1803. [Google Scholar] [CrossRef]
- Altier, J.; Oates, J.; Ward, C. Polymyalgia Rheumatica or Late Onset Lupus? A Case Report. J. Investig. Med. High Impact Case Rep. 2022, 10, 23247096221089493. [Google Scholar] [CrossRef]
- Hasegawa, T.; Nishikawa, K.; Ohjino, Y.; Sano, C.; Ohta, R. A Case of Late-Onset Systemic Lupus Erythematosus With Systemic Symptoms Leading to Multiple Organ Failure. Cureus 2023, 15, e46428. [Google Scholar] [CrossRef]
- Ameer, M.A.; Chaudhry, H.; Mushtaq, J.; Khan, O.S.; Babar, M.; Hashim, T.; Zeb, S.; Tariq, M.A.; Patlolla, S.R.; Ali, J.; et al. An Overview of Systemic Lupus Erythematosus (SLE) Pathogenesis, Classification, and Management. Cureus 2022, 14, e30330. [Google Scholar] [CrossRef]
- Fujita, Y.; Fukui, S.; Ishida, M.; Endo, Y.; Tsuji, S.; Takatani, A.; Igawa, T.; Shimizu, T.; Umeda, M.; Sumiyoshi, R.; et al. Reversible Cognitive Dysfunction in Elderly-onset Systemic Lupus Erythematosus, Successfully Treated with Aggressive Immunosuppressive Therapy. Intern. Med. 2018, 57, 3025–3028. [Google Scholar] [CrossRef]
- Hammami, S.; Chaabane, N.; Mahmoudi, H.; Bdioui, F.; Saffar, H. Late-onset systemic lupus erythematosus-associated primary biliary cirrhosis. Int. Arch. Med. 2013, 6, 3. [Google Scholar] [CrossRef]
- Viveiros, L.; Neves, A.; Gouveia, T.; Isenberg, D.A. A large cohort comparison of very late-onset systemic lupus erythematosus with younger-onset patients. Clin. Exp. Rheumatol. 2024, 42, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Celińska-Löwenhoff, M.; Musiał, J. Late-onset systemic lupus erythematosus: Clinical manifestations, course, and prognosis. Pol. Arch. Med. Wewn. 2015, 125, 497–499. [Google Scholar]
- Kim, E.J.; DeSimone, M.S.; Shi, C.R. Subacute cutaneous lupus erythematosus following osimertinib therapy for non-small cell lung cancer: A case report. JAAD Case Rep. 2024, 53, 30–33. [Google Scholar] [PubMed]
- Mrabet, S.; Boukadida, R.; Sidina, E.; Zellama, D.; Achour, A. Late-Onset Familial Systemic Lupus Erythematosus With Lupus Nephritis in an 82-Year-Old Male: A Case Report and Literature Review. Am. J. Mens. Health 2024, 18, 15579883241293781. [Google Scholar] [PubMed]
- Tsuji, N.; Inoguchi, N.; Sakai, T.; Furumuro, T.; Takaya, K. Unilateral Pleural Effusion as an Initial Manifestation of Systemic Lupus Erythematosus in a Patient of Advanced Age. Cureus 2024, 16, e63327. [Google Scholar] [CrossRef]
- Rodriguez-Perez, N. Systemic Lupus Erythematosus in a Nonagenarian Woman: A Case Report. Cureus 2024, 16, e69812. [Google Scholar]
- Kioi, Y.; Yorifuji, H.; Higami, Y.; Katada, Y. Serositis and lymphopenia are common features of systemic lupus erythematosus following SARS-CoV-2 infection: A case report and literature review. Int. J. Rheum. Dis. 2023, 26, 2267–2271. [Google Scholar]
- Chao, Y.H.; Chen, H.Y. Rare cause of ascites and pleural effusion: The first case report and literature review of pseudo-pseudo Meig’s syndrome in Taiwan. J. Formos. Med. Assoc. 2022, 121, 2633–2638. [Google Scholar]
- Helali, W.; El Euch, M.; Sassi, C.; Kefi, A.; Ben Hamida, F.; Ben Abdelghani, K.; Turki, S.; Abderrahim, E. Fulminant lupus pneumonitis complicating systemic lupus erythematosus in the elderly. Clin. Case Rep. 2023, 11, e6966. [Google Scholar]
- Xu, Z.-G.; Li, W.-L.; Wang, X.; Zhang, S.-Y.; Zhang, Y.-W.; Wei, X.; Li, C.-D.; Zeng, P.; Luan, S.-D. Systemic lupus erythematosus and antineutrophil cytoplasmic antibody-associated vasculitis overlap syndrome in a 77-year-old man: A case report. World J. Clin. Cases 2021, 9, 707–713. [Google Scholar]
- Kuroda, K.; Itagane, M.; Kinjo, M. Late-Onset Systemic Lupus Erythematosus Associated with Autoimmune Hemolytic Anemia and Sixth Cranial Nerve Palsy. Am. J. Case Rep. 2021, 22, e932959. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, A.; Cobilinschi, C.; Gradinaru, E.; Saulescu, I.; Ionescu, R. Features of Late-Onset Systemic Lupus Erythematosus. Rom. J. Rheumatol. 2021, 30, 121–124. [Google Scholar] [CrossRef]
- Bao, D.; Tan, Y.; Yu, X.; Wang, B.; Wang, H.; Xu, R.; Zhou, F.; Zhao, M. Case Report: A Rare Case of Lupus Nephritis Associated With Mantle Cell Lymphoma. Front. Med. 2021, 8, 759279. [Google Scholar]
- Tay, H.B.; Angkodjojo, S.; Tay, Z.E.A.; Tan, P.H.; Tan, Y.D. Angioimmunoblastic T-cell Lymphoma: A Mimic for Lupus. Eur. J. Case Rep. Intern. Med. 2020, 7, 001734. [Google Scholar]
- Rezazadegan, R.; Koushk-Jalali, B.; Kuntz, T.; Oellig, F.; Tigges, C.; Kreuter, A. Paraneoplastischer subakut kutaner Lupus erythematodes. Z. Rheumatol. 2021, 80, 189–193. [Google Scholar] [CrossRef]
- Bonometti, R.; Sacchi, M.C.; Stobbione, P.; Lauritano, E.C.; Tamiazzo, S.; Marchegiani, A.; Novara, E.; Molinaro, E.; Benedetti, I.; Massone, L.; et al. The first case of systemic lupus erythematosus (SLE) triggered by COVID-19 infection. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 9695–9697. [Google Scholar]
