Effectiveness of Occupational Therapy Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Middle-Aged and Older People with Chronic Stroke: A Systematic Review with Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information and Database Search Process
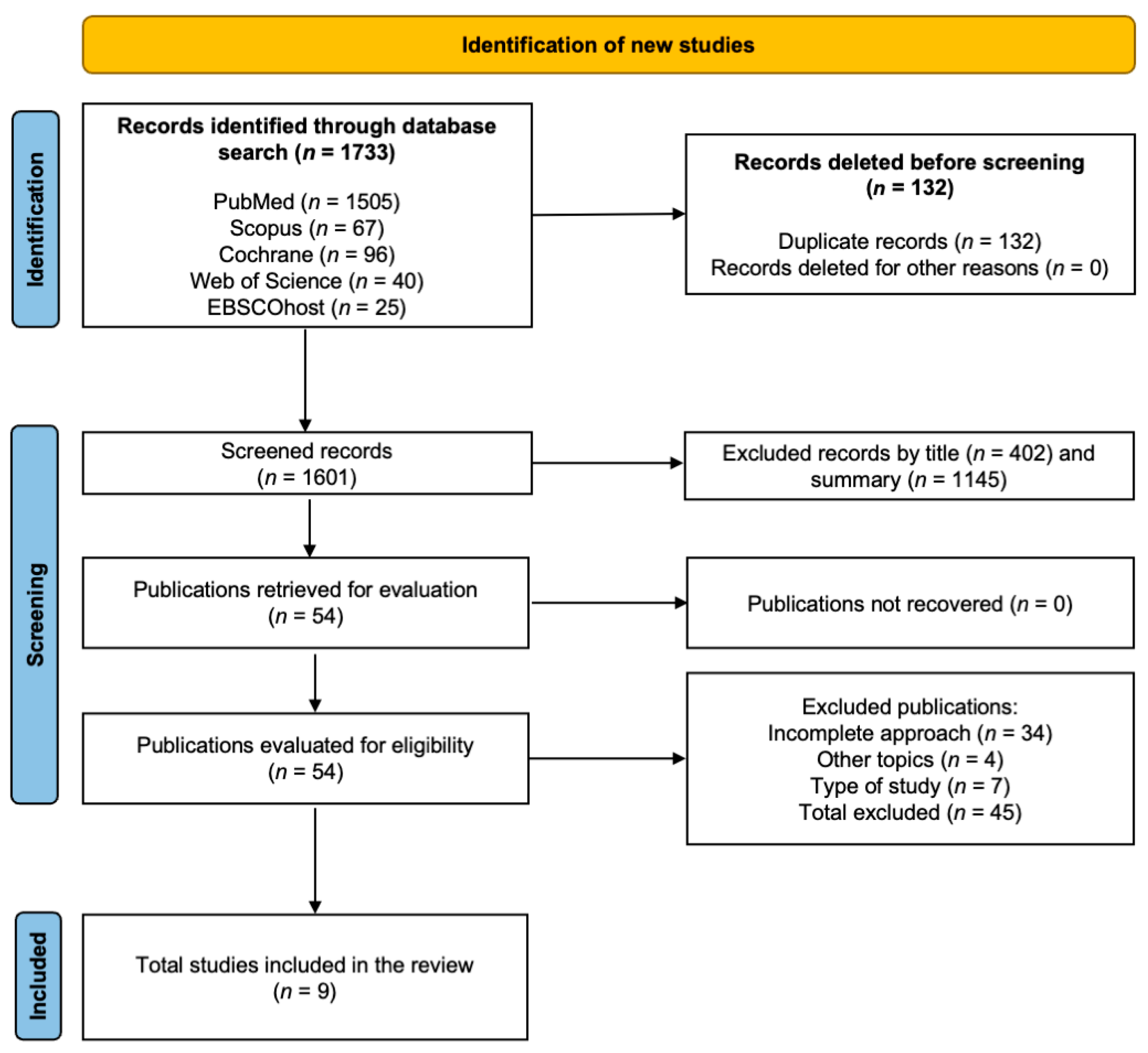
2.4. Study Selection and Data Collection Process
2.5. Methodological Quality Assessment
2.6. Data Extraction
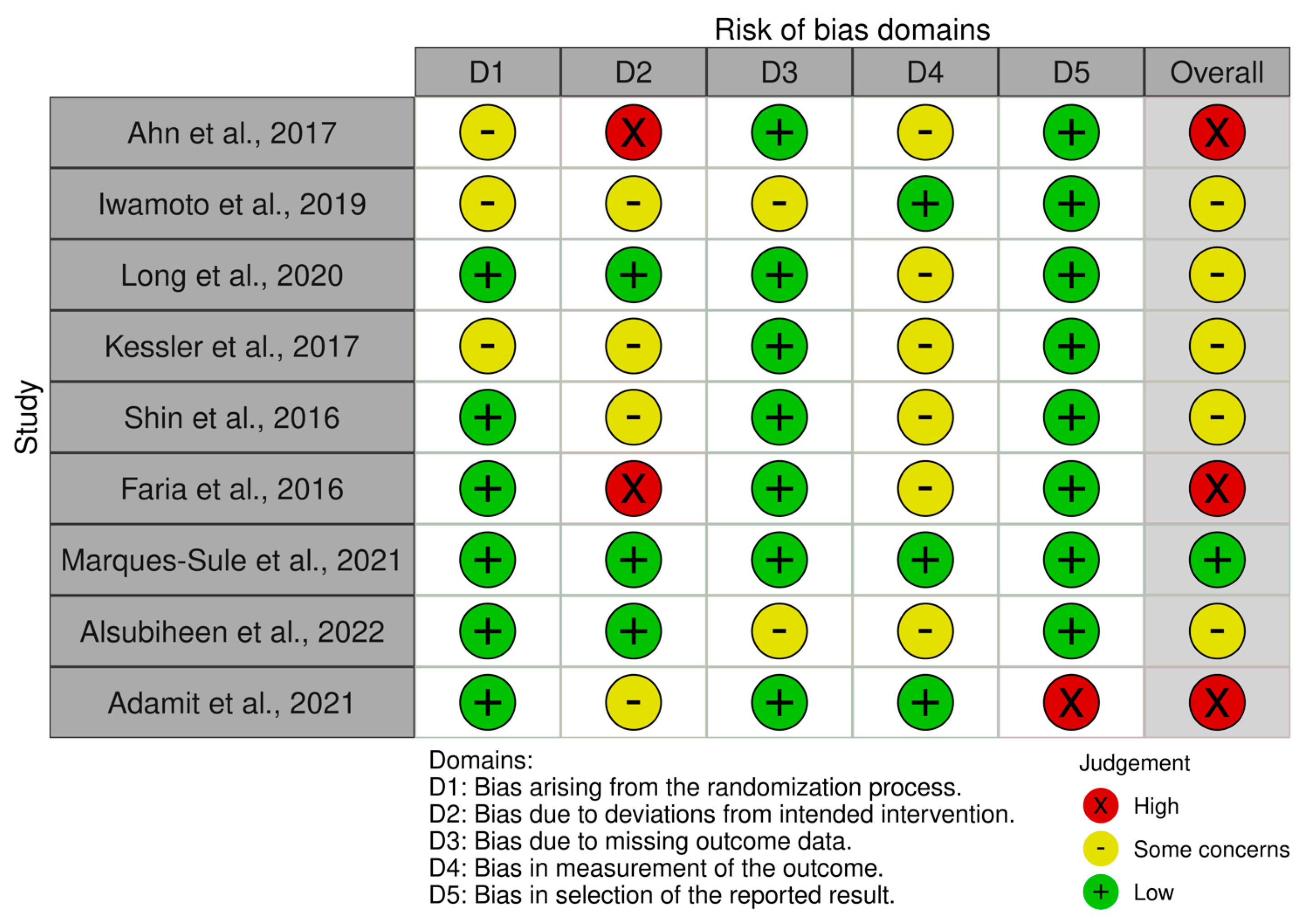
