1. Introduction
Articular cartilage consists of water and an extracellular matrix composed of aggrecan, type II collagen, hyaluronic acid, and a small number of chondrocytes. Regenerating articular cartilage is challenging due to its absence of nerves, blood vessels, and lymph vessels [
1]. From a histological perspective, articular cartilage comprises distinct superficial, middle, deep, and calcified layers. The deep layer is also referred to as the calcified layer; beneath it lies the directly continuous subchondral bone. Articular cartilage is a hyaline cartilage that possesses exceptional compression, shearing, and tension properties. It can withstand mechanical loads, minimize friction, and reduce the force transmitted to the subchondral bone [
2]. However, when exposed to excessive mechanical stress, articular cartilage exhibits metabolic abnormalities including decreased production of extracellular matrix components such as aggrecan and type II collagen by chondrocytes at the molecular level, increased chondrocyte apoptosis, and extracellular matrix destruction by a number of proteolytic enzymes. These changes ultimately lead to its degradation.
Osteoarthritis (OA), the most prevalent joint disease, is a degenerative disorder primarily characterized by articular cartilage degeneration. Current estimates indicate that more than 250 million individuals worldwide are affected by OA [
3]. As the global population ages, the prevalence of OA is also expected to increase. Knee OA, in particular, has been identified as a major contributor to disability in both middle-aged and elderly populations, significantly impacting activities of daily living, often manifesting as knee pain and gait disturbances. This condition imposes a substantial financial and economic burden on healthcare systems and the broader economy [
4]. The primary risk factors for knee OA include obesity and lower-limb malalignment such as varus or valgus deformities. Excessive loading on the articular cartilage is responsible for cartilage wear and degeneration [
5]. Severe impairment of the hoop function of the meniscus due to a medial meniscus posterior root tear reportedly results in excessive loading on the articular cartilage, increasing the risk of rapid progression of knee osteoarthritis and osteonecrosis [
6]. Consequently, the treatment of these diseases requires reducing the excessive loading on the articular cartilage and meniscus.
Radiography, magnetic resonance imaging (MRI), and ultrasonography are commonly used to diagnose OA. In recent years, vibration arthrography has been proposed as a new, inexpensive, and non-invasive screening method for cartilage damage [
7,
8,
9] that enables the early detection and treatment of OA. Conservative treatment is typical for early-stage OA. Diet and exercise therapy are the cornerstones of treatment, while drug therapy, encompassing the oral administration of acetaminophen and non-steroidal anti-inflammatory drugs and the intra-articular injection of hyaluronic acid and corticosteroids, has also been employed [
10]. In recent years, biotherapies such as platelet-rich plasma and stem cell therapies have also been used, with evidence of their ability to provide adequate pain relief and enhance patient function. However, the pathogenesis of OA is intricate and not fully understood, and issues such as the absence of an established drug delivery system for chondrocytes preclude these treatments from suppressing articular cartilage degeneration. In cases in which symptoms persist or cartilage degeneration progresses, surgical treatment is preferred. The most common surgical interventions include osteotomy and artificial joint replacement. High tibial osteotomy (HTO) is considered a conventional surgical procedure that reduces the medial stress by shifting the load axis from the medial to the lateral side, thereby reducing pain. Two surgical approaches have been employed to treat medial compartment overload in varus knees: medial open wedge high tibial osteotomy (MOWHTO) and lateral closing wedge high tibial osteotomy (LCWHTO). The traditional approach is LCWHTO, which involves partial resection of the fibula and wedge-shaped resection of the lateral side of the proximal tibia. However, with the advent of locking plates and mechanically robust artificial bones, MOWHTO has gained popularity because it allows the opening of the medial side of the proximal tibia [
11]. The advent of MOWHTO surgical techniques and implants has facilitated early weight-bearing as a relatively simple surgical technique uncomplicated by peroneal nerve palsy, a potential complication of LCWHTO. Preservation of the pes anserinus at the osteotomy site further facilitates its minimally invasive nature [
12]. MOWHTO has also demonstrated favorable short- and midterm outcomes [
13,
14]. Moreover, its use enables the possible long-term avoidance of total knee arthroplasty (TKA). Conversely, in MOWHTO, patient background factors that influence postoperative outcomes include age, sex, weight, OA progression, deformity etiology, and joint instability. Other factors associated with MOWHTO success include target alignment, surgical technique, and increased patellofemoral joint load owing to its low postoperative position [
15,
16]. Other potential concerns include excessive increases in the inclination of the articular surface and posterior tibial slope. Although many unknown factors of MOWHTO persist, its indications for surgery, surgical technique, and postoperative alignment are crucial factors in achieving favorable clinical outcomes. The identification of factors that exert a detrimental influence on the clinical outcomes of MOWHTO will facilitate the achievement of enhanced long-term results through the selection of appropriate patients and surgical techniques. Here, we sought to analyze the clinical outcomes of patients who could be followed up for >5 years after MOWHTO and identify the influential factors.
