Controversies in the Treatment Strategies of Intertrochanteric Fractures: A Scoping Review and Discussion of a Literature-Based Algorithm
Abstract
1. Introduction
General Considerations for Decision-Making
- -
- Treatment in the case of polytrauma or monotrauma;
- -
- Reconstruction vs. arthroplasty;
- -
- Open vs. closed reduction;
- -
- Reconstruction with or without additional cables and plates;
- -
- Cephalomedullary nail vs. dynamic hip screw (DHS);
- -
- Long cephalomedullary nail vs. short cephalomedullary nail.
2. Methods
- -
- Regulations (Preferred Reporting Items for Systematic review and MetaAnalysis); however, the focus was rather on examining and discussing controversies. Initially, the title and abstract were screened, and, if applicable, the whole manuscript was screened. The following search terms were used in PubMed/MEDLINE in August 2024: (intertrochanteric fracture) AND (long cephalomedullary nail) OR (short cephalomedullary nail); (intertrochanteric fracture) AND (open) OR (closed reduction), (intertrochanteric fracture) AND (arthroplasty), (intertrochanteric fracture) AND (dynamic hip screw) OR (gliding hip screw), (intertrochanteric fracture) AND (polytrauma), (intertrochanteric fracture) AND (implant failure). Data extraction was focused on literature, including manuscripts from the last decade. Eligibility criteria were (1) manuscripts in the English or German language, (2) clinical or biomechanical studies reporting the outcome after treatment of intertrochanteric fractures, and (3) data published in a peer review process. Studies were excluded if they were conference papers, letters or comments, or case reports. A ranking of the level of evidence was performed, favoring manuscripts in a hierarchical process with (1) high-quality randomized trials or prospective studies, (2) prospective comparative studies, (3) case–control studies, and (4) case series. A low level of evidence is interpreted as a limitation, which is discussed if applicable in the manuscript.
- -
- Only for Figure 1D was AI (ChatGPT) used to produce the image. AI was not further used in the processing process of this work. Neither in the literature research process nor in the writing or processing process of this manuscript was AI used.
3. Classification
4. Monotrauma or Polytrauma
Fixation vs. Arthroplasty
5. Different Forms of Reconstruction
5.1. Basic Considerations
5.2. Open vs. Closed Procedure
5.3. Reconstruction With or Without Additional Cables and Plates
5.4. Cephalomedullary Nail vs. Dynamic Hip Screw (DHS)
5.5. Long Cephalomedullary Nail vs. Short Cephalomedullary Nail
5.6. Factors Defining Stability
5.7. Arthroplasty
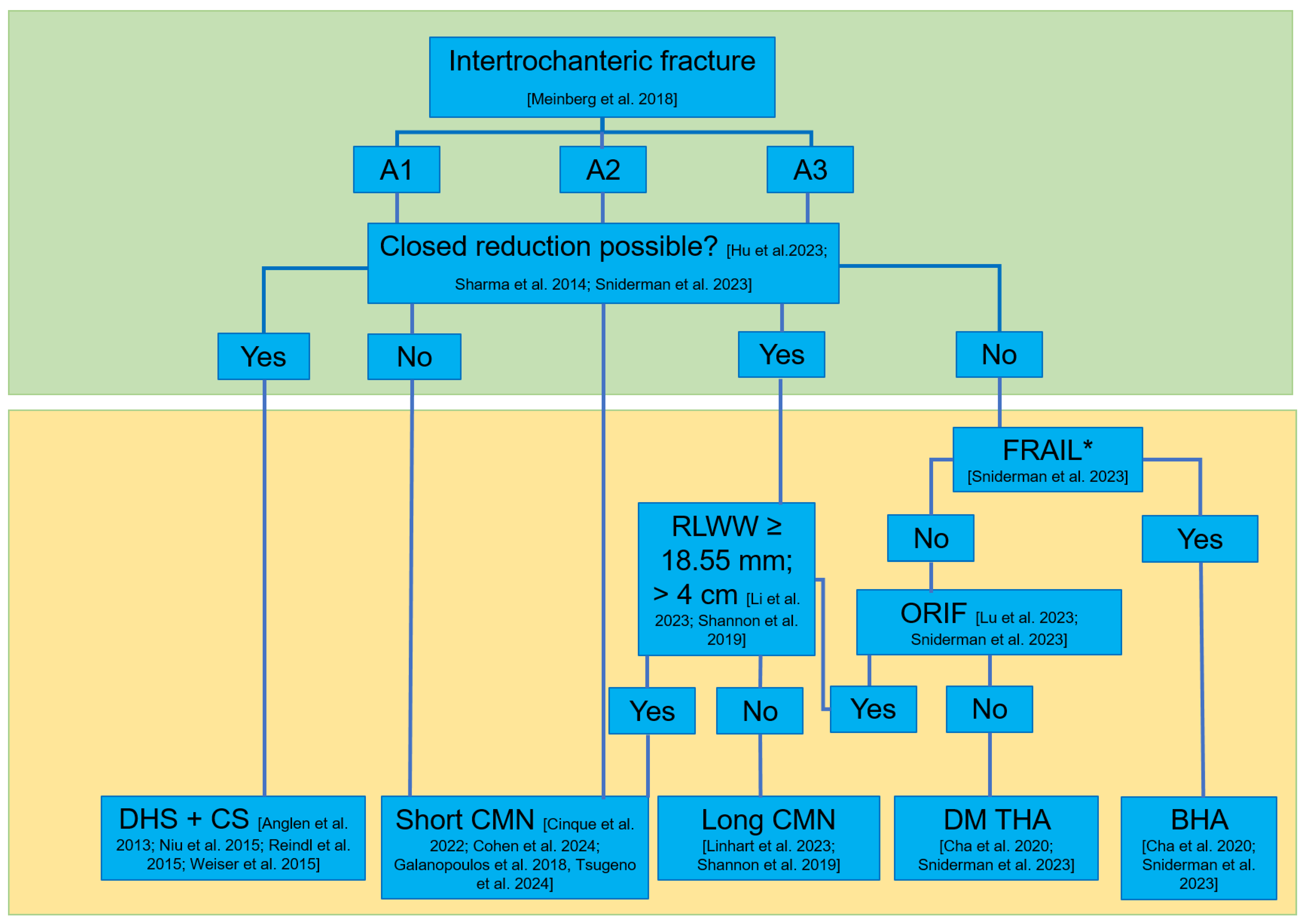
5.8. Algorithm for Treating Intertrochanteric Femoral Fractures