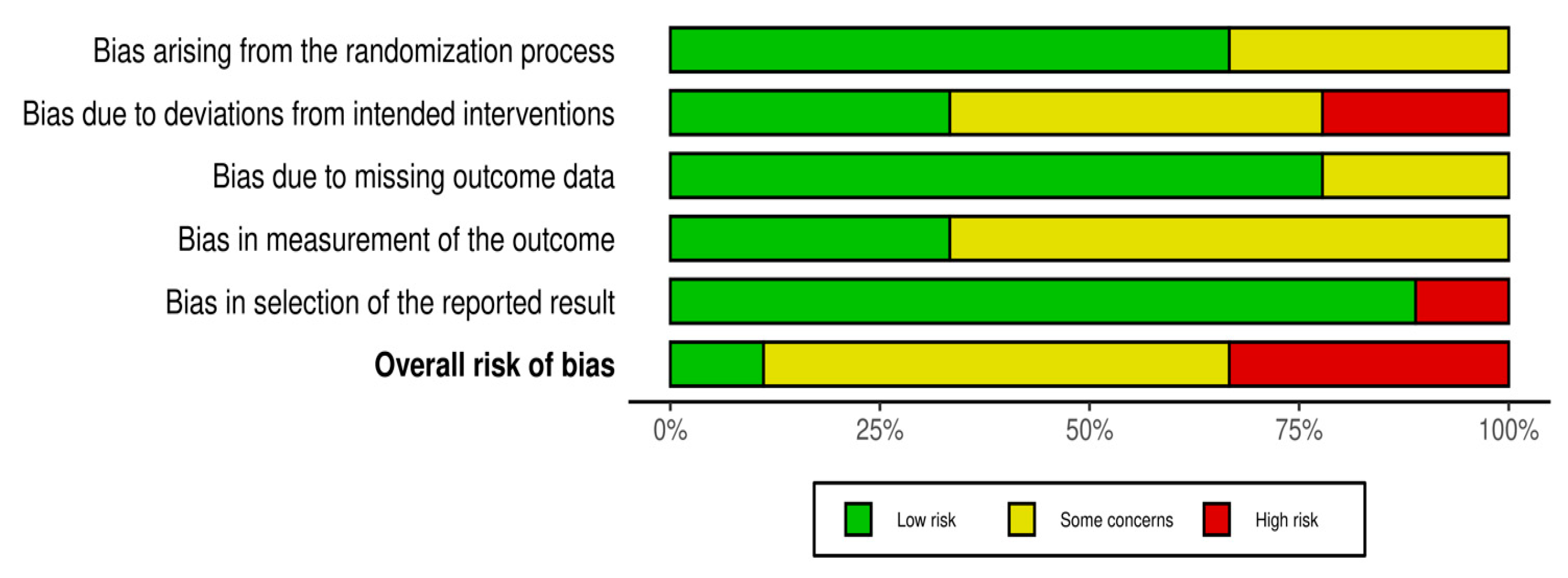
2.7. Risk of Bias Assessment
2.8. Meta-Analysis Measures
2.9. Certainty of Evidence
3. Results
3.1. Methodological Quality
3.2. Risks of Bias Within Studies
3.3. Characteristics of the Studies
3.4. Sample Characteristics
3.5. Dosages and Interventions Performed
3.6. Activities of Daily Living
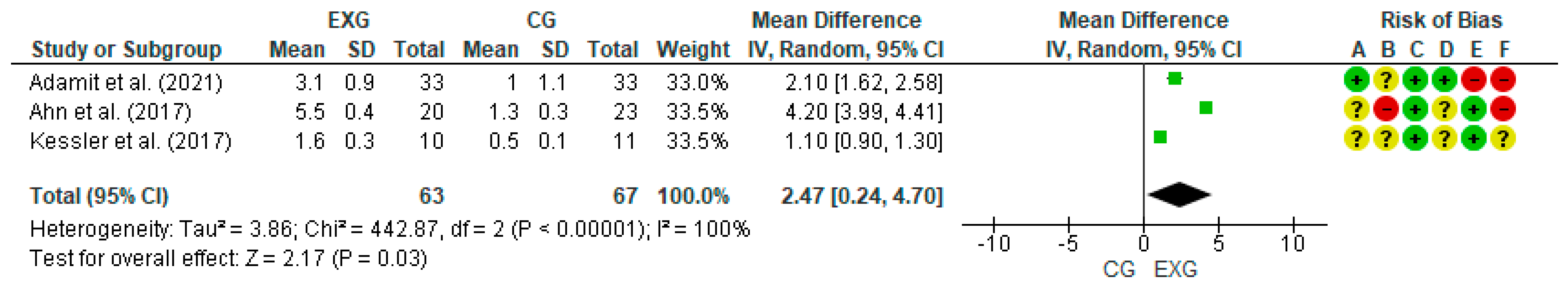
3.7. Cognitive Function
3.8. Physical Function
3.9. Certainty of Evidence
3.10. Adverse Effects and Adherence
4. Discussion
4.1. Activities of Daily Living
4.2. Cognitive Function
4.3. Physical Function
4.4. Limitations and Strengths
4.5. Practical Applications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Reveals Leading Causes of Death and Disability Worldwide: 2000–2019. 2020. Available online: https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019 (accessed on 4 November 2022).
