Abstract
Background: Osteoarthritis (OA) is a degenerative joint disease characterized by progressive cartilage breakdown, synovial inflammation, and pain, which leads to significant disability. IAHA is widely used because of its viscoelastic properties, which restore synovial fluid homeostasis and reduce symptoms. However, emerging evidence suggests that IAHA exerts additional biological effects including chondroprotection, inflammatory modulation, oxidative stress reduction, and pain modulation, which may influence disease progression. Objective: This narrative review examines the biological mechanisms underlying IAHA’s role in OA management. The review explored IAHA’s effects on synovial fluid viscoelasticity, inflammatory cytokine modulation, cartilage preservation, oxidative stress regulation, and pain pathways, emphasizing the influence of molecular weight variations on therapeutic efficacy. Additionally, this review evaluates IAHA’s integration into multimodal treatment strategies, its potential disease-modifying effects, and future directions for personalized treatment approaches. Methods: A comprehensive literature review was conducted using PubMed, Cochrane Library, EMBASE, Scopus, and Web of Science for studies published between January 2000 and March 2024. The search focused on IAHA’s molecular, cellular, and biochemical effects in OA and clinical findings assessing its impact on joint function, pain relief, and disease progression. Results: IAHA improves synovial fluid lubrication, reduces proinflammatory cytokines (IL-1β, TNF-α), inhibits matrix metalloproteinases (MMPs), scavenges reactive oxygen species (ROS), and modulates nociceptive pathways. High-molecular-weight IAHA demonstrates superior efficacy in advanced OA, while low-molecular-weight formulations may be better suited for early-stage disease. Although IAHA’s symptom relief is comparable to corticosteroids and NSAIDs, its favorable safety profile and emerging disease-modifying potential support its long-term use in OA management. Conclusions: IAHA represents a multifaceted therapeutic approach bridging symptomatic relief and regenerative strategies. While long-term efficacy, optimal administration protocols, and patient-specific responses remain subjects of ongoing research, refining treatment selection criteria, dosing regimens, and combination strategies may enhance clinical outcomes. Future studies should explore biomarker-driven approaches, standardize treatment protocols, and assess IAHA’s synergy with regenerative medicine to optimize its role in OA management.
1. Introduction
Osteoarthritis (OA) is one of the most prevalent chronic joint diseases, leading to progressive cartilage degeneration, inflammation, and pain, with a significant impact on quality of life. OA, the most prevalent form of arthritis worldwide [1,2,3,4], affects a substantial proportion of the aging population [2,5,6,7,8]. The incidence of OA is higher than that of other arthropathies [1,2], and according to the World Health Organization (WHO) [9], up to 25% of the population aged >65 years may require treatment, including surgery, for OA [4,10]. In 2020 [2], an estimated 595 million people worldwide were affected by OA, representing 7.6% of the global population [2,11]. OA has increased by 132.2% since 1990, and by 2050, the number of cases is expected to rise significantly across various joints, including the knee, hand, and hip [7,12,13,14]. OA is characterized by the gradual deterioration of the joints, including the destruction of joint cartilage [1,15,16,17], leading to joint pain [2,12], stiffness, swelling, and reduced mobility [6]. The development of OA results from a complex interplay of mechanical stress (obesity), genetic predisposition, metabolic factors, aging, and inflammatory processes that contribute to cartilage breakdown and changes in the subchondral bone [18,19,20]. In addition to articular cartilage, OA involves the subchondral and trabecular bones and all other joint structures. Exposed subchondral bone increases pain and reduces joint mobility during cartilage decay. OA can affect any joint, but the most commonly affected joints bear the body weight and are highly susceptible to mechanical stress [1,2,5,21]. OA can present as an asymptomatic incidental finding or a severely disabling disorder [1,4,11,18,19]. Progressive degeneration of articular cartilage reduces the structural integrity of the joint and significantly deteriorates the quality of life. OA is a significant public health problem because of its prevalence and significant impact on mobility and activities of daily living (ADL) [22]. Traditionally, OA is categorized into two major forms: Primary OA (Idiopathic) and Secondary OA. Primary OA occurs without any identifiable underlying cause, while Secondary OA develops in the presence of a specific predisposing factor or pathology (e.g., congenital abnormalities, trauma, or avascular necrosis). Primary or idiopathic OA arises without obvious traumatic, congenital, or metabolic triggers. It is most strongly associated with aging and the cumulative effects of mechanical loading over time. Common sites involved in osteoarthritis include the knees, which are often affected due to their critical role in weight-bearing and mobility; the hips, where degenerative changes in the femoral head and acetabulum cause significant disability; the hands, particularly the distal interphalangeal joints (Heberden’s nodes) and proximal interphalangeal joints (Bouchard’s nodes); the spine, with the cervical and lumbar regions frequently involved, leading to facet joint OA; the first carpometacarpal joint (base of the thumb), which contributes to grip and pinch strength, with OA here causing functional limitations; and the first metatarsophalangeal joint (hallux rigidus), which manifests as pain and stiffness in the big toe. Secondary OA develops when a known pathological or mechanical factor contributes to the breakdown of normal joint architecture. Key causes include congenital abnormalities, traumatic injuries, and conditions that compromise the structural integrity of bone and/or cartilage. Post-traumatic OA arises when an injury (acute or chronic) disrupts normal joint structure. Even with repair or reconstruction, joint integrity may not fully return to its pre-injury condition, setting the stage for progressive cartilage degeneration.
Avascular necrosis, also known as osteonecrosis, entails the loss of blood supply to the subchondral bone. It is most common in the femoral head but can affect the humeral head, talus, scaphoid, or other bones. Secondary forms have a well-defined primary pathogenetic factor that should be prioritized for treatment [23,24]. In contrast, primary OA is influenced by its localization, which is linked to a distinct pathogenetic factor. As a result, different therapeutic interventions may have varying effects. Endophenotypes refer to distinct subgroups of patients within the exact localization of primary OA, categorized based on specific clinical, biological, or morphological characteristics. In recent years, scientists and health professionals have focused on identifying and characterizing the phenotypes of OA and its associated endotypes. As a starting point, six clinical phenotypes and nine endotypes of knee OA have been described [25]. Four distinct endophenotypes were identified for hip OA (HOA) [26], each reflecting specific clinical, radiological, or biochemical patterns. These variations highlight the multifaceted nature of HOA, in which factors such as joint congruence, acetabular morphology, and systemic inflammatory markers intersect differently in individual patients. By contrast, the categorization of hand OA remains a subject of ongoing debate. While [26] proposed three endophenotypes, ref. [27] suggested five, reflecting diverse presentations involving different joints in the hand, inflammation levels, and cartilage degeneration patterns. These discrepancies underscore the complexity of OA pathogenesis and the need for continued research. These endophenotypes help clarify why certain patients may present with more pronounced inflammatory changes, whereas others exhibit primarily mechanical issues or cartilage deterioration. By identifying and understanding these subgroups, clinicians can better tailor treatment approaches, such as targeted pharmacotherapy for inflammation, mechanical realignment procedures, regenerative techniques, and other interventions, aiming for more effective and personalized management of OA. Although widely used, IAHA is often seen as merely symptomatic rather than disease-modifying.
IAHA has a long history, originating in the early 1990s as a way to restore rheological balance within the joint [27,28]. Early research highlighted IAHA’s ability to supplement synovial fluid and improve lubrication. Over time, multiple clinical studies supported its efficacy in alleviating pain and enhancing joint function, incorporating it into numerous treatment guidelines [22,29,30]. As a result, IAHA has become a commonly employed intervention for osteoarthritis management, particularly in knee OA. Meanwhile, researchers continue investigating novel formulations, varying molecular weights, and adjunctive therapies to optimize outcomes, minimize side effects, and address challenges such as patient selection and long-term efficacy. This review demonstrates that IAHA remains a dynamic and evolving component of osteoarthritis treatment.
Recent insights into IAHA’s molecular and cellular mechanisms of IAHA, particularly its anti-inflammatory, chondroprotective, and oxidative stress-modulating effects, suggest its broader role in OA management. These findings and evidence of tailored applications based on molecular weight and disease stage warrant further investigation.
Hyaluronic Acid (HA) in OA Management
Despite numerous treatment options, including non-pharmacological and pharmacological interventions, there is an urgent need for more effective long-term strategies to alleviate symptoms and delay surgical intervention. HA, a naturally occurring glycosaminoglycan in synovial fluid, is vital for joint homeostasis [31,32]. It enhances the viscoelastic properties of synovial fluid, which are crucial for joint lubrication, shock absorption, and smooth, pain-free movement [33,34,35,36,37,38]. In OA, particularly KOA, HA concentration and molecular weight in synovial fluid are often reduced, leading to decreased lubrication and increased joint friction, exacerbating symptoms, and accelerating degeneration [34]. Viscosupplementation (VS) involving IAHA has become an essential treatment option [39,40,41,42,43,44,45,46,47,48,49,50,51,52], a process in which it is directly injected into the affected joint [49,50,53,54,55,56,57,58,59,60,61,62,63,64,65]. IAHA aims to restore the viscoelastic properties of synovial fluid, reduce pain, and improve joint function, potentially delaying surgical interventions, such as total joint replacement [66,67,68,69,70,71].
This review examines the modulation of key biological processes in osteoarthritis (OA) by intra-articular hyaluronic acid (IAHA), including synovial fluid homeostasis, chondroprotection, inflammatory suppression, oxidative stress reduction, and pain modulation. It synthesizes current evidence regarding IAHA’s clinical effectiveness in OA management, focusing on molecular weight variations. The review assesses IAHA’s potential disease-modifying effects, its role in multimodal treatment strategies, and future biomarker-driven personalized approaches. Identifying research gaps aims to provide insights for optimizing IAHA therapy in clinical practice. The study aimed to collate and discuss IAHA’s mechanisms and clinical aspects from various studies, rather than pool statistical results into a single quantitative effect size estimate. Many included studies use different populations, outcome measures, and interventions (such as varying IAHA formulations), making direct comparisons or pooled statistical analyses challenging. Consequently, this work focuses on synthesizing themes and identifying mechanistic insights, rather than combining datasets for inferential statistics.
2. Materials and Methods
2.1. Literature Search and Data Sources
This narrative review synthesizes the current evidence of the biological mechanisms of IAHA in osteoarthritis (OA). A literature search was conducted across PubMed, the Cochrane Library, EMBASE, Scopus, and Web of Science for studies published between January 2000 and December 2024. The key mechanisms of action of IAHA in OA treatment have been investigated and analyzed. Multiple mechanisms comprising the potential joint effects were traced, and the following were highlighted: viscoelastic and lubricating action, chondroprotection, modulation of inflammation, reduction in oxidative stress, and modulation of pain. The search terms were combined using Boolean operators (AND and OR). Core IAHA concepts keywords included the following: “hyaluronic acid” OR “hyaluronan” OR “IAHA” OR “viscosupplementation”; Osteoarthritis Pathophysiology: “osteoarthritis” OR “degenerative joint disease” OR “cartilage degradation”; Biological Mechanisms: “synovial fluid homeostasis” OR “joint lubrication” OR “viscoelasticity”; Chondroprotection: “cartilage preservation” OR “proteoglycan synthesis” OR “extracellular matrix stability”; Inflammatory Modulation: “cytokines” OR “immune response” OR “CD44 receptor” OR “RHAMM receptor”; Oxidative Stress Regulation: “reactive oxygen species” OR “antioxidant defense” OR “oxidative damage”; Pain Modulation: “nociceptive pathways” OR “neuroinflammation” OR “pain signaling”; Molecular Weight Considerations: “low molecular weight HA” OR “high molecular weight HA”. Additional studies were identified by manually screening the reference lists from systematic reviews and meta-analyses.
2.2. Criteria Selection Criteria for the Study
Studies were selected based on predefined criteria:
Inclusion Criteria:
The inclusion criteria encompassed randomized controlled trials (RCTs), observational cohort studies, systematic reviews, and investigations into the molecular mechanisms of intra-articular hyaluronic acid (IAHA) in synovial fluid and cartilage. Studies were selected based on mechanistic investigations exploring the effects of IAHA; assessments of IAHA’s impact on synovial fluid, cartilage, inflammation, oxidative stress, and pain pathways; comparative analyses of IAHA formulations based on molecular weight; and evaluations of IAHA’s potential as a disease-modifying agent. Only articles published in English were considered for inclusion in the present study. Broad inclusion criteria were employed because the primary objective was to delineate the clinical and mechanistic landscape of IAHA. The study included peer-reviewed original research articles, reviews, and meta-analyses focusing on IAHA or viscosupplementation in human osteoarthritis (OA) populations, as well as studies providing mechanistic insights into the effects of hyaluronic acid on cartilage, synovial fluid, inflammation, oxidative stress, or pain modulation.
Exclusion Criteria:
Studies that lacked clinical relevance to humans and those without molecular or biochemical evaluations were excluded. Strategies such as sensitivity analysis by excluding low-quality studies, prioritizing studies from high-impact journals, categorizing results by study design to highlight discrepancies, and critically evaluating bias in industry-sponsored studies were employed to address conflicts arising from contradictory studies. Non-peer-reviewed articles, conference abstracts, case reports, and animal or in vitro studies without clinical relevance were excluded. Furthermore, studies focusing solely on the efficacy and safety of IAHA, without discussing the biological mechanisms of action, were not considered. The exclusion criteria included conference abstracts lacking sufficient data for assessment, animal or in vitro studies that did not provide clinically translatable insights, and articles unrelated to intra-articular HA or OA pathophysiology.
2.3. Data Extraction and Synthesis
Two independent reviewers extracted data, including study details (author, year, journal), study design (RCT, cohort study, mechanistic study, review), patient characteristics (OA severity, synovial fluid composition, prior treatments), intervention details (IAHA molecular weight, dosing regimen, and frequency), and mechanistic outcomes (synovial fluid restoration and lubrication, chondroprotection and extracellular matrix integrity, inflammatory cytokine suppression, oxidative stress reduction, and pain pathway modulation).
Discrepancies were resolved by consensus discussion, and a third reviewer was consulted if necessary. Because of the heterogeneity in the study designs, IAHA formulations, and mechanistic endpoints, a narrative approach was used.
3. Results
The review used the PRISMA guidelines’ rigorous and transparent methodological approach (Figure 1).
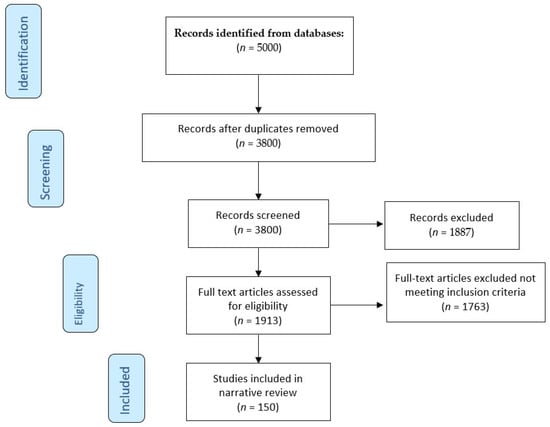
Figure 1.
Flow chart of the literature search using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
3.1. Hyaluronic Acid
Hyaluronic acid (HA), hyaluronan, and hyaluronate are critical in managing OA, particularly knee OA [31,32]. Its application in VS aims to restore the viscoelastic properties of synovial fluid, alleviate pain, improve joint function, and potentially delay surgical intervention [33,34,35,36]. The pathophysiology of OA involves mechanical joint stress, genetic susceptibility, ethnicity, nutrition, sex [35], and age-related alterations in HA concentration and molecular weight within the joint tissues [34].
