Comparative Analysis of Perioperative Analgesia Methods in Thoracic Surgery: A Literature Systemic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
- 1.
- Adult patients undergoing thoracic surgical procedures;
- 2.
- Comparative evaluation of at least one of the specified analgesia interventions;
- 3.
- Randomized controlled trial, prospective cohort study, or systematic review/meta-analysis design;
- 4.
- Reporting of pain scores, analgesic consumption, complications, or patient satisfaction as outcomes;
- 5.
- Published in peer-reviewed journals.
- Pediatric populations;
- Non-thoracic procedures;
- Case reports/series;
- Animal studies;
- An exclusive focus on chronic post-thoracotomy pain.
2.2. Data Extraction and Quality Assessment
3. Results
3.1. Characteristics of Included Studies
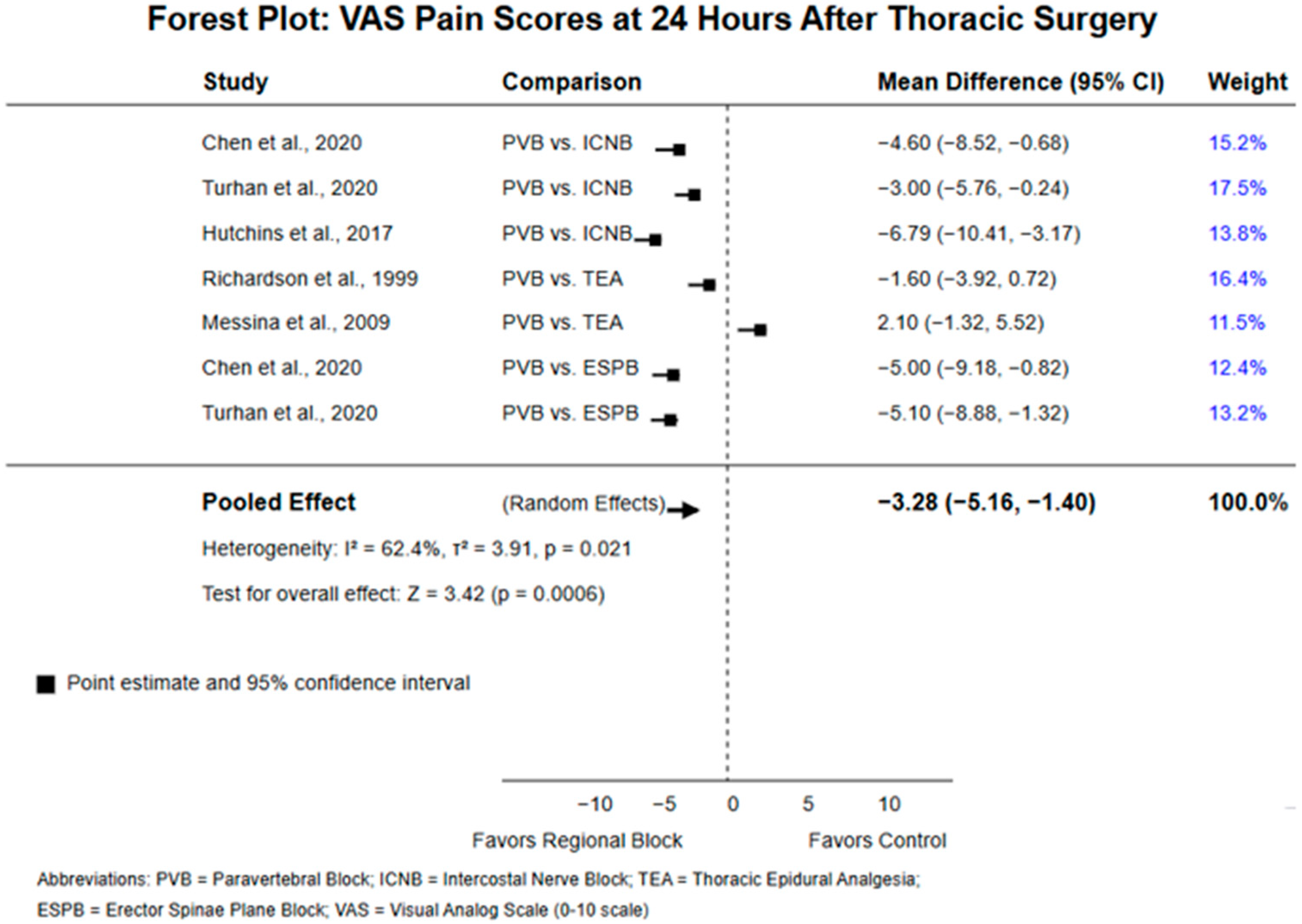
3.2. Comparative Efficacy of Analgesia Techniques
3.2.1. Pain Control
3.2.2. Opioid Consumption
3.2.3. Patient Satisfaction
3.3. Safety and Complications
3.3.1. Technical Complications
3.3.2. Adverse Events
3.3.3. Recovery Metrics
4. Discussion
4.1. Comparison of Analgesia Techniques
4.1.1. Paravertebral Block vs. Intercostal Nerve Block
4.1.2. Paravertebral Block vs. Epidural Analgesia
4.1.3. Regional vs. Systemic Analgesia
4.1.4. Emerging Techniques
4.2. Clinical Implications
- 1.