- de Montjoye, S.; Boland, B.; Van Raemdonck, J.; Houssiau, F.A. Very Late-Onset Systemic Lupus Erythematosus as Unusual Cause of Reversible Functional and Cognitive Impairments in an Octogenarian Patient. Eur. J. Case Rep. Intern. Med. 2020, 7, 001570. [Google Scholar]
- Kalenchic, T.I.; Didenko, N.S.; Kabak, S.L. Pulmonary Manifestations of Late-Onset Systemic Lupus Erythematosus: A Case Report. Revmatologiia 2019, 4, 63–66. [Google Scholar]
- D’Andréa, A.; Peillet, D.L.; Serratrice, C.; Petignat, P.A.; Prendki, V.; Reny, J.L.; Serratrice, J. Diagnosis of systemic lupus erythematosus by presence of Hargraves cells in eosinophilic pleural effusion: Case report. Medicine 2018, 97, e12871. [Google Scholar]
- Jatwani, S.; Handa, R.; Jatwani, K.; Chugh, K. Bronchiolitis obliterans organising pneumonia as an initial manifestation in a patient with systemic lupus erythematosus: A rare presentation. BMJ Case Rep. 2018, 2018, bcr2017224094. [Google Scholar] [CrossRef]
- Arai, H.; Hayashi, H.; Ogata, S.; Uto, K.; Saegusa, J.; Takahashi, K.; Koide, S.; Inaguma, D.; Hasegawa, M.; Yuzawa, Y. Progression of immunoglobulin G4-related disease to systematic lupus erythematosus after gastric cancer surgery: A case report. Medicine 2018, 97, e13545. [Google Scholar] [CrossRef] [PubMed]
- Shirai, H.; Shoda, H.; Kobayashi, S.; Fujio, K.; Setoguchi, K.; Yamamoto, K. Two cases of very elderly onset male lupus patient; the characteristics and sex differences of elderly onset systemic lupus erythematosus patients. Mod. Rheumatol. Case 2017, 1, 84–88. [Google Scholar] [CrossRef]
- Boddu, P.; Nadiri, M.; Malik, O. Diffuse Bullous Eruptions in an Elderly Woman: Late-Onset Bullous Systemic Lupus Erythematosus. Case Rep. Dermatol. 2016, 8, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, Y.; Toyoshima, M.; Akiyama, N.; Suda, T. Combined Pulmonary Fibrosis and Emphysema Preceding Lupus Pleuritis. Intern. Med. 2016, 55, 783–786. [Google Scholar] [CrossRef][Green Version]
- Hammami, S.; Bdioui, F.; Ouaz, A.; Loghmari, H.; Mahjoub, S.; Saffar, H. Successful treatment of massive ascites due to lupus peritonitis with hydroxychloroquine in old- onset lupus erythematosus. Pan Afr. Med. J. 2014, 18, 165. [Google Scholar] [CrossRef]
- Aguirre, H.D.; López, A.F.P.; Aponte Monsalve, J.E.; Estupiñan, M.F. Lupus eritematoso sistémico en el anciano: Una presentación atípica de una enfermedad común. Rev. Colomb. Reumatol. 2014, 21, 104–108. [Google Scholar] [CrossRef]
- Chebbi, W.; Berriche, O. Pulmonary fibrosis revealing systemic lupus erythematosus in an elderly subject. Pan Afr. Med. J. 2014, 18, 311. [Google Scholar]
- Iyoda, M.; Suzuki, H.; Ashikaga, E.; Nagai, H.; Kuroki, A.; Shibata, T.; Kitazawa, K.; Akizawa, T. Elderly onset systemic lupus erythematosus (SLE) presenting with disseminated intravascular coagulation (DIC). Clin. Rheumatol. 2008, 27, S15–S18. [Google Scholar] [CrossRef]
- Ito, H.; Nanamiya, W.; Kuroda, N.; Inoue, M.; Sasaoka, A.; Chijiwa, T.; Nishiya, K.; Hashimoto, K.; Nakagawa, O. Chronic lupus peritonitis with massive ascites at elderly onset: Case report and review of the literature. Intern. Med. 2002, 41, 1056–1061. [Google Scholar] [CrossRef][Green Version]
- Aharon, A.; Zandman-Goddard, G.; Shoenfeld, Y. Autoimmune Multiorgan Involvement in Elderly Men Is It SLE? Clin. Rheumatol. 1994, 13, 631–634. [Google Scholar] [CrossRef]
- Bolouri, N.; Akhtari, M.; Farhadi, E.; Mansouri, R.; Faezi, S.T.; Jamshidi, A.; Mahmoudi, M. Role of the innate and adaptive immune responses in the pathogenesis of systemic lupus erythematosus. Inflamm. Res. 2022, 71, 537–554. [Google Scholar] [CrossRef] [PubMed]
- Mathian, A.; Felten, R.; Alarcon-Riquelme, M.E.; Psarras, A.; Mertz, P.; Chasset, F.; Vital, E.M.; Arnaud, L. Type 1 interferons: A target for immune-mediated inflammatory diseases (IMIDs). Jt. Bone Spine 2024, 91, 105627. [Google Scholar] [CrossRef] [PubMed]
- Goyani, P.; Christodoulou, R.; Vassiliou, E. Immunosenescence: Aging and Immune System Decline. Vaccines 2024, 12, 1314. [Google Scholar] [CrossRef] [PubMed]
- Liphaus, B.L.; Kiss, M.H. The role of apoptosis proteins and complement components in the etiopathogenesis of systemic lupus erythematosus. Clinics 2010, 65, 327–333. [Google Scholar] [CrossRef]
- Tsokos, G.C.; Lo, M.S.; Costa Reis, P.; Sullivan, K.E. New insights into the immunopathogenesis of systemic lupus erythematosus. Nat. Rev. Rheumatol. 2016, 12, 716–730. [Google Scholar] [CrossRef]
- Lorenz, G.; Lech, M.; Anders, H.J. Toll-like receptor activation in the pathogenesis of lupus nephritis. Clin. Immunol. 2017, 185, 86–94. [Google Scholar] [CrossRef]
- Murayama, G.; Chiba, A.; Kuga, T.; Makiyama, A.; Yamaji, K.; Tamura, N.; Miyake, S. Inhibition of mTOR suppresses IFNα production and the STING pathway in monocytes from systemic lupus erythematosus patients. Rheumatology 2020, 59, 2992–3002. [Google Scholar] [CrossRef]