HA is a non-sulfated glycosaminoglycan (GAG) mucopolysaccharide, an anionic polysaccharide found in all living organisms [72]. It was initially isolated from a bovine vitreous body and reported in 1934 by Karl Meyer and John W. Palmer [73]. HA’s first biomedical application of HA for ophthalmic surgery occurred in the late 1950s [74]. Its chemical structure and biological properties have led to its extensive utilization in therapies such as dermal fillers, tissue engineering, VS, ocular treatments, wound healing, drug delivery, and cancer therapy [36,72]. Intra-articular injections of VS have been documented in various joints, including the knee, hip, shoulder, ankle, temporomandibular, and interphalangeal joints. Currently, HA is indicated for OA treatment in any synovial joint, either as part of a comprehensive treatment plan or selectively, particularly in early-stage OA.
3.2. Hyaluronan (HA) Production
Hyaluronan (HA) is a polysaccharide of significant biological importance and is synthesized by specialized enzymes known as hyaluronan synthases, which reside on the cytoplasmic face of the plasma membrane [75]. These enzymes meticulously incorporate UDP-activated sugar residues during polymerization into an elongated HA chain. The newly formed hyaluronan strand is then carefully moved through channel-like or pore-like structures, ensuring its final destination is outside the cell in the extracellular compartment [76].
Mammals have three primary hyaluronan synthases: HAS1, HAS2, and HAS3 [77,78,79,80]. Although each has a distinct gene locus, all three enzymes share a fundamental enzymatic characteristic; they use two specific substrates, UDP-α-N-acetyl-D-glucosamine (UDP-GlcNAc) and UDP-α-D-glucuronate (UDP-GlcUA), to build the HA chain [81]. Several researchers have categorized known HA synthase enzymes into Class I and II based on their homology, catalytic features, and evolutionary lineage. The eukaryotic and Streptococcal HAS isoforms align with Class I, whereas a lone representative from Pasteurella multocida comprises Class II [82]. This classification has helped clarify functional and structural differences among synthases from diverse organisms. A substantial portion of our understanding of HA synthase’s mechanistic intricacies comes from bacterial HA synthase [83,84]. A significant leap forward in the field has occurred with the successful cloning of HAS genes from both prokaryotic and mammalian organisms. The DeAngelis group notably isolated and characterized the hasA gene from Group A Streptococcus, which encodes a protein called HasA. Subsequent studies confirmed that HasA is a bona fide HA synthase in Streptococcus pyogenes. Moreover, transferring HasA into bacteria lacking native HA capsules, such as certain Streptococcus strains and Enterococcus faecalis, enables these organisms to synthesize HA, thereby establishing HasA as the core enzyme in forming the bacterial HA capsule [82]. Parallel research efforts in mammals have led to the cloning of mouse and human HA synthases [85]. Upon further examination, these mammalian enzymes showed a high degree of amino acid sequence homology between themselves and across various species, including frogs (Xenopus) and certain bacteria. Notably, the human haS1 isoform closely resembles the hasA gene product of Streptococcus pyogenes, highlighting a striking level of evolutionary conservation. Additional work has mapped the genomic locations and structural organization of HAS1, HAS2, and HAS3, revealing that they occupy different autosomes. These findings suggest that the HAS gene family emerged early in vertebrate evolution, possibly via the serial duplication of an ancestral HAS gene. Collectively, these insights illuminate the complex molecular choreography of HA biosynthesis, from genetic foundations and enzyme architecture to stepwise addition of sugar units and extracellular release of the growing polysaccharide. By integrating bacterial and eukaryotic findings, researchers have shed light on how a widely conserved enzyme family orchestrates the formation of this critical extracellular matrix component, which is indispensable to both health and disease. Most HA supplementation products are avian-derived; hyaluronan is often sourced from rooster combs and then chemically crosslinked or produced via bacterial fermentation [74]. While many fermentation protocols employ genetic engineering to increase yield or alter properties, these items are seldom labeled “recombinant”. Instead, manufacturers typically say “fermented HA” or “microbial fermentation”, even if the process could be considered recombinant in a technical sense. Both avian and bacterial sources of HA require thorough purification. Residues from either process may pose side effect risks if they are not removed. In peer-reviewed studies on hyaluronic acid (e.g., for viscosupplementation injections), the origin of HA is often specified, although not always standardized. Consequently, physicians and patients may be unaware of the differences among the various HA products in everyday clinical use.
3.3. Molecular Mechanisms of IAHA
HA, a naturally occurring substance in the body, exerts therapeutic effects on OA via several physical and molecular mechanisms. These mechanisms are crucial for understanding HA’s role in OA [86].
HA restores the flexibility of synovial fluid and improves joint movement and shock absorption [87]. This is primarily achieved by increasing the concentration and size of hyaluronic acid molecules in the joint. At the molecular level, hyaluronic acid is a large molecule with repeating sugar units. When injected into the joint, hyaluronic acid supplements the naturally occurring hyaluronic acid, increasing its size and concentration in the synovial fluid [34,87,88]. The electrostatic and osmotic properties of the extracellular matrix (ECM) are also improved, thanks to proteoglycans that contain negatively charged glycosaminoglycan (GAG) chains (e.g., chondroitin sulfate and keratan sulfate), which attract water molecules, create osmotic pressure in the ECM and retain water in the cartilage [89].
HA helps maintain the integrity of the pericellular matrix (PCM), a specialized layer of ECM that surrounds each chondrocyte and protects chondrocytes from mechanical stress [90]. HA interacts with aggrecan to form large, hydrated complexes that help improve cartilage elasticity. Hyaluronate–aggrecan complexes form the primary molecular mechanism providing cartilage elasticity and load-bearing capacity [34].
HA is a long-chain GAG composed of repeating disaccharide units that provide a strong and flexible structure for binding multiple aggregate molecules. The connection between HA and aggrecan is facilitated by a small molecule known as a linking protein that stabilizes the bond between HA and aggrecan, creating a strong and durable connection [91]. The aggrecan molecule has a core protein densely decorated with GAG side chains, mainly chondroitin sulfate and keratan sulfate. GAG chains have a high negative charge, attract water molecules, and create an osmotic environment that increases the hydration of the complex [92].
HA–aggrecan complexes interact with water to form a gel-like structure that fills the cartilage’s extracellular matrix (ECM). The gel-like matrix imparts unique viscoelastic properties to the cartilage, allowing it to compress and rebound. A high hydration level promotes the diffusion of nutrients to chondrocytes embedded in the cartilage, supporting their survival and function [93].
Highly hydrated HA–aggrecan complexes resist compression by generating internal swelling pressure. The negatively charged GAG chains on aggrecan repel each other and resist compression because of their electrostatic interactions [94]. By binding aggrecan to stable complexes, HA helps protect aggrecan from enzymatic degradation owing to the effects of enzymes typical of osteoarthritis, such as aggrecanases and matrix metalloproteinases (MMPs), which are elevated and degrade ECM components, including aggrecan [95].
The stability of the HA–aggrecan complex reduces the likelihood of cleavage and release of aggrecan from the ECM, thus preserving the cartilage matrix structure and function [92,93]. Large HA–aggrecan complexes evenly distribute mechanical loads in the cartilage. Forming a uniform and resilient matrix, these complexes help maintain the smooth cartilage surface necessary for efficient joint movement and reduce the local stress concentrations leading to cartilage wear. Through these molecular interactions, HA and aggrecan together form a resilient, hydrated matrix that enables the cartilage to absorb shock, resist compressive forces, and maintain its structural integrity [96]. Together, these molecular mechanisms contribute to the therapeutic effect of HA delivery in treating osteoarthritis.
Hyaluronic acid (HA) is a potent mediator of inflammation. This reduces the production of proinflammatory cytokines and joint inflammation. HA binds primarily to CD44 and the receptor for hyaluronan-mediated motility (RHAMM), which are expressed on the surface of synovial cells, chondrocytes, and immune cells [97,98]. The binding of HA to CD44 can inhibit the nuclear factor kappa-light-chain-enhancer (NF-κB) pathway, a master transcriptional regulator of inflammation [99,100]. Under inflammatory conditions, NF-κB translocates to the nucleus and promotes the expression of genes encoding proinflammatory cytokines, including interleukin-1β (IL-1β) and tumor necrotizing factor-α (TNF-α). Additionally, suppression of Toll-like receptor (TLR) activation occurs because HA interacts with Toll-like receptors (TLR-2 and TLR-4) on immune cells, which are frequently upregulated in OA and contribute to inflammation when activated [101]. By binding to these receptors, HA reduces the activation of TLR-mediated pathways that would otherwise trigger the production of inflammatory cytokines [102]. Another element is reducing reactive oxygen species (ROS), as HA exhibits antioxidant activity and thus modulates inflammation. By scavenging reactive oxygen species, HA reduces oxidative stress, which can otherwise activate inflammatory signaling pathways, including those that stimulate the release of IL-1β and TNF-α. HA also interacts with synovial membrane cells and chondrocytes, reducing cell sensitivity to proinflammatory cytokines by downregulating cytokine receptor expression on the cell surface, such as IL-1β and TNF-α [103,104].
HA’s role in promoting chondroprotection is critical for preventing and managing OA. HA stimulates the synthesis of endogenous hyaluronic acid and proteoglycans by chondrocytes, contributing to the maintenance and repair of the cartilage matrix [105,106]. This function of HA demonstrates its potential to protect and preserve the integrity of the cartilage matrix, which is a crucial aspect of OA management. This process contributes to the cartilage matrix’s maintenance, integrity, and repair. The activation of CD44 receptors on chondrocytes plays a significant role in this mechanism. Exogenous HA binds to CD44 receptors on the surface of chondrocytes, triggering intracellular signaling pathways that promote anabolic processes in these cells. CD44 is the primary receptor for HA in chondrocytes [107]. The binding of HA to CD44 activates the mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) signaling pathway, which is associated with increased chondrocyte proliferation and enhanced synthesis of ECM components [98,108]. The ERK pathway plays a crucial role in regulating the gene expression of matrix proteins, such as aggrecan and type II collagen. TGF-β signaling is enhanced under the influence of administered HA, which increases the activity of transforming growth factor beta (TGF-β) receptors on chondrocytes. TGF-β is an essential cytokine for cartilage health and stimulates the production of matrix components through the Smad signaling pathway, contributing to the maintenance and repair of the ECM. HA’s interaction with chondrocytes also reduces the expression of catabolic enzymes, such as matrix metalloproteinases (MMPs) and aggrecanase, which degrade ECM components in OA [109,110].
HA plays a protective role against chondrocyte apoptosis by modulating cell survival pathways, including the phosphoinositide three kinase (PI3K)/Akt pathway. HA interacts with cell surface receptors such as CD44 and RHAMM, activating the PI3K/Akt signaling pathway, a critical regulator of cell survival and apoptosis [98]. This activation leads to Akt phosphorylation, inhibiting pro-apoptotic signals by inactivating proteins like Bad, caspase-9, and Forkhead transcription factors (FOXO) [111]. Akt activation promotes cell survival by upregulating anti-apoptotic proteins, such as Bcl-2 and Bcl-xL, maintaining mitochondrial integrity and preventing cytochrome c release. HA can reduce oxidative stress in chondrocytes by enhancing the expression of antioxidant enzymes via the PI3K/Akt pathway [112]. Additionally, HA maintains the extracellular matrix (ECM), providing a supportive environment for chondrocytes. A well-maintained ECM can signal through integrins and other receptors to activate survival pathways, including PI3K/Akt [98].
HA acts as an antioxidant, scavenger of reactive oxygen species, and protects cartilage from oxidative stress-induced damage. This antioxidant function is crucial because ROS such as superoxide anions (O2−), hydroxyl radicals (OH-), and hydrogen peroxide (H2O2) accumulate in OA joints and contribute to cartilage degradation, inflammation, and chondrocyte apoptosis. HA’s ability to reduce oxidative stress provides a sense of security regarding its potential to protect cartilage from damage caused by OA [113].
The molecular mechanisms of antioxidant activity include direct uptake of ROS, inhibition of oxidative enzyme activity, regulation of antioxidant enzymes in chondrocytes, protection of cell membranes and DNA, reduction in ROS-mediated inflammatory signaling, and protection against apoptosis and aging [114]. The molecular structure of hyaluronic acid allows it to interact directly with ROS [115]. Hydroxyl groups (-OH) on HA can donate electrons to ROS, neutralize them, reduce their oxidative potential, and minimize oxidative stress on chondrocytes and the extracellular matrix (ECM) in cartilage. HA can inhibit the activity of enzymes, such as NADPH oxidase and xanthine oxidase, which generate ROS in response to inflammatory stimuli in the joint. By decreasing the activity of these enzymes, HA reduces ROS production at the cellular level, thereby reducing oxidative stress in the cartilage environment [116]. HA also stimulates intracellular signaling pathways that regulate antioxidant enzymes (mediated by CD44 binding). This interaction increases the activity and expression of antioxidant enzymes such as superoxide dismutase (SOD), catalase, and glutathione peroxidase in chondrocytes [117]. These enzymes play a key role in converting ROS into less harmful molecules, thereby protecting the cells from oxidative damage. ROS uptake by HA helps to protect chondrocyte cell membranes from lipid peroxidation, a destructive process in which ROS oxidizes lipids in cell membranes [103]. HA maintains the membrane integrity by preventing lipid peroxidation, which is essential for chondrocyte function. HA also reduces ROS-induced DNA damage, preserves genetic material in chondrocytes, and prevents apoptosis and mutations that could impair cartilage regeneration [112,118].
By scavenging ROS, HA indirectly reduces the activation of redox-sensitive inflammatory signaling pathways such as NF-κB and MAPK. ROS acts as secondary messengers in these pathways, promoting the expression of proinflammatory cytokines and matrix-degrading enzymes [103]. Chronic oxidative stress can induce chondrocyte apoptosis (cell death) and senescence (aging), processes that contribute to cartilage degeneration [19,119]. HA also interacts with pain receptors in the joint, attenuating nociceptive signaling and relieving pain. HA modulates pain in OA through several molecular mechanisms that affect nociceptive (pain) signaling in the joints. By interacting with specific pain receptors, particularly transient receptor vanilloid potential 1 (TRPV1) and acid-sensing ion channels (ASICs), and modulating inflammatory pathways, HA helps alleviate joint pain associated with OA [120,121]. These receptors are sensitive to changes in pH and inflammatory mediators, and their activation contributes to pain sensation. HA in the joint cavity creates a protective barrier around these receptors, reducing their exposure to inflammatory mediators and acidic byproducts generated by OA. HA has been shown to reduce the release of substance P, a neuropeptide involved in pain transmission and inflammation [122]. Substance P is released from nerve endings in response to joint damage and inflammation, sensitizing pain receptors and promoting the production of inflammatory cytokines [123]. The anti-inflammatory effects also include a reduction in the production of prostaglandin E2 (PGE2), a lipid mediator that sensitizes pain-sensing neurons (nociceptors) in response to inflammation [124]. HA can reduce the action of nerve growth factor (NGF), a protein involved in pain signaling and nociceptor sensitization. NGF levels are typically elevated in patients with OA and contribute to increased pain perception by increasing pain receptor sensitivity. Restoration of the joint viscoelastic properties of HA reduces the mechanical stress on the pain receptors in the joint [1].
The anti-inflammatory effect of hyaluronic acid also contributes to pain modulation by reducing the activation of redox-sensitive pain signaling pathways such as NF-κB and MAPK. In OA, these pathways are upregulated, increasing the production of proinflammatory cytokines and pain mediators that enhance nociceptive signaling. Thus, HA directly and indirectly modulates pain receptors, reduces the production of pain mediators, and improves the joint environment, collectively leading to reduced pain in patients with OA [125].