- Paravertebral block as a first-line option: The consistent evidence supporting the efficacy and safety of paravertebral block suggests it should be considered a first-line analgesic approach for thoracic surgery patients.
- 2.
- Patient-specific considerations: While paravertebral block demonstrates overall favorable outcomes, individual patient factors such as coagulation status, anatomy, and comorbidities should guide technique selection.
- 3.
- Continuous catheter techniques: The extended analgesic benefits observed with continuous paravertebral catheters highlight the importance of addressing pain beyond the immediate postoperative period.
- 4.
- Multimodal approaches: The variability in outcomes across studies suggests that multimodal analgesia, combining regional techniques with appropriate systemic agents, may offer the most comprehensive pain management strategy.
- 5.
- Technical expertise: The lower failure rates associated with paravertebral block compared to epidural analgesia underscore the importance of procedural competence and institutional experience.
4.3. Research Gaps and Future Directions
- 1.
- Limited reporting of patient satisfaction: Only one study explicitly reported patient satisfaction outcomes, highlighting the need for more patient-centered assessments in future research.
- 2.
- Inconsistent time points for pain assessment: The variability in pain measurement timing across studies complicates direct comparisons and meta-analyses.
- 3.
- Minimal data on oral analgesics: None of the identified studies included comprehensive evaluations of oral analgesic regimens, representing a significant gap in the literature.
- 4.
- Limited long-term follow-up: Most studies focused on immediate postoperative outcomes, with little attention to potential long-term effects such as chronic post-thoracotomy pain.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PVB | Paravertebral block |
| TPVB | Thoracic paravertebral block |
| ICNB | Intercostal nerve block |
| ICB | Intercostal block |
| EPI | Epidural analgesia |
| ESPB | Erector spinae plane block |
| PCA | Patient-controlled analgesia |
| CWC | Continuous wound catheter |
| VAS | Visual analog scale |
| NRS | Numeric rating scale |
| VATS | Video-assisted thoracoscopic surgery |
| TEA | Thoracic epidural analgesia |
| PORP | Postoperative respiratory parameters |
| RCT | Randomized controlled trial |
| OR | Odds ratio |
| CI | Confidence interval |
| PONV | Postoperative nausea and vomiting |
| MD | Mean difference |
| CPTP | Chronic post-thoracotomy pain |
References
- Joshi, G.P.; Bonnet, F.; Shah, R.; Wilkinson, R.C.; Camu, F.; Fischer, B.; Neugebauer, E.A.M.; Rawal, N.; Schug, S.A.; Simanski, C.; et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth. Analg. 2008, 107, 1026–1040. [Google Scholar] [CrossRef] [PubMed]
- Sabanathan, S.; Eng, J.; Mearns, A.J. Alterations in respiratory mechanics following thoracotomy. J. R. Coll. Surg. Edinb. 1990, 35, 144–150. [Google Scholar]
- Wildgaard, K.; Ravn, J.; Kehlet, H. Chronic post-thoracotomy pain: A critical review of pathogenic mechanisms and strategies for prevention. Eur. J. Cardiothorac. Surg. 2009, 36, 170–180. [Google Scholar] [CrossRef]
- Kotemane, N.C.; Gopinath, N.; Vaja, R. Analgesic techniques following thoracic surgery: A survey of United Kingdom practice. Eur. J. Anaesthesiol. 2010, 27, 897–899. [Google Scholar] [CrossRef]
- Gottschalk, A.; Cohen, S.P.; Yang, S.; Ochroch, E.A.; Warltier, D.C. Preventing and treating pain after thoracic surgery. Anesthesiology 2006, 104, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Bottiger, B.A.; Esper, S.A.; Stafford-Smith, M. Pain management strategies for thoracotomy and thoracic pain syndromes. Semin. Cardiothorac. Vasc. Anesth. 2014, 18, 45–56. [Google Scholar] [CrossRef]