- Kato, Y.; Park, J.; Takamatsu, H.; Konaka, H.; Aoki, W.; Aburaya, S.; Ueda, M.; Nishide, M.; Koyama, S.; Hayama, Y.; et al. Apoptosis-derived membrane vesicles drive the cGAS-STING pathway and enhance type I IFN production in systemic lupus erythematosus. Ann. Rheum. Dis. 2018, 77, 1507–1515. [Google Scholar] [CrossRef]
- de Bont, C.M.; Boelens, W.C.; Pruijn, G.J.M. NETosis, complement, and coagulation: A triangular relationship. Cell Mol. Immunol. 2019, 16, 19–27. [Google Scholar] [CrossRef]
- Tseng, C.W.; Liu, G.Y. Expanding roles of neutrophils in aging hosts. Curr. Opin. Immunol. 2014, 29, 43–48. [Google Scholar] [CrossRef]
- Ray, D.; Yung, R. Immune Senescence, Epigenetics and Autoimmunity. Clin. Immunol. 2018, 196, 59–63. [Google Scholar]
- Lood, C.; Blanco, L.P.; Purmalek, M.M.; Carmona-Rivera, C.; De Ravin, S.S.; Smith, C.K.; Malech, H.L.; A Ledbetter, J.; Elkon, K.B.; Kaplan, M.J. Neutrophil extracellular traps enriched in oxidized mitochondrial DNA are interferogenic and contribute to lupus-like disease. Nat. Med. 2016, 22, 146–153. [Google Scholar] [CrossRef]
- Wang, T.; Mei, Y.; Li, Z. Research Progress on Regulatory B Cells in Systemic Lupus Erythematosus. BioMed Res. Int. 2019, 2019, 7948687. [Google Scholar]
- Hudspeth, K.L.; Shu, W.; Wang, J.; Rahman, S.; A Smith, M.; Casey, K.A.; Stephens, G.L.; A Sanjuan, M.; Team, A.M.; A Hasni, S.; et al. NK Cell Phenotype and Proliferation in Systemic Lupus Erythematosus. J. Immunol. 2016, 196, 194.5. [Google Scholar]
- Dossybayeva, K.; Abdukhakimova, D.; Poddighe, D. Basophils and Systemic Lupus Erythematosus in Murine Models and Human Patients. Biology 2020, 9, 308. [Google Scholar] [CrossRef]
- Soni, C.; Reizis, B. Self-DNA at the Epicenter of SLE: Immunogenic Forms, Regulation, and Effects. Front. Immunol. 2019, 10, 1601. [Google Scholar] [CrossRef]
- Men, K.; Chen, Y.; Zhang, J.; Wei, D. The evaluation of cellular immune function in elderly patients with systemic lupus erythematosus. Korean J. Intern. Med. 2019, 34, 932–937. [Google Scholar]
- Suárez-Fueyo, A.; Bradley, S.J.; Tsokos, G.C. T Cells in Systemic Lupus Erythematosus. Curr. Opin. Immunol. 2016, 43, 32–38. [Google Scholar]
- Wu, M.; Yang, J.; Li, X.; Chen, J. The Role of γδ T Cells in Systemic Lupus Erythematosus. J. Immunol. Res. 2016, 2016, 2932531. [Google Scholar] [CrossRef]
- Lu, Y.; Ruan, Y.; Hong, P.; Rui, K.; Liu, Q.; Wang, S.; Cui, D. T-cell senescence: A crucial player in autoimmune diseases. Clin. Immunol. 2023, 248, 109202. [Google Scholar]
- Hristova, M.H.; Stoyanova, V.S. Autoantibodies against Complement Components in Systemic Lupus Erythematosus—Role in the Pathogenesis and Clinical Manifestations. Lupus 2017, 26, 1550–1555. [Google Scholar]
- Pickering, M.C.; Botto, M. Are anti-C1q antibodies different from other SLE autoantibodies? Nat. Rev. Rheumatol. 2010, 6, 490–493. [Google Scholar]
- Leffler, J.; Bengtsson, A.A.; Blom, A.M. The complement system in systemic lupus erythematosus: An update. Ann. Rheum. Dis. 2014, 73, 1601–1606. [Google Scholar]
- Ramsey-Goldman, R.; Li, J.; Dervieux, T.; Alexander, R.V. Cell-bound complement activation products in SLE. Lupus Sci. Med. 2017, 4, e000236. [Google Scholar]
- Baschant, U.; Tuckermann, J. The role of the glucocorticoid receptor in inflammation and immunity. J. Steroid Biochem. Mol. Biol. 2010, 120, 69–75. [Google Scholar] [CrossRef]
- Zen, M.; Canova, M.; Campana, C.; Bettio, S.; Nalotto, L.; Rampudda, M.; Ramonda, R.; Iaccarino, L.; Doria, A. The kaleidoscope of glucorticoid effects on immune system. Autoimmun. Rev. 2011, 10, 305–310. [Google Scholar]
- Ferreira, N.S.; Tostes, R.C.; Paradis, P.; Schiffrin, E.L. Aldosterone, Inflammation, Immune System, and Hypertension. Am. J. Hypertens. 2021, 34, 15–27. [Google Scholar] [CrossRef]
- Bereshchenko, O.; Bruscoli, S.; Riccardi, C. Glucocorticoids, Sex Hormones, and Immunity. Front. Immunol. 2018, 9, 1332. [Google Scholar]
- Pan, Q.; Chen, X.; Liao, S.; Chen, X.; Zhao, C.; Xu, Y.-Z.; Liu, H.-F. Updated advances of linking psychosocial factors and sex hormones with systemic lupus erythematosus susceptibility and development. PeerJ 2019, 7, e7179. [Google Scholar]
- Alberro, A.; Iribarren-Lopez, A.; Sáenz-Cuesta, M.; Matheu, A.; Vergara, I.; Otaegui, D. Inflammaging markers characteristic of advanced age show similar levels with frailty and dependency. Sci. Rep. 2021, 11, 4358. [Google Scholar]
- Cisneros, B.; García-Aguirre, I.; Unzueta, J.; Arrieta-Cruz, I.; González-Morales, O.; Domínguez-Larrieta, J.M.; Tamez-González, A.; Leyva-Gómez, G.; Magaña, J.J. Immune system modulation in aging: Molecular mechanisms and therapeutic targets. Front. Immunol. 2022, 13, 1059173. [Google Scholar] [CrossRef]
- Montoya-Ortiz, G. Immunosenescence, Aging, and Systemic Lupus Erythematous. Autoimmune Dis. 2013, 2013, 267078. [Google Scholar] [CrossRef]