- World Stroke Organization. Global Stroke Fact Sheet 2022. 2022. Available online: https://www.world-stroke.org/assets/downloads/WSO_Global_Stroke_Fact_Sheet.pdf (accessed on 4 November 2022).
- Elendu, C.; Amaechi, D.C.; Elendu, T.C.; Ibhiedu, J.O.; Egbunu, E.O.; Ndam, A.R.; Ogala, F.; Ologunde, T.; Peterson, J.C.; Boluwatife, A.I.; et al. Stroke and Cognitive Impairment: Understanding the Connection and Managing Symptoms. Ann. Med. Surg. 2023, 85, 6057–6066. [Google Scholar] [CrossRef] [PubMed]
- American Stroke Association. Stroke Rehabilitation. 2023. Available online: https://www.stroke.org/en/life-after-stroke/stroke-rehab (accessed on 1 August 2024).
- World Federation of Occupational Therapists (WFOT). Definition of Occupational Therapy. Available online: https://wfot.org/about (accessed on 18 December 2024).
- Kotler, J.M.; Mahoney, D.; Nilsen, D.M.; Gillen, G. Effectiveness of occupational therapy interventions to improve performance and participation in instrumental activities of daily living (IADL) among adult stroke survivors (2009–2019). Am. J. Occup. Ther. 2023, 77 (Suppl. S1), 7710393090. [Google Scholar] [CrossRef] [PubMed]
- Yamakawa, S.; Nagayama, H.; Tomori, K.; Ikeda, K.; Niimi, A. Effectiveness of Active Occupational Therapy in Patients with Acute Stroke: A Propensity Score-Weighted Retrospective Study. Front. Rehabil. Sci. 2023, 3, 1045231. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, M.W.; Geller, D.; Proffitt, R. Occupational therapy practice guidelines for adults with stroke. Am. J. Occup. Ther. 2023, 77, 7705397010. [Google Scholar] [CrossRef] [PubMed]
- Tedla, J.S.; Gular, K.; Reddy, R.S.; de Sá Ferreira, A.; Rodrigues, E.C.; Kakaraparthi, V.N.; Gyer, G.; Sangadala, D.R.; Qasheesh, M.; Kovela, R.K.; et al. Effectiveness of Constraint-Induced Movement Therapy (CIMT) on Balance and Functional Mobility in the Stroke Population: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 495. [Google Scholar] [CrossRef]
- Gibson, E.; Koh, C.L.; Eames, S.; Bennett, S.; Scott, A.M.; Hoffmann, T.C. Occupational Therapy for Cognitive Impairment in Stroke Patients. Cochrane Database Syst. Rev. 2022, 3, CD006430. [Google Scholar] [CrossRef]
- Landim, S.F.; López, R.; Caris, A.; Castro, C.; Castillo, R.D.; Avello, D.; Magnani Branco, B.H.; Valdés-Badilla, P.; Carmine, F.; Sandoval, C.; et al. Effectiveness of Virtual Reality in Occupational Therapy for Post-Stroke Adults: A Systematic Review. J. Clin. Med. 2024, 13, 4615. [Google Scholar] [CrossRef]
- The American Occupational Therapy Association. Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. Am. J. Occup. Ther. 2020, 74 (Suppl. S2), 7412410010p1–7412410010p87. [Google Scholar] [CrossRef]
- Su, F.; Xu, W. Enhancing brain plasticity to promote stroke recovery. Front. Neurol. 2020, 11, 554089. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, L. Robotic technologies in occupational therapy for stroke: Enhancing motor training and remote access. J. Rehabil. Robot. 2022, 19, 45–58. [Google Scholar]
- Higgins, J.P.T.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Chapter 8: Assessing Risk of Bias in a Randomized Trial. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; John Wiley & Sons: Chichester, UK, 2023. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. 2021, 74, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Manterola, C.; Zavando, D. Cómo interpretar los “Niveles de Evidencia” en los diferentes escenarios clínicos. Rev. Chil. Cir. 2009, 61, 582–595. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, v6.3; Cochrane: London, UK, 2022; Available online: https://training.cochrane.org/handbook (accessed on 4 November 2024).