The binding of HA to CD44 activates the MAPK/ERK pathway for cell proliferation and matrix synthesis, which promotes chondrocyte proliferation and synthesis of ECM components, such as proteoglycans and collagen, by increasing the expression of matrix protein genes, thereby promoting anabolic processes necessary for cartilage maintenance and repair [108]. HA-CD44 binding also activates the phosphoinositide kinase 3 (PI3K)/Akt signaling pathway, which promotes cell survival and inhibits programmed cell death (apoptosis) [98,108]. The binding of HA to RHAMM and CD44 can activate the GTPase signaling Rho pathway, which regulates the cytoskeleton and is critical for chondrocyte and synoviocyte migration and repositioning within the joint, facilitating repair processes and helping cells migrate to areas of tissue damage [34,126].
HA may contribute to the maintenance of subchondral bone integrity by affecting the activity of osteoblasts and osteoclasts [127]. The molecular mechanisms underlying HA’s protective effects of HA on subchondral bone include interaction with osteoblast receptors to increase bone formation, inhibition of osteoclastogenesis through modulation of the RANKL/OPG pathway, reduction in inflammatory mediators affecting bone cells, modulation of Wnt/β-catenin signaling for bone remodeling, enhancement of osteoblast matrix production and mineralization, reduction in oxidative stress in bone cells, and support of angiogenesis [128,129,130]. HA, by binding to CD44 receptors on osteoblasts, activates signaling pathways that promote osteoblast proliferation, differentiation, and activity, such as the MAPK/ERK pathway, which is involved in osteoblast function and bone matrix production and inhibition of osteoclastogenesis through modulation of the RANKL/OPG pathway [131,132].
HA can affect the receptor activator of nuclear factor-kappa B ligand (RANKL)/osteoprotegerin (OPG) balance. RANKL promotes osteoclast formation and bone resorption, whereas OPG acts as a decoy receptor for RANKL and inhibits osteoclastogenesis [133]. The anti-inflammatory effect of HA on subchondral bone is achieved by reducing the levels of proinflammatory cytokines such as TNF-α and IL-1β, which stimulate osteoclast activity and inhibit osteoblast function [134].
The Wnt/β-catenin signaling pathway is central to regulating osteoblast activity and bone formation, which is Wnt/β-Catenin signaling for bone remodeling [135]. The activation of this pathway promotes osteoblast differentiation and reduces bone resorption.
In addition, the presence of HA in the joint environment promotes osteoblasts’ production of matrix proteins, including collagen and non-collagen proteins. It improves mineralization, bone density, and strength in the subchondral region [136].
HA can act as a scavenger of ROS, protecting osteoblasts from oxidative stress. HA preserves osteoblast function and reduces osteoclast-induced bone degradation, promoting healthy subchondral bone maintenance. HA also plays a role in supporting angiogenesis in the subchondral bone layer [137].
HA promotes balanced osteoblast and osteoclast activity through these mechanisms, thereby protecting subchondral bone from excessive degradation and abnormal remodeling associated with OA. This effect not only preserves the integrity of the bone but also indirectly protects the underlying cartilage, keeping the subchondral bone stable and resilient, reducing mechanical stress on the cartilage, and improving joint function.
HA is a long-chain GAG composed of repeating disaccharide units that provide a strong and flexible structure for binding multiple aggregate molecules [138]. A small molecule known as a linking protein facilitates the connection between HA and aggrecan, stabilizing their bond and creating a strong and durable connection [93].
The aggrecan molecule has a core protein densely decorated with GAG side chains, mainly chondroitin sulfate and keratan sulfate. GAG chains have a high negative charge, attract water molecules, and create an osmotic environment that increases complex hydration [93].
HA–aggrecan complexes interact with water to form a gel-like structure that fills the cartilage’s ECM [84,86]. The gel-like matrix imparts unique viscoelastic properties to the cartilage, allowing it to compress and rebound. The high hydration level promotes the diffusion of nutrients to chondrocytes embedded in the cartilage, supporting their survival and function.
Highly hydrated HA–aggrecan complexes resist compression by generating internal swelling pressure. The negatively charged GAG chains on aggrecan repel each other and resist compression because of their electrostatic interactions. This allows the cartilage to absorb impact and protect the underlying bone, providing joint stability and shock absorption during movement [93,94,96].
By binding aggrecan to stable complexes, HA helps protect aggrecan from enzymatic degradation. This is owing to the effects of enzymes typical of osteoarthritis, such as aggrecanases and matrix metalloproteinases (MMPs), which are elevated and degrade ECM components, including aggrecan [139].
The stability of the HA–aggrecan complex reduces the likelihood of cleavage and release of aggrecan from the ECM, thus preserving the cartilage matrix structure and function [140]. Large HA–aggrecan complexes evenly distribute mechanical loads in the cartilage. Forming a uniform and resilient matrix, these complexes help maintain the smooth cartilage surface necessary for efficient joint movement and reduce the local stress concentrations leading to cartilage wear. Together, these molecular mechanisms contribute to the therapeutic effect of HA delivery in treating osteoarthritis.
Over the past two decades, IAHA VS [39,41,43,44,68,141,142,143,144,145,146,147,148] has been widely adopted in clinical practice because it provides symptomatic relief and improves patients’ quality of life. The effectiveness of IAHA in treating osteoarthritis is confirmed by its dual role in the mechanical and biological processes occurring in the joint (Table 1) [149,150,151,152,153,154,155]. Mechanically, IAHAs replenish the loss of synovial fluid, thereby improving lubrication and shock absorption [34,43,105,152,155,156]. Biologically, IAHA exerts anti-inflammatory effects, modulates the local immune response [157,158], and stimulates endogenous HA production [43,159], contributing to joint homeostasis [7,43,60,160].

Table 1.
Summary of HA’s molecular mechanisms in OA.
Considering the chronic nature of OA and the limitations of current treatments, IAHA VS is a valuable addition to the therapeutic armamentarium, especially for patients who do not respond adequately to first-line therapy. However, the efficacy of IAHA varies with its molecular weight, disease severity, and individual patient characteristics.
Studies are ongoing to refine the use of IAHA in clinical practice [33,35,38,161]. Numerous studies have investigated the efficacy of IAHA injections in OA treatment [33,40,44,55,56,63,149,162]. IAHA has provided symptomatic relief [45,50,54,55,65,142,149,163,164,165,166,167] and improved joint function [33,39,54,60,144,148,166,168] in many patients. The benefits of using HA vary between studies. Despite several debates regarding its effectiveness compared with other treatments, IAHA remains a widely used and essential option in nonsurgical OA management [33,34,35,68,169,170,171].
Because IAHA has become a routine method, the availability of new studies has decreased. The management of IAHA injections for OA is debated in the medical community.
Clinicians must navigate biological factors such as patient adherence, resource availability, and decisions regarding HA formulations (Table 2).

Table 2.
Comparison of HA formulations used in IAHA for OA treatment.
A critical consideration is choosing between low- and ultra-high-molecular-weight (UHMW) HA, which is influenced by patient characteristics, healthcare access, cost, and resource constraints. In resource-limited settings, clinicians may favor low-molecular-weight (LMW) HA owing to its lower cost and easier availability. UHMW HA may be preferred for patients with advanced OA requiring longer-lasting symptom relief, though it may be more expensive and less accessible [172,173].
Adherence to HA treatment protocols is critical. Some patients may discontinue treatment because of unmet expectations or perceived ineffectiveness, especially if they are unaware of the need for repeated injections. Educating patients about HA’s expected outcomes and the role of HA in managing OA symptoms is essential for improving adherence. Clinicians must make decisions based on resource availability because not all patients can access UHMW HA formulations, which are often more costly and may require specialized administration techniques [173]. Despite decades of use, the debate continues regarding its efficacy, safety, and administration protocols. HA injections mimic the viscoelastic properties of synovial fluid, improve joint lubrication, and modulate inflammatory responses [16,34,105,155]. However, discrepancies existed in the study’s outcomes. Randomized controlled trials have shown that some patients do not respond adequately to oral NSAIDs or physical therapy [33]. A network meta-analysis indicated that specific HA formulations may offer superior outcomes compared to placebo or other injectables such as corticosteroids [174]. Critical analysis revealed heterogeneity in patient selection, HA molecular weight, injection regimens, follow-up duration, and outcome measures, complicating the consensus on the effectiveness of HA.
Some studies have suggested that HA has superior results depending on the design and formulation [175]. Higher-molecular-weight HA preparations may offer substantial benefits for pain relief and functional improvement [160]. Despite over three decades of use [34], controversy persists regarding dosing schedules, preparation types, combination therapies, and safety concerns [33]. Advances have highlighted HA’s lubricating properties and biological activities of HA, which influence articular cartilage physiology [16,152,176]. HA shows potential disease-modifying effects by promoting extracellular matrix preservation/restoration, downregulating proinflammatory factors, and providing antinociceptive effects [32,105]. Studies have reinforced HA’s role in improving pain and joint function in knee OA (KOA) patients. HA injections significantly improved WOMAC pain and function scores compared to placebo at the monthly follow-up [174]. Patients receiving HA injections experience a significant reduction in pain and mobility, particularly in the early stages [177]. However, no significant difference in pain relief between HA and saline injections over 12 months has been reported [178], challenging HA’s universal effectiveness and suggesting its benefits may be more pronounced in certain patient subgroups or depending on specific HA formulations. These findings suggest HA may be particularly beneficial when incorporated early in treatment regimens as part of a comprehensive strategy to delay surgical interventions. HA-based hydrogel scaffolds have promising applications beyond joint diseases [179], specifically stem cell transplantation, highlighting HA’s versatility of HA but not providing direct evidence for its efficacy in traditional intra-articular injection contexts. HA hydrogels interact with immune cells, potentially impacting regenerative medicine applications, but do not directly translate to enhanced efficacy in conventional OA treatments [180].
Despite numerous studies investigating IAHA effects on joint conditions with varying patient populations, evidence quality remains mixed owing to methodological inconsistencies across trials. The heterogeneity among clinical trials complicates the establishment of definitive conclusions regarding HA’s role of HA in multimodal treatment regimens. Although it demonstrates potential as part of a comprehensive treatment strategy for OA through joint lubrication and possible cartilage health promotion [64,181,182], its standalone effectiveness remains controversial [183]. Clinical practice has shifted towards individualized patient care plans incorporating pharmacological and non-pharmacological interventions [184]. Future research should focus on elucidating optimal combinations of HA properties and establishing therapies to maximize patient outcomes.
3.4. Consideration of HA Formulations
Hyaluronans are the basic, non-cross-linked forms of hyaluronic acid, often derived from bacterial fermentation or animal sources, and vary primarily in molecular weight. Hylans, on the other hand, are chemically cross-linked variants of hyaluronic acid that offer increased viscosity and potentially longer intra-articular residence times compared to standard hyaluronans [185], and HYADD®4 compounds represent a further chemically modified class of hyaluronic acid, designed to improve viscoelastic properties, enhance biological activity, and optimize joint retention for more sustained therapeutic effects [186].
Low-molecular-weight (LMW) HA (<1 MDa) typically exhibits lower viscosity, providing less mechanical cushioning and shorter intra-articular residence times, which can lead to quicker clearance from the joint; in some cases, LMW fragments may be proinflammatory, though this varies by product and formulation. In contrast, high molecular weight (HMW) HA (~1–3 MDa) generally features higher viscosity, offering more robust mechanical protection and forming a thicker “coating” on cartilage surfaces; it also tends to remain in the joint longer, potentially yielding extended symptom relief and more pronounced anti-inflammatory effects by stabilizing the extracellular matrix and synovial environment.
The choice of LMW HA or UHMW HA is crucial when deciding on treatment. Studies have indicated that UHMW HA provides long-lasting pain relief and requires fewer injections, ideal for patients seeking longer intervals between treatments. LMW HA formulations are thought to have fewer immediate adverse effects and lower upfront costs, although they require frequent administration [60,100]. Clinicians must consider the clinical characteristics and practical factors, such as costs and patient access to follow-up care. Although clinical evidence supports the efficacy of both formulations, individualized treatment that suits patients’ financial and logistical situations is crucial.
The table (Table 3) summarizes several products that contain hyaluronic acid (HA). However, actual values may vary depending on the manufacturer’s formulas, newer research results, and updated labels.

Table 3.
Summary of several hyaluronic acid (HA) products.
In the table, molecular weight (MW) refers to the products from lower MW to cross-linked/high MW (“hylans”), each affecting viscosity and potential biological effects. Retention time indicates how long the injected material is expected to remain active in the joint, although individual patient factors (e.g., metabolism and activity level) can also influence this time. The application regimen can include weekly injections for several weeks; however, single-injection (one-shot) options are also available.
3.5. Inconsistencies in the Literature
The inconsistencies in HA VS efficacy may stem from variations in study design, patient populations, and HA formulations. Differences in molecular weight, cross-linking, and the number of injections significantly influenced the outcomes. UHMW HA formulations have shown more sustained pain relief than low-molecular-weight formulations. However, not all studies have accounted for these variations, leading to mixed results. Patient selection criteria vary widely across studies. Some trials included patients with mild OA, whereas others focused on more severe cases, influencing the overall effectiveness of HA. HA may be more effective in early-stage OA, where synovial fluid is less degraded, and the joint environment is more responsive to VS [198]. Total knee replacement (TKR) may be delayed in KOA patients with more HA courses [61].
The quality of evidence supporting HA use is mixed, ranging from moderate to low certainty across studies, questioning its role as a first-line treatment for contemporary OA. Given the current evidence landscape, indicating both HA’s potential benefits and limitations, clinicians may consider integrating newer therapies with traditional options rather than relying solely on HA VS.
UHMW HA is recommended for pain relief and functional improvement, particularly in moderate-to-severe OA [21,22,160]. Although individual studies of AHA show promising results, the overall landscape is characterized by variability in study design, patient demographics, dosing regimens, and follow-up periods. This inconsistency makes it difficult to establish HA as the definitive treatment for KOA and other joint disorders. Future studies should standardize the methodology and improve the study designs to obtain more reliable comparisons and conclusions regarding HA efficacy [199,200,201]. Rigorous trials with larger sample sizes and consistent outcome measures are essential to advance our understanding of IAHA therapies.
3.6. The Need for Standardized Protocols in HA Research
In assessing the role of IAHA in knee osteoarthritis management, a critical analysis revealed significant inconsistencies across various studies regarding its efficacy and application [202].
Chavda et al.’s [33] systematic review provided a comprehensive overview of IAHA’s safety and effectiveness. It concluded that IAHA can offer symptomatic relief for up to six months, with efficacy depending on the molecular weight and formulation type [33]. Combining IAHA with other treatments may enhance outcomes; however, further research is required. Most clinical practice guidelines (CPG) favor using IAHA as second-line therapy after conservative measures, contingent on individual patient profiles and responses to initial treatments [203]. A network meta-analysis of 137 studies ranked IAHA among interventions with modest efficacy but lacked long-term data [204].
Long-term pain control is associated with pharmacological treatments for OA beyond 12 months, highlighting the need for robust evidence before establishing IAHA as a standard treatment [205].
Although the literature supports IAHA use in OA management under specific conditions, substantial variability in clinical outcomes based on product formulation and injection protocols remains. Studies support IAHA as a viable treatment for patients who do not achieve adequate symptom relief from conservative measures [33,203]. However, many experts urge caution due to inconsistent evidence on its efficacy compared to other interventions [205,206,207]. The heterogeneity across trials complicates efforts to establish standardized protocols for their use.
There is an urgent need for well-designed RCTs with standardized methodologies to better delineate the role of IAHA within OA management strategies, particularly given the increasing interest in alternative therapies, which appear promising based on recent analyses [44,207,208,209].