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Metcalfe, D.; Judge, A.; Perry, D.C.; Gabbe, B.; Zogg, C.K.; Costa, M.L. Total hip arthroplasty versus hemiarthroplasty for independently mobile older adults with intracapsular hip fractures. BMC Musculoskelet. Disord. 2019, 4, 226. [Google Scholar] [CrossRef] [PubMed]
- Schipper, I.B.; Bresina, S.; Wahl, D.; Linke, B.; Vugt, A.B.V.; Schneider, E. Biomechanical evaluation of the proximal femoral nail. Clin. Orthop. Relat. Res. 2002, 405, 277–286. [Google Scholar] [CrossRef]
- Parker, M.; Johansen, A. Hip fracture. BMJ 2006, 1, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Ridha, M.; Al-Jabri, T.; Stelzhammer, T.; Shah, Z.; Oragui, E.; Giannoudis, P.V. Osteosynthesis, hemiarthroplasty, total hip arthroplasty in hip fractures: All I need to know. Injury 2024, 55, 111377. [Google Scholar] [CrossRef] [PubMed]
- Fischer, H.; Maleitzke, T.; Eder, C.; Shmad, S.; Stöckle, U.; Braun, K.F. Management of proximal femur fractures in the elderly: Current concepts and treatment options. Eur. J. Med. Res. 2021, 26, 86. [Google Scholar] [CrossRef]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.S.; Kellam, J. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma. 2018, 32, S1–S170. [Google Scholar] [CrossRef]
- Agel, J.; Evans, A.R.; Marsh, J.L.; Decoster, T.A.; Lundy, D.W.; Kellam, J.F.; Jones, C.B.; Desilva, G.L. The OTA Open Fracture Classification. J. Orthop. Trauma. 2013, 27, 379–384. [Google Scholar] [CrossRef]
- Evans, E. The treatment of trochanteric fractures of the femur. J. Bone Jt. Surg. Br. 1949, 31, 190–203. [Google Scholar] [CrossRef]
- Pincus, D.; Ravi, B.; Wasserstein, D.; Govindarajan, A.; Huang, A.; Austin, P.C.; Jenkinson, R.; Henry, P.D.G.; Paterson, J.M.; Kreder, H.J. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. JAMA 2017, 318, 1994. [Google Scholar] [CrossRef]
- Friedman, S.M. Impact of a Comanaged Geriatric Fracture Center on Short-term Hip Fracture Outcomes. Arch. Intern. Med. 2009, 169, 1712. [Google Scholar] [CrossRef]
- von Rüden, C.; Tauber, M.; Woltmann, A.; Friederichs, J.; Hackl, S.; Bühren, V.; Hierholzer, C. Surgical treatment of ipsilateral multi-level femoral fractures. J. Orthop. Surg. Res. 2015, 10, 7. [Google Scholar] [CrossRef] [PubMed]
- Miric, D.M.; Bumbasirevic, M.Z.; Senohradski, K.K.; Djordjevic, Z.P. Pelvifemoral external fixation for the reatment of open fractures of the proximal femur caused by firearms. Acta Orthop. Belg 2002, 68, 37–41. [Google Scholar] [PubMed]
- Lu, X.; Gou, W.; Wu, S.; Wang, Y.; Wang, Z.; Xiong, Y. Complication Rates and Survival of Nonagenarians after Hip Hemiarthroplasty versus Proximal Femoral Nail Antirotation for Intertrochanteric Fractures: A 15-Year Retrospective Cohort Study of 113 Cases. Orthop. Surg. 2023, 15, 3231–3242. [Google Scholar] [CrossRef] [PubMed]
- Sniderman, J.; Vivekanantha, P.; Shah, A.; Safir, O.; Wolfstadt, J.; Kuzyk, P. Hemiarthroplasty for Unstable Intertrochanteric Hip Fractures: A Matched Cohort Study. J. Arthroplast. 2023, 38, 1522–1527. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The Value of Tip-Ape Distance in Predicting Failure of FIxation of Peritrochanteric Fractures of the Hip. J. Bone Jt. Surg. 1995, 77, 1058–1064. [Google Scholar] [CrossRef]