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying Heterogeneity in a Meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Ahn, S.; Jung, M.; Park, H.; Lee, J.; Choi, Y.; Yoo, E. Comparison of Cognitive Orientation to daily Occupational Performance and conventional occupational therapy on occupational performance in individuals with stroke: A randomized controlled trial. NeuroRehabilitation 2017, 40, 285–292. [Google Scholar] [CrossRef]
- Iwamoto, Y.; Imura, T.; Suzukawa, T.; Fukuyama, H.; Ishii, T.; Taki, S.; Koyama, Y.; Matsumura, A.; Onodera, H.; Shibuya, K. Combination of exoskeletal upper limb robot and occupational therapy improve activities of daily living function in acute stroke patients. J. Stroke Cerebrovasc. Dis. 2019, 28, 2018–2025. [Google Scholar] [CrossRef]
- Long, Y.; Ouyang, R.G.; Zhang, J.Q. Effects of virtual reality training on occupational performance and self-efficacy of patients with stroke: A randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 150. [Google Scholar] [CrossRef]
- Kessler, D.; Egan, M.; Dubouloz, C.J.; McEwen, S.; Graham, F.P. Occupational performance coaching for stroke survivors: A pilot randomized controlled trial. Am. J. Occup. Ther. 2017, 71, 7103190020p1–7103190020p7. [Google Scholar] [CrossRef]
- Shin, J.H.; Kim, M.Y.; Lee, J.Y.; Jeon, Y.J.; Kim, S.; Lee, S.; Choi, Y.H.; Song, M.K.; Jang, S.H. Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: A single-blinded, randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 17. [Google Scholar] [CrossRef]
- Faria, A.L.; Andrade, A.; Soares, L.; Badia, I.S.B. Benefits of virtual reality based cognitive rehabilitation through simulated activities of daily living: A randomized controlled trial with stroke patients. J. Neuroeng. Rehabil. 2016, 13, 96. [Google Scholar] [CrossRef]
- Marques-Sule, E.; Miró-Ferrer, S.; Muñoz-Gómez, E.; Bermejo-Fernández, A.; Juárez-Vela, R.; Gea-Caballero, V.; Martínez-Muñoz, M.D.C.; Espí-López, G.V. Physical Activity in Health Care Professionals as a Means of Primary Prevention of Cardiovascular Disease: A STROBE Compliant Cross-Sectional Study. Medicine 2021, 100, e26184. [Google Scholar] [CrossRef] [PubMed]
- Alsubiheen, A.M.; Choi, W.; Yu, W.; Lee, H. The Effect of Task-Oriented Activities Training on Upper-Limb Function, Daily Activities, and Quality of Life in Chronic Stroke Patients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 14125. [Google Scholar] [CrossRef] [PubMed]
- Adamit, T.; Shames, J.; Rand, D. Effectiveness of the Functional and Cognitive Occupational Therapy (FaCoT) Intervention for Improving Daily Functioning and Participation of Individuals with Mild Stroke: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2021, 18, 7988. [Google Scholar] [CrossRef]
- Legg, L.A.; Lewis, S.R.; Schofield-Robinson, O.J.; Drummond, A.; Langhorne, P. Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst. Rev. 2017, 7, CD003585. [Google Scholar] [CrossRef]
- Eraifej, J.; Clark, W.; France, B.; Desando, S.; