Treatment Strategy for Subaxial Minimal Facet/Lateral Mass Fractures: A Comprehensive Clinical Review
Abstract
1. Introduction
2. Anatomy and Biomechanics of the Subaxial Cervical Spine
2.1. Facet Joint Anatomy and Stability
2.2. Disc and Ligamentous Complex in Stability
2.3. Mechanisms of Facet and Lateral Mass Fractures
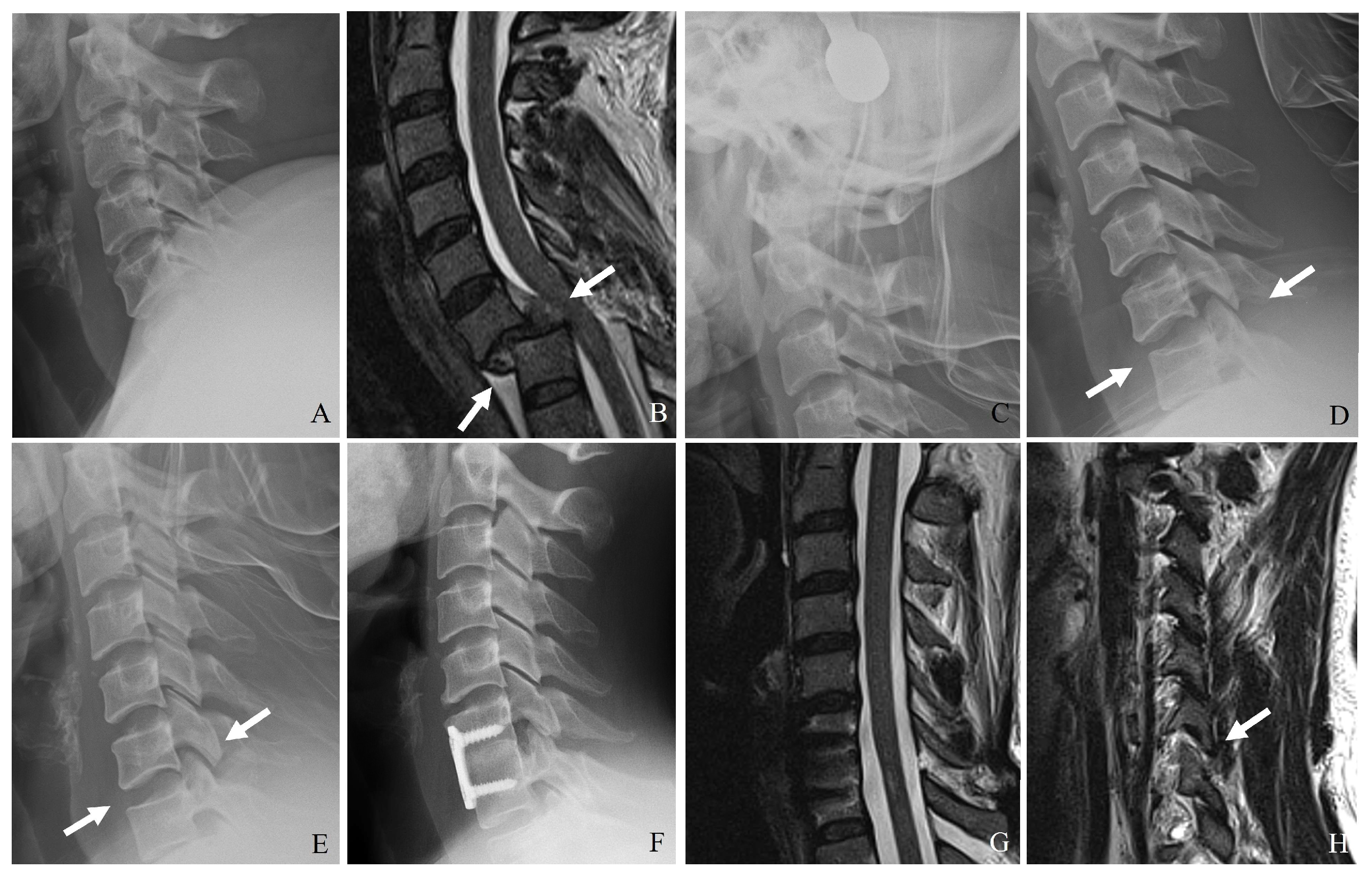
3. Imaging Modalities
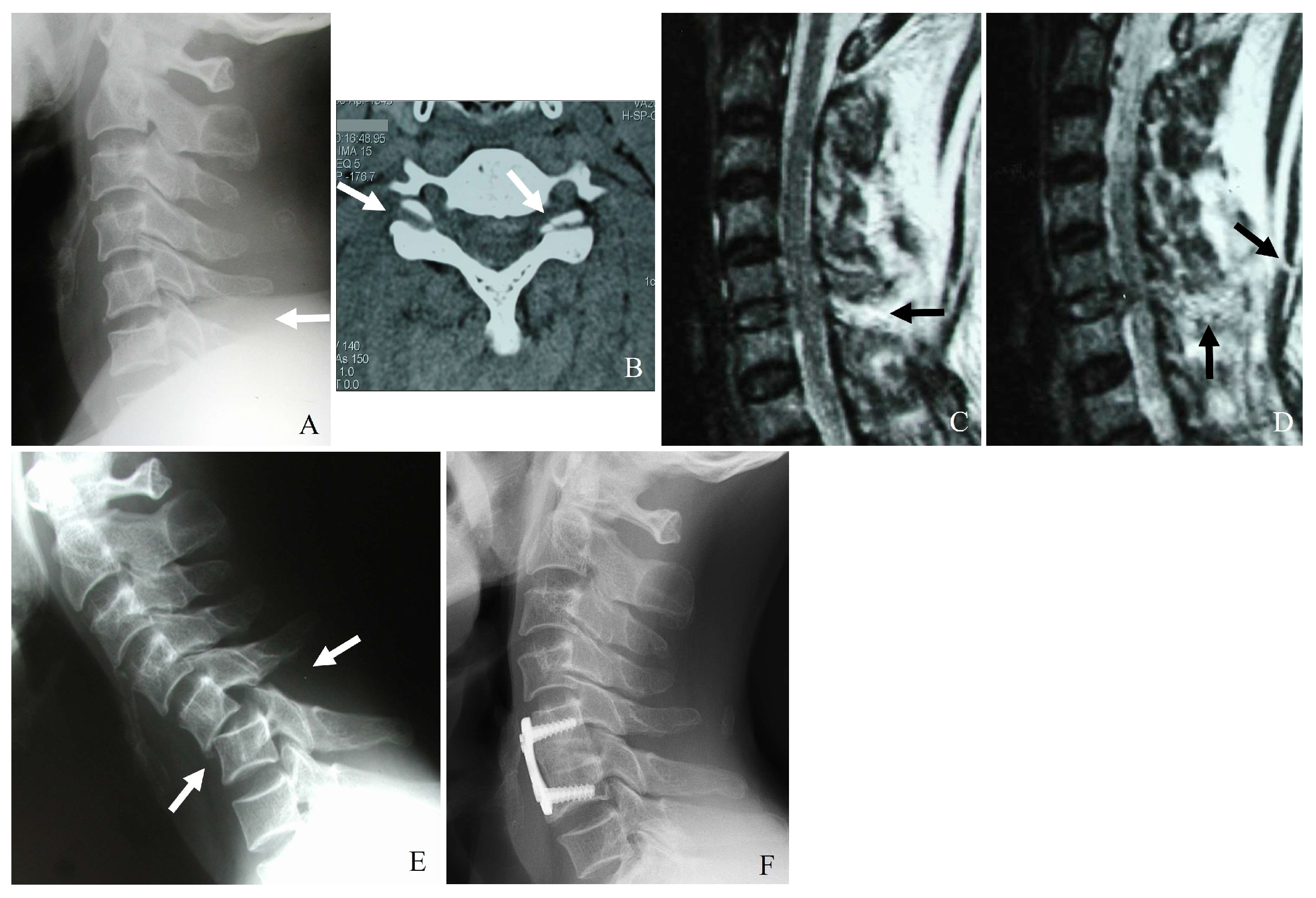