- Chen, N.; Qiao, Q.; Chen, R.; Xu, Q.; Zhang, Y.; Tian, Y. The effect of ultrasound-guided intercostal nerve block, single-injection erector spinae plane block and multiple-injection paravertebral block on postoperative analgesia in thoracoscopic surgery: A randomized, double-blinded, clinical trial. J. Clin. Anesth. 2020, 66, 109962. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.N.; Lamture, Y.; Krishna, M. Enhanced Recovery After Surgery: Exploring the Advances and Strategies. Cureus 2023, 15, e47237. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Page, M.J.; Mckenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Ding, X.; Jin, S.; Niu, X.; Ren, H.; Fu, S.; Li, Q. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: An updated meta-analysis. PLoS ONE 2014, 9, e96233. [Google Scholar] [CrossRef]
- Fortier, S.; Hanna, H.A.; Bernard, A.; Girard, C. Comparison between systemic analgesia, continuous wound catheter analgesia and continuous thoracic paravertebral block: A randomised, controlled trial of postthoracotomy pain management. Eur. J. Anaesthesiol. 2012, 29, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Guerra-Londono, C.E.; Privorotskiy, A.; Cozowicz, C.; Hicklen, R.S.; Memtsoudis, S.G.; Mariano, E.R.; Cata, J.P. Assessment of intercostal nerve block analgesia for thoracic surgery: A systematic review and meta-analysis. JAMA Netw. Open 2021, 4, e2133394. [Google Scholar] [CrossRef]
- Hutchins, J.; Sanchez, J.; Andrade, R.; Podgaetz, E.; Wang, Q.; Sikka, R. Ultrasound-guided paravertebral catheter versus intercostal blocks for postoperative pain control in video-assisted thoracoscopic surgery: A prospective randomized trial. J. Cardiothorac. Vasc. Anesth. 2017, 31, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Messina, M.; Boroli, F.; Landoni, G.; Bignami, E.; Dedola, E.; Batonga, J.N.; Magrin, A.; Zangrillo, S. A comparison of epidural vs. paravertebral blockade in thoracic surgery. Minerva Anestesiol. 2009, 75, 616–621. [Google Scholar]
- Richardson, J.; Sabanathan, S.; Mearns, A.J.; Shah, R.D.; Goulden, C. A prospective, randomized comparison of interpleural and paravertebral analgesia in thoracic surgery. Br. J. Anaesth. 1995, 75, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.; Sabanathan, S.; Jones, J.; Shah, R.D.; Cheema, S.; Mearns, A.J. A prospective, randomized comparison of preoperative and continuous balanced epidural or paravertebral bupivacaine on post-thoracotomy pain, pulmonary function and stress responses. Br. J. Anaesth. 1999, 83, 387–392. [Google Scholar] [CrossRef]
- Turhan, Ö.; Sivrikoz, N.; Sungur, Z.; Duman, S.; Özkan, B.; Şentürk, M. Thoracic paravertebral block achieves better pain control than erector spinae plane block and intercostal nerve block in thoracoscopic surgery: A randomized study. J. Cardiothorac. Vasc. Anesth. 2020, 34, 2996–3003. [Google Scholar] [CrossRef] [PubMed]
- Davies, R.G.; Myles, P.S.; Graham, J.M. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—A systematic review and meta-analysis of randomized trials. Br. J. Anaesth. 2006, 96, 418–426. [Google Scholar] [CrossRef]
- Yeung, J.H.; Gates, S.; Naidu, B.V.; Wilson, M.J.; Gao Smith, F. Paravertebral block versus thoracic epidural for patients undergoing thoracotomy. Cochrane Database Syst Rev. 2016, 2, CD009121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pintaric, T.S.; Potocnik, I.; Hadzic, A.; Stupnik, T.; Pintaric, M.; Jankovic, V.N. Comparison of continuous thoracic epidural with paravertebral block on perioperative analgesia and hemodynamic stability in patients having open lung surgery. Reg. Anesth. Pain Med. 2011, 36, 256–260. [Google Scholar] [CrossRef]