- Gibson, K.L.; Wu, Y.; Barnett, Y.; Duggan, O.; Vaughan, R.; Kondeatis, E.; Nilsson, B.; Wikby, A.; Kipling, D.; Dunn-Walters, D.K. B-cell diversity decreases in old age and is correlated with poor health status. Aging Cell 2009, 8, 18–25. [Google Scholar] [CrossRef]
- Buffa, S.; Bulati, M.; Pellicanò, M.; Dunn-Walters, D.K.; Wu, Y.-C.; Candore, G.; Vitello, S.; Caruso, C.; Colonna-Romano, G. B cell immunosenescence: Different features of naive and memory B cells in elderly. Biogerontology 2011, 12, 473–483. [Google Scholar] [CrossRef]
- Uhl, B.; Vadlau, Y.; Zuchtriegel, G.; Nekolla, K.; Sharaf, K.; Gaertner, F.; Massberg, S.; Krombach, F.; Reichel, C.A. Aged neutrophils contribute to the first line of defense in the acute inflammatory response. Blood 2016, 128, 2327–2337. [Google Scholar] [CrossRef]
- Gullotta, G.S.; De Feo, D.; Friebel, E.; Semerano, A.; Scotti, G.M.; Bergamaschi, A.; Butti, E.; Brambilla, E.; Genchi, A.; Capotondo, A.; et al. Age-induced alterations of granulopoiesis generate atypical neutrophils that aggravate stroke pathology. Nat. Immunol. 2023, 24, 925–940. [Google Scholar] [CrossRef]
- Gubbels Bupp, M.R.; Potluri, T.; Fink, A.L.; Klein, S.L. The Confluence of Sex Hormones and Aging on Immunity. Front. Immunol. 2018, 9, 1269. [Google Scholar] [CrossRef]
- Costenbader, K.H.; Gay, S.; Alarcón-Riquelme, M.E.; Iaccarino, L.; Doria, A. Genes, epigenetic regulation and environmental factors: Which is the most relevant in developing autoimmune diseases? Autoimmun. Rev. 2012, 11, 604–609. [Google Scholar] [CrossRef]
- Cutolo, M.; Sulli, A.; Capellino, S.; Villaggio, B.; Montagna, P.; Seriolo, B.; Straub, R.H. Sex hormones influence on the immune system: Basic and clinical aspects in autoimmunity. Lupus 2004, 13, 635–638. [Google Scholar] [CrossRef]
- Fairweather, D.; Beetler, D.J.; McCabe, E.J.; Lieberman, S.M. Mechanisms underlying sex differences in autoimmunity. J. Clin. Investig. 2024, 134, e180076. [Google Scholar] [CrossRef]
- Richardson, B. Reprint of The Interaction between Environmental Triggers and Epigenetics in Autoimmunity. Clin. Immunol 2018, 196, 72–76. [Google Scholar] [CrossRef]
- Merrheim, J.; Villegas, J.; Van Wassenhove, J.; Khansa, R.; Berrih-Aknin, S.; le Panse, R.; Dragin, N. Estrogen, estrogen-like molecules and autoimmune diseases. Autoimmun. Rev. 2020, 19, 102468. [Google Scholar] [CrossRef]
- Schilirò, D.; Silvagni, E.; Ciribè, B.; Fattorini, F.; Maccarrone, V.; Elefante, E.; Signorini, V.; Zucchi, D.; Cardelli, C.; Bortoluzzi, A.; et al. Systemic Lupus Erythematosus: One Year in Review 2024. Clin. Exp. Rheumatol. 2024, 42, 583–592. [Google Scholar]
- Fanouriakis, A.; Tziolos, N.; Bertsias, G.; Boumpas, D.T. Update on the Diagnosis and Management of Systemic Lupus Erythematosus. Ann. Rheum. Dis. 2020, 80, 14–25. [Google Scholar]
- Suda, M.; Kishimoto, M.; Ohde, S.; Okada, M. Validation of the 2019 ACR/EULAR classification criteria of systemic lupus erythematosus in 100 Japanese patients: A real-world setting analysis. Clin. Rheumatol. 2020, 39, 1823–1827. [Google Scholar] [CrossRef]
- Piga, M.; Tselios, K.; Viveiros, L.; Chessa, E.; Neves, A.; Urowitz, M.B.; Isenberg, D. Clinical patterns of disease: From early systemic lupus erythematosus to late-onset disease. Best Pract. Res. Clin. Rheumatol. 2023, 37, 101938. [Google Scholar] [CrossRef]
- Rovenský, J.; Tuchyňová, A. Systemic lupus erythematosus in the elderly. Autoimmun. Rev. 2008, 7, 235–239. [Google Scholar]
- Fanouriakis, A.; Kostopoulou, M.; Andersen, J.; Aringer, M.; Arnaud, L.; Bae, S.-C.; Boletis, J.; Bruce, I.N.; Cervera, R.; Doria, A.; et al. EULAR recommendations for the management of systemic lupus erythematosus: 2023 update. Ann. Rheum. Dis. 2024, 83, 15–29. [Google Scholar]
- Xu, Y.X.; Tan, Y.; Yu, F.; Zhao, M.H. Late onset lupus nephritis in Chinese patients: Classified by the 2003 International Society of Nephrology and Renal Pathology Society system. Lupus 2011, 20, 801–808. [Google Scholar]
- Kutky, M.; Aloudat, S. Late-Onset Systemic Lupus Erythematosus with Lupus Nephritis in a 74-Year-Old Male: A Brief Case and Review. Can. J. Kidney Health Dis. 2018, 5, 2054358118793397. [Google Scholar] [CrossRef]
- Aljohani, R.; Gladman, D.D.; Su, J.; Urowitz, M.B. Disease evolution in late-onset and early-onset systemic lupus erythematosus. Lupus 2017, 26, 1190–1196. [Google Scholar] [PubMed]
- Wilhelmus, S.; Bajema, I.M.; Bertsias, G.K.; Boumpas, D.T.; Gordon, C.; Lightstone, L.; Tesar, V.; Jayne, D.R. Lupus nephritis management guidelines compared. Nephrol. Dial. Transplant. 2016, 31, 904–913. [Google Scholar] [PubMed]
- Catoggio, L.J.; Soriano, E.R.; Imamura, P.M.; Wojdyla, D.; Jacobelli, S.; Massardo, L.; Díaz, R.C.; Guibert-Toledano, M.; Alvarellos, A.; Saurit, V.; et al. Late-onset systemic lupus erythematosus in Latin Americans: A distinct subgroup? Lupus 2015, 24, 788–795. [Google Scholar]