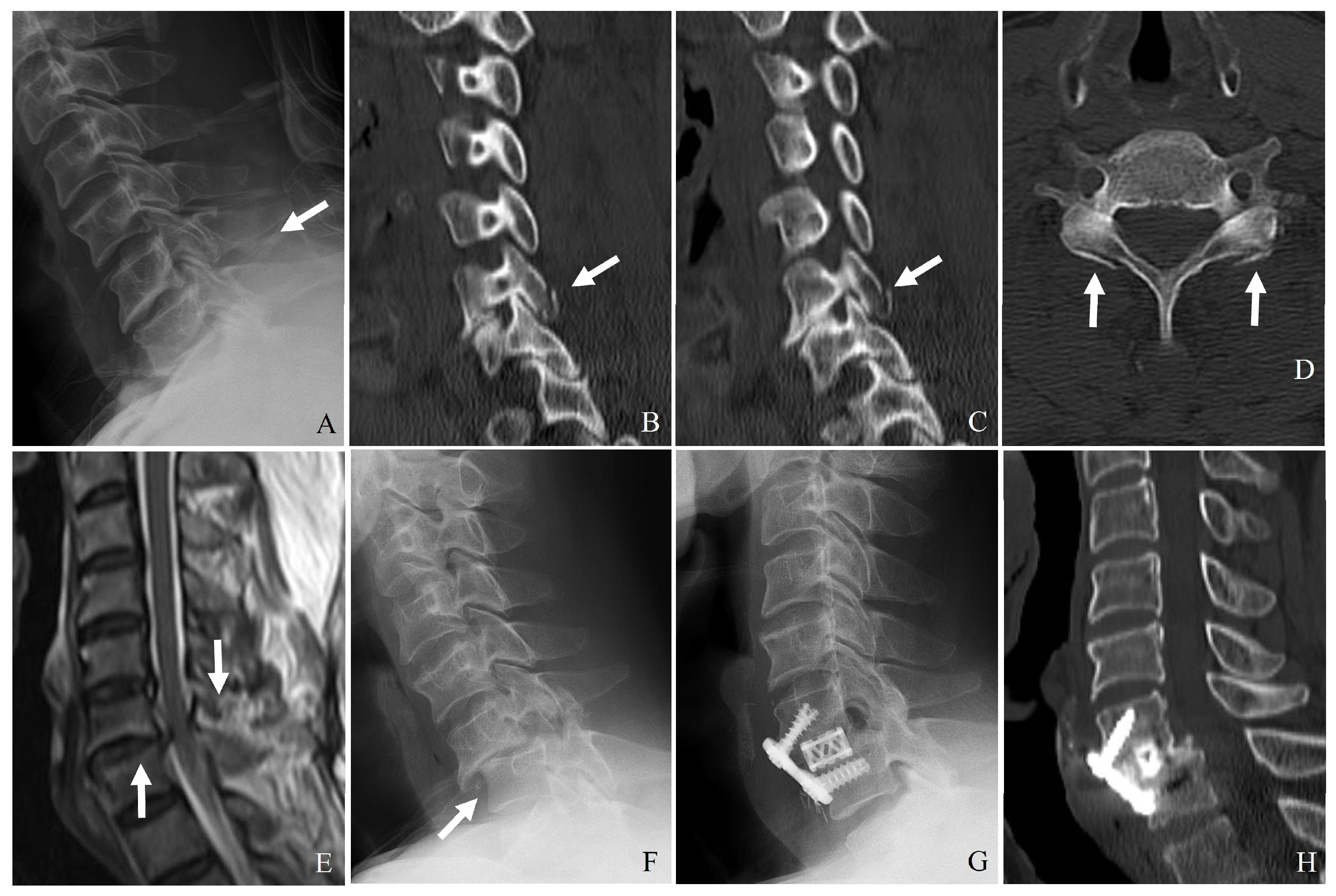
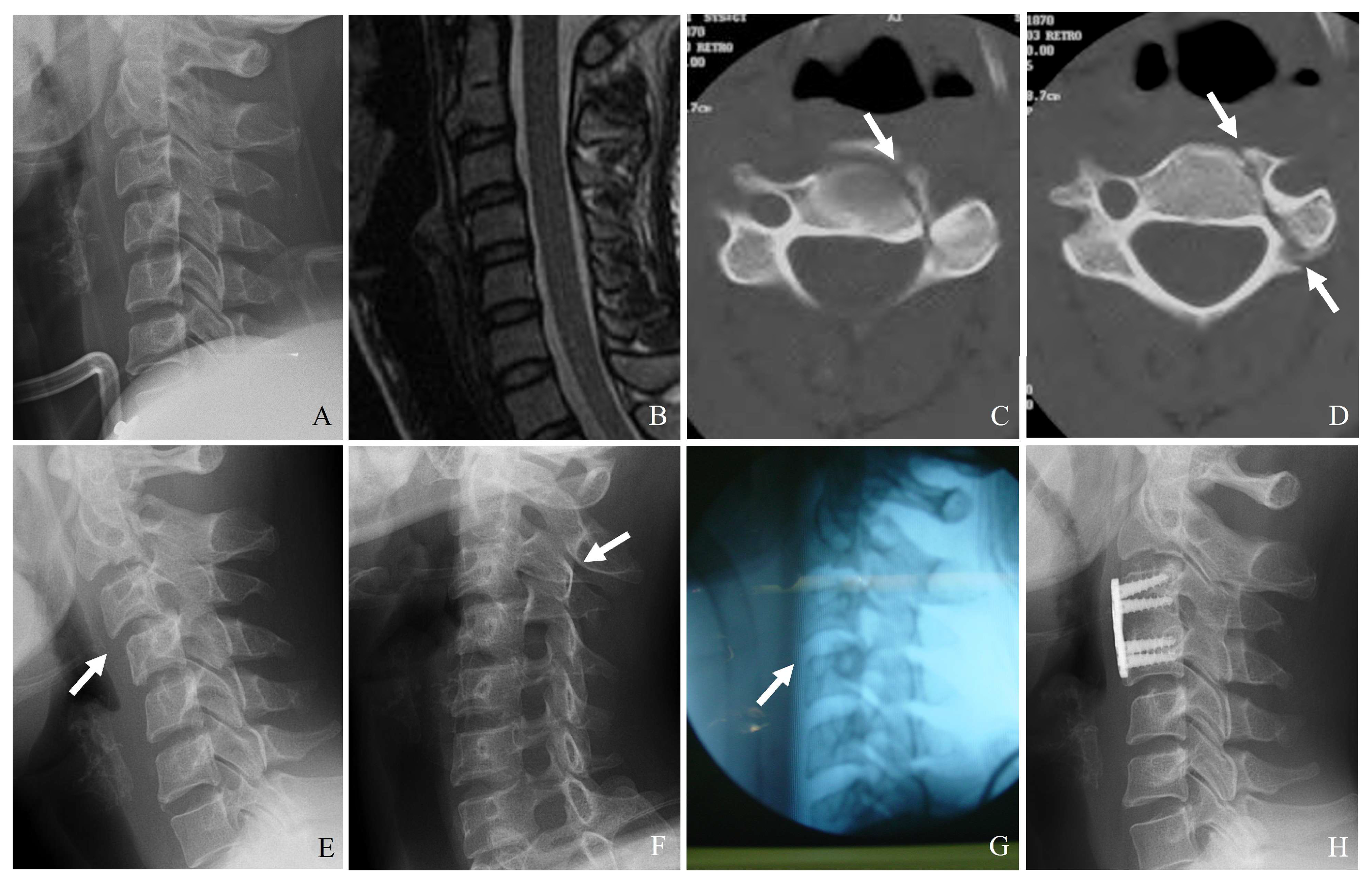
3.1. Plain Radiography
- (1)
- Malalignment of posterior elements in the lateral view.
- (2)
- Widening of the facet joint space, suggesting ligamentous disruption.
- (3)
- Perched or dislocated facets may indicate instability requiring surgical intervention.
- (4)
- Loss of vertebral height or step-off deformities, suggesting compression injuries.