4. Discussion
This study demonstrated that a MOWHTO with a target %MA of 62.5% yields favorable long-term outcomes. In addition, preoperative obesity and high joint instability negatively influenced post-MOWHTO survival. Furthermore, a postoperative %MA of <62.5% was associated with difficulty in maintaining stable alignment and an increased risk of conversion to TKA.
Historically, LCWHTO has yielded the most favorable long-term outcomes for medial-compartment knee osteoarthritis, as Coventry’s technique is the inaugural approach utilized for this indication. Constantin et al. conducted a prospective study of 100 patients who underwent LCWHTO. When conversion to TKA was used as the endpoint, the 20-year survival rate was 44%. The factors that had a positive impact on improving survival were age < 55 years, BMI < 30 kg/m
2, and absence of serious symptoms [
19]. Sasaki et al. conducted a survey of 120 knees subjected to LCWHTO and found that the 15-year survival rate was 92.5%, with obesity and high preoperative symptom severity identified as risk factors for requiring TKA [
20]. Ishizuka et al. conducted a survey of 56 knees that underwent LCWHTO and found that the 10-, 20-, and 35-year survival rates were 83.8%, 75.9%, and 75.9%, respectively. The analysis revealed that a BMI ≥ 25 and a femorotibial angle < 185° affected TKA conversion [
21].
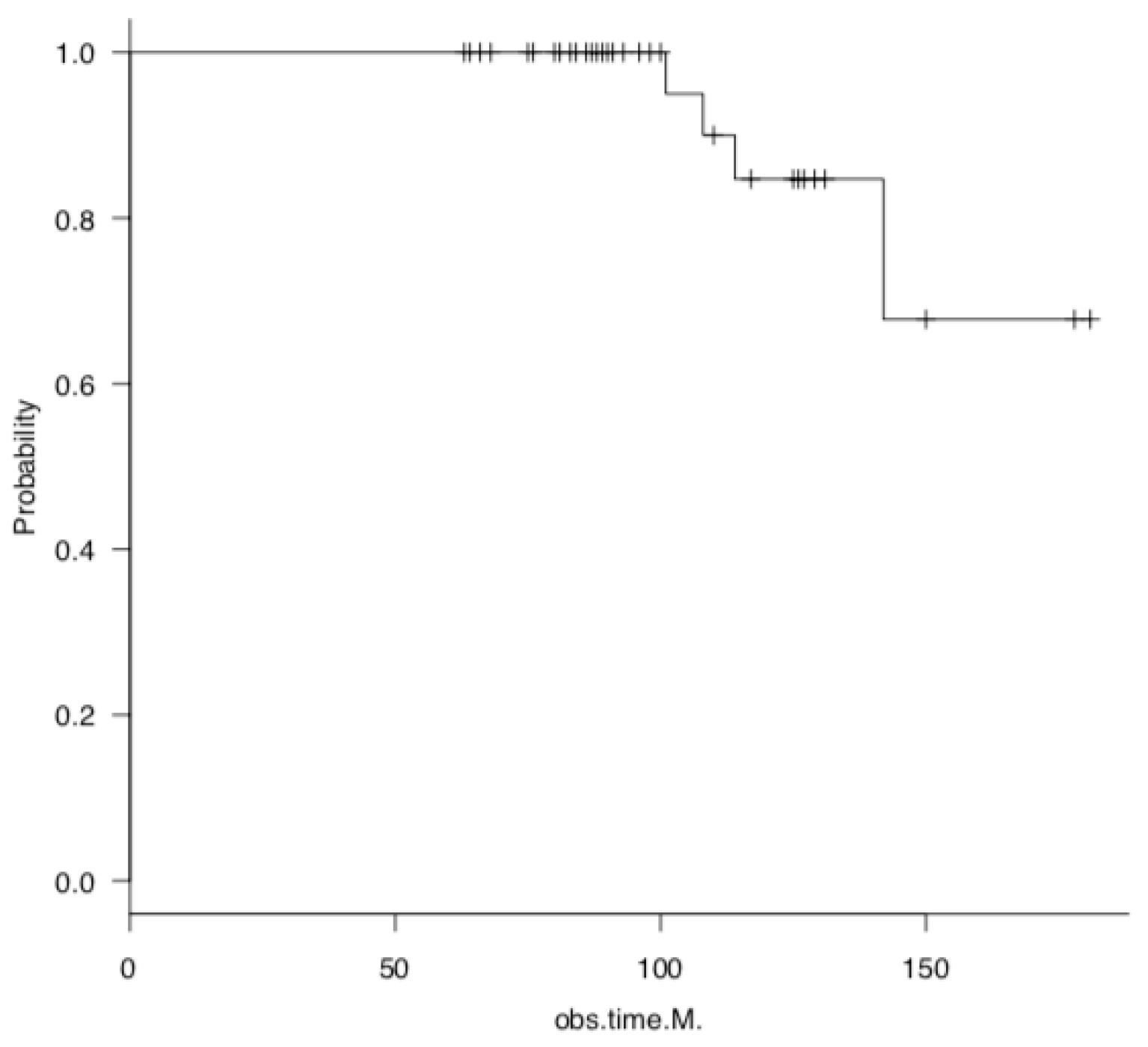
Conversely, given the relatively recent introduction of MOWHTO, the number of studies examining its long-term survival, sample size, and follow-up period is considerably smaller than those examining LCWHTO. In an early report on MOWHTO with a large sample size, a study of 245 knees, with a target postoperative alignment of 183–186°, was conducted in 2001. The 5-, 10-, and 15-year survival rates were 94%, 85%, and 68%, respectively, with an endpoint of TKA conversion [
22]. A meta-analysis conducted by Kim et al. reviewed 23 studies of MOWHTO and LCWHTO with a minimum 5-year follow-up period. The survival rates after conversion to TKA were 95.1% and 91.6% at 5 and 10 years, respectively. Notably, the survival rate at 10 years was higher in the MOWHTO versus LCWHTO group [
23]. Keenan et al. reported a 10-year survival rate of 65% and a 15-year survival rate of 55% in 111 patients who underwent MOWHTO [
24]. In a comparative study of the long-term outcomes of MOWHTO and UKA, Jin et al. [
25] observed that the survival rates at 10 years were 96.2% and 91.6%, respectively. In a large study of 556 patients conducted by Primeau et al., the revision rate from MOWHTO to TKA was 5% at 5 years and 21% at 10 years [
26]. In a small study by Lau et al. spanning 13 years, the 10-year survival rate of patients treated with MOWHTO was 87% [