- Kaiser, A.M.; Zollinger, A.; De Lorenzi, D.; Largiadèr, F.; Weder, W. Prospective, randomized comparison of extrapleural versus epidural analgesia for postthoracotomy pain. Ann. Thorac. Surg. 1998, 66, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Bimston, D.N.; McGee, J.P.; Liptay, M.J.; Fry, W.A. Continuous paravertebral extrapleural infusion for post-thoracotomy pain management. Surgery 1999, 126, 650–656; discussion 656–657. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, M.K. Thoracic paravertebral block. Anesthesiology 2001, 95, 771–780. [Google Scholar] [CrossRef]
- Koyyalamudi, V.B.; Arulkumar, S.; Yost, B.R.; Fox, C.J.; Urman, R.D.; Kaye, A.D. Supraclavicular and paravertebral blocks: Are we underutilizing these regional techniques in perioperative analgesia? Best Pract. Res. Clin. Anaesthesiol. 2014, 28, 127–138. [Google Scholar] [CrossRef]
- Thiruvenkatarajan, V.; Adhikary, S.; Pruett, A.; Forero, M. Erector spinae plane block as an alternative to epidural analgesia for postoperative analgesia following video-assisted thoracoscopic surgery: A case study and a literature review on the spread of local anaesthetic in the erector spinae plane. Indian J. Anaesth. 2018, 62, 75–78. [Google Scholar] [CrossRef] [PubMed]


| Study | Study Design | Sample Size | Intervention Types | Primary Outcomes | Quality Assessment |
|---|---|---|---|---|---|
| Chen et al., 2020 [7] | Randomized controlled trial | 72 | Paravertebral block (PVB), Intercostal nerve block (ICNB), Erector spinae plane block (ESPB) | Cumulative morphine consumption at 24 h postoperatively | Low risk of bias; adequate randomization and allocation concealment; double-blinded design |
| Ding et al., 2014 [10] | Meta-analysis | 777 (across 18 trials) | Paravertebral blockade (PVB), Epidural analgesia (EPI) | Pain scores at 4–8 h, 24 h, 48 h postoperatively; Morphine usage during first 24 h | Moderate quality (AMSTAR-2); comprehensive search strategy; appropriate risk of bias assessment |
| Fortier et al., 2012 [11] | Randomized controlled trial | 140 | Systemic analgesia (patient-controlled analgesia, PCA), Continuous wound catheter (CWC), Thoracic paravertebral block (TPVB) | Pain score at rest as assessed by Visual Analog Scale (VAS) | Some concerns; adequate randomization but unclear blinding of outcome assessment |
| Guerra-Londono et al., 2021 [12] | Systematic review and meta-analysis | 5184 (across 66 studies) | Intercostal nerve block (ICNB) | Analgesic benefit during first 24 h after thoracic surgery | High quality (AMSTAR-2); comprehensive search; appropriate statistical methods; publication bias assessment |
| Hutchins et al., 2017 [13] | Randomized controlled trial | 48 | Ultrasound-guided paravertebral (PV) catheter, Single-shot intercostal blocks (ICB) | Maximum pain score during 24 to 48 h post-surgery | Some concerns; adequate randomization but incomplete blinding |
| Joshi et al., 2008 [1] | Systematic review | Not specified | Thoracic epidural, Paravertebral, Intrathecal, Intercostal, and Interpleural analgesic techniques | Postoperative pain, Analgesic use, and Complications | Low quality (AMSTAR-2); limited search strategy; inadequate risk of bias assessment |
| Messina et al., 2009 [14] | Randomized controlled trial | 24 | Paravertebral block, Epidural analgesia | Postoperative pain and Respiratory function | High risk of bias; small sample size; inadequate blinding |