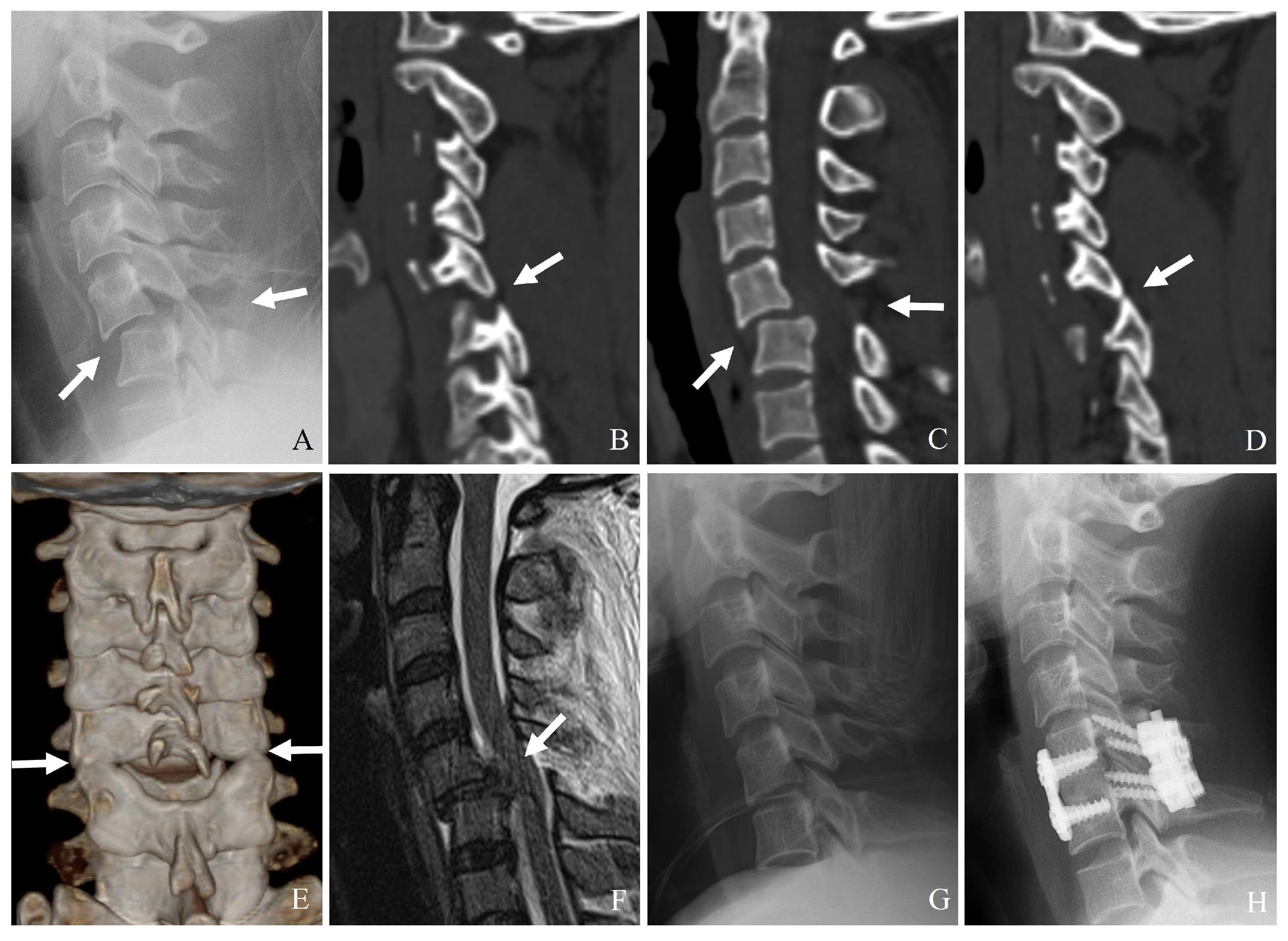
3.2. Computed Tomography (CT)
- (1)
- Identifying minimally displaced facet fractures that may be missed on radiographs.
- (2)
- Assessing lateral mass comminution and fracture propagation.
- (3)
- Evaluating facet joint alignment in axial and sagittal reconstructions.
- (4)
- Determining the extent of impaction or subluxation.
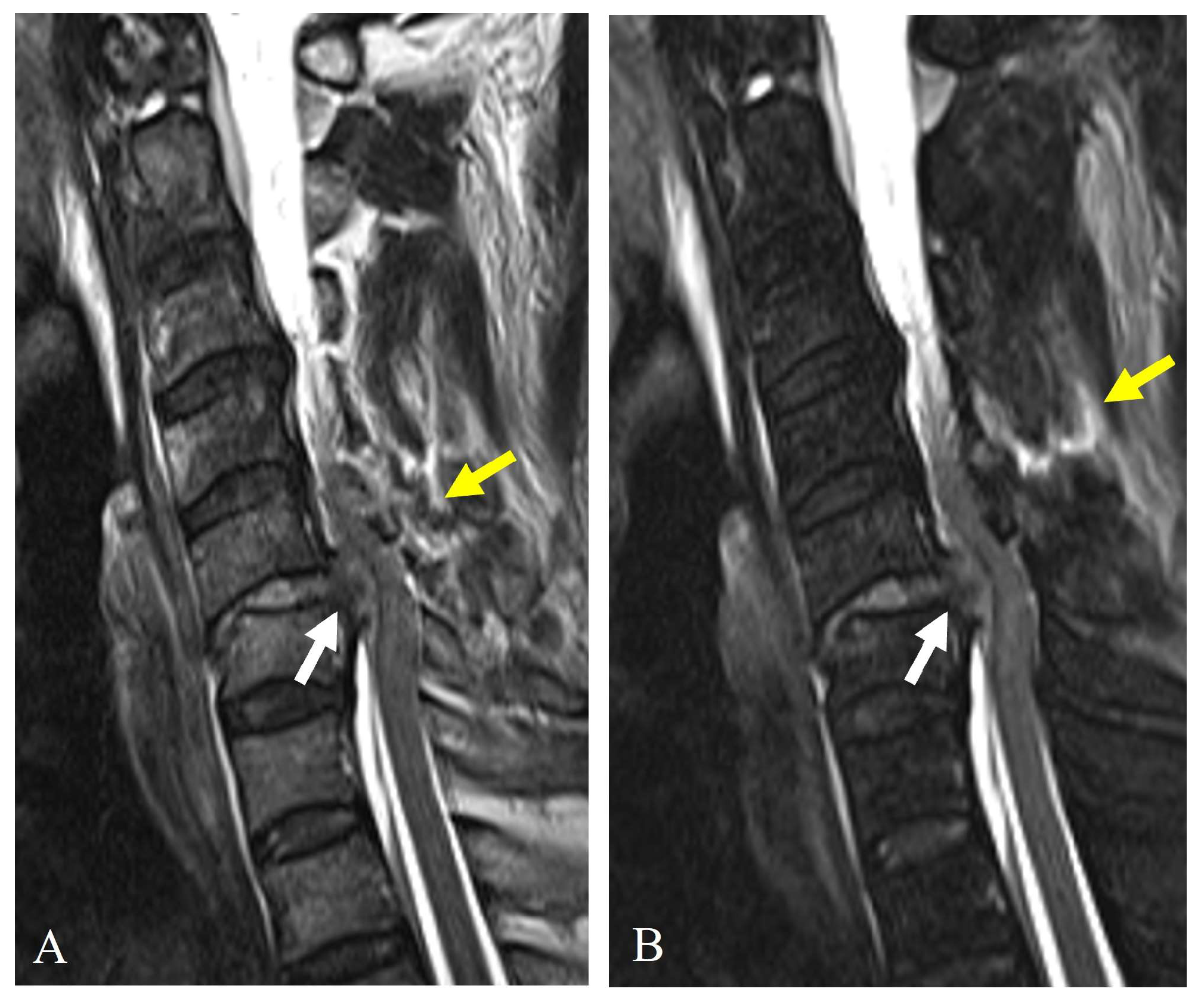
3.3. Magnetic Resonance Imaging (MRI)
4. AO Spine Subaxial Facet Injury Classification
4.1. Importance of Classification in Clinical Decision-Making
4.2. Challenges in Differentiating Facet Fracture Types (F2 and F3)
- (1)
- Subjectivity in determining displacement and instability: The definition of “displacement” varies among studies, leading to inconsistencies in classification. Some authors argue that even F2 fractures (displaced but stable) may require fixation based on clinical judgment rather than classification.
- (2)
- Lack of biomechanical validation: Limited biomechanical evidence distinguishes F2 from F3 fractures, making the classification somewhat reliant on subjective assessment rather than objective mechanical properties.
- (3)
- Neurological considerations: The classification accounts for radiculopathy (N2), but in real practice, surgical decision-making is influenced by pain severity, duration, and response to conservative management—factors that the classification system does not fully capture.
4.3. Proposed Modifications and Future Directions
- (1)
- Refinement of F2 vs. F3 criteria; a stricter, CT-based definition of facet displacement and instability could improve interobserver reliability.
- (2)
- Integration of dynamic imaging: some authors propose incorporating extended X-rays or dynamic CT scans to better assess stability.
- (3)
- Clinical modifiers: adding clinical parameters such as pain severity, response to conservative treatment, and facet capsule integrity could enhance decision-making.
- (4)
- Machine learning-based classification, AI-driven models can analyze large datasets of facet injuries, which could improve the objectivity and reliability of classification in future research.
4.4. Interobserver Reliability and Limitations of Classification Systems
4.4.1. Interobserver Reliability
4.4.2. Limitations in Clinical Practice
5. Conservative Treatment
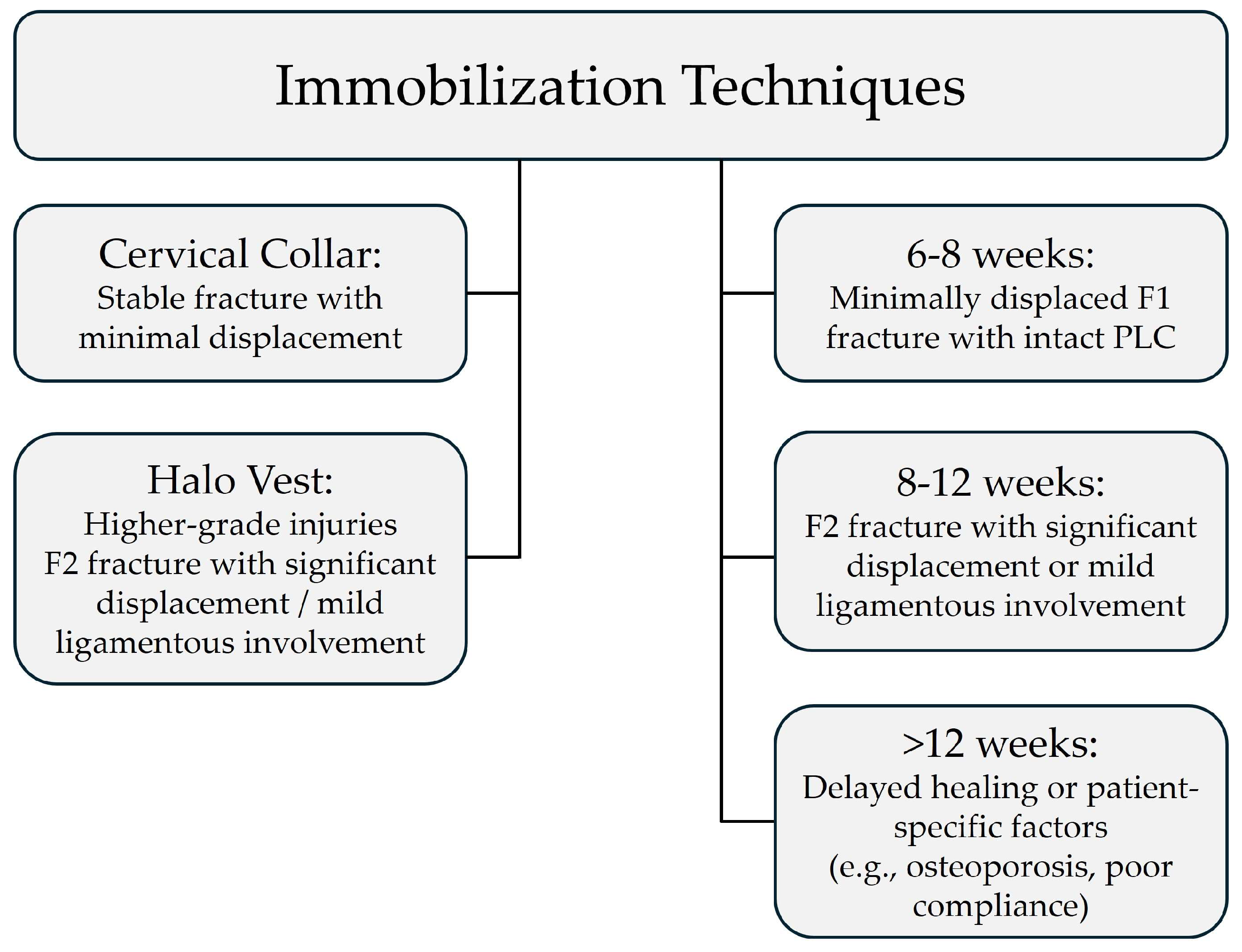
5.1. Immobilization Techniques
- (1)
- Cervical collar: A rigid cervical collar is preferred for stable fractures with minimal displacement. It is suitable for unilateral, nondisplaced, or minimally displaced fractures without significant ligamentous injury (i.e., intact posterior ligamentous complex—PLC). It is worn for 6–8 weeks, with periodic clinical and radiographic evaluations.
- (2)
- Halo vest immobilization: A halo vest is considered for higher-grade injuries where a higher level of immobilization is required (e.g., F2 injuries with significant displacement or mild ligamentous involvement). It is typically used for 8–12 weeks, followed by gradual weaning into a collar. It is not recommended for F3 injuries involving gross instability or complete PLC disruption because surgical intervention is generally required.
5.2. Duration of Immobilization
- (1)
- Six to eight weeks: For minimally displaced F1 fractures with no ligamentous injury (intact PLC). Conservative management with a rigid cervical collar is usually sufficient.
- (2)
- Eight to twelve weeks: For F2 fractures with significant displacement or mild ligamentous involvement, halo vest immobilization is typically applied for 8–12 weeks, with a gradual transition to a cervical collar if stability is achieved. However, if PLC disruption is extensive, surgical intervention may be required.
- (3)
- Longer immobilization (>12 weeks): Considered in cases of delayed healing, patient-specific factors (e.g., osteoporosis, poor compliance), or where there is concern for potential instability despite conservative management.
5.3. Patient-Specific Factors Influencing Conservative Treatment
- (1)
- Age and bone quality: Older patients with osteoporosis may have delayed healing and require prolonged immobilization.
- (2)
- Compliance: Some patients may struggle with prolonged collar use, requiring adjustments in treatment strategy.
- (3)
- Occupation and lifestyle: Athletes or individuals with physically demanding jobs may require more extended rehabilitation or early consideration of surgery.
- (4)
- Associated injuries: If additional cervical trauma or soft tissue injury is present, a more conservative approach with extended monitoring is warranted.
5.4. Follow-Up and Transition to Surgery
- (1)
- Progressive deformity or kyphosis on serial imaging.
- (2)
- Persistent severe pain despite adequate immobilization.
- (3)
- Delayed union or nonunion of the fracture.
- (4)
- Neurological deterioration or worsening instability.
6. Surgical Treatment
6.1. Indications for Surgery
- (1)
- Significant instability: Facet fractures classified as F3 or F4 in the AO Spine Subaxial Facet Injury Classification.
- (2)
- Neurological deficit: Compression of the spinal cord or nerve roots, leading to weakness, sensory deficits, or radiculopathy.
- (3)
- Progressive deformity: Increasing kyphotic angulation or worsening alignment on follow-up imaging.
- (4)
- Failure of conservative management: Persistent severe pain, progressive subluxation, or delayed instability on serial imaging.
6.2. Surgical Approaches
6.2.1. Posterior Fixation
- (1)
- Lateral mass screws: This is preferred in subaxial cervical spine fixation due to their strong biomechanical support. They can provide rigid internal fixation while allowing controlled motion. They are used in isolated lateral mass fractures or unstable facet fractures.
- (2)
- Pedicle screws: They offer stronger fixation than lateral mass screws, particularly in cases with severe comminution or vertebral instability. They are utilized when additional biomechanical stability is needed, such as in F4 fractures with severe facet fragmentation.
- (3)
- Rod constructs and posterior fusion: They are used in bilateral facet dislocations or extensive ligamentous injury cases. Posterior fusion is indicated when long-term stability is required due to extensive ligamentous damage.
6.2.2. Anterior Reconstruction
- (1)
- Anterior cervical discectomy and fusion (ACDF): ACDF is indicated when facet fractures are associated with disc herniation or anterior subluxation. It can restore anterior column stability and decompress neural elements.
- (2)
- Anterior cervical corpectomy and fusion (ACCF): ACCF is reserved for severe vertebral body comminution or multi-level instability. It requires structural grafting or cage placement to maintain spinal height.
6.2.3. Combined Anterior-Posterior Stabilization
- (1)
- Anterior decompression and fusion (ACDF or ACCF) followed by posterior fixation provides superior stability.
- (2)
- Indicated for severe F3 or F4 fractures with compromised ligamentous integrity.
6.3. Minimally Invasive Techniques
- (1)
- Percutaneous pedicle screw fixation: This is ideal for patients with isolated facet fractures and minimizes soft tissue disruption while maintaining stability.
- (2)
- Computer-assisted navigation and robotics: This enhances screw placement accuracy and reduces operative time and is particularly useful for complex subaxial fractures requiring precise screw trajectories.
6.4. Comparative Analysis of Treatment Outcomes
6.5. Decision Trees for Management Strategy
6.5.1. Decision Tree 1: Management of F1 Injury
- (1)
- Conservative treatment: Cervical collar (6–8 weeks) → clinical and radiological monitoring (every 2–4 weeks).
- (2)
- Surgical treatment: Not indicated unless there is evidence of progressive instability, neurological compromise, or persistent pain.
6.5.2. Decision Tree 2: Management of F2 Injury
- (1)
- Conservative treatment: Rigid cervical collar (8–12 weeks) if minimal displacement and stable PLC → clinical and radiological monitoring (every 2–4 weeks) to detect instability.
- (2)
- Surgical treatment: Indicated if progressive symptoms or instability are identified.
- (a)
- Posterior fixation: Preferred approach using lateral mass screws or pedicle screws depending on fracture severity.
- (b)
- Anterior reconstruction (ACDF or ACCF): Considered if there is disc herniation or anterior column instability.
- (c)
- Combined anterior-posterior stabilization: Rarely needed but considered if both anterior and posterior instability are suspected.
6.5.3. Decision Tree 3: Management of F3 Injury
- (1)
- Conservative treatment: Not recommended due to high risk of deformity, neurological compromise, and chronic instability.