3.7. Comparative Efficacy and Clinical Implications
When comparing LMW and UHMW HA formulations, evidence suggests that UHMW HA may offer longer-lasting symptom relief and require fewer injections, enhancing patient compliance and quality of life. LMW HA may be more suitable for patients who are sensitive to injection-related discomfort or those in the early OA stages. Despite the fact that both formulations were found to be clinically effective, UHMW HA showed superior pain reduction and functional improvement at six- and twelve-month follow-ups [179]. The choice between LMW and UHMW HA should be individualized based on patient-specific factors, including disease severity, comorbidities, treatment goals, and injection tolerance [210]. UHMW HAs, such as Hylan G-F 20 [35,67,167,211] are preferred for advanced OA because of their long-lasting effects and excellent joint lubrication properties. These formulations are recommended for patients requiring less frequent injections and seeking long-term relief. UHMW HA is often considered more effective in providing sustained pain relief and improving joint function [42].
Systematic reviews and meta-analyses over the past two decades have consistently demonstrated the superior efficacy of UHMW HA over LMW HA in managing OA. UHMW HA provided significant pain relief and functional improvement lasting up to six months [33]. In multiple studies [191], UHMW HA consistently yielded better pain reduction than LMW HA and revealed significant differences in clinical outcomes based on the molecular weight and source of HA used in the treatment protocols.
Among the injectable treatments for OA, only UHMW HA surpassed the minimal clinically essential difference thresholds for pain relief and functional improvement [212]. This underscores the importance of selecting appropriate HA formulations based on their molecular weight. As noted by Aggarwal and Sempowski [193], UHMW HA is considered more effective than LMW formulations in improving pain and function in patients with OA.
A systematic review of HOA supports the idea that UHMW HA provides superior outcomes without increased adverse effects compared to other molecular weights [173]. High-molecular-weight HAs are preferred over low-molecular-weight variants for KOA management because of their better efficacy in reducing pain and improving function while being cost-effective compared to traditional therapies. Although some studies suggest limited benefits of postsurgical HA injections [163], the evidence favors their use as a conservative treatment before surgery. Systematic reviews and meta-analyses have shown that UHMW HA is more practical for managing OA symptoms [67,203,212]. Indications and patient selection are crucial. HA administration is generally recommended for patients with mild-to-moderate OA, particularly KOA, who do not respond adequately to first-line treatment. IAHA mainly benefits patients who want to delay or avoid surgery such as total knee arthroplasty (TKA) [22]. LMW HA is often preferred in patients requiring frequent injections because of its short half-life and is typically administered in three to five weekly injections. Clinical benefits can last several months; however, repeated cycles are often necessary [147]. UHMW HA has a longer duration of action and is used in patients who require fewer injections. These formulations have better viscoelastic properties, potentially resulting in more significant and longer-lasting symptom relief [165,213]. Some patients may respond better to LMW HA, suggesting individualized treatment plans are needed [42]. Both are generally safe, with the most common side effects being local injection-site reactions. UHMW HA formulations have a slightly higher incidence of side effects, possibly because of the more viscous nature of the product [22]. Shared decision-making between medical specialists and patients is essential for optimal treatment outcomes.
Evidence from clinical trials has shown that HA injections lead to significantly better outcomes than placebo or nonsteroidal anti-inflammatory drugs (NSAIDs). The current literature supports HA’s efficacy in treating OA symptoms and suggests its potential disease-modifying effects (Table 4), but clinical practice guidelines remain inconsistent [30]. HA is considered as a second-line option owing to its safety profile and potential to delay the need for TKA.

Table 4.
Summary of clinical study outcomes for IAHA in osteoarthritis.
Individualized care and tailored treatment approaches considering disease severity, patient age, activity level, and prior treatment response remain essential for optimizing outcomes.
Implications for clinical practice include incorporating IAHA VS into treatment regimens for moderate to severe OA, which may significantly benefit patients. Clinicians should consider patient-specific factors, including disease severity, prior treatment response, and individual health profiles when implementing IAHA [210,214,215].
Acknowledging the current review limitations is essential to ensuring the accurate interpretation and generality of findings regarding IAHA in OA. The limitations include significant heterogeneity in design, sample size, follow-up duration, outcome measures, and patient population, making direct comparisons difficult. Variability in HA administration protocols further complicates the efficacy assessment. The inclusion criteria often varied, introducing a potential bias. The placebo effect and short follow-up may limit understanding of its long-term benefits. Although short-term benefits are well documented, the lack of long-term data beyond two years remains a fundamental limitation. Future research should focus on standardizing treatment protocols, investigating cost-effectiveness in preventing surgical intervention, and evaluating combination therapies involving HA and other treatments, such as platelet-rich plasma (PRP), to enhance patient outcomes [200,216]. Further studies addressing these issues will help resolve inconsistencies in clinical practice guidelines and improve the standardization of HA treatment protocols, leading to more reliable patient outcomes.
Current research on IAHA(HA) therapy faces limitations due to variability in study design and outcomes across conditions such as knee OA. Inconsistency in patient populations, treatment protocols, and follow-up durations hinders firm conclusions regarding the efficacy of HA. Costa et al. found that platelet-rich plasma (PRP) may offer pain relief similar to HA, but the evidence quality was low owing to study bias [199]. Garcia et al. [200] reported no significant difference in pain reduction between PRP and HA groups. These inconsistencies highlight the need for standardized research methodologies to evaluate the clinical benefits of HA. Xavier et al. [217] noted that innovative treatments like exosome-laden scaffolds face challenges such as rapid clearance rates and inconsistent dosing regimens. Cui et al. [218] found that patients receiving HA injections had a higher risk of knee arthroplasty than those receiving corticosteroids. Chen et al. [219] explored traditional Chinese medicine (TCM) as an alternative to HA for OA management, but clinical heterogeneity complicated direct result comparisons.
Research on newer therapies, such as adipose-derived stem cell therapy, has shown promise. However, Kim et al.’s [201] review noted inconclusive evidence due to the variability in the study methodology. Riley et al. [220] concluded that no injection-based therapies for base-of-thumb osteoarthritis, including HA, demonstrated superiority over placebo, emphasizing the need for more high-quality randomized controlled trials.
3.8. Future Directions
Further research is needed to optimize IAHA treatment protocols to enhance outcomes for specific patient populations, particularly when exploring combination therapies such as IAHA with PRP. Refining the patient selection criteria will also ensure that IAHA is used effectively by those most likely to benefit from it.
Future research should focus on larger, more diverse populations with standardized treatment protocols, extended follow-up periods, and consistent and objective outcome measures [50,202,203,221,222,223,224]. Comparative studies are also needed to assess HA’s relative effectiveness and cost-effectiveness compared with alternative treatments. Studies should examine the effects of different molecular weights and formulations on outcomes and the interaction between HA and other conservative treatments, such as physical therapy or new pharmacological agents.
The therapeutic usefulness of IAHA can be optimized toward precision medicine by tailoring treatment to individual patient phenotypes, such as OA with inflammation dominance, mechanical overload, or post-traumatic OA. Incorporating biomarkers, imaging characteristics, and disease stages into treatment decisions could guide the choice of molecular weight, formulation type, and injection schedule. Such a stratified approach holds promise for maximizing clinical outcomes and advancing IAHA toward a precision medicine model for the treatment of osteoarthritis.
4. Conclusions
Intra-articular hyaluronic acid (IAHA) represents a versatile and evolving therapy for osteoarthritis, combining mechanical relief with biological modulation. Future directions include exploring personalized treatments based on patient-specific factors to enhance therapeutic outcomes. IAHA is a versatile therapeutic option for OA, offering symptomatic relief and potential disease-modifying benefits. Its multifaceted mechanisms, including anti-inflammatory, chondroprotective, and pain-modulating effects, underscore its role in personalized OA management. Stage-specific applications based on molecular weights and biomarker-driven approaches have advanced precision medicine. This review analyzes the efficacy, safety, and clinical use of IAHA for treating OA. Results indicate that IAHA effectively reduces pain and improves joint function in OA, particularly in the knees. IAHA injections provide significant short- and medium-term pain relief and improved function. Although data beyond two years are limited, repeated treatments have shown durable benefits in several studies. Long-term studies are necessary to confirm these findings. HMW HA formulations offer superior symptom relief and longer-lasting effects than low-molecular-weight formulations. Future studies should optimize the treatment protocols and identify ideal HA formulations for patient profiles. IAHA remains a safe treatment option, with a low incidence of adverse events, primarily local injection site reactions. The minimal occurrence of systemic adverse events underscores a favorable safety profile compared to alternative treatments. IAHA remains viable due to its established safety, ease of administration, and patient satisfaction. Comparative studies are required to assess the long-term efficacy and cost-effectiveness of IAHA compared with newer treatments. Future research should focus on long-term efficacy studies, direct comparisons between IAHA and other treatments, and studies that optimize dosing schedules and explore personalized treatment protocols. IAHA remains integral to osteoarthritis treatment, particularly for patients seeking nonsurgical options. Its efficacy and safety profile support its continued use, although future studies are necessary to elucidate its role in new therapies and optimize treatment regimens for different patient populations.
IAHA is a multifaceted, relatively safe, and patient-friendly treatment that offers meaningful pain relief and improved function, particularly in knee osteoarthritis.
Higher-molecular-weight formulations may provide superior, longer-lasting benefits, yet further research is needed to optimize dosing regimens and compare IAHA’s long-term efficacy with emerging alternatives.
Personalizing IAHA therapy based on patient-specific biomarkers and disease characteristics ultimately enhances outcomes and solidifies its role in nonsurgical osteoarthritis management.
Key Takeaways for Clinicians:
IAHA is a well-tolerated, multifaceted therapy offering symptomatic relief and potential disease-modifying effects via anti-inflammatory, antioxidant, and chondroprotective mechanisms.
Molecular weight matters: Low-molecular-weight (LMW) HA is best suited for early-stage OA and resource-limited settings. Ultra-high-molecular-weight (UHMW) HA demonstrates longer-lasting symptom relief and may benefit patients with advanced OA.
Personalized treatment strategies based on OA phenotypes, disease stage, and patient-specific biomarkers can improve therapeutic outcomes.
Adherence to injection protocols and patient education on expected outcomes are essential to maximizing IAHA’s clinical benefits.
IAHA should be considered in multimodal treatment strategies, particularly for patients aiming to delay or avoid surgical intervention like total joint arthroplasty.
Author Contributions
Conceptualization, W.G.; Methodology, W.G., W.T. and D.Ś.; Validation, W.G. and W.T.; Formal analysis, W.G. and D.Ś.; Investigation, W.G., D.Ś., W.T. and Pol-IAHA Study Group; Resources, W.G. and W.T.; Data curation, W.G.; Writing—original draft preparation, W.G.; Writing—review and editing, W.G., D.Ś. and W.T.; Visualization, W.G.; Supervision, W.G., D.Ś. and W.T.; Project administration, W.G. and W.T.; funding acquisition, W.G. and W.T. All authors have read and agreed to the published version of the manuscript.
Funding
This study did not receive external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created for this study.
Acknowledgments
We would like to acknowledge the engagement in the study of our colleagues—collaborators from the Pol-IAHA Study Group (in alphabetic order): Dariusz Boguszewski (Department of Individual Sports. University of Physical Education in Warsaw, Poland); Ewa Brzeziańska-Lasota (Department of Biomedicine and Genetics, Medical University of Lodz, Poland); Leszek Kulej (First Airlift Base in Warsaw, Poland and Military Institute of Medicine-National Research Institute, Department of Traumatology and Orthopedics, Warsaw, Poland); Anna Ostrowska (Department of Rehabilitation, The Jozef Pilsudski University of Physical Education, Warsaw, Poland); Jakub Szewczyk (ZOZ UMAMED, Rehabilitation Clinic, Gorlice, Poland); Jan Szypuła (Department of Orthopaedic Surgery, Luxmed Hospital, Warsaw, Poland).