- Cleveland, M.; Bosworth, D.M.; Thompson, F.R.; Wilson, H.J., Jr.; Ishizuka, T. A ten-year analysis of intertrochanteric fractures of the femur. J. Bone Joint Surg. Am. 1959, 41-A, 1399–1408. [Google Scholar] [CrossRef]
- Schopper, C.; Keck, K.; Zderic, I.; Migliorini, F.; Link, B.C.; Beeres, F.J.P.; Babst, R.; Nebelung, S.; Eschbach, D.; Knauf, T.; et al. Screw-blade fixation systems for implant anchorage in the femoral head: Horizontal blade orientation provides superior stability. Injury 2021, 52, 1861–1867. [Google Scholar] [CrossRef]
- Zirngibl, B.; Biber, R.; Bail, H.J. How to prevent cut-out and cut-through in biaxial proximal femoral nails: Is there anything beyond lag screw positioning and tip-apex distance? Int. Orthop. 2013, 37, 1363–1368. [Google Scholar] [CrossRef][Green Version]
- Huang, X.; Leung, F.; Liu, M.; Chen, L.; Xiang, Z. Is helical blade superior to screw design in terms of cut-out rate for elderly trochanteric fractures? A meta-analysis of randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1461–1468. [Google Scholar] [CrossRef]
- Stern, R.; Lübbeke, A.; Suva, D.; Miozzari, H.; Hoffmeyer, P. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures. Int. Orthop. 2011, 35, 1855–1861. [Google Scholar] [CrossRef]
- Stern, L.C.; Gorczyca, J.T.; Kates, S.; Ketz, J.; Soles, G.; Humphrey, C.A. Radiographic Review of Helical Blade Versus Lag Screw Fixation for Cephalomedullary Nailing of Low-Energy Peritrochanteric Femur Fractures: There is a Difference in Cutout. J. Orthop. Trauma. 2017, 31, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Chapman, T.; Zmistowski, B.; Krieg, J.; Stake, S.; Jones, C.M.; Levicoff, E. Helical Blade Versus Screw Fixation in the Treatment of Hip Fractures With Cephalomedullary Devices: Incidence of Failure and Atypical “Medial Cutout”. J. Orthop. Trauma. 2018, 32, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Flores, S.A.; Woolridge, A.; Caroom, C.; Jenkins, M. The Utility of the Tip–Apex Distance in Predicting Axial Migration and Cutout With the Trochanteric Fixation Nail System Helical Blade. J. Orthop. Trauma. 2016, 30, e207–e211. [Google Scholar] [CrossRef] [PubMed]
- Kammerlander, C.; Doshi, H.; Gebhard, F.; Scola, A.; Meier, C.; Linhart, W.; Garcia-Alonso, M.; Nistal, J.; Blauth, M. Long-term results of the augmented PFNA: A prospective multicenter trial. Arch. Orthop. Trauma. Surg. 2014, 134, 343–349. [Google Scholar] [CrossRef]
- Kammerlander, C.; Hem, E.S.; Klopfer, T.; Gebhard, F.; Sermon, A.; Dietrich, M.; Bach, O.; Weil, Y.; Babst, R.; Blauth, M. Cement augmentation of the Proximal Femoral Nail Antirotation (PFNA)—A multicentre randomized controlled trial. Injury 2018, 49, 1436–1444. [Google Scholar] [CrossRef]