- (2)
- Surgical treatment
- (a)
- Posterior fixation: Primary approach using lateral mass screws or pedicle screws.
- (b)
- Anterior reconstruction (ACDF or ACCF): Used when significant disc disruption or anterior instability is present.
- (c)
- Combined anterior-posterior stabilization: Recommended for complex or multi-level instability to provide robust stabilization.
6.5.4. Decision Tree 4: Management of F4 Injury
- (1)
- Conservative treatment: Not recommended due to profound instability and high risk of neurological deterioration.
- (2)
- Surgical treatment:
- (a)
- Posterior fixation: Preferably using pedicle screws for maximum stability.
- (b)
- Lateral mass screws: May be used but often requires additional fixation techniques.
- (c)
- Combined anterior-posterior stabilization: Frequently indicated for severe injuries to achieve adequate stabilization.
- (d)
- Anterior decompression (ACDF or ACCF) followed by posterior fixation: Recommended when there is extensive vertebral body involvement or traumatic disc herniation.
6.6. Expected Recovery Trajectories and Functional Outcomes
6.6.1. Recovery Trajectories
- (1)
- Conservative management: Healing times for minimally displaced F1 fractures are generally favorable, with immobilization for 6–8 weeks followed by a gradual return to normal activities. For F2 injuries managed conservatively, extended immobilization (8–12 weeks) may be necessary, with clinical and radiographic monitoring to detect delayed instability. Potential complications include residual pain, deformity, or progression to instability, especially in cases with incomplete ligamentous healing.
- (2)
- Surgical management: Surgical stabilization is typically followed by a structured rehabilitation program to restore neck mobility and strength. Recovery trajectories depend on the severity of the injury and the type of surgical intervention performed (e.g., posterior fixation, anterior reconstruction, or combined approaches). Early surgical intervention in unstable fractures (F3, F4) is associated with improved alignment, reduced pain, and enhanced functional recovery.
6.6.2. Patient-Reported Functional Outcomes
- (1)
- Functional outcome measures: Commonly used patient-reported outcome measures (PROMs) include the Neck Disability Index (NDI), Visual Analog Scale (VAS) for pain, and SF-36 for quality of life assessment. Surgical management is generally associated with better functional outcomes in unstable fractures, whereas conservative management can yield satisfactory results in stable injuries.
- (2)
- Comparison of conservative vs. surgical management: Studies comparing conservative and surgical management have reported superior functional outcomes following surgical stabilization in F3 and F4 fractures. However, for stable fractures (F1, stable F2), conservative management often results in comparable outcomes without the risks associated with surgery.
6.7. Ranking of Treatment Strategies Based on Evidence Levels
6.7.1. High-Level Evidence (RCTs, Cohort Studies)
6.7.2. Moderate to Low-Level Evidence (Retrospective Studies, Expert Opinion)
6.8. Economic Considerations of Conservative vs. Surgical Management
6.8.1. Conservative Management
6.8.2. Surgical Management
6.8.3. Future Considerations
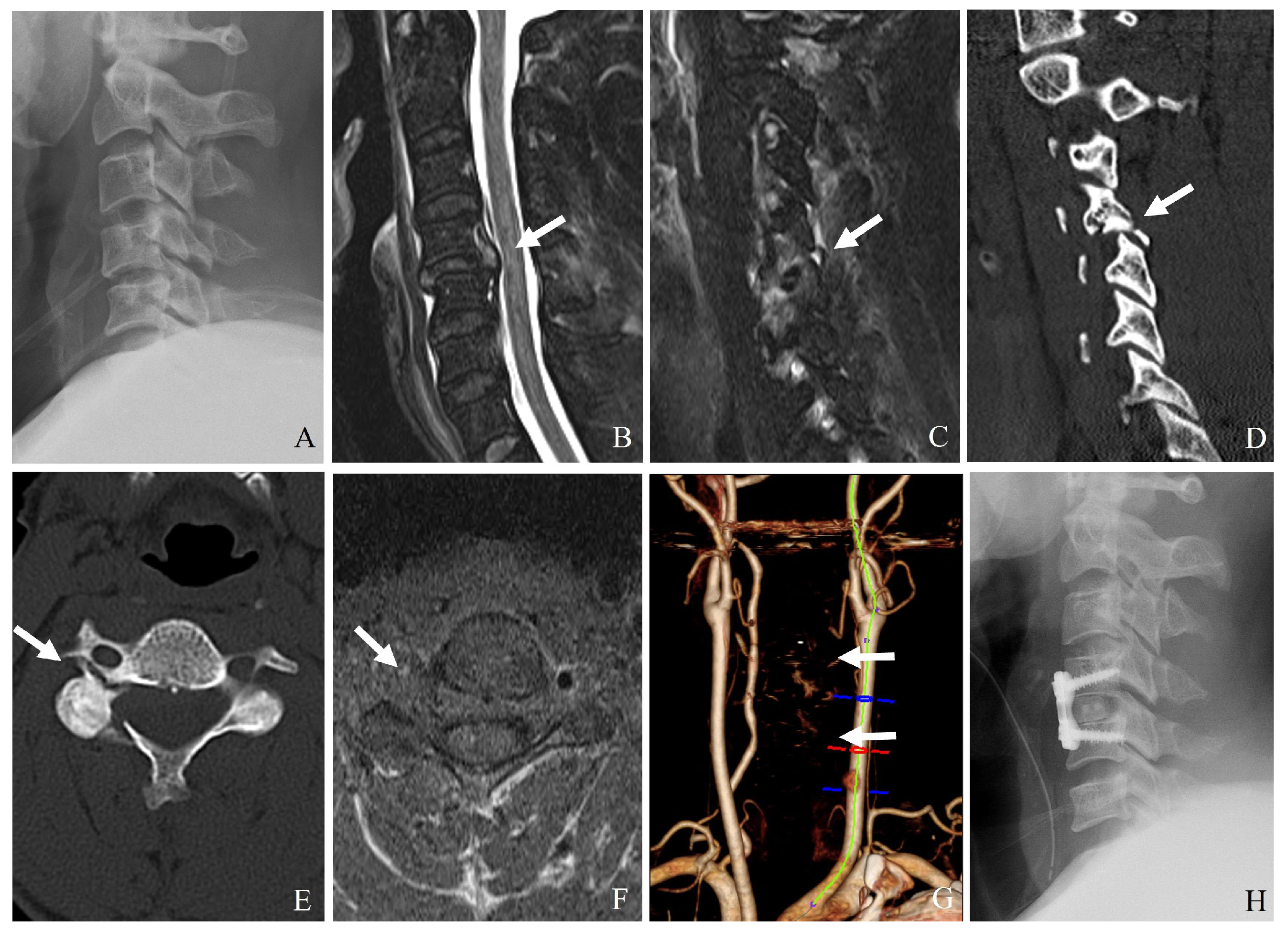
7. Vertebral Artery Injury in Subaxial Facet Injuries (C3–C7)
7.1. Anatomical Considerations of the Vertebral Artery (C3–C7)
- (1)
- V1 (pre-foraminal segment): From its origin to the transverse foramen of C6.
- (2)
- V2 (foraminal segment): Ascends through the transverse foramina of C6 to C2.
- (3)
- V3 (extracranial segment): From C2 to the dura mater at the foramen magnum.
- (4)
- V4 (intracranial segment): From dural penetration to its termination at the basilar artery.
7.2. Mechanisms of VAI in Subaxial Facet Injuries
7.2.1. Direct Compression or Stretching
- (1)
- Unilateral or bilateral facet dislocation can cause excessive rotational and translational forces on the vertebral artery, particularly at C3–C6 levels.
- (2)
- Perched or locked facets can lead to excessive stretch or kinking of the artery within the transverse foramen.