- Ahn, S.S.; Yoo, J.; Jung, S.M.; Song, J.J.; Park, Y.B.; Lee, S.W. Comparison of clinical features and outcomes between patients with early and delayed lupus nephritis. BMC Nephrol. 2020, 21, 258. [Google Scholar] [CrossRef]
- Delfino, J.; Dos Santos, T.A.F.G.; Skare, T.L. Comparison of lupus patients with early and late onset nephritis: A study in 71 patients from a single referral center. Adv. Rheumatol. 2020, 60, 5. [Google Scholar]
- Zucchi, D.; Cardelli, C.; Elefante, E.; Tani, C.; Mosca, M. Treat-to-Target in Systemic Lupus Erythematosus: Reality or Pipe Dream. J. Clin. Med. 2023, 12, 3348. [Google Scholar] [CrossRef]
- Tomic-Lucic, A.; Petrovic, R.; Radak-Perovic, M.; Milovanovic, D.; Milovanovic, J.; Zivanovic, S.; Pantovic, S.; Veselinovic, M. Late-onset systemic lupus erythematosus: Clinical features, course, and prognosis. Clin. Rheumatol. 2013, 32, 1053–1058. [Google Scholar]



| Author, Year Number of Cases [Reference] | Age, Gender | Clinical Manifestation | Laboratory Test Abnormalities | Observations |
|---|---|---|---|---|
| So et al., 2019 3 cases [3] | 75 y/o ♂ | bilateral pleural effusion | positive tests for anti-dsDNA Ab hypocomplementemia pancytopenia, hematuria | In elderly patients with cardiovascular history, bilateral pleural effusion can mimic congestive heart failure. Thoracocentesis is essential for evaluating diuretic-resistant bilateral pleural effusion in elderly patients. |
| 80 y/o ♀ | bilateral pleural effusion | positive tests for ANA hypocomplementemia leukopenia, proteinuria | ||
| 83 y/o ♂ | bilateral pleural effusion | positive tests for ANA, anti-dsDNA Ab, elevated CRP levels | ||
| Ikushima et al., 2018 1 case [4] | 85 y/o ♀ | fatigue, bilateral lower extremity edema, arthritis, pleural effusion, pericardial effusion | positive tests for ANA, anti-dsDNA Ab hypocomplementemia anemia, elevated ESR and CRP levels, elevated D-dimers levels | This report describes a case of very-late-onset SLE with serositis as the predominant clinical feature, highlighting the need to consider SLE in the differential diagnosis of rapidly accumulating pleural effusion in elderly patients. |
| Hasegawa et al., 2023 1 case [7] | 87 y/o ♂ | anorexia, decreased food intake, bilateral pleural effusion, ascites, painful aphthous ulcers | positive tests for ANA hypocomplementemia leukopenia, thrombocytopenia, proteinuria | Diagnosing late-onset SLE in the elderly is challenging due to the prevalence of comorbidities and the need to distinguish it from other conditions. In some cases, conditions like pneumonia or heart failure may not fully explain the symptoms, leading to the eventual diagnosis of late-onset SLE through thorough testing and examinations. |
| Fujita et al., 2018 1 case [9] | 70 y/o ♀ | gait disturbance, cognitive dysfunction, muscle rigidity, bilateral pleural effusion, bilateral lower extremity edema | positive tests for ANA, anti-dsDNA Ab, anti-La/SS-B Ab hypocomplementemia lymphocytopenia, anemia, thrombocytopenia, elevated ESR and ferritin levels | Differentiating causes of cognitive impairment in elderly patients is challenging, with neurodegenerative diseases like Alzheimer’s being common considerations. Neuropsychiatric SLE should also be included in the differential diagnosis. Prompt and appropriate immunosuppressive therapy can potentially reverse cognitive dysfunction. |
| Kim et al., 2024 1 case [13] | 81 y/o ♀ | photosensitive lesions in sun-exposed sites | positive tests for ANA, anti-Ro/SS-A Ab | This case illustrates the development of SCLE after starting osimertinib for non-small-cell lung cancer. Prompt recognition and management of cutaneous side effects are crucial to maintaining targeted cancer therapy. |
| Mrabet et al., 2024 1 case [14] | 82 y/o ♂ | fatigue, dyspnea, abdominal pain, hepatosplenomegaly, pericardial effusion | positive tests for ANA, anti-nucleosome Ab, anti-histone Ab hypocomplementemia anemia, acute kidney injury, proteinuria, hematuria, hepatic cholestasis | Late-onset SLE often presents insidiously with atypical features, leading to delayed diagnosis, as seen in this case, who had abdominal pain and dyspnea without typical skin or joint signs. Moreover, this case demonstrates that familial late-onset SLE can occur in elderly men, presenting with a relatively mild form that does not necessitate intensive immunosuppressive therapy. |
| Tsuji et al., 2024 1 case [15] | 75 y/o ♂ | pleural effusion, pericardial effusion, gait ataxia, hand dexterity impairments, arthralgias | positive tests for ANA, anti-Ro/SS-A Ab, RF lymphocytopenia, anemia, elevated CRP levels | This case emphasizes that late-onset SLE can present with diverse symptoms, including unilateral pleural effusion and neurological issues, and should be considered when the cause of pleural effusion is unclear. |