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| ADL | Activities of Daily Living |
| ASICs | Acid-Sensing Ion Channels |
| CPG | Clinical Practice Guidelines |
| ECM | Extracellular Matrix |
| ERK | Extracellular Signal-Regulated Kinase |
| GAG | Glycosaminoglycan |
| HA | Hyaluronic Acid |
| HAS1 | Hyaluronan Synthase 1 |
| HMW | High Molecular Weight |
| HOA | Hip Osteoarthritis |
| IAHA | Intra-Articular Hyaluronic Acid |
| IL-1β | Interleukin One Beta |
| KOA | Knee Osteoarthritis |
| LMW | Low Molecular Weight |
| MAPK | Mitogen-Activated Protein Kinase |
| MMPs | Matrix Metalloproteinases |
| NADP | Nicotinamide Adenine Dinucleotide Phosphate |
| NF-κB | Nuclear Factor Kappa-Light-Chain-Enhancer |
| OA | Osteoarthritis |
| OPG | Osteoprotegerin |
| PCM | Pericellular Matrix |
| PGE2 | Prostaglandin E2 |
| PI3K | Phosphoinositide Three Kinase |
| RCT | Randomized Clinical Trial |
| RHAMM | Receptor for Hyaluronan-Mediated Motility |
| RANKL | Receptor Activator of Nuclear Factor Kappa-B Ligand |
| ROS | Reactive Oxygen Species |
| TGF-β | Transforming Growth Factor Beta |
| TKA | Total Knee Arthroplasty |
| TKA | Total Knee Replacement |
| TLR | Toll-Like Receptor |
| TNF-α | Tumor Necrosis Factor Alpha |
| TRPV1 | Transient Receptor Vanilloid Potential 1 |
| UDP | Uridine Diphosphate |
| UDP-GlcUA | UDP-α-D-Glucuronate |
| UHMW | Ultra High Molecular Weight |
| VS | Viscosupplementation |
| WHO | World Health Organization |
References
- Yao, Q.; Wu, X.; Tao, C.; Gong, W.; Chen, M.; Qu, M.; Zhong, Y.; He, T.; Chen, S.; Xiao, G. Osteoarthritis: Pathogenic signaling pathways and therapeutic targets. Signal Transduct. Target. Ther. 2023, 8, 56. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, J.D.; Culbreth, G.T.; Haile, L.M.; Rafferty, Q.; Lo, J.; Fukutaki, K.G. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef] [PubMed]
- Turkiewicz, A. Epidemiology of Osteoarthritis in Sweden. In Register and Cohort Studies on Prevalence and Mortality; Lund University: Lund, Sweden, 2016. [Google Scholar]
- Johnson, V.L.; Hunter, D.J. The epidemiology of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2014, 28, 5–15. [Google Scholar] [CrossRef]
- Hannon, C.P.; Delanois, R.E.; Nandi, S.; Fillingham, Y.; Management of Osteoarthritis of the Hip Work Group. American Academy of Orthopaedic Surgeons Clinical Practice Guideline Summary Management of Osteoarthritis of the Hip. JAAOS J. Am. Acad. Orthop. Surg. 2022, 32, e1027–e1034. [Google Scholar] [CrossRef]
- Tong, L.; Yu, H.; Huang, X.; Shen, J.; Xiao, G.; Chen, L.; Wang, H.; Xing, L.; Chen, D. Current understanding of osteoarthritis pathogenesis and relevant new approaches. Bone Res. 2022, 10, 60. [Google Scholar] [CrossRef]
- Batushansky, A.; Zhu, S.; Komaravolu, R.K.; South, S.; Mehta-D’souza, P.; Griffin, T.M. Fundamentals of OA. An initiative of Osteoarthritis and Cartilage. Obesity and metabolic factors in OA. Osteoarthr. Cartil. 2022, 30, 501–515. [Google Scholar] [CrossRef]
- Lv, Z.; Shi, D. Molecule-Based osteoarthritis diagnosis comes of age. Ann. Transl. Med. 2021, 9, 1112. [Google Scholar] [CrossRef] [PubMed]
- Oral, A.; Arman, S.; Tarakci, E.; Patrini, M.; Arienti, C.; Etemadi, Y.; Rauch, A.; Negrini, S. A systematic review of clinical practice guidelines for persons with osteoarthritis. A “Best Evidence for Rehabilitation” (be4rehab) paper to develop the WHO’s Package of Interventions for Rehabilitation: A systematic review of Clinical Practice Guidelines for persons with osteoarthritis for the identification of best evidence for rehabilitation. Int. J. Rheum. Dis. 2022, 25, 383–393. [Google Scholar] [CrossRef]
- Lohmander, L.S. What can we do about osteoarthritis? Arthritis Res. 2000, 2, 95–100. [Google Scholar] [CrossRef][Green Version]
- Peat, G.; Thomas, M.J. Osteoarthritis year in review 2020: Epidemiology & therapy. Osteoarthr. Cartil. 2021, 29, 180–189. [Google Scholar] [CrossRef]
- Sethi, V.; Anand, C.; Della Pasqua, O. Clinical Assessment of Osteoarthritis Pain: Contemporary Scenario, Challenges, and Future Perspectives. Pain Ther. 2024, 13, 391–408. [Google Scholar] [CrossRef]
- Eyles, J.P.; Sharma, S.; Telles, R.W.; Namane, M.; Hunter, D.J.; Bowden, J.L. Implementation of Best-Evidence Osteoarthritis Care: Perspectives on Challenges for, and Opportunities From, Low and Middle-Income Countries. Front. Rehabil. Sci. 2021, 2, 826765. [Google Scholar] [CrossRef]
- Hochberg, M.C. Osteoarthritis: The Rheumatologist’s Perspective. HSS J. 2012, 8, 35–36. [Google Scholar] [CrossRef]
- Zaki, S.; Blaker, C.L.; Little, C.B. OA foundations—Experimental models of osteoarthritis. Osteoarthr. Cartil. 2022, 30, 357–380. [Google Scholar] [CrossRef]
- Li, Y.; Yuan, Z.; Yang, H.; Zhong, H.; Peng, W.; Xie, R. Recent Advances in Understanding the Role of Cartilage Lubrication in Osteoarthritis. Molecules 2021, 26, 6122. [Google Scholar] [CrossRef] [PubMed]
- Samvelyan, H.J.; Hughes, D.; Stevens, C.; Staines, K.A. Models of Osteoarthritis: Relevance and New Insights. Calcif. Tissue Int. 2021, 109, 243–256. [Google Scholar] [CrossRef]
- Chen, D.; Shen, J.; Zhao, W.; Wang, T.; Han, L.; Hamilton, J.L.; Im, H.J. Osteoarthritis: Toward a comprehensive understanding of pathological mechanism. Bone Res. 2017, 5, 16044. [Google Scholar] [CrossRef]
- Loeser, R.F. The Role of Aging in the Development of Osteoarthritis. Trans. Am. Clin. Climatol. Assoc. 2017, 128, 44–54. [Google Scholar]
- Snochowska, A.; Szmigielska, P.; Brzeziańska-Lasota, E.; Tomaszewski, W. Genetic and Epigenetic Interactions in the Etiopathogenesis of Osteoarthritis. Selected Molecular Factors in OA Etiopathogenesis. Ortop. Traumatol. Rehabil. 2017, 19, 227–237. [Google Scholar] [CrossRef]
- Arden, N.K.; Perry, T.A.; Bannuru, R.R.; Bruyere, O.; Cooper, C.; Haugen, I.K.; Hochberg, M.C.; McAlindon, T.E.; Mobasheri, A.; Reginster, J.Y. Non-Surgical management of knee osteoarthritis: Comparison of ESCEO and OARSI 2019 guidelines. Nat. Rev. Rheumatol. 2021, 17, 59–66. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef]
- Berenbaum, F. Deep phenotyping of osteoarthritis: A step forward. Ann. Rheum. Dis. 2019, 78, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Young, D.A.; Barter, M.J.; Soul, J. Osteoarthritis year in review: Genetics, genomics, epigenetics. Osteoarthr. Cartil. 2022, 30, 216–225. [Google Scholar] [CrossRef]
- Henrotin, Y. Osteoarthritis in year 2021: Biochemical markers. Osteoarthr. Cartil. 2022, 30, 237–248. [Google Scholar]
- Marshall, M.; Watt, F.E.; Vincent, T.L.; Dziedzic, K. Hand osteoarthritis: Clinical phenotypes, molecular mechanisms and disease management. Nat. Rev. Rheumatol. 2018, 14, 641–656. [Google Scholar] [PubMed]
- Bragantini, A.; Molinaroli, F. A pilot clinical evaluation of the treatment of hip osteoarthritis with hyaluronic acid. Curr. Ther. Res. 1994, 55, 319–330. [Google Scholar]
- Balazs, E.A.; Denlinger, J.L. Viscosupplementation: A new concept in the treatment of osteoarthritis. J. Rheumatol. 1993, 20 (Suppl. S39), 3–9. [Google Scholar]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. 2020, 72, 149–162. [Google Scholar]
- Glinkowski, W.M.; Tomaszewski, W. Intra-Articular Hyaluronic Acid for Knee Osteoarthritis: A Systematic Umbrella Review. J. Clin. Med. 2025, 14, 1272. [Google Scholar] [CrossRef]
- Abatangelo, G.; Vindigni, V.; Avruscio, G.; Pandis, L.; Brun, P. Hyaluronic Acid: Redefining Its Role. Cells 2020, 9, 1743. [Google Scholar] [CrossRef]
- Kotla, N.G.; Bonam, S.R.; Rasala, S.; Wankar, J.; Bohara, R.A.; Bayry, J.; Rochev, Y.; Pandit, A. Recent advances and prospects of hyaluronan as a multifunctional therapeutic system. J. Control. Release 2021, 336, 598–620. [Google Scholar] [CrossRef]
- Chavda, S.; Rabbani, S.A.; Wadhwa, T. Role and Effectiveness of Intra-articular Injection of Hyaluronic Acid in the Treatment of Knee Osteoarthritis: A Systematic Review. Cureus 2022, 14, e24503. [Google Scholar] [CrossRef]
- Gupta, R.C.; Lall, R.; Srivastava, A.; Sinha, A. Hyaluronic Acid: Molecular Mechanisms and Therapeutic Trajectory. Front. Vet. Sci. 2019, 6, 192. [Google Scholar] [CrossRef] [PubMed]
- Peck, J.; Slovek, A.; Miro, P.; Vij, N.; Traube, B.; Lee, C.; Berger, A.A.; Kassem, H.; Kaye, A.D.; Sherman, W.F.; et al. A Comprehensive Review of Viscosupplementation in Osteoarthritis of the Knee. Orthop. Rev. 2021, 13, 25549. [Google Scholar] [CrossRef] [PubMed]
- Fakhari, A.; Berkland, C. Applications and emerging trends of hyaluronic acid in tissue engineering, as a dermal filler and in osteoarthritis treatment. Acta Biomater. 2013, 9, 7081–7092. [Google Scholar] [CrossRef]
- Tomaszewski, W. Availability of Hyaluronic Acids and Their Indications. Ortop. Traumatol. Rehabil. 2015, 17, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, W. Is the use of STABHA™ for supplementation of damaged extracellular matrix of soft tissues in the musculoskeletal system an effective treatment of acute injuries and tendinopathies? Ortop. Traumatol. Rehabil. 2015, 17, 99–104. [Google Scholar] [CrossRef][Green Version]
- Bellamy, N.; Campbell, J.; Robinson, V.; Gee, T.; Bourne, R.; Wells, G. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst. Rev. 2005, 2005, Cd005321. [Google Scholar] [CrossRef]
- Migliore, A.; Granata, M.; Tormenta, S.; Laganà, B.; Piscitelli, P.; Bizzi, E.; Massafra, U.; Alimonti, A.; Maggi, C.; De Chiara, R.; et al. Hip viscosupplementation under ultra-sound guidance riduces NSAID consumption in symptomatic hip osteoarthritis patients in a long follow-up. Data from Italian registry. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 25–34. [Google Scholar]
- Jevsevar, D.; Donnelly, P.; Brown, G.A.; Cummins, D.S. Viscosupplementation for Osteoarthritis of the Knee: A Systematic Review of the Evidence. J. Bone Jt. Surg. Am. 2015, 97, 2047–2060. [Google Scholar] [CrossRef]
- Altman, R.D.; Bedi, A.; Karlsson, J.; Sancheti, P.; Schemitsch, E. Product Differences in Intra-articular Hyaluronic Acids for Osteoarthritis of the Knee. Am. J. Sports Med. 2016, 44, 2158–2165. [Google Scholar] [CrossRef] [PubMed]
- Maheu, E.; Rannou, F.; Reginster, J.Y. Efficacy and safety of hyaluronic acid in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Semin. Arthritis Rheum. 2016, 45 (Suppl. S4), S28–S33. [Google Scholar] [CrossRef]
- Cooper, C.; Rannou, F.; Richette, P.; Bruyère, O.; Al-Daghri, N.; Altman, R.D.; Brandi, M.L.; Collaud Basset, S.; Herrero-Beaumont, G.; Migliore, A.; et al. Use of Intraarticular Hyaluronic Acid in the Management of Knee Osteoarthritis in Clinical Practice. Arthritis Care Res. 2017, 69, 1287–1296. [Google Scholar] [CrossRef]
- Vincent, P. Intra-Articular Hyaluronic Acid in the Symptomatic Treatment of Knee Osteoarthritis: A Meta-Analysis of Single-Injection Products. Curr. Ther. Res. Clin. Exp. 2019, 90, 39–51. [Google Scholar] [CrossRef]
- Bernetti, A.; Agostini, F.; Alviti, F.; Giordan, N.; Martella, F.; Santilli, V.; Paoloni, M.; Mangone, M. New Viscoelastic Hydrogel Hymovis MO.RE. Single Intra-articular Injection for the Treatment of Knee Osteoarthritis in Sportsmen: Safety and Efficacy Study Results. Front. Pharmacol. 2021, 12, 673988. [Google Scholar] [CrossRef]
- Zhao, D.; Pan, J.K.; Yang, W.Y.; Han, Y.H.; Zeng, L.F.; Liang, G.H.; Liu, J. Intra-Articular Injections of Platelet-Rich Plasma, Adipose Mesenchymal Stem Cells, and Bone Marrow Mesenchymal Stem Cells Associated with Better Outcomes Than Hyaluronic Acid and Saline in Knee Osteoarthritis: A Systematic Review and Network Meta-analysis. Arthroscopy 2021, 37, 2298–2314.e10. [Google Scholar] [CrossRef] [PubMed]
- Micu, M.C.; Micu, A.; Bolboacă, S.D. Ultrasound-Guided injection with hyaluronic acid in hip osteoarthritis: Efficacy and safety in a real-life setting. Clin. Rheumatol. 2022, 41, 2491–2498. [Google Scholar] [CrossRef]
- Familiari, F.; Ammendolia, A.; Rupp, M.C.; Russo, R.; Pujia, A.; Montalcini, T.; Marotta, N.; Mercurio, M.; Galasso, O.; Millett, P.J.; et al. Efficacy of intra-articular injections of hyaluronic acid in patients with glenohumeral joint osteoarthritis: A systematic review and meta-analysis. J. Orthop. Res. 2023, 41, 2345–2358. [Google Scholar] [CrossRef]
- Nicholas, E.; Cheng, J.; Moley, P.J. Non-Operative Treatment Options for Osteoarthritis in the Hip. HSS J. 2023, 19, 486–493. [Google Scholar] [CrossRef]
- Conrozier, T.; Diracoglu, D.; Monfort, J.; Chevalier, X.; Bard, H.; Baron, D.; Jerosch, J.; Migliore, A.; Richette, P.; Henrotin, Y. EUROVISCO Good Practice Recommendations for a First Viscosupplementation in Patients with Knee Osteoarthritis. Cartilage 2023, 14, 125–135. [Google Scholar] [CrossRef]
- Materkowski, M.; Malinowska, K.; Tomaszewski, W. Practical Aspects of Hyaluronic Acid Application in Biolevox HA Preparations—Report on Research. Ortop. Traumatol. Rehabil. 2018, 20, 431–435. [Google Scholar] [CrossRef]
- Qvistgaard, E.; Christensen, R.; Torp-Pedersen, S.; Bliddal, H. Intra-Articular treatment of hip osteoarthritis: A randomized trial of hyaluronic acid, corticosteroid, and isotonic saline. Osteoarthr. Cartil. 2006, 14, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.F.; Chou, Y.J.; Hsu, C.W.; Hwang, C.W.; Hsu, P.T.; Wang, J.L.; Hsu, Y.W.; Chou, M.C. Efficacy of intra-articular hyaluronic acid in patients with osteoarthritis of the ankle: A prospective study. Osteoarthr. Cartil. 2006, 14, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Chapelle, C. Intra-Articular injections. Rev. Med. Brux 2015, 36, 281–287. [Google Scholar] [PubMed]