- (3)
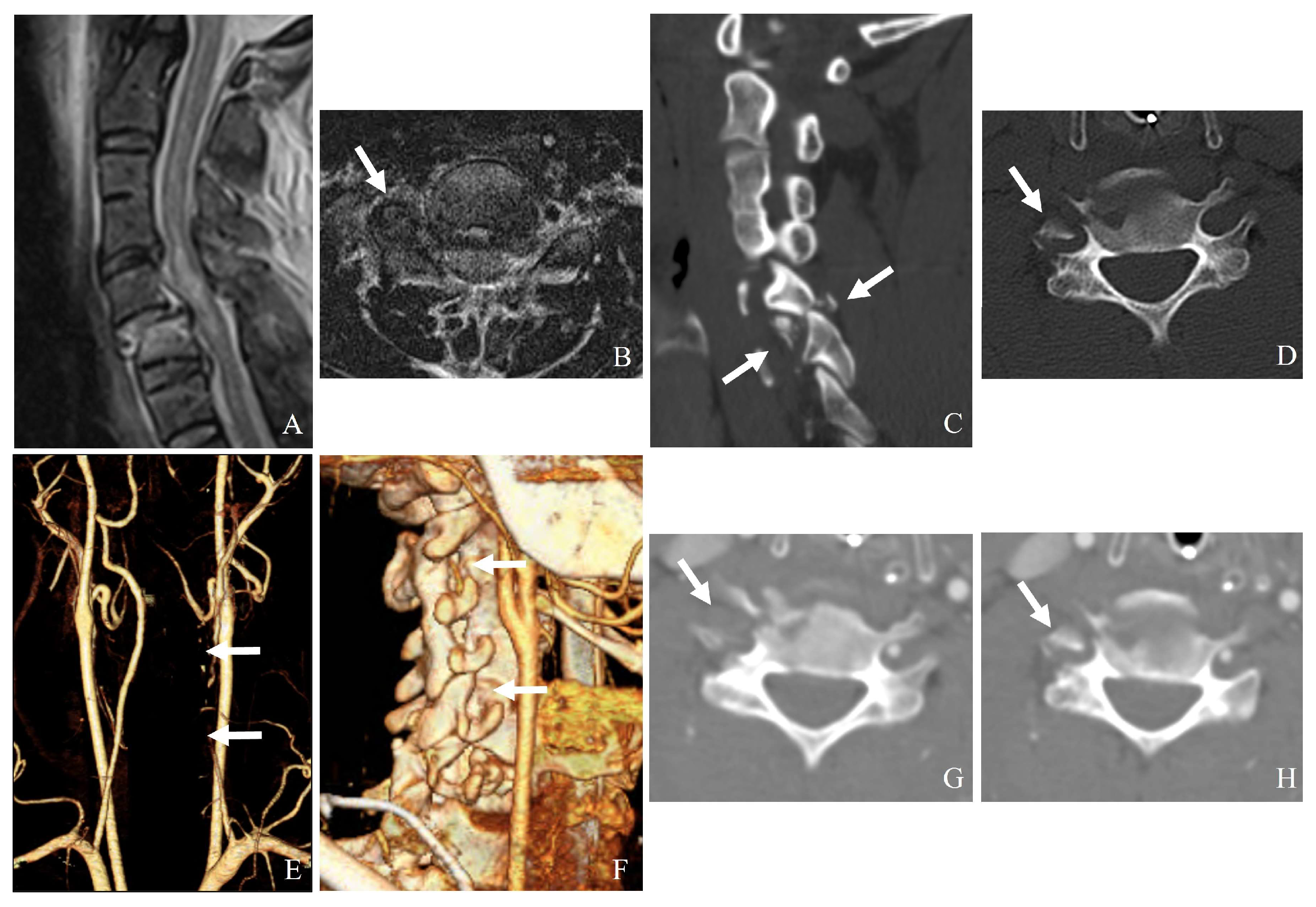
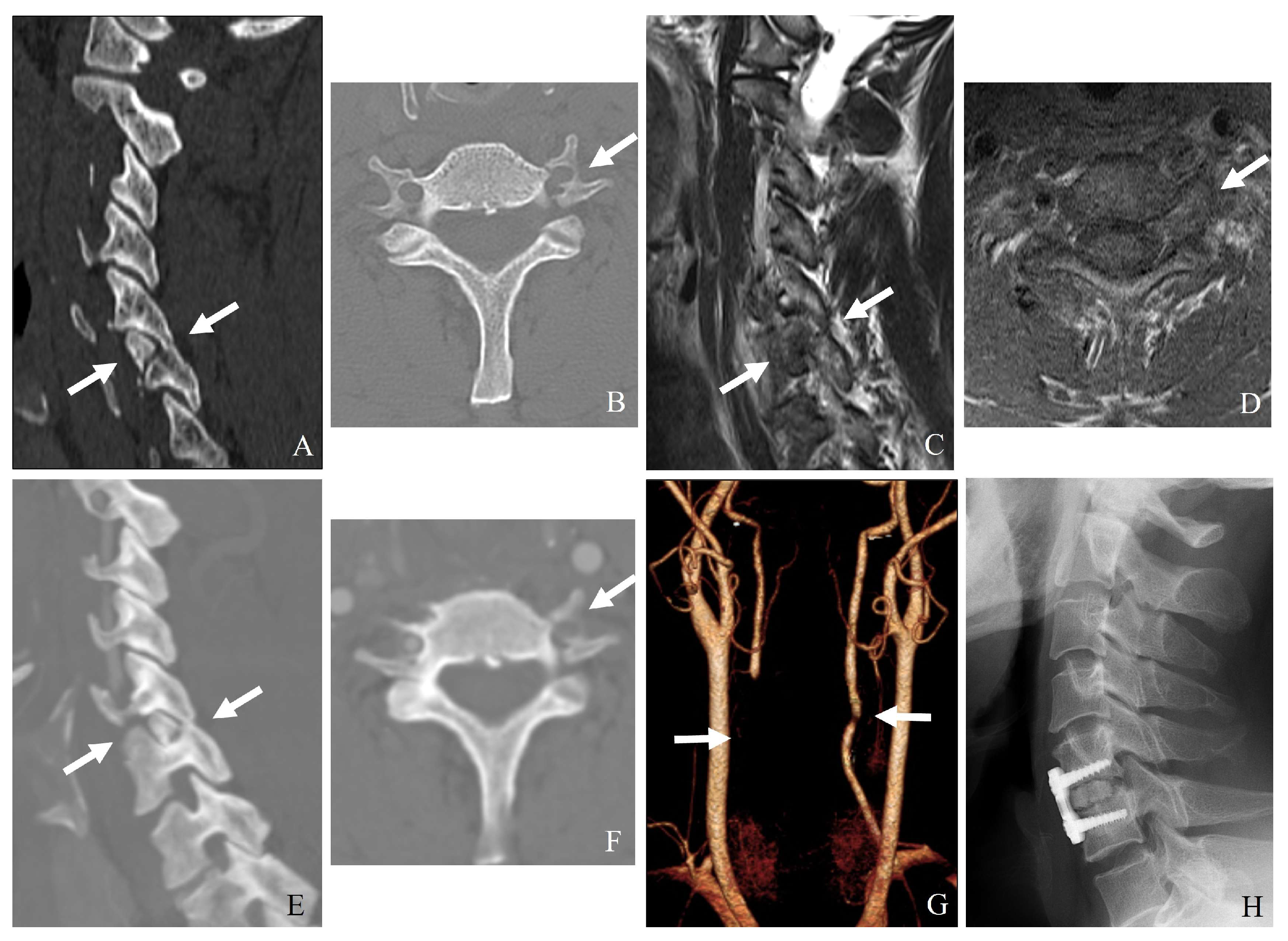
- Fracture of the lateral mass or pedicle can lead to direct bony impingement on the vertebral artery (Figure 8).
7.2.2. Occlusion from Displacement or Thrombosis
7.2.3. Laceration or Dissection
- (1)
- A facet fracture extending into the transverse foramen may directly lacerate the vertebral artery.
- (2)
- High-energy trauma can cause intimal tears, leading to dissection and secondary stenosis or occlusion.
7.2.4. Hyperextension and Rotational Injury
7.2.5. Penetrating Trauma or Iatrogenic Injury
7.3. Clinical Implications and Diagnosis
7.3.1. Symptoms: Patients with Vertebral Artery Injury May Present with
- (1)
- Posterior circulation ischemic symptoms (dizziness, vertigo, ataxia).
- (2)
- Stroke-like symptoms (contralateral weakness, dysphagia).
- (3)
- Neck pain with or without neurological deficits.
- (4)
- Delayed-onset symptoms due to progressive thrombosis.
7.3.2. Imaging [13,14,15]
- (1)
- CT angiography: The gold standard for detecting vertebral artery injuries (Figure 9).
- (2)
- Magnetic resonance angiography: Useful for assessing arterial dissection and thrombus formation.
- (3)
- Digital subtraction angiography: The most sensitive but invasive method.
7.4. Management Strategies for VAI [12,16]
7.5. Prevention of Stroke in VAI
7.5.1. Short-Term Stroke Prevention
- (1)
- Immediate initiation of antiplatelet therapy (aspirin or clopidogrel) for grade I–II injuries.
- (2)
- Avoid abrupt cervical spinal manipulation before confirming vertebral artery patency.
- (3)
- Depending on the risk of bleeding, heparin or warfarin may be considered in patients with significant stenosis or thrombus formation.
7.5.2. Long-Term Stroke Prevention
- (1)
- Continued antiplatelet therapy for 3–6 months, followed by re-evaluation with CTA or MRA.
- (2)
- Endovascular stenting for persistent pseudoaneurysm or progressive stenosis.
- (3)
- Lifestyle modifications (blood pressure control, smoking cessation, cholesterol management).
- (4)
- Rehabilitation and physical therapy to prevent secondary falls and injuries.
7.6. Complications and Prognosis
- (1)
- Ischemic stroke is the most severe complication, occurring in 7–24% of patients with untreated or poorly managed VAI.