| Rodriguez- Perez, 2024 1 case [16] | 90 y/o ♀ | recurrent unilateral pleural effusion, pericardial effusion, arthralgias, bilateral lower extremity edema | positive tests for ANA, p-ANCA anemia, marked proteinuria | This case emphasizes the significance of recognizing autoimmune conditions such as SLE in elderly patients over 90 y/o, with the presentation of marked proteinuria representing a rare and atypical manifestation. |
| Kioi et al., 2023 1 case [17] | 86 y/o ♂ | persistent unilateral pleural effusion | positive tests for ANA, anti-dsDNA Ab, anti-cardiolipin immunoglobulin G Ab, anti-U1-RNP Ab, anti-La/SS-B Ab, anti-CCP Ab lymphocytopenia, elevated CRP levels | The growing number of long COVID cases raises concerns about undiagnosed autoimmune conditions, such as lupus. In patients with persistent pleural effusion or lymphocytopenia post-COVID-19, testing for SLE-specific autoantibodies, including anti-dsDNA and anti-Sm Ab, should be considered. |
| Chao et al., 2022 1 case [18] | 82 y/o ♀ | ascites, pleural effusion, spontaneous oral bleeding, multiple ecchymoses | positive tests for ANA, anti-Sm Ab hypocomplementemia normocytic anemia, thrombocytopenia, renal dysfunction, proteinuria, elevated CA-125 levels | Pseudo-pseudo Meigs’ syndrome should be considered as a key differential diagnosis in female patients presenting with ascites, pleural effusion, and elevated CA-125 levels. The initial evaluation should focus on ruling out pelvic tumors associated with Meigs’ or pseudo-Meigs’ syndrome. An SLE flare should be considered, even in elderly patients. |
| Helali et al., 2022 1 case [19] | 75 y/o ♂ | weakness, dyspnea, respiratory failure | positive tests for ANA, anti-dsDNA Ab anemia, thrombocytopenia, proteinuria | Non-infectious fulminant lupus pneumonitis is a rare, severe syndrome with high mortality, with only a few cases reported in the literature, particularly in young patients. It is often challenging to diagnose, especially as an initial SLE manifestation. |
| Xu et al., 2021 1 case [20] | 77 y/o ♂ | unilateral pleural effusion, shortness of breath over the past 3 years | positive tests for ANA, anti-dsDNA Ab, MPO-ANCA anemia, renal dysfunction, proteinuria, microscopic hematuria | The overlap syndrome of SLE and antineutrophil cytoplasmic antibody-associated vasculitis is a rare condition. It is marked by the presence of serological markers and severe clinical features, such as rapidly progressive glomerulonephritis and pulmonary involvement, meeting the diagnostic criteria for both diseases. This syndrome predominantly affects women of childbearing age. |
| Kuroda et al., 2021 1 case [21] | 78 y/o ♀ | fatigue, diplopia, left sixth cranial nerve palsy, polyarthritis | positive tests for ANA, anti-dsDNA Ab, lupus anticoagulant hypocomplementemia leukopenia, anemia, elevated erythrocyte sedimentation rate (ESR) levels | This case highlights a challenging diagnostic scenario involving an elderly woman with autoimmune hemolytic anemia and isolated sixth cranial nerve palsy. The advanced age, low ANA titers, and atypical presentation made the diagnosis of SLE particularly complex. |
| Constantinescu et al., 2021 2 cases [22] | 81 y/o ♀ | vesperal fever, weight loss, arthralgias, myalgias, unilateral pleural effusion, pericardial fluid, atrophic erythematous squamous plaques | positive tests for ANA, anti-dsDNA Ab, anti-Ro/SS-A Ab leukopenia with lymphocytopenia, normocytic anemia | Skin lesions are less commonly reported in late-onset lupus, with malar rash being particularly rare in this group. However, the two cases discussed showed chronic and subacute cutaneous lupus lesions, later confirmed by skin biopsy. |
| 72 y/o ♀ | weight loss, recurring fever, arthralgias, rounded erythematous squamous plaques | positive tests for ANA, anti-dsDNA Ab, RF leukopenia with lymphocytopenia, anemia | ||
| Bao et al., 2021 1 case [23] | 84 y/o ♂ | bilateral peripheral edema | positive tests for ANA, anti-dsDNA Ab hypocomplementemia renal dysfunction, hypoalbuminemia, proteinuria, microscopic hematuria, pyuria | This case highlights a rare presentation of lupus nephritis as a paraneoplastic manifestation of mantle cell lymphoma. The rapid remission of renal and immune symptoms following chemotherapy supports the secondary nature of the lupus nephritis. |
| Tay et al., 2020 1 case [24] | 71 y/o ♀ | fever, alopecia, hepatomegaly, multiple intra-abdominal and intra-thoracic lymphadenopathies | positive tests for ANA, anti-dsDNA Ab leukopenia, anemia, renal dysfunction, microscopic hematuria, proteinuria | This case highlights the established connection between rheumatological disorders and cancers, as evidenced by unusual clinical features such as pronounced hepatomegaly and extensive lymphadenopathy, suggesting the presence of an underlying malignancy. Angioimmunoblastic T-cell lymphoma is a rare subtype of non-Hodgkin lymphoma. Its diagnosis is challenging due to subtle histological features. |
| Rezazadegan et al., 2020 1 case [25] | 78 y/o ♀ | papulosquamous itching skin lesions, weight loss, heartburn, arthralgias, myalgias | positive tests for ANA, anti-Ro/SS-A Ab hypocomplementemia anemia, biopsy of gastric mass showing gastric adenocarcinoma | Rheumatic diseases, like dermato-myositis, have been well established as paraneoplastic syndromes. More recently, growing evidence has linked SCLE to various malignancies, primarily solid tumors. These cancers may arise before, simultaneously with, or after the onset of SCLE. |
| Bonemetti et al., 2020 1 case [26] | 85 y/o ♀ | hemodynamic instability, diffuse dyscrasia edemas, peripheral cyanosis, particularly on her fingers, pleural effusion | positive tests for ANA, anti-Ku Ab, ANCA leukocytosis with lymphocytopenia, thrombocytopenia, renal dysfunction, elevated CRP and ferritin levels | This is the first documented case in the literature of SLE with vasculitis triggered by COVID-19 infection. |
| de Montjoye et al., 2020 1 case [27] | 81 y/o ♀ | impaired spatial and time orientation, dyspnea, weight loss, fever, arthritis, facial rash | positive tests for ANA, anti-dsDNA Ab, anti-Ro/SS-A Ab anemia, hypoalbuminemia, proteinuria, elevated CRP levels | Late-onset SLE is an uncommon but significant cause of reversible functional and cognitive decline in elderly patients. Its presentation in this age group is often atypical, making the diagnosis challenging. |
| Kalenchic et al., 2019 1 case [28] | 75 y/o ♀ | dyspnea, low-grade fever, arthritis, pericardial effusion, pleural effusion | positive tests for ANA, anti-dsDNA Ab, anti-nucleosome Ab lymphocytopenia, anemia, elevated ESR and CRP levels | This case illustrates that late-onset SLE can be a potential cause of pleural fluid accumulation in elderly patients. |
| D’Andréa et al., 2018 1 case [29] | 82 y/o ♀ | anorexia, weight loss, fatigue, arthralgia, unilateral pleural effusion | positive tests for ANA, anti-nucleosome Ab leukopenia with eosinophilia, anemia, elevated CRP levels, pleural effusion cytological examination showing Hargraves cells | In elderly patients, eosinophilic pleural effusion is most often linked to malignancies and infections. In rare instances, pleural eosinophilia may be associated with connective tissue diseases. When accompanied by chronic joint pain and hematologic abnormalities, SLE should be considered in the differential diagnosis. |
| Jatwani et al., 2018 1 case [30] | 81 y/o ♂ | shortness of breath, pericardial effusion, bilateral pleural effusion, bilateral lower extremity edema | positive tests for ANA, anti-dsDNA Ab, anti-beta-2 glycoprotein IgA, anti-CCP hypocomplementemia anemia, thrombocytopenia | Bronchiolitis obliterans organizing pneumonia (BOOP) is a rare manifestation of connective tissue disorders like SLE. In this case, BOOP was diagnosed 8 years before SLE. The high relapse rate, despite adequate steroid therapy, suggests a causal link to underlying SLE and indicates BOOP as the initial presentation. |
| Arai et al., 2018 1 case [31] | 74 y/o ♂ | fever, dyspnea, pericardial effusion, pleural effusion, arthritis | positive tests for ANA, anti-dsDNA Ab hypergammaglobulinemia, hypocomplementemia renal dysfunction | This report highlights a unique case of comorbid autoimmune diseases, featuring the coexistence of IgG4-related disease (IgG4-RD) and SLE. The clinical course demonstrated a transition from ANA-positive IgG4-RD to SLE after the surgical removal of gastric cancer. |
| Shirai et al., 2017 2 cases [32] | 82 y/o ♂ | bilateral polyarthritis | positive tests for ANA, anti-dsDNA Ab lymphocytopenia, mild thrombocytopenia, renal dysfunction, proteinuria | These two cases demonstrated that very-late-onset male SLE can present with atypical features, such as the absence of characteristic skin lesions, severe cytopenia, hypocomplementemia, anti-SS-A, anti-RNP, or anti-Sm antibodies, which complicate the diagnosis of SLE. |
| 83 y/o ♂ | fatigue, dyspnea, bilateral pleural effusion, bilateral lower extremity edema | positive tests for ANA, anti-dsDNA Ab lymphocytopenia, hypoalbuminemia, elevated ESR and CRP levels | ||
| Boddu et al., 2016 1 case [33] | 73 y/o ♀ | painful blistering skin rash, oral ulcers | positive tests for ANA, anti-RNP Ab, anti-Sm Ab hypocomplementemia anemia, thrombocytopenia, hypoalbuminemia, proteinuria | This case highlights the challenges physicians face in diagnosing among the numerous immunobullous dermatoses. Bullous SLE must be especially distinguished from pemphigoid and epidermolysis bullosa acquisita. |
| Kamiya et al., 2016 1 case [34] | 83 y/o ♀ | bilateral pleural effusion | positive tests for ANA, anti-dsDNA Ab, anti-RNP Ab hypocomplementemia proteinuria, elevated CRP levels, elevated CA-125 levels | Some studies have suggested a potential link between anti-RNP antibodies and lupus serositis. These findings indicate that lupus serositis should be considered in patients with anti-RNP-positive interstitial pneumonia. |