- Dıraçoğlu, D.; Tunçay, T.B.; Şahbaz, T.; Aksoy, C. Single versus multiple dose hyaluronic acid: Comparison of the results. J. Back Musculoskelet. Rehabil. 2016, 29, 881–886. [Google Scholar] [CrossRef]
- Billesberger, L.M.; Fisher, K.M.; Qadri, Y.J.; Boortz-Marx, R.L. Procedural Treatments for Knee Osteoarthritis: A Review of Current Injectable Therapies. Pain Res. Manag. 2020, 2020, 3873098. [Google Scholar] [CrossRef]
- Xu, Z.; He, Z.; Shu, L.; Li, X.; Ma, M.; Ye, C. Intra-Articular Platelet-Rich Plasma Combined with Hyaluronic Acid Injection for Knee Osteoarthritis Is Superior to Platelet-Rich Plasma or Hyaluronic Acid Alone in Inhibiting Inflammation and Improving Pain and Function. Arthroscopy 2021, 37, 903–915. [Google Scholar] [CrossRef]
- La Gatta, A.; Stellavato, A.; Vassallo, V.; Di Meo, C.; Toro, G.; Iolascon, G.; Schiraldi, C. Hyaluronan and Derivatives: An In Vitro Multilevel Assessment of Their Potential in Viscosupplementation. Polymers 2021, 13, 3208. [Google Scholar] [CrossRef]
- Fusco, G.; Gambaro, F.M.; Di Matteo, B.; Kon, E. Injections in the osteoarthritic knee: A review of current treatment options. EFORT Open Rev. 2021, 6, 501–509. [Google Scholar] [CrossRef]
- Uson, J.; Rodriguez-García, S.C.; Castellanos-Moreira, R.; O’Neill, T.W.; Doherty, M.; Boesen, M.; Pandit, H.; Möller Parera, I.; Vardanyan, V.; Terslev, L.; et al. EULAR recommendations for intra-articular therapies. Ann. Rheum. Dis. 2021, 80, 1299–1305. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Turchetta, M.; Giardina, S.M.C.; Culmone, A.; Testa, G. Injection-Based Management of Osteoarthritis of the Knee: A Systematic Review of Guidelines. Front. Pharmacol. 2021, 12, 661805. [Google Scholar] [CrossRef]
- Poliwoda, S.; Noor, N.; Mousa, B.; Sarwary, Z.; Noss, B.; Urits, I.; Viswanath, O.; Behara, R.; Ulicny, K.; Howe, A.; et al. A comprehensive review of intraarticular knee injection therapy, geniculate injections, and peripheral nerve stimulation for knee pain in clinical practice. Orthop. Rev. 2022, 14, 38676. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, H.; He, F.; Zhu, X. Intra-Articular injection choice for osteoarthritis: Making sense of cell source—An updated systematic review and dual network meta-analysis. Arthritis Res. Ther. 2022, 24, 260. [Google Scholar] [CrossRef] [PubMed]
- Khalid, S.; Ali, A.; Deepak, F.; Zulfiqar, M.S.; Malik, L.U.; Fouzan, Z.; Nasr, R.A.; Qamar, M.; Bhattarai, P. Comparative effectiveness of intra-articular therapies in knee osteoarthritis: A meta-analysis comparing platelet-rich plasma (PRP) with other treatment modalities. Ann. Med. Surg. 2024, 86, 361–372. [Google Scholar] [CrossRef]
- Makris, E.A.; Gomoll, A.H.; Malizos, K.N.; Hu, J.C.; Athanasiou, K.A. Repair and tissue engineering techniques for articular cartilage. Nat. Rev. Rheumatol. 2015, 11, 21–34. [Google Scholar] [CrossRef]
- Ranawat, A.; Guo, K.; Phillips, M.; Guo, A.; Niazi, F.; Bhandari, M.; Waterman, B. Health Economic Assessments of Hyaluronic Acid Treatments for Knee Osteoarthritis: A Systematic Review. Adv. Ther. 2023, 41, 65–81. [Google Scholar] [CrossRef]
- van den Bekerom, M.P.; Rys, B.; Mulier, M. Viscosupplementation in the hip: Evaluation of hyaluronic acid formulations. Arch. Orthop. Trauma Surg. 2008, 128, 275–280. [Google Scholar] [CrossRef]
- Donell, S. Subchondral bone remodelling in osteoarthritis. EFORT Open Rev. 2019, 4, 221–229. [Google Scholar] [CrossRef]
- Ong, K.L.; Runa, M.; Lau, E.; Altman, R. Is Intra-Articular Injection of Synvisc Associated with a Delay to Knee Arthroplasty in Patients with Knee Osteoarthritis? Cartilage 2019, 10, 423–431. [Google Scholar] [CrossRef]
- Tomaszewski, W. Osteoarthritis—How to Treat to Slow its Progress. Ortop. Traumatol. Rehabil. 2016, 18, 91–97. [Google Scholar] [CrossRef]
- Valachová, K.; Hassan, M.E.; Šoltés, L. Hyaluronan: Sources, Structure, Features and Applications. Molecules 2024, 29, 739. [Google Scholar] [CrossRef]
- Meyer, K.; Palmer, J.W. The polysaccharide of the vitreous humor. J. Biol. Chem. 1934, 107, 629–634. [Google Scholar] [CrossRef]
- Necas, J.; Bartosikova, L.; Brauner, P.; Kolar, J. Hyaluronic acid (hyaluronan): A review. Vet. Med. 2008, 53, 397–411. [Google Scholar] [CrossRef]
- Prehm, P. Hyaluronate is synthesized at plasma membranes. Biochem. J. 1984, 220, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Prehm, P. Release of hyaluronate from eukaryotic cells. Biochem. J. 1983, 211, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Itano, N.; Kimata, K. Mammalian hyaluronan synthases. IUBMB Life 2002, 54, 195–199. [Google Scholar] [CrossRef]
- Kultti, A.; Makkonen, K.M.; Saavalainen, K.; Jauhiainen, M.; Hölttä, E.; Tammi, M.I.; Pirttilä, T. 2-Deoxyglucose inhibits hyaluronan synthesis in keratinocytes. Glycobiology 2009, 19, 537–546. [Google Scholar]
- Kögelberg, M.; Nicholls, J.M.; Conners, R.; Cossins, A.; Jayson, G.C.; Gardiner, J.M. Synthesis of hyaluronan oligosaccharides toward the production of specific molecular weight markers. Chemistry 2007, 13, 659–670. [Google Scholar]
- Spicer, A.P.; Tien, J.Y. Hyaluronan and hyaluronan synthases. Front. Biosci. 2004, 9, 1241–1247. [Google Scholar]
- Itano, N.; Sawai, T.; Yoshida, M.; Lenas, P.; Yamada, Y.; Imagawa, M.; Shinomura, T.; Hamaguchi, M.; Yoshida, Y.; Ohnuki, Y.; et al. Three isoforms of mammalian hyaluronan synthases have distinct enzymatic properties. J. Biol. Chem. 1999, 274, 25085–25092. [Google Scholar] [CrossRef]
- DeAngelis, P.L. Evolution of glycosaminoglycans and their glycosyltransferases: Implications for the extracellular matrices of animals and the capsules of pathogenic bacteria. Anat. Rec. 2002, 268, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Chong, B.F.; Blank, L.M.; McLaughlin, R.; Nielsen, L.K. Microbial hyaluronic acid production. Appl. Microbiol. Biotechnol. 2005, 66, 341–351. [Google Scholar] [CrossRef]
- de Oliveira, J.D.; Carvalho, L.S.; Gomes, A.M.; Queiroz, L.R.; Magalhães, B.S.; Parachin, N.S. Genetic basis for hyper production of hyaluronic acid in natural and engineered microorganisms. Microb. Cell Factories 2016, 15, 119. [Google Scholar] [CrossRef]
- Shyjan, A.M.; Heldin, P.; Butcher, E.C.; Yoshino, T.; Briskin, M.J. Functional cloning of mouse and human hyaluronan synthase. Biochem. Biophys. Res. Commun. 1996, 225, 391–398. [Google Scholar]
- Salih, A.R.C.; Farooqi, H.M.U.; Amin, H.; Karn, P.R.; Meghani, N.; Nagendran, S. Hyaluronic acid: Comprehensive review of a multifunctional biopolymer. Future J. Pharm. Sci. 2024, 10, 63. [Google Scholar] [CrossRef]
- Iaconisi, G.N.; Lunetti, P.; Gallo, N.; Cappello, A.R.; Fiermonte, G.; Dolce, V.; Capobianco, L. Hyaluronic Acid: A Powerful Biomolecule with Wide-Ranging Applications—A Comprehensive Review. Int. J. Mol. Sci. 2023, 24, 10296. [Google Scholar] [CrossRef] [PubMed]
- Iaconisi, G.N.; Gallo, N.; Caforio, L.; Ricci, V.; Fiermonte, G.; Della Tommasa, S.; Bernetti, A.; Dolce, V.; Farì, G.; Capobianco, L. Clinical and Biochemical Implications of Hyaluronic Acid in Musculoskeletal Rehabilitation: A Comprehensive Review. J. Pers. Med. 2023, 13, 1647. [Google Scholar] [CrossRef] [PubMed]
- Menezes, R.; Vincent, R.; Osorno, L.; Hu, P.; Arinzeh, T.L. Biomaterials and tissue engineering approaches using glycosaminoglycans for tissue repair: Lessons learned from the native extracellular matrix. Acta Biomater. 2023, 163, 210–227. [Google Scholar] [CrossRef]
- Gilbert, S.J.; Bonnet, C.S.; Blain, E.J. Mechanical Cues: Bidirectional Reciprocity in the Extracellular Matrix Drives Mechano-Signalling in Articular Cartilage. Int. J. Mol. Sci. 2021, 22, 13595. [Google Scholar] [CrossRef]
- Perez, S.; Makshakova, O.; Angulo, J.; Bedini, E.; Bisio, A.; de Paz, J.L.; Fadda, E.; Guerrini, M.; Hricovini, M.; Hricovini, M.; et al. Glycosaminoglycans: What Remains to Be Deciphered? JACS Au 2023, 3, 628–656. [Google Scholar] [CrossRef]
- Horkay, F.; Douglas, J.F.; Raghavan, S.R. Rheological Properties of Cartilage Glycosaminoglycans and Proteoglycans. Macromolecules 2021, 54, 2316–2324. [Google Scholar] [CrossRef]
- Hayes, A.J.; Melrose, J. Aggrecan, the Primary Weight-Bearing Cartilage Proteoglycan, Has Context-Dependent, Cell-Directive Properties in Embryonic Development and Neurogenesis: Aggrecan Glycan Side Chain Modifications Convey Interactive Biodiversity. Biomolecules 2020, 10, 1244. [Google Scholar] [CrossRef]
- Eschweiler, J.; Horn, N.; Rath, B.; Betsch, M.; Baroncini, A.; Tingart, M.; Migliorini, F. The Biomechanics of Cartilage—An Overview. Life 2021, 11, 302. [Google Scholar] [CrossRef] [PubMed]
- Roughley, P.J.; Mort, J.S. The role of aggrecan in normal and osteoarthritic cartilage. J. Exp. Orthop. 2014, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Hashemi-Afzal, F.; Fallahi, H.; Bagheri, F.; Collins, M.N.; Eslaminejad, M.B.; Seitz, H. Advancements in hydrogel design for articular cartilage regeneration: A comprehensive review. Bioact. Mater. 2025, 43, 1–31. [Google Scholar] [CrossRef]
- Al-Sharif, A.; Jamal, M.; Zhang, L.X.; Larson, K.; Schmidt, T.A.; Jay, G.D.; Elsaid, K.A. Lubricin/Proteoglycan 4 Binding to CD44 Receptor: A Mechanism of the Suppression of Proinflammatory Cytokine-Induced Synoviocyte Proliferation by Lubricin. Arthritis Rheumatol. 2015, 67, 1503–1513. [Google Scholar] [CrossRef]
- Misra, S.; Hascall, V.C.; Markwald, R.R.; Ghatak, S. Interactions between Hyaluronan and Its Receptors (CD44, RHAMM) Regulate the Activities of Inflammation and Cancer. Front. Immunol. 2015, 6, 201. [Google Scholar] [CrossRef]
- Mirzaei, S.; Zarrabi, A.; Hashemi, F.; Zabolian, A.; Saleki, H.; Ranjbar, A.; Seyed Saleh, S.H.; Bagherian, M.; Sharifzadeh, S.O.; Hushmandi, K.; et al. Regulation of Nuclear Factor-KappaB (NF-κB) signaling pathway by non-coding RNAs in cancer: Inhibiting or promoting carcinogenesis? Cancer Lett. 2021, 509, 63–80. [Google Scholar] [CrossRef]
- Jayab, N.A.; Abed, A.; Talaat, I.M.; Hamoudi, R. The molecular mechanism of NF-κB dysregulation across different subtypes of renal cell carcinoma. J. Adv. Res. 2024; in press. [Google Scholar] [CrossRef]
- Guo, Q.; Jin, Y.; Chen, X.; Ye, X.; Shen, X.; Lin, M.; Zeng, C.; Zhou, T.; Zhang, J. NF-κB in biology and targeted therapy: New insights and translational implications. Signal Transduct. Target. Ther. 2024, 9, 53. [Google Scholar] [CrossRef]
- Leifer, C.A.; Medvedev, A.E. Molecular mechanisms of regulation of Toll-like receptor signaling. J. Leukoc. Biol. 2016, 100, 927–941. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Han, X.; Zhang, T.; Tian, K.; Li, Z.; Luo, F. Reactive oxygen species (ROS) scavenging biomaterials for anti-inflammatory diseases: From mechanism to therapy. J. Hematol. Oncol. 2023, 16, 116. [Google Scholar] [CrossRef]
- Hong, Y.; Boiti, A.; Vallone, D.; Foulkes, N.S. Reactive Oxygen Species Signaling and Oxidative Stress: Transcriptional Regulation and Evolution. Antioxidants 2024, 13, 312. [Google Scholar] [CrossRef] [PubMed]
- Sprott, H.; Fleck, C. Hyaluronic Acid in Rheumatology. Pharmaceutics 2023, 15, 2247. [Google Scholar] [CrossRef]
- Deng, S.; Cao, H.; Lu, Y.; Shi, W.; Chen, M.; Cui, X.; Liang, J.; Fan, Y.; Wang, Q.; Zhang, X. Injectable dECM-enhanced hyaluronic microgels with spatiotemporal release of cartilage-specific molecules to improve osteoarthritic chondrocyte’s function. Collagen Leather 2024, 6, 14. [Google Scholar] [CrossRef]
- Michelacci, Y.M.; Baccarin, R.Y.A.; Rodrigues, N.N.P. Chondrocyte Homeostasis and Differentiation: Transcriptional Control and Signaling in Healthy and Osteoarthritic Conditions. Life 2023, 13, 1460. [Google Scholar] [CrossRef]
- Tavianatou, A.G.; Caon, I.; Franchi, M.; Piperigkou, Z.; Galesso, D.; Karamanos, N.K. Hyaluronan: Molecular size-dependent signaling and biological functions in inflammation and cancer. FEBS J. 2019, 286, 2883–2908. [Google Scholar] [CrossRef]
- Li, T.F.; O’Keefe, R.J.; Chen, D. TGF-beta signaling in chondrocytes. Front. Biosci. 2005, 10, 681–688. [Google Scholar] [CrossRef]
- Du, X.; Cai, L.; Xie, J.; Zhou, X. The role of TGF-beta3 in cartilage development and osteoarthritis. Bone Res. 2023, 11, 2. [Google Scholar] [CrossRef]
- He, X.; Li, Y.; Deng, B.; Lin, A.; Zhang, G.; Ma, M.; Wang, Y.; Yang, Y.; Kang, X. The PI3K/AKT signalling pathway in inflammation, cell death and glial scar formation after traumatic spinal cord injury: Mechanisms and therapeutic opportunities. Cell Prolif. 2022, 55, e13275. [Google Scholar] [CrossRef]
- Lepetsos, P.; Papavassiliou, A.G. ROS/oxidative stress signaling in osteoarthritis. Biochim. Biophys. Acta (BBA) Mol. Basis Dis. 2016, 1862, 576–591. [Google Scholar] [CrossRef]
- Pizzino, G.; Irrera, N.; Cucinotta, M.; Pallio, G.; Mannino, F.; Arcoraci, V.; Squadrito, F.; Altavilla, D.; Bitto, A. Oxidative Stress: Harms and Benefits for Human Health. Oxidative Med. Cell. Longev. 2017, 2017, 8416763. [Google Scholar] [CrossRef] [PubMed]
- Mucha, P.; Skoczyńska, A.; Małecka, M.; Hikisz, P.; Budzisz, E. Overview of the Antioxidant and Anti-Inflammatory Activities of Selected Plant Compounds and Their Metal Ions Complexes. Molecules 2021, 26, 4886. [Google Scholar] [CrossRef] [PubMed]
- Berdiaki, A.; Neagu, M.; Spyridaki, I.; Kuskov, A.; Perez, S.; Nikitovic, D. Hyaluronan and Reactive Oxygen Species Signaling-Novel Cues from the Matrix? Antioxidants 2023, 12, 824. [Google Scholar] [CrossRef]