- (2)
- Embolic events can lead to posterior circulation infarcts, particularly affecting the brainstem, thalamus, and cerebellum.
- (3)
- Chronic vertebrobasilar insufficiency can result from vascular remodeling and progressive stenosis.
8. Future Directions and Defining Instability
Instability Definition Challenges
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CT | Computed tomography |
| MRI | Magnetic resonance Imaging |
| ALL | Anterior longitudinal ligament |
| PLL | Posterior longitudinal ligament |
| DLC | Disco-ligamentous complex |
| PLC | Posterior ligamentous complex |
| ACDF | Anterior cervical discectomy and fusion |
| ACCF | Anterior cervical corpectomy and fusion |
| MISS | Minimally invasive spine surgery |
| CTA | Computed tomography angiography |
| VAI | Vertebral artery injury |
References
- Khezri, N.; Tamir Ailon, T.; Kwon, B.K. Treatment of facet injuries in the cervical spine. Neurosurg. Clin. N. Am. 2017, 28, 125–137. [Google Scholar]
- Crawford, N.R.; Duggal, N.; Chamberlain, R.H.; Park, S.C.; Sonntag, V.K.; Dickman, C.A. Unilateral cervical facet dislocation: Injury mechanism and biomechanical consequences. Spine 2002, 27, 1858–1864. [Google Scholar]
- Feuchtbaum, E.; Buchowski, J.; Zebala, L. Subaxial cervical spine trauma. Curr. Rev. Musculoskelet. Med. 2016, 9, 496–504. [Google Scholar]
- Kwon, B.K.; Vaccaro, A.R.; Grauer, J.N.; Fisher, C.G.; Dvorak, M.F. Subaxial cervical spine trauma. Am. Acad. Orthop. Surg. 2006, 14, 78–89. [Google Scholar]
- Wang, T.Y.; Mehta, V.A.; Dalton, T.; Sankey, E.W.; Goodwin, C.R.; Karikari, I.O.; Shaffrey, C.I.; Than, K.D.; Abd-El-Barr, M.M. Biomechanics, evaluation, and management of subaxial cervical spine injuries: A comprehensive review of the literature. J. Clin. Neurosci. 2021, 83, 131–139. [Google Scholar]
- Quarrington, R.D.; Jones, C.F.; Tcherveniakov, P.; Clark, J.M.; Sandler, S.J.; Lee, Y.C.; Torabiardakani, S.; Costi, J.J.; Freeman, B.J. Traumatic subaxial cervical facet subluxation and dislocation: Epidemiology, radiographic analyses, and risk factors for spinal cord injury. Spine J. 2018, 18, 387–398. [Google Scholar]
- Vedantam, A.; Fridley, J.S.; Navarro, J.C.; Gopinath, S.P. Management of acute unilateral nondisplaced subaxial cervical facet fractures. Oper. Neurosurg. 2018, 14, 104–111. [Google Scholar]
- Kepler, C.K.; Vaccaro, A.R.; Chen, E.; Patel, A.A.; Ahn, H.; Nassr, A.; Shaffrey, C.I.; Harrop, J.; Schroeder, G.D.; Agarwala, A.; et al. Treatment of isolated cervical facet fractures: A systematic review. J. Neurosurg. Spine 2016, 24, 347–354. [Google Scholar] [PubMed]
- AlBayar, A.; Sullivan, P.Z.; Blue, R.; Leonard, J.; Kung, D.K.; Ozturk, A.K.; Chen, H.I.; Schuster, J.M. Risk of vertebral artery injury and stroke following blunt and penetrating cervical spine trauma: A retrospective review of 729 patients. World Neurosurg. 2019, 130, e672–e679. [Google Scholar] [CrossRef] [PubMed]
- Page, P.S.; Josiah, D.T. Traumatic vertebral artery injuries in the geriatric population: A retrospective cohort study. J. Neurosurg. Spine 2020, 32, 657–660. [Google Scholar]
- Torina, P.J.; Flanders, A.E.; Carrino, J.A.; Burns, A.S.; Friedman, D.P.; Harrop, J.S.; Vacarro, A.R. Incidence of vertebral artery thrombosis in cervical spine trauma: Correlation with severity of spinal cord injury. Am. J. Neuroradiol. 2005, 26, 2645–2651. [Google Scholar]
- Inamasu, J.; Guiot, B.H. Vertebral artery injury after blunt cervical trauma: An update. Surg. Neurol. 2006, 65, 238–246. [Google Scholar]
- Friedman, D.; Flanders, A.; Thomas, C.; Millar, W.; Friedman, A.F.D.; Higashida, R.; Halbach, V.; Tsai, F.; Norman, D.; Pribram, H.; et al. Vertebral artery injury after acute cervical spine trauma: Rate of occurrence as detected by MR angiography and assessment of clinical consequences. Am. J. Roentgenol. 1995, 164, 4430–4447. [Google Scholar]
- Malhotra, A.K.; Camacho, M.; Ivatury, R.R.; Davis, I.C.; Komorowski, D.J.; Leung, D.A.; Grizzard, J.D.; Aboutanos, M.B.; Duane, T.M.; Cockrell, C.; et al. Computed tomographic angiography for the diagnosis of blunt carotid/vertebral artery injury: A note of caution. Ann. Surg. 2007, 246, 632–643. [Google Scholar]
- Auer, A.; Felber, S.; Schmidauer, C.; Waldenberger, P.; Aichner, F. Magnetic resonance angiographic and clinical features of extracranial vertebral artery dissection. J. Neurol. Neurosurg. Psychiatry 1998, 64, 474–481. [Google Scholar]
- Ray, C.E., Jr.; Spalding, S.C.; Cothren, C.C.; Wang, W.-S.; Moore, E.E.; Johnson, S.P. State of the art: Noninvasive imaging and management of neurovascular trauma. World J. Emerg. Surg. 2007, 2, 1. [Google Scholar]
- Vaccaro, A.R.; Koerner, J.D.; Radcliff, K.E.; Oner, F.C.; Reinhold, M.; Schnake, K.J.; Kandziora, F.; Fehlings, M.G.; Dvorak, M.F.; Aarabi, B.; et al. AOSpine subaxial cervical spine injury classification system. Eur. Spine J. 2016, 25, 2173–2184. [Google Scholar]
- Schnake, K.J.; Schroeder, G.D.; Vaccaro, A.R.; Oner, C. AOSpine Classification Systems (Subaxial, Thoracolumbar). J. Orthop. Trauma 2017, 31, S14–S23. [Google Scholar]
- Tang, C.; Fan, Y.H.; Liao, Y.H.; Tang, Q.; Ma, F.; Wang, Q.; Zhong, D.J. Classification of unilateral cervical locked facet with or without lateral mass-facet fractures and a retrospective observational study of 55 cases. Sci. Rep. 2021, 11, 16615. [Google Scholar]
- McDonald, C.L.; Daniels, A.H.; Anderson, G.A.; Alsoof, D.; Kuris, E.O. Traumatic cervical facet fractures and dislocations. JBJS Rev. 2022, 10, e22.00023. [Google Scholar]
- Elsissy, J.; Kutzner, A.; Danisa, O. Delayed diagnosis and management of traumatic cervical spine subluxation. J. Orthop. Case Rep. 2019, 9, 84–87. [Google Scholar]
- King, S.W.; Hosler, B.K.; King, M.A.; Eiselt, E.W. Missed cervical spine fracture-dislocations: The importance of clinical and radiographic assessment. J. Manip. Physiol. Ther. 2002, 25, 263–269. [Google Scholar]
- Maki, S.; Kitamura, M.; Furuya, T.; Miyamoto, T.; Okimatsu, S.; Shiga, Y.; Inage, K.; Orita, S.; Eguchi, Y.; Ohtori, S. Minimally displaced unilateral facet fracture of cervical spine can lead to spinal cord injury: A report of two cases. BMC Musculoskelet. Disord. 2021, 22, 168. [Google Scholar] [CrossRef]
- Cabrera, J.P.; Yurac, R.; Joaquim, A.F.; Guiroy, A.; Carazzo, C.A.; Zamorano, J.J.; Valacco, M.; AO Spine Latin America Trauma Study Group. CT scan in subaxial cervical facet injury: Is it enough for decision-making? Glob. Spine J. 2023, 13, 344–352. [Google Scholar]
- Grauer, J.N.; Vaccaro, A.R.; Lee, J.Y.; Nassr, A.; Dvorak, M.F.; Harrop, J.S.; Dailey, A.T.; Shaffrey, C.I.; Arnold, P.M.; Brodke, D.S.; et al. The timing and influence of MRI on the management of patients with cervical facet dislocations. Remains highly variable. A survey of members of the Spine Trauma Study Group. J. Spinal Disord. Tech. 2009, 22, 96–99. [Google Scholar] [CrossRef]
- Joaquim, A.F.; Patel, A.A.; Vaccaro, A.R. Cervical injuries scored according to the Subaxial Injury Classification system: An analysis of the literature. J. Craniovertebr. Junction Spine 2014, 5, 65–70. [Google Scholar]
- Cabrera, J.P.; Yurac, R.; Guiroy, A.; Joaquim, A.F.; Carazzo, C.A.; Zamorano, J.J.; White, K.P.; Valacco, M.; AO Spine Latin America Trauma Study Group. Accuracy and reliability of the AO Spine subaxial cervical spine classification system grading subaxial cervical facet injury morphology. Eur. Spine J. 2021, 30, 1607–1614. [Google Scholar]