27]. According to a systematic review and meta-analysis of 59 studies (5162 patients) by Loke et al., conversion to TKA occurred in 4.5%, 8.3%, and 11.2% of cases at <5, 5–10, and >10 years, respectively [
28]. Thus, despite differences in study design, sample size, and surgical technique, the survival rates for MOWHTO are approximately 95% at 5 years, 65–92% at 10 years, and 55–75% at 15 years or longer. In our small study, four of the 48 knees required TKA, with a 5-year survival rate of 100% and a 10-year survival rate of 82%. These findings are consistent with the survival rates observed in the aforementioned clinical trials and generally indicate good long-term results.
As a target postoperative alignment for HTO, the criterion that the weight-bearing line passes through 62–66% of the tibial plateau width, as recommended by Dugdale et al. in 1992, has been widely utilized [
29]. This criterion is consistent with the finding that the weight-bearing line passes laterally to the lateral intercondylar ridge of the tibia in alignment with the HKA at an angle of 3–5° and includes the Fujisawa point, which was used as our target alignment point. Conversely, numerous approaches to target alignment have been proposed in recent years. Atkinson et al. utilized MRI T2 mapping to qualitatively evaluate articular cartilage pre- versus postoperatively and reported that correcting the alignment to be closer to neutral versus excessive valgus alignment enhanced cartilage quality without compromising the lateral compartment [
30]. Kim et al. reported favorable clinical outcomes in valgus cases with a mechanical axis of 0–3° by performing cartilage repair surgery involving microfracture, autologous cultured chondrocyte transplantation, and stem cell transplantation with concomitant MOWHTO [
31]. However, inadequate correction and residual postoperative varus alignment are also associated with a poor prognosis and the progression of medial compartment osteoarthritis of the knee [
32]. In this study, regardless of preoperative lower-limb alignment, the mean %MA at the time of implant removal was 62.2%, which approached the target value of 62.5%. Furthermore, significant improvements in clinical scores were maintained at the final follow-up. The 10-year survival rate was 82%, and a univariate analysis demonstrated that the alignment at the time of implant removal was associated with postoperative outcomes. A univariate analysis demonstrated that alignment at the time of implant removal was not a risk factor for conversion to TKA. This indicates that MOWHTO, targeting this alignment, is advantageous for achieving a favorable long-term outcome.