- He, F.; Wu, H.; He, B.; Han, Z.; Chen, J.; Huang, L. Antioxidant hydrogels for the treatment of osteoarthritis: Mechanisms and recent advances. Front. Pharmacol. 2024, 15, 1488036. [Google Scholar] [CrossRef]
- Katarina, B.; Jarmila, K.; Silvester, P.; Lukas, S.; Karol, S.; Vladimir, J.; Jana, M. The Role of Endogenous Antioxidants in the Treatment of Experimental Arthritis. In Antioxidants; Emad, S., Ed.; IntechOpen: Rijeka, Croatia, 2019; p. Ch. 8. [Google Scholar]
- Zheng, L.; Zhang, Z.; Sheng, P.; Mobasheri, A. The role of metabolism in chondrocyte dysfunction and the progression of osteoarthritis. Ageing Res. Rev. 2021, 66, 101249. [Google Scholar] [CrossRef]
- Loeser, R.F. Aging and osteoarthritis: The role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthr. Cartil. 2009, 17, 971–979. [Google Scholar] [CrossRef]
- Jayakar, S.; Shim, J.; Jo, S.; Bean, B.P.; Singeç, I.; Woolf, C.J. Developing nociceptor-selective treatments for acute and chronic pain. Sci. Transl. Med. 2021, 13, eabj9837. [Google Scholar] [CrossRef] [PubMed]
- Mickle, A.D.; Shepherd, A.J.; Mohapatra, D.P. Nociceptive TRP Channels: Sensory Detectors and Transducers in Multiple Pain Pathologies. Pharmaceuticals 2016, 9, 72. [Google Scholar] [CrossRef]
- Kurenkova, A.D.; Timashev, P.S. Mast cells: A dark horse in osteoarthritis treatment. AIMS Allergy Immunol. 2022, 6, 228–247. [Google Scholar] [CrossRef]
- Li, F.X.; Xu, F.; Lin, X.; Wu, F.; Zhong, J.Y.; Wang, Y.; Guo, B.; Zheng, M.H.; Shan, S.K.; Yuan, L.Q. The Role of Substance P in the Regulation of Bone and Cartilage Metabolic Activity. Front. Endocrinol. 2020, 11, 77. [Google Scholar] [CrossRef] [PubMed]
- Gambari, L.; Cellamare, A.; Grassi, F.; Grigolo, B.; Panciera, A.; Ruffilli, A.; Faldini, C.; Desando, G. Overview of Anti-Inflammatory and Anti-Nociceptive Effects of Polyphenols to Halt Osteoarthritis: From Preclinical Studies to New Clinical Insights. Int. J. Mol. Sci. 2022, 23, 15861. [Google Scholar] [CrossRef] [PubMed]
- Kuppa, S.S.; Kang, J.Y.; Yang, H.Y.; Lee, S.C.; Sankaranarayanan, J.; Kim, H.K.; Seon, J.K. Hyaluronic Acid Viscosupplement Modulates Inflammatory Mediators in Chondrocyte and Macrophage Coculture via MAPK and NF-κB Signaling Pathways. ACS Omega 2024, 9, 21467–21483. [Google Scholar] [CrossRef]
- Yang, J.; Wang, L.; Zhang, Z.; Sun, Q.; Zhang, Y. Downregulation of HAS-2 regulates the chondrocyte cytoskeleton and induces cartilage degeneration by activating the RhoA/ROCK signaling pathway. Int. J. Mol. Med. 2023, 52, 57. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Chan, Y.T.; Yung, P.S.H.; Tuan, R.S.; Jiang, Y. Subchondral Bone Remodeling: A Therapeutic Target for Osteoarthritis. Front. Cell Dev. Biol. 2020, 8, 607764. [Google Scholar] [CrossRef]
- Chen, W.; Wang, Q.; Tao, H.; Lu, L.; Zhou, J.; Wang, Q.; Huang, W.; Yang, X. Subchondral osteoclasts and osteoarthritis: New insights and potential therapeutic avenues. Acta Biochim. Biophys. Sin. 2024, 56, 499–512. [Google Scholar] [CrossRef]
- Di Cicco, G.; Marzano, E.; Mastrostefano, A.; Pitocco, D.; Castilho, R.S.; Zambelli, R.; Mascio, A.; Greco, T.; Cinelli, V.; Comisi, C.; et al. The Pathogenetic Role of RANK/RANKL/OPG Signaling in Osteoarthritis and Related Targeted Therapies. Biomedicines 2024, 12, 2292. [Google Scholar] [CrossRef]
- Yuan, X.L.; Meng, H.Y.; Wang, Y.C.; Peng, J.; Guo, Q.Y.; Wang, A.Y.; Lu, S.B. Bone–Cartilage interface crosstalk in osteoarthritis: Potential pathways and future therapeutic strategies. Osteoarthr. Cartil. 2014, 22, 1077–1089. [Google Scholar] [CrossRef]
- Amarasekara, D.S.; Kim, S.; Rho, J. Regulation of Osteoblast Differentiation by Cytokine Networks. Int. J. Mol. Sci. 2021, 22, 2851. [Google Scholar] [CrossRef]
- Si, J.; Wang, C.; Zhang, D.; Wang, B.; Zhou, Y. Osteopontin in Bone Metabolism and Bone Diseases. Med. Sci. Monit. 2020, 26, e919159. [Google Scholar] [CrossRef]
- Trouvin, A.P.; Goëb, V. Receptor activator of nuclear factor-κB ligand and osteoprotegerin: Maintaining the balance to prevent bone loss. Clin. Interv. Aging 2010, 5, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Marinho, A.; Nunes, C.; Reis, S. Hyaluronic Acid: A Key Ingredient in the Therapy of Inflammation. Biomolecules 2021, 11, 1518. [Google Scholar] [CrossRef]
- Duan, P.; Bonewald, L.F. The role of the wnt/β-catenin signaling pathway in formation and maintenance of bone and teeth. Int. J. Biochem. Cell Biol. 2016, 77, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.S.; Lee, C.S. Recent Progress in Hyaluronic-Acid-Based Hydrogels for Bone Tissue Engineering. Gels 2023, 9, 588. [Google Scholar] [CrossRef]
- Torre, E. Molecular signaling mechanisms behind polyphenol-induced bone anabolism. Phytochem. Rev. 2017, 16, 1183–1226. [Google Scholar] [CrossRef]
- Miller, T.; Goude, M.C.; McDevitt, T.C.; Temenoff, J.S. Molecular engineering of glycosaminoglycan chemistry for biomolecule delivery. Acta Biomater. 2014, 10, 1705–1719. [Google Scholar] [CrossRef]
- Pérez-García, S.; Carrión, M.; Gutiérrez-Cañas, I.; Villanueva-Romero, R.; Castro, D.; Martínez, C.; González-Álvaro, I.; Blanco, F.J.; Juarranz, Y.; Gomariz, R.P. Profile of Matrix-Remodeling Proteinases in Osteoarthritis: Impact of Fibronectin. Cells 2020, 9, 40. [Google Scholar]
- Knudson, W.; Ishizuka, S.; Terabe, K.; Askew, E.B.; Knudson, C.B. The pericellular hyaluronan of articular chondrocytes. Matrix Biol. 2019, 78, 32–46. [Google Scholar] [CrossRef]
- Conrozier, T.; Raman, R.; Chevalier, X.; Henrotin, Y.; Monfort, J.; Diracoglu, D.; Bard, H.; Baron, D.; Jerosch, J.; Richette, P.; et al. Viscosupplementation for the treatment of osteoarthritis. The contribution of EUROVISCO group. Ther. Adv. Musculoskelet. Dis. 2021, 13, 1759720X211018605. [Google Scholar] [CrossRef]
- Leite, V.F.; Daud Amadera, J.E.; Buehler, A.M. Viscosupplementation for Hip Osteoarthritis: A Systematic Review and Meta-Analysis of the Efficacy on Pain and Disability, and the Occurrence of Adverse Events. Arch. Phys. Med. Rehabil. 2018, 99, 574–583.e1. [Google Scholar] [CrossRef]
- Santilli, V.; Paoloni, M.; Mangone, M.; Alviti, F.; Bernetti, A. Hyaluronic acid in the management of osteoarthritis: Injection therapies innovations. Clin. Cases Miner. Bone Metab. 2016, 13, 131–134. [Google Scholar] [CrossRef]
- Campbell, K.A.; Erickson, B.J.; Saltzman, B.M.; Mascarenhas, R.; Bach, B.R., Jr.; Cole, B.J.; Verma, N.N. Is Local Viscosupplementation Injection Clinically Superior to Other Therapies in the Treatment of Osteoarthritis of the Knee: A Systematic Review of Overlapping Meta-analyses. Arthroscopy 2015, 31, 2036–2045.e14. [Google Scholar] [CrossRef]
- Lubowitz, J.H. Editorial Commentary: Knee Hyaluronic Acid Viscosupplementation Reduces Osteoarthritis Pain. Arthroscopy 2015, 31, 2046. [Google Scholar] [CrossRef]
- Evaniew, N.; Hanson, B.; Winemaker, M. Viscosupplementation for knee osteoarthritis: Current evidence and recommendations. J. Long Term Eff. Med. Implant. 2013, 23, 151–159. [Google Scholar] [CrossRef][Green Version]
- Rutjes, A.W.; Juni, P.; da Costa, B.R.; Trelle, S.; Nuesch, E.; Reichenbach, S. Viscosupplementation for osteoarthritis of the knee: A systematic review and meta-analysis. Ann. Intern. Med. 2012, 157, 180–191. [Google Scholar] [CrossRef]
- Bellamy, N.; Campbell, J.; Robinson, V.; Gee, T.; Bourne, R.; Wells, G. Viscosupplementation for the treatment of osteoarthritis of the knee. Cochrane Database Syst. Rev. 2006, 2006, Cd005321. [Google Scholar] [CrossRef]
- Lu, K.H.; Lu, P.W.; Lin, C.W.; Lu, E.W.; Yang, S.F. Different molecular weights of hyaluronan research in knee osteoarthritis: A state-of-the-art review. Matrix Biol. 2023, 117, 46–71. [Google Scholar] [CrossRef]
- Rezuş, E.; Burlui, A.; Cardoneanu, A.; Macovei, L.A.; Tamba, B.I.; Rezuş, C. From Pathogenesis to Therapy in Knee Osteoarthritis: Bench-to-Bedside. Int. J. Mol. Sci. 2021, 22, 2697. [Google Scholar] [CrossRef] [PubMed]
- Antich, C.; de Vicente, J.; Jiménez, G.; Chocarro, C.; Carrillo, E.; Montañez, E.; Gálvez-Martín, P.; Marchal, J.A. Bio-Inspired hydrogel composed of hyaluronic acid and alginate as a potential bioink for 3D bioprinting of articular cartilage engineering constructs. Acta Biomater. 2020, 106, 114–123. [Google Scholar] [CrossRef]
- Li, C.; Cao, Z.; Li, W.; Liu, R.; Chen, Y.; Song, Y.; Liu, G.; Song, Z.; Liu, Z.; Lu, C.; et al. A review on the wide range applications of hyaluronic acid as a promising rejuvenating biomacromolecule in the treatments of bone related diseases. Int. J. Biol. Macromol. 2020, 165, 1264–1275. [Google Scholar] [CrossRef]
- Li, L.; Yu, F.; Zheng, L.; Wang, R.; Yan, W.; Wang, Z.; Xu, J.; Wu, J.; Shi, D.; Zhu, L.; et al. Natural hydrogels for cartilage regeneration: Modification, preparation and application. J. Orthop. Transl. 2019, 17, 26–41. [Google Scholar] [CrossRef]
- Giubertoni, G.; Burla, F.; Martinez-Torres, C.; Dutta, B.; Pletikapic, G.; Pelan, E.; Rezus, Y.L.A.; Koenderink, G.H.; Bakker, H.J. Molecular Origin of the Elastic State of Aqueous Hyaluronic Acid. J. Phys. Chem. B 2019, 123, 3043–3049. [Google Scholar] [CrossRef]
- Schiavinato, A.; Whiteside, R.A. Effective lubrication of articular cartilage by an amphiphilic hyaluronic acid derivative. Clin. Biomech. 2012, 27, 515–519. [Google Scholar] [CrossRef]
- Abate, M.; Salini, V. Safety and tolerability of intra-articular hyaluronic acid (Sinovial®/GELSYN-3tm) injections in the treatment of knee osteoarthritis. J. Biol. Regul. Homeost. Agents 2017, 31, 1139–1145. [Google Scholar] [PubMed]
- Nagy, N.; Kuipers, H.F.; Marshall, P.L.; Wang, E.; Kaber, G.; Bollyky, P.L. Hyaluronan in immune dysregulation and autoimmune diseases. Matrix Biol. 2019, 78, 292–313. [Google Scholar] [CrossRef]
- Szczęsny, G.; Tomaszewski, W.; Domżalski, M. Evolution of the Hyaluronic Acid in Viscosupplementation—From Linear Particles to Hybrid Complexes. Ortop. Traumatol. Rehabil. 2021, 23, 229–238. [Google Scholar] [CrossRef]
- Sundman, E.A.; Cole, B.J.; Karas, V.; Della Valle, C.; Tetreault, M.W.; Mohammed, H.O.; Fortier, L.A. The anti-inflammatory and matrix restorative mechanisms of platelet-rich plasma in osteoarthritis. Am. J. Sports Med. 2014, 42, 35–41. [Google Scholar] [CrossRef]
- Yu, P.; Li, Y.; Sun, H.; Zhang, H.; Kang, H.; Wang, P.; Xin, Q.; Ding, C.; Xie, J.; Li, J. Mimicking Antioxidases and Hyaluronan Synthase: A Zwitterionic Nanozyme for Photothermal Therapy of Osteoarthritis. Adv. Mater. 2023, 35, e2303299. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef]
- Lamo-Espinosa, J.M.; Mora, G.; Blanco, J.F.; Granero-Molto, F.; Nunez-Cordoba, J.M.; Lopez-Elio, S.; Andreu, E.; Sanchez-Guijo, F.; Aquerreta, J.D.; Bondia, J.M.; et al. Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: Long-term follow up of a multicenter randomized controlled clinical trial (phase I/II). J. Transl. Med. 2018, 16, 213. [Google Scholar] [CrossRef] [PubMed]
- Mao, B.; Pan, Y.; Zhang, Z.; Yu, Z.; Li, J.; Fu, W. Efficacy and Safety of Hyaluronic Acid Intra-articular Injection after Arthroscopic Knee Surgery: A Systematic Review and Meta-analysis. Orthop. Surg. 2023, 15, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Belk, J.W.; Kraeutler, M.J.; Houck, D.A.; Goodrich, J.A.; Dragoo, J.L.; McCarty, E.C. Platelet-Rich Plasma Versus Hyaluronic Acid for Knee Osteoarthritis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 2021, 49, 249–260. [Google Scholar] [CrossRef]
- Concoff, A.; Sancheti, P.; Niazi, F.; Shaw, P.; Rosen, J. The efficacy of multiple versus single hyaluronic acid injections: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2017, 18, 542. [Google Scholar] [CrossRef]
- Bhandari, M.; Bannuru, R.R.; Babins, E.M.; Martel-Pelletier, J.; Khan, M.; Raynauld, J.P.; Frankovich, R.; McLeod, D.; Devji, T.; Phillips, M.; et al. Intra-Articular hyaluronic acid in the treatment of knee osteoarthritis: A Canadian evidence-based perspective. Ther. Adv. Musculoskelet. Dis. 2017, 9, 231–246. [Google Scholar] [CrossRef] [PubMed]
- Petrella, R.J.; Wakeford, C. Pain relief and improved physical function in knee osteoarthritis patients receiving ongoing hylan G-F 20, a high-molecular-weight hyaluronan, versus other treatment options: Data from a large real-world longitudinal cohort in Canada. Drug Des. Dev. Ther. 2015, 9, 5633–5640. [Google Scholar] [CrossRef]
- Abate, M.; Scuccimarra, T.; Vanni, D.; Pantalone, A.; Salini, V. Femoroacetabular impingement: Is hyaluronic acid effective? Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 889–892. [Google Scholar] [CrossRef]
- Papalia, R.; Salini, V.; Voglino, N.; Fortina, M.; Carta, S.; Sadile, F.; Costantino, C. Single-Dose Intra-Articular Administration of a Hybrid Cooperative Complex of Sodium Hyaluronate and Sodium Chondroitin in the Treatment of Symptomatic Hip Osteoarthritis: A Single-Arm, Open-Label, Pilot Study. Rheumatol. Ther. 2021, 8, 151–165. [Google Scholar] [CrossRef]
- Mehl, J.; Imhoff, A.B.; Beitzel, K. Osteoarthritis of the shoulder: Pathogenesis, diagnostics and conservative treatment options. Orthopade 2018, 47, 368–376. [Google Scholar] [CrossRef]
- Conrozier, T. Is the Addition of a Polyol to Hyaluronic Acid a Significant Advance in the Treatment of Osteoarthritis? Curr. Rheumatol. Rev. 2018, 14, 226–230. [Google Scholar] [CrossRef]
- Dasa, V.; DeKoven, M.; Sun, K.; Scott, A.; Lim, S. Clinical and cost outcomes from different hyaluronic acid treatments in patients with knee osteoarthritis: Evidence from a US health plan claims database. Drugs Context 2016, 5, 212296. [Google Scholar] [CrossRef]