- Bono, C.M.; Schoenfeld, A.; Gupta, G.; Harrop, J.S.; Anderson, P.; Patel, A.A.; Dimar, J.; Aarabi, B.; Dailey, A.; Vaccaro, A.R.; et al. Reliability and reproducibility of subaxial cervical injury description system. A standardized nomenclature schema. Spine 2011, 36, E1140–E1144. [Google Scholar] [CrossRef]
- Pehler, S.; Jones, R.; Staggers, J.R.; Antonetti, J.; McGwin, G.; Theiss, S.M. Clinical outcomes of cervical facet fractures treated nonoperatively with hard collar or halo immobilization. Glob. Spine J. 2019, 9, 48–54. [Google Scholar] [CrossRef]
- van Eck, C.F.; Fourman, M.S.; Abtahi, A.M.; Alarcon, L.; Donaldson, W.F.; Lee, J.Y. Risk factors for failure of nonoperative treatment for unilateral cervical facet fractures. Asian Spine J. 2017, 11, 356–364. [Google Scholar] [CrossRef]
- Totera, J.I.C.; Vargas, G.H.; Martini, I.F.; Romero, M.G.; Bacciarini, A.U.; Plaza, J.V.B. Unilateral cervical facet fractures: Relevance of acute disc injury in conservative treatment failure. Asian Spine J. 2023, 17, 30–36. [Google Scholar] [CrossRef]
- Anissipour, A.K.; Agel, J.; Baron, M.; Magnusson, E.; Bellabarba, C.; Bransford, R.J. Traumatic cervical unilateral and bilateral facet dislocations treated with anterior cervical discectomy and fusion has a low failure rate. Glob. Spine J. 2017, 7, 110–115. [Google Scholar] [CrossRef]
- Yang, J.S.; Liu, J.J.; Liu, P.; Liu, T.-J.; Tuo, Y.; Yan, L.; Zhang, Z.-P.; Zhang, H.-P.; Chen, H.; Hao, D.-J. Can posterior ligament structure be functionally healed after anterior reduction and fusion surgery in patients with traumatic subaxial cervical fracture-dislocations? World Neurosurg. 2020, 134, e243–e248. [Google Scholar] [CrossRef]
- Jin, C.; Xie, N.; Wang, J.; Ren, Y.; Guo, Q.; Jia, L.; Cheng, L. Clinical and radiographic outcomes of combined posterior transfacet screw fixation and anterior cervical discectomy and fusion surgery for unilateral cervical facet fracture with traumatic disc herniation: A retrospective cohort study. Pain Ther. 2022, 11, 225–240. [Google Scholar] [CrossRef]
- Abdelgawaad, A.S.; Metry, A.B.S.; Elnady, B.; El Sheriff, E. Anterior cervical reduction decompression fusion with plating for management of traumatic subaxial cervical spine dislocations. Glob. Spine J. 2021, 11, 312–320. [Google Scholar] [CrossRef]
- Jin, C.; Wang, Z.; Liu, P.; Liu, Y.; Wang, Z.; Xie, N. A biomechanical analysis of anterior cervical discectomy and fusion alone or combined cervical fixations in treating compression extension injury with unilateral facet joint. fracture: A finite element study. BMC Musculoskelet. Disord. 2021, 22, 938. [Google Scholar] [CrossRef]
- Zhang, K.; Chen, H.; Chen, K.; Yang, P.; Yang, H.; Mao, H. O-Arm navigated cervical pedicle screw fixation in the treatment of lower cervical fracture-dislocation. Orthop. Surg. 2022, 14, 1135–1142. [Google Scholar] [CrossRef]
| Aspect | Description |
|---|---|
| Facet Joint Structure | Synovial articulations between superior and inferior articular processes of adjacent vertebrae |
| Orientation | Oriented at approximately 45 degrees in the coronal plane |
| Movements Facilitated | Controlled flexion, extension, and rotational movements prevent excessive anterior translation |
| Supporting Structures | Fibrous capsule, ligamentum flavum, interspinous ligaments, posterior longitudinal ligament (PLL) |
| Stability Importance | The integrity of the facet joint is critical for maintaining the segmental motion of the cervical spine |
| Aspect | Description |
|---|---|
| Intervertebral Disc | Located between vertebral bodies, it contributes to the stability and load distribution. |
| Anterior Column | Includes anterior longitudinal ligament (ALL) and vertebral bodies with intervertebral discs. |
| Middle Column | Includes posterior longitudinal ligament (PLL) and posterior aspect of vertebral bodies. |
| Posterior Column | Includes facet joints, ligamentum flavum, interspinous, and supraspinous ligaments. |
| Functions of Ligaments |
|
| Classification | Definition | Radiologic Findings | Clinical Significance |
|---|---|---|---|
| F1 Fracture | Nondisplaced or minimally displaced facet fracture | CT: Hairline or incomplete fracture without subluxation or misalignment. MRI: Minimal or no disruption of the DLC. | Mechanically stable; treated conservatively with immobilization. |
| F2 Fracture | Displaced facet fracture without significant instability | CT: Displaced fracture, but no complete subluxation or dislocation. Fracture extends < 40% into vertebral body. MRI: Partial PLC injury, intact DLC. | May be treated conservatively; surgical stabilization if symptoms progress. |
| F3 Fracture | Unstable facet fracture with significant displacement or dislocation | CT: Completely displaced or perched facet with significant translation and rotation. Fracture extends ≥ 40% into vertebral body. MRI: Complete disruption of PLC and DLC. | Highly unstable; surgical intervention usually required to prevent neurological deterioration. |
| F4 Fracture | Comminuted facet fracture with severe instability | CT: Highly comminuted fragment with vertebral displacement. MRI: Complete ligamentous disruption and extensive soft tissue injury. | Requires immediate surgical intervention; posterior fusion or combined stabilization. |
| Parameter | Conservative Management (F1, F2) | Surgical Management (F2, F3, F4) |
|---|---|---|
| Conservative Management | High in F1; moderate in F2 (if stable) | High in F3, F4; moderate in F2 |
| Complications | Delayed instability, deformity, kyphosis | Surgical site infection, hardware failure |
| Long-term Outcomes | Favorable in stable fractures (F1) | Favorable in appropriate stabilization |
| Risk of Neurologic Deficit | Low (F1); moderate (F2 if instability exists) | High (F3, F4) without intervention |
| Indications | Stable fractures (F1, stable F2) | Unstable fractures (F2, F3, F4) |
| Management Type | Indications | Treatment |
|---|---|---|
| Conservative Management | Minor dissection or thrombosis without neurologic deficits | Anticoagulant or antiplatelet therapy (e.g., aspirin, heparin) Close radiological follow-up |
| Surgical Considerations | Open reduction of facet dislocations Transverse foramen involvement in fractures Severe arterial disruption | Careful; dissection around the transverse foramen Avoid exacerbating vertebral artery injury Endovascular interventions (e.g., stenting, embolization) |
| Endovascular Interventions | Vessel narrowing or dissection Pseudoaneurysm or Active bleeding | Stenting for vessel stabilization Coil embolization |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kong, C.-G.; Park, J.-B. Treatment Strategy for Subaxial Minimal Facet/Lateral Mass Fractures: A Comprehensive Clinical Review. J. Clin. Med. 2025, 14, 2554. https://doi.org/10.3390/jcm14082554
Kong C-G, Park J-B. Treatment Strategy for Subaxial Minimal Facet/Lateral Mass Fractures: A Comprehensive Clinical Review. Journal of Clinical Medicine. 2025; 14(8):2554. https://doi.org/10.3390/jcm14082554
Chicago/Turabian StyleKong, Chae-Gwan, and Jong-Beom Park. 2025. "Treatment Strategy for Subaxial Minimal Facet/Lateral Mass Fractures: A Comprehensive Clinical Review" Journal of Clinical Medicine 14, no. 8: 2554. https://doi.org/10.3390/jcm14082554
APA StyleKong, C.-G., & Park, J.-B. (2025). Treatment Strategy for Subaxial Minimal Facet/Lateral Mass Fractures: A Comprehensive Clinical Review. Journal of Clinical Medicine, 14(8), 2554. https://doi.org/10.3390/jcm14082554