| Hammami et al., 2014 1 case [35] | 77 y/o ♀ | massive ascites, unilateral exudative pleuritis 4 years prior to presentation | positive tests for ANA, anti-dsDNA Ab, anti-Sm Ab hypocomplementemia leukopenia with lymphocytopenia, anemia, hypoalbuminemia | Massive ascites is a rare presentation of SLE. Lupus peritonitis may mimic acute abdominal conditions or present chronically as persistent painless ascites, chronic pancreatitis, or mild abdominal pain. |
| Agguire et al., 2014 1 case [36] | 72 y/o ♂ | right-sided chest pain, dyspnea, erythematous lesions on the sun-exposed areas, oral ulcers, bilateral lower and upper extremity edema, massive unilateral pleural effusion | positive tests for ANA, anti-dsDNA Ab, anti-RNP Ab hypocomplementemia leukopenia with lymphocytopenia, elevated CRP levels | Diagnosing late-onset SLE in elderly patients is challenging due to its nonspecific presentation and broad differential diagnoses. While elderly-onset SLE typically shows lower rates of anti-dsDNA, anti-RNP Ab, and hypocomplementemia, this case demonstrated elevated levels of these markers alongside complement consumption. |
| Chebbi et al., 2014 1 case [37] | 82 y/o ♀ | anorexia, weight loss, fatigue, arthralgia, unilateral pleural effusion | positive tests for ANA, anti-nucleosome Ab leukopenia with eosinophilia, anemia, elevated CRP levels, pleural effusion cytological examination showing Hargraves cells | In elderly patients, eosinophilic pleural effusion is most often linked to malignancies and infections. In rare instances, pleural eosinophilia may be associated with connective tissue diseases. When accompanied by chronic joint pain and hematologic abnormalities, SLE should be considered in the differential diagnosis. |
| Iyoda et al., 2008 1 case [38] | 86 y/o ♂ | general malaise | positive tests for ANA, lupus anticoagulant anemia, thrombocytopenia, elevated activated partial thromboplastin time, hypofibrinogenemia, elevated fibrin degradation products, elevated D-dimers, renal dysfunction, proteinuria, elevated CRP levels | The presence of disseminated intravascular coagulation (DIC) without an identifiable cause should raise suspicion for SLE, even in elderly patients. There have been only a few reports of DIC as the initial manifestation of SLE. |
| Ito et al., 2002 1 case [39] | 77 y/o ♀ | massive ascites, bilateral pleural effusion, pericardial effusion, bilateral lower extremity edema | positive tests for ANA, anti-dsDNA Ab hypocomplementemia leukopenia, anemia, renal dysfunction, hypoalbuminemia, proteinuria, microscopic hematuria | Chronic lupus peritonitis in elderly patients may show limited response to glucocorticoid therapy due to persistent peritoneal inflammation and impaired vascular function. |
| Aharon et al., 1994 2 cases [40] | 70 y/o ♂ | pleural effusion, generalized maculopapular rash 3 years prior to presentation | positive tests for ANA, anti-dsDNA Ab, anti-Sm Ab hypocomplementemia pancytopenia, renal dysfunction, proteinuria | SLE should be considered in elderly patients presenting with multiorgan autoimmune disease. For elderly patients where other immunosuppressive therapies are contraindicated, low-dose monthly intravenous immunoglobulin may be a treatment option. |
| 82 y/o ♀ | anorexia, weakness, nodular purplish generalized skin rash, pericardial effusion, recurrent pleural effusion and recurrent chondritis over a period of 9 years prior to presentation | hypocomplementemia pancytopenia, renal dysfunction, elevated ESR levels |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceasovschih, A.; Alexa, R.-E.; Șorodoc, V.; Asaftei, A.; Stoian, D.C.; Morărașu, B.C.; Balta, A.; Lionte, C.; Stoica, A.; Sîrbu, O.; et al. Systemic Lupus Erythematosus Features in Elderly Patients: Case-Based Review. J. Clin. Med. 2025, 14, 2558. https://doi.org/10.3390/jcm14082558
Ceasovschih A, Alexa R-E, Șorodoc V, Asaftei A, Stoian DC, Morărașu BC, Balta A, Lionte C, Stoica A, Sîrbu O, et al. Systemic Lupus Erythematosus Features in Elderly Patients: Case-Based Review. Journal of Clinical Medicine. 2025; 14(8):2558. https://doi.org/10.3390/jcm14082558
Chicago/Turabian StyleCeasovschih, Alexandr, Raluca-Elena Alexa, Victorița Șorodoc, Andreea Asaftei, Denisa Cristiana Stoian, Bianca Codrina Morărașu, Anastasia Balta, Cătălina Lionte, Alexandra Stoica, Oana Sîrbu, and et al. 2025. "Systemic Lupus Erythematosus Features in Elderly Patients: Case-Based Review" Journal of Clinical Medicine 14, no. 8: 2558. https://doi.org/10.3390/jcm14082558
APA StyleCeasovschih, A., Alexa, R.-E., Șorodoc, V., Asaftei, A., Stoian, D. C., Morărașu, B. C., Balta, A., Lionte, C., Stoica, A., Sîrbu, O., Constantin, M., Diaconu, A.-D., Lăcătușu, C.-M., Grigorescu, E.-D., & Șorodoc, L. (2025). Systemic Lupus Erythematosus Features in Elderly Patients: Case-Based Review. Journal of Clinical Medicine, 14(8), 2558. https://doi.org/10.3390/jcm14082558