- Wu, Y.-Z.; Huang, H.-T.; Ho, C.-J.; Shih, C.-L.; Chen, C.-H.; Cheng, T.-L.; Wang, Y.-C.; Lin, S.-Y. Molecular Weight of Hyaluronic Acid Has Major Influence on Its Efficacy and Safety for Viscosupplementation in Hip Osteoarthritis: A Systematic Review and Meta-Analysis. Cartilage 2021, 13 (Suppl. S1), 169S–184S. [Google Scholar] [CrossRef] [PubMed]
- Anil, U.; Markus, D.H.; Hurley, E.T.; Manjunath, A.K.; Alaia, M.J.; Campbell, K.A.; Jazrawi, L.M.; Strauss, E.J. The efficacy of intra-articular injections in the treatment of knee osteoarthritis: A network meta-analysis of randomized controlled trials. Knee 2021, 32, 173–182. [Google Scholar] [CrossRef]
- Hulsopple, C. Musculoskeletal Therapies: Musculoskeletal Injection Therapy. FP Essent. 2018, 470, 21–26. [Google Scholar] [PubMed]
- Hascall, V.C.; Majors, A.K.; De La Motte, C.A.; Evanko, S.P.; Wang, A.; Drazba, J.A.; Strong, S.A.; Wight, T.N. Intracellular hyaluronan: A new frontier for inflammation? Biochim. Biophys. Acta 2004, 1673, 3–12. [Google Scholar] [CrossRef]
- Sun, Z.P.; Wu, S.P.; Liang, C.D.; Zhao, C.X.; Sun, B.Y. The synovial fluid neuropeptide PACAP may act as a protective factor during disease progression of primary knee osteoarthritis and is increased following hyaluronic acid injection. Innate Immun. 2019, 25, 255–264. [Google Scholar] [CrossRef]
- Jorgensen, A.; Stengaard-Pedersen, K.; Simonsen, O.; Pfeiffer-Jensen, M.; Eriksen, C.; Bliddal, H.; Pedersen, N.W.; Bodtker, S.; Horslev-Petersen, K.; Snerum, L.O.; et al. Intra-articular hyaluronan is without clinical effect in knee osteoarthritis: A multicentre, randomised, placebo-controlled, double-blind study of 337 patients followed for 1 year. Ann. Rheum. Dis. 2010, 69, 1097–1102. [Google Scholar] [CrossRef]
- Yazdani, M.; Shahdadfar, A.; Jackson, C.J.; Utheim, T.P. Hyaluronan-Based Hydrogel Scaffolds for Limbal Stem Cell Transplantation: A Review. Cells 2019, 8, 245. [Google Scholar] [CrossRef]
- Lin, C.; Ekblad-Nordberg, Å.; Michaëlsson, J.; Götherström, C.; Hsu, C.C.; Ye, H.; Johansson, J.; Rising, A.; Sundström, E.; Åkesson, E. In Vitro Study of Human Immune Responses to Hyaluronic Acid Hydrogels, Recombinant Spidroins and Human Neural Progenitor Cells of Relevance to Spinal Cord Injury Repair. Cells 2021, 10, 1713. [Google Scholar] [CrossRef]
- Zhang, W.; Moskowitz, R.W.; Nuki, G.; Abramson, S.; Altman, R.D.; Arden, N.; Bierma-Zeinstra, S.; Brandt, K.D.; Croft, P.; Doherty, M.; et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr. Cartil. 2008, 16, 137–162. [Google Scholar] [CrossRef]
- Zhang, Z.; Huang, C.; Jiang, Q.; Zheng, Y.; Liu, Y.; Liu, S.; Chen, Y.; Mei, Y.; Ding, C.; Chen, M.; et al. Guidelines for the diagnosis and treatment of osteoarthritis in China (2019 edition). Ann. Transl. Med. 2020, 8, 1213. [Google Scholar] [CrossRef]
- Busse, J.W.; Casassus, R.; Carrasco-Labra, A.; Durham, J.; Mock, D.; Zakrzewska, J.M.; Palmer, C.; Samer, C.F.; Coen, M.; Guevremont, B.; et al. Management of chronic pain associated with temporomandibular disorders: A clinical practice guideline. BMJ 2023, 383, e076227. [Google Scholar] [CrossRef] [PubMed]
- Abdulla, A.; Adams, N.; Bone, M.; Elliott, A.M.; Gaffin, J.; Jones, D.; Knaggs, R.; Martin, D.; Sampson, L.; Schofield, P. Guidance on the management of pain in older people. Age Ageing 2013, 42 (Suppl. S1), i1–i57. [Google Scholar] [CrossRef] [PubMed]
- Moreland, L.W. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: Mechanisms of action. Arthritis Res. Ther. 2003, 5, 54–67. [Google Scholar] [CrossRef]
- Mainil-Varlet, P.; Schiavinato, A.; Ganster, M.M. Efficacy Evaluation of a New Hyaluronan Derivative HYADD((R)) 4-G to Maintain Cartilage Integrity in a Rabbit Model of Osteoarthritis. Cartilage 2013, 4, 28–41. [Google Scholar] [CrossRef]
- US Food and Drug Administration. Product Labeling for [Hyalgan] (P950027a). 1997. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/P950027a.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Supartz TM] (P980044c). Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/P980044c.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [GenVisc® 850] (P140005). 2004. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140005d.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Synvisc (Hylan G-F 20)] (PP940015). 1997. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/P940015b.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Orthovisc (High MW HA)] (p030019c). 2004. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf3/p030019c.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Monovisc (Cross-Linked HA)] (P090031B). 2014. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf9/P090031B.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Durolane (Non-Animal Stabilized HA)] (P170007B). 2017. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170007B.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Euflexxa (1% Sodium Hyaluronate)] (P010029S008c). 2004. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/P010029S008c.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [Gelsyn-3 (HA Chemically Modified)] (p110005d). 2014. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf11/p110005d.pdf (accessed on 25 January 2025).
- US Food and Drug Administration. Product Labeling for [VISCO-3 (Sodium Hyaluronate)] (p980044s027d). 2008. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/p980044s027d.pdf (accessed on 25 January 2025).
- HYMOVIS® High Molecular Weight Viscoelastic Hyaluronan. 2024. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150010d.pdf (accessed on 25 January 2025).
- Johansen, M.; Bahrt, H.; Altman, R.D.; Bartels, E.M.; Juhl, C.B.; Bliddal, H.; Lund, H.; Christensen, R. Exploring reasons for the observed inconsistent trial reports on intra-articular injections with hyaluronic acid in the treatment of osteoarthritis: Meta-regression analyses of randomized trials. Semin. Arthritis Rheum. 2016, 46, 34–48. [Google Scholar] [CrossRef]
- Costa, L.A.V.; Lenza, M.; Irrgang, J.J.; Fu, F.H.; Ferretti, M. How Does Platelet-Rich Plasma Compare Clinically to Other Therapies in the Treatment of Knee Osteoarthritis? A Systematic Review and Meta-analysis. Am. J. Sports Med. 2023, 51, 1074–1086. [Google Scholar] [CrossRef] [PubMed]
- Garcia, F.L.; Williams, B.T.; Polce, E.M.; Heller, D.B.; Aman, Z.S.; Nwachukwu, B.U.; Nho, S.J.; Chahla, J. Preparation Methods and Clinical Outcomes of Platelet-Rich Plasma for Intra-articular Hip Disorders: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Orthop. J. Sports Med. 2020, 8, 2325967120960414. [Google Scholar] [CrossRef]
- Kim, K.I.; Kim, M.S.; Kim, J.H. Intra-Articular Injection of Autologous Adipose-Derived Stem Cells or Stromal Vascular Fractions: Are They Effective for Patients with Knee Osteoarthritis? A Systematic Review with Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 2023, 51, 837–848. [Google Scholar] [CrossRef]
- Gibbs, A.J.; Gray, B.; Wallis, J.A.; Taylor, N.F.; Kemp, J.L.; Hunter, D.J.; Barton, C.J. Recommendations for the management of hip and knee osteoarthritis: A systematic review of clinical practice guidelines. Osteoarthr. Cartil. 2023, 31, 1280–1292. [Google Scholar] [CrossRef]
- Phillips, M.; Bhandari, M.; Grant, J.; Bedi, A.; Trojian, T.; Johnson, A.; Schemitsch, E. A Systematic Review of Current Clinical Practice Guidelines on Intra-articular Hyaluronic Acid, Corticosteroid, and Platelet-Rich Plasma Injection for Knee Osteoarthritis: An International Perspective. Orthop. J. Sports Med. 2021, 9, 23259671211030272. [Google Scholar] [CrossRef]
- Bannuru, R.R.; McAlindon, T.E.; Sullivan, M.C.; Wong, J.B.; Kent, D.M.; Schmid, C.H. Effectiveness and Implications of Alternative Placebo Treatments: A Systematic Review and Network Meta-analysis of Osteoarthritis Trials. Ann. Intern. Med. 2015, 163, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Gregori, D.; Giacovelli, G.; Minto, C.; Barbetta, B.; Gualtieri, F.; Azzolina, D.; Vaghi, P.; Rovati, L.C. Association of Pharmacological Treatments with Long-term Pain Control in Patients with Knee Osteoarthritis: A Systematic Review and Meta-analysis. JAMA 2018, 320, 2564–2579. [Google Scholar] [CrossRef] [PubMed]
- Jüni, P.; Hari, R.; Rutjes, A.W.; Fischer, R.; Silletta, M.G.; Reichenbach, S.; da Costa, B.R. Intra-Articular corticosteroid for knee osteoarthritis. Cochrane Database Syst. Rev. 2015, 2015, Cd005328. [Google Scholar] [CrossRef]
- McLarnon, M.; Heron, N. Intra-Articular platelet-rich plasma injections versus intra-articular corticosteroid injections for symptomatic management of knee osteoarthritis: Systematic review and meta-analysis. BMC Musculoskelet. Disord. 2021, 22, 550. [Google Scholar] [CrossRef]
- Singh, H.; Knapik, D.M.; Polce, E.M.; Eikani, C.K.; Bjornstad, A.H.; Gursoy, S.; Perry, A.K.; Westrick, J.C.; Yanke, A.B.; Verma, N.N.; et al. Relative Efficacy of Intra-articular Injections in the Treatment of Knee Osteoarthritis: A Systematic Review and Network Meta-analysis. Am. J. Sports Med. 2022, 50, 3140–3148. [Google Scholar] [CrossRef]
- McAlindon, T.E.; Bannuru, R.R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef]
- Honvo, G.; Reginster, J.Y.; Rannou, F.; Rygaert, X.; Geerinck, A.; Rabenda, V.; McAlindon, T.; Charles, A.; Fuggle, N.; Cooper, C.; et al. Safety of Intra-articular Hyaluronic Acid Injections in Osteoarthritis: Outcomes of a Systematic Review and Meta-Analysis. Drugs Aging 2019, 36 (Suppl. S1), 101–127. [Google Scholar] [CrossRef]
- Clarke, S.; Lock, V.; Duddy, J.; Sharif, M.; Newman, J.H.; Kirwan, J.R. Intra-articular hylan G-F 20 (Synvisc) in the management of patellofemoral osteoarthritis of the knee (POAK). Knee 2005, 12, 57–62. [Google Scholar] [CrossRef]
- Phillips, M.; Vannabouathong, C.; Devji, T.; Patel, R.; Gomes, Z.; Patel, A.; Dixon, M.; Bhandari, M. Differentiating factors of intra-articular injectables have a meaningful impact on knee osteoarthritis outcomes: A network meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3031–3039. [Google Scholar] [CrossRef]
- Concoff, A.; Rosen, J.; Fu, F.; Bhandari, M.; Boyer, K.; Karlsson, J.; Einhorn, T.A.; Schemitsch, E. A Comparison of Treatment Effects for Nonsurgical Therapies and the Minimum Clinically Important Difference in Knee Osteoarthritis: A Systematic Review. JBJS Rev. 2019, 7, e5. [Google Scholar] [CrossRef]
- Tapasvi, S.; Mohanty, S.S.; Vedavyasa Acharya, K.K.; Bhattacharya, K.; Easwaran, R.; Charugulla, S.N. Viscosupplementation for Management of Knee Osteoarthritis from an Indian Perspective: An Expert Consensus Report. Pain Ther. 2019, 8, 217–231. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Huber, C.; Portelli, A.; Baker-Wagner, M.; Kelley, S.; Lang, K. Patient and physician perspectives guiding intra-articular treatment choice in knee osteoarthritis: Stakeholders are aligned on treatment priorities but have different assessments of treatment effect. J. ISAKOS 2021, 6, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Palco, M.; Rizzo, P.; Basile, G.C.; Alito, A.; Bruschetta, D.; Accorinti, M.; Restuccia, R.; Leonetti, D. Short- and Midterm Comparison of Platelet-Rich Plasma with Hyaluronic Acid versus Leucocyte and Platelet-Rich Plasma on Pain and Function to Treat Hip Osteoarthritis. A Retrospective Study. Gels 2021, 7, 222. [Google Scholar] [CrossRef]
- Xavier, J.; Jerome, W.; Zaslav, K.; Grande, D. Exosome-Laden Scaffolds for Treatment of Post-Traumatic Cartilage Injury and Osteoarthritis of the Knee: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 15178. [Google Scholar] [CrossRef]
- Cui, B.; Chen, Y.; Tian, Y.; Liu, H.; Huang, Y.; Yin, G.; Xie, Q. Effects of medications on incidence and risk of knee and hip joint replacement in patients with osteoarthritis: A systematic review and meta-analysis. Adv. Rheumatol. 2022, 62, 22. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Zhan, H.; Marszalek, J.; Chung, M.; Lin, X.; Zhang, M.; Pang, J.; Wang, C. Traditional Chinese Medications for Knee Osteoarthritis Pain: A Meta-Analysis of Randomized Controlled Trials. Am. J. Chin. Med. 2016, 44, 677–703. [Google Scholar] [CrossRef]
- Riley, N.; Vella-Baldacchino, M.; Thurley, N.; Hopewell, S.; Carr, A.J.; Dean, B.J.F. Injection therapy for base of thumb osteoarthritis: A systematic review and meta-analysis. BMJ Open 2019, 9, e027507. [Google Scholar] [CrossRef]
- Terwee, C.B.; Ahmed, S.; Alhasani, R.; Alonso, J.; Bartlett, S.J.; Chaplin, J.E.; Cho, J.; Choi, H.; Correia, H.; Efficace, F.; et al. Comparable Real-World Patient-Reported Outcomes Data Across Health Conditions, Settings, and Countries: The PROMIS International Collaboration. NEJM Catal. 2024, 5, CAT.24.0045. [Google Scholar] [CrossRef]
- Pesare, E.; Vicenti, G.; Kon, E.; Berruto, M.; Caporali, R.; Moretti, B.; Randelli, P.S. Italian Orthopaedic and Traumatology Society (SIOT) position statement on the non-surgical management of knee osteoarthritis. J. Orthop. Traumatol. 2023, 24, 47. [Google Scholar] [CrossRef]
- Bichsel, D.; Liechti, F.D.; Schlapbach, J.M.; Wertli, M.M. Cross-Sectional Analysis of Recommendations for the Treatment of Hip and Knee Osteoarthritis in Clinical Guidelines. Arch. Phys. Med. Rehabil. 2022, 103, 559–569.e5. [Google Scholar] [CrossRef]
- Brophy, R.H.; Fillingham, Y.A. AAOS Clinical Practice Guideline Summary: Management of Osteoarthritis of the Knee (Nonarthroplasty), Third Edition. J. Am. Acad. Orthop. Surg. 2022, 30, e721–e729. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).