- Serrano, R.; Blair, J.A.; Watson, D.T.; Infante, A.F., Jr.; Shah, A.R.; Mir, H.R.; Maxson, B.J.; Downes, K.L.; Sanders, R.W. Cephalomedullary Nail Fixation of Intertrochanteric Femur Fractures: Are Two Proximal Screws Better Than One? J. Orthop. Trauma. 2017, 31, 577–582. [Google Scholar] [CrossRef]
- Berger-Groch, J.; Rupprecht, M.; Schoepper, S.; Schroeder, M.; Rueger, J.M.; Hoffmann, M. Five-Year Outcome Analysis of Intertrochanteric Femur Fractures: A Prospective Randomized Trial Comparing a 2-Screw and a Single-Screw Cephalomedullary Nail. J. Orthop. Trauma. 2016, 30, 483–488. [Google Scholar] [CrossRef]
- Hu, S.; Chang, S.-M.; Du, S.-C.; Zhang, L.-Z.; Xiong, W.-F. Two-Part Intertrochanteric Femur Fractures with Bisection of the Lesser Trochanter: An Irreducible Fracture Pattern. Geriatr. Orthop. Surg. Rehabil. 2023, 14, 21514593231153827. [Google Scholar] [CrossRef]
- Sharma, G.; GNK kumar Yadav, S.; Lakhotia, D.; Singh, R.; Gamanagatti, S.; Sharma, V. Pertrochanteric fractures (AO/OTA 31-A1 and A2) not amenable to closed reduction: Causes of irreducibility. Injury 2014, 45, 1950–1957. [Google Scholar] [CrossRef]
- Förch, S.; Sandriesser, S.; Fenwick, A.; Mayr, E. Beeinträchtigung der Blutversorgung durch Cerclagen: Mythos oder Realität? Unfallchirurg 2021, 124, 231–240. [Google Scholar] [CrossRef]
- Dietze, C.; Brand, A.; Friederichs, J.; Stuby, F.; Schneidmueller, D.; von Rüden, C. Results of revision intramedullary nailing with and without auxillary plate in aseptic trochanteric and subtrochanteric nonunion. Eur. J. Trauma Emerg. Surg. 2022, 48, 1905–1911. [Google Scholar] [CrossRef] [PubMed]
- McGarry, L.; Rotaru, J.; Gunaratne, R.; Hickey, I. Medial buttress plate use in neck of femur fracture fixations: A systematic review. Injury 2025, 56, 112160. [Google Scholar] [CrossRef] [PubMed]
- Anglen, J.O.; Weinstein, J.N. Nail or Plate Fixation of Intertrochanteric Hip Fractures: Changing Pattern of Practice. J. Bone Jt. Surg.-Am. Vol. 2008, 90, 700–707. [Google Scholar] [CrossRef] [PubMed]
- Niu, E.; Yang, A.; Harris, A.H.S.; Bishop, J. Which Fixation Device is Preferred for Surgical Treatment of Intertrochanteric Hip Fractures in the United States? A Survey of Orthopaedic Surgeons. Clin. Orthop. Relat. Res. 2015, 473, 3647–3655. [Google Scholar] [CrossRef]
- Kyriakopoulos, G.; Panagopoulos, A.; Pasiou, E.; Kourkoulis, S.K.; Diamantakos, I.; Anastopoulos, G.; Tserpes, K.; Tatani, I.; Lakoumentas, J.; Megas, P. Optimizing fixation methods for stable and unstable intertrochanteric hip fractures treated with sliding hip screw or cephalomedullary nailing: A comparative biomechanical and finite element analysis study. Injury 2022, 53, 4072–4085. [Google Scholar] [CrossRef]