| Richardson et al., 1995 [15] | Randomized controlled trial | 53 (45 analyzed) | Interpleural analgesia, Paravertebral analgesia | Visual analogue pain scores (VAS), Patient-controlled morphine (PCM) requirements | Some concerns; adequate randomization but incomplete blinding; high attrition rate |
| Richardson et al., 1999 [16] | Randomized controlled trial | 100 | Thoracic epidural bupivacaine, Thoracic paravertebral bupivacaine | Visual analogue pain scores at rest and on coughing | Low risk of bias; adequate randomization and allocation concealment; appropriate blinding |
| Turhan et al., 2020 [17] | Randomized controlled trial | 106 | Erector spinae plane block (ESPB), Thoracic paravertebral block (TPVB), Intercostal nerve block (ICNB) | Dynamic visual analog scale in the first hour postoperatively | Low risk of bias; adequate randomization and allocation concealment; appropriate blinding |
| Jain et al., 2023 [8] | Systematic review | 58 studies included (after screening 480 records) | Enhanced Recovery After Surgery (ERAS) protocols with preoperative, intraoperative, and postoperative components | Recovery time; Hospital length of stay; Complication rates; Patient satisfaction | High quality; comprehensive search strategy using PRISMA methodology; appropriate inclusion criteria; thorough review of evidence |
| Davies et al., 2006 [18] | Meta-analysis | 520 (across 10 trials) | Paravertebral blockade, Thoracic epidural analgesia | Pain scores; Analgesia-related side effects; Pulmonary complications | Moderate quality (AMSTAR-2); comprehensive search; appropriate statistical methods |
| Kotemane et al., 2010 [4] | Systematic review | Not specified | Thoracic epidural, Paravertebral, Intercostal, and other analgesic techniques | Technique prevalence and effectiveness in UK practice | Low quality (AMSTAR-2); limited methodology description; no formal quality assessment |
| Yeung et al., 2016 [19] | Meta-analysis | 1120 (across 14 trials) | Paravertebral block, Thoracic epidural | Pain scores; Analgesia-related complications; Pulmonary outcomes | High quality (AMSTAR-2); comprehensive search; rigorous risk of bias assessment; publication bias evaluation |
| Pintaric et al., 2011 [20] | Randomized controlled trial | 32 | Continuous thoracic epidural, Continuous paravertebral block | Hemodynamic stability; Analgesia efficacy; Stress hormone levels | Some concerns; adequate randomization but incomplete blinding of outcomes |
| Kaiser et al., 1998 [21] | Randomized controlled trial | 30 | Extrapleural analgesia, Epidural analgesia | Pain scores; Pulmonary function; Patient satisfaction | Some concerns; adequate randomization but unclear allocation concealment |
| Bimston et al., 1999 [22] | Randomized controlled trial | 50 | Continuous paravertebral infusion, Thoracic epidural analgesia | Pain control; Respiratory function; Side effects | Some concerns; adequate randomization but incomplete outcome data |
| Study | Intervention | Pain Scores (24 h) | Opioid Consumption | Patient Satisfaction |
|---|---|---|---|---|
| Chen et al., 2020 [7] | PVB, ICNB, ESPB | VAS scores lower in PVB vs. ESPB at 0, 2, 4, 8 h; lower in PVB vs. ICNB at 8 h | PVB: 10.5 mg, ICNB: 18 mg, ESPB: 22 mg (24 h) | No mention found |
| Ding et al., 2014 [10] | PVB vs. EPI | No significant difference (mean difference 0.06; 95% CI: −0.31 to 0.42; p = 0.77) | No significant difference (mean difference 1.11; 95% CI: −2.20 to 4.41; p = 0.51) | No mention found |
| Fortier et al., 2012 [11] | TPVB, CWC, PCA | VAS scores lower in TPVB vs. PCA (p < 0.0026) | Lower in TPVB vs. PCA at 24 h (p = 0.0036) | No mention found |
| Guerra-Londono et al., 2021 [12] | ICNB | Superior to systemic analgesia, non-inferior to other techniques | Reduction in consumption, but inferior to thoracic epidural and PVB | No mention found |