Using a musculoskeletal computer model, Kuriyama et al. analyzed the correction of various frontal planes in MOWHTO during walking and squatting. They found that Fujisawa point alignment (%MA, 62.5%) sufficiently loaded the lateral femorotibial joint after MOWHTO, maintaining normal knee kinematics [
33]. In this study, no significant changes were observed in the cartilage evaluation using the ICRS classification with arthroscopy, either medially or laterally, pre- versus postoperatively. This suggests that this surgical technique also protects the medial compartment biomechanically and can avoid excessive lateral-side loading. Conversely, the %MA at the final follow-up was 57.8%, lower than that at the time of implant removal, indicating that alignment was inversely related to the long-term outcome of MOWHTO. Additionally, a univariate analysis demonstrated that both %MA and Δ%MA at the final follow-up were associated with an increased risk of conversion to TKA. Furthermore, a multivariate analysis indicated that Δ%MA was an independent predictor of conversion to TKA. Moreover, a comparison of 26 patients with a %MA ≥ 62.5% at the time of implant removal, which included 22 patients who did not reach this threshold, revealed a significantly greater Δ%MA in those who did not reach the threshold. This suggests that if the postoperative %MA is <62.5% in MOWHTO, the risk of conversion to TKA may increase owing to difficulty maintaining stable alignment.
The survival rate after HTO is influenced by several prognostic factors, including sex, age, obesity, and preoperative knee osteoarthritis severity. Regarding sex, some studies have indicated that females are at increased risk, whereas others did not identify any such association [
34,
35,
36,
37]. The present study did not identify an association between sex and survival among patients who underwent MOWHTO. Further research is required to ascertain the impact of sex on this outcome. Evidence indicates that older adults aged ≥ 60 years demonstrate comparable performance on short-term tests to younger individuals [
38,
39,
40]. However, a predominant finding suggests that advanced age (specifically, 50–60 years) tends to have a deleterious impact on survival outcomes [
41]; in the majority of cases, age 55 years or older is considered a risk factor. In this study, the mean patient age was 55 years, and no age-based effect was observed. The acceptable BMI range is 25–30 kg/m² [
41]. In a recent study, Bouguennec et al. [
42] demonstrated that a BMI > 25 kg/m² significantly elevated the risk of conversion to TKA; moreover, a higher BMI (>35 kg/m²) further augmented this risk. In the present study, a BMI > 30 kg/m² was also associated with an increased risk of revision TKA, indicating that obesity has a detrimental impact on the long-term outcomes of MOWHTO. Therefore, the indications for MOWHTO in patients with obesity should be carefully evaluated; if indicated, patients should be encouraged to lose weight before undergoing surgery.
Regarding the adverse impact of knee osteoarthritis on HTO, an Ahlbäck classification grade of III or higher with loss of joint space and mild loss of subchondral bone on plain radiographs is considered a risk factor. Cartilage degeneration severity on arthroscopic findings is also a poor prognostic factor [
26,
27,
42,
43]. One study examining cartilage damage severity on arthroscopy and the long-term outcomes of MOWHTO found that patients > 40 years of age with advanced cartilage damage and an Outerbridge classification of 3–4 had a higher rate of conversion to TKA [
44]. Gkekas et al. reported favorable long-term outcomes for cases of high-severity OA (KL3 and 4), with a survival rate of 91.5% after a mean of 13.6 years [
45]. Knee osteoarthritis severity did not appear to influence the MOWHTO outcomes in this study. However, it is possible that this was not identified as a risk factor because of the limited number of cases included in the study; specifically, only four cases of KL 4 with no joint space were included. Conversely, preoperative varus–valgus joint instability may also have an influence. In particular, postoperative alignment adjustment is challenging when MOWHTO is employed to treat patients with advanced knee osteoarthritis who have lost medial articular cartilage and have a large JLCA, resulting in instability [
46,
47]. As this study identified JLCA as a factor that negatively affects the survival rate of MOWHTO, alternative techniques such as tibial condylar valgus osteotomy [
48,
49] and double-level osteotomy [
50] should be considered in patients with significant preoperative joint instability.
This study is clinically significant in that it demonstrates the importance of evaluating patient weight and knee joint instability in the application of MOWHTO for medial knee joint disease. Furthermore, good long-term results can be obtained with MOWHTO targeting the Fujisawa point.