- Weiser, L.; Ruppel, A.A.; Nüchtern, J.V.; Sellenschloh, K.; Zeichen, J.; Püschel, K.; Morlock, M.M.; Lehmann, W. Extra- vs. intramedullary treatment of pertrochanteric fractures: A biomechanical in vitro study comparing dynamic hip screw and intramedullary nail. Arch. Orthop. Trauma. Surg. 2015, 135, 1101–1106. [Google Scholar] [CrossRef]
- Reindl, R.; Harvey, E.J.; Berry, G.K.; Rahme, E. Intramedullary Versus Extramedullary Fixation for Unstable Intertrochanteric Fractures. J. Bone Jt. Surg.-Am. Vol. 2015, 97, 1905–1912. [Google Scholar] [CrossRef]
- Zeelenberg, M.L.; Plaisier, A.C.; Nugteren, L.H.T.; Loggers, S.A.I.; Joosse, P.; Verhofstad, M.H.J.; Hartog, D.D.; Lieshout, E.M.M. STABLE-HIP Study Group. Extramedullary versus intramedullary fixation of unstable trochanteric femoral fractures (AO type 31-A2): A systematic review and meta-analysis. Arch. Orthop. Trauma. Surg. 2024, 144, 1189–1209. [Google Scholar] [CrossRef]
- Cohen, D.; Tolwin, Y.; Toybenshlak, M.; Zinger, G.; Peyser, A.; Levy, Y. Complications and survival rates of subtrochanteric fractures are similar between short and long intramedullary nail fixation and independent of weight-bearing. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2779–2784. [Google Scholar] [CrossRef]
- Tsugeno, H.; Takegami, Y.; Tokutake, K.; Mishima, K.; Nakashima, H.; Kobayashi, K.; Imagama, S. Comparing short vs. intermediate and long nails in elderly patients with unstable multifragmental femoral trochanteric fractures (AO type A2): Multicenter (TRON group) retrospective study. Injury 2024, 55, 111420. [Google Scholar] [CrossRef]
- Cinque, M.E.; Goodnough, L.H.; Schultz Md, B.J.; Fithian, A.T.; BeBaun, M.; Lucas, J.F.; Gardner Md, M.J.; Bishop, J.A. Short versus long cephalomedullary nailing of intertrochanteric fractures: A meta-analysis of 3208 patients. Arch. Orthop. Trauma Surg. 2022, 142, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Galanopoulos, I.P.; Mavrogenis, A.F.; Megaloikonomos, P.D.; Vottis, C.T.; Mitsiokapa, E.; Koulouvaris, P.; Mastrokalos, D.S.; Papagelopoulos, P.J.; Kontogeorgakos, V.A. Similar function and complications for patients with short versus long hip nailing for unstable pertrochanteric fractures. SICOT J. 2018, 4, 23. [Google Scholar] [CrossRef]
- Irgit, K.; Richard, R.D.; Beebe, M.J.; Bowen, T.R.; Kubiak, E.; Horwitz, D.S. Reverse Oblique and Transverse Intertrochanteric Femoral Fractures Treated With the Long Cephalomedullary Nail. J. Orthop. Trauma. 2015, 29, e299–e304. [Google Scholar] [CrossRef]
- Linhart, C.; Kistler, M.; Kussmaul, A.C.; Woiczinski, M.; Böcker, W.; Ehrenthaller, C. Biomechanical stability of short versus long proximal femoral nails in osteoporotic subtrochanteric A3 reverse-oblique femoral fractures: A cadaveric study. Arch. Orthop. Trauma. Surg. 2023, 143, 389–397. [Google Scholar] [CrossRef]
- Shannon, S.F.; Yuan, B.J.; Cross, W.W.; Barlow, J.D.; Torchia, M.E.; Holte, P.K.; Sems, S.A. Short Versus Long Cephalomedullary Nails for Pertrochanteric Hip Fractures: A Randomized Prospective Study. J. Orthop. Trauma. 2019, 33, 480–486. [Google Scholar] [CrossRef]