| Hutchins et al., 2017 [13] | PV Catheter vs. ICB | Lower in PV catheter group (3.65 vs. 6.44, p < 0.001) | PV: 14.39 mg vs. ICB: 30.50 mg (24–48 h, p = 0.046) | PV: 74% vs. ICB: 44% (p = 0.036) |
| Joshi et al., 2008 [1] | Various Regional Techniques | Continuous PVB as effective as thoracic epidural | No mention found | No mention found |
| Messina et al., 2009 [14] | PVB vs. Epidural | No significant difference | Epidural: 9 mg vs. PVB: 36 mg (p = 0.003) | No mention found |
| Richardson et al., 1995 [15] | Interpleural vs. PVB | Similar VAS scores | Similar PCM use | No mention found |
| Richardson et al., 1999 [16] | PVB vs. Epidural | Lower in PVB group | Lower in PVB group | No mention found |
| Turhan et al., 2020 [17] | ESPB, TPVB, ICNB | Lower in TPVB vs. ESPB and ICNB at 24 h (p < 0.017) | Similar in TPVB and ICNB, lower than ESPB (p < 0.017) | No mention found |
| Study | Intervention | Technical Complications | Adverse Events | Recovery Metrics |
|---|---|---|---|---|
| Chen et al., 2020 [7] | PVB, ICNB, ESPB | No mention found | No mention found | No mention found |
| Ding et al., 2014 [10] | PVB vs. EPI | Lower failed block rates with PVB (odds ratio 0.51; p = 0.01) | Lower urinary retention (OR 0.21; p < 0.0001), nausea/vomiting (OR 0.49; p = 0.01), hypotension (OR 0.11; p < 0.00001) with PVB | No significant difference in pulmonary complications (OR 0.51; p = 0.09) |
| Fortier et al., 2012 [11] | TPVB, CWC, PCA | No mention found | No signs of toxicity or local complications observed | No mention found |
| Guerra-Londono et al., 2021 [12] | ICNB | No mention found | No mention found | No mention found |
| Hutchins et al., 2017 [13] | PV Catheter vs. ICB | No mention found | No mention found | No mention found |
| Joshi et al., 2008 [1] | Various Regional Techniques | No mention found | Reduced incidence of hypotension with PVB vs. epidural | Reduced pulmonary complications with PVB vs. systemic analgesia |
| Messina et al., 2009 [14] | PVB vs. Epidural | No mention found | No mention found | Better spirometer values at 72 h with epidural (p = 0.03) |
| Richardson et al., 1995 [15] | Interpleural vs. PVB | No mention found | Five patients with temporary confusion in interpleural group (p = 0.02) | Lower PORM and shorter hospital stay with PVB |
| Richardson et al., 1999 [16] | PVB vs. Epidural | No mention found | More side effects (nausea, vomiting, hypotension) in epidural group | Higher oxygen saturations and less respiratory morbidity with PVB |
| Turhan et al., 2020 [17] | ESPB, TPVB, ICNB | No mention found | Similar side effects among groups | No mention found |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanani, F.; Nugzar, R.; Shimonov, M.; Akar, F.A. Comparative Analysis of Perioperative Analgesia Methods in Thoracic Surgery: A Literature Systemic Review. J. Clin. Med. 2025, 14, 2484. https://doi.org/10.3390/jcm14072484
Kanani F, Nugzar R, Shimonov M, Akar FA. Comparative Analysis of Perioperative Analgesia Methods in Thoracic Surgery: A Literature Systemic Review. Journal of Clinical Medicine. 2025; 14(7):2484. https://doi.org/10.3390/jcm14072484
Chicago/Turabian StyleKanani, Fahim, Rijini Nugzar, Mordechai Shimonov, and Firas Abu Akar. 2025. "Comparative Analysis of Perioperative Analgesia Methods in Thoracic Surgery: A Literature Systemic Review" Journal of Clinical Medicine 14, no. 7: 2484. https://doi.org/10.3390/jcm14072484
APA StyleKanani, F., Nugzar, R., Shimonov, M., & Akar, F. A. (2025). Comparative Analysis of Perioperative Analgesia Methods in Thoracic Surgery: A Literature Systemic Review. Journal of Clinical Medicine, 14(7), 2484. https://doi.org/10.3390/jcm14072484