- Li, S.-J.; Chang, S.-M.; Liu, H.; Hu, S.-J.; Du, S.-C. Residual lateral wall width predicts a high risk of mechanical complications in cephalomedullary nail fixation of intertrochanteric fractures: A retrospective cohort study with propensity score matching. Int. Orthop. 2023, 47, 1827–1836. [Google Scholar] [CrossRef]
- Costa, M.L.; Griffin, X.L.; Pendleton, N.; Pearson, M.; Parsons, N. Does cementing the femoral component increase the risk of peri-operative mortality for patients having replacement surgery for a fracture of the neck of femur? J. Bone Jt. Surg. Br. 2011, 93-B, 1405–1410. [Google Scholar] [CrossRef]
- Kannan, A.; Kancherla, R.; McMahon, S.; Hawdon, G.; Soral, A.; Malhotra, R. Arthroplasty options in femoral-neck fracture: Answers from the national registries. Int. Orthop. 2012, 36, 1–8. [Google Scholar] [CrossRef]
- Klopfer, T.; Hemmann, P.; Ziegler, P.; Stöckle, U.; Bahrs, C. Proximale Femurfraktur und Insuffizienzfrakturen im Alter. Trauma. Berufskrankh. 2017, 19, 27–36. [Google Scholar] [CrossRef][Green Version]
- Kreipke, R.; Rogmark, C.; Pedersen, A.B.; Kärrholm, J.; Hallan, G.; Havelin, L.I.; Mäkelä, K.; Overgaard, S. Dual Mobility Cups: Effect on Risk of Revision of Primary Total Hip Arthroplasty Due to Osteoarthritis. J. Bone Jt. Surg. 2019, 101, 169–176. [Google Scholar] [CrossRef]
- Yli-Kyyny, T.; Sund, R.; Heinänen, M.; Malmivaara, A.; Kröger, H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop. 2014, 85, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.-H.; Yoo, J.-I.; Kim, J.-T.; Park, C.H.; Ahn, Y.S.; Choy, W.S.; Ha, Y.C.; Koo, K.H. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures. Bone Joint J. 2020, 102-B, 1457–1466. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graulich, T.; Omar, M.; Sehmisch, S.; Liodakis, E. Controversies in the Treatment Strategies of Intertrochanteric Fractures: A Scoping Review and Discussion of a Literature-Based Algorithm. J. Clin. Med. 2025, 14, 2200. https://doi.org/10.3390/jcm14072200
Graulich T, Omar M, Sehmisch S, Liodakis E. Controversies in the Treatment Strategies of Intertrochanteric Fractures: A Scoping Review and Discussion of a Literature-Based Algorithm. Journal of Clinical Medicine. 2025; 14(7):2200. https://doi.org/10.3390/jcm14072200
Chicago/Turabian StyleGraulich, Tilman, Mohamed Omar, Stephan Sehmisch, and Emmanouil Liodakis. 2025. "Controversies in the Treatment Strategies of Intertrochanteric Fractures: A Scoping Review and Discussion of a Literature-Based Algorithm" Journal of Clinical Medicine 14, no. 7: 2200. https://doi.org/10.3390/jcm14072200
APA StyleGraulich, T., Omar, M., Sehmisch, S., & Liodakis, E. (2025). Controversies in the Treatment Strategies of Intertrochanteric Fractures: A Scoping Review and Discussion of a Literature-Based Algorithm. Journal of Clinical Medicine, 14(7), 2200. https://doi.org/10.3390/jcm14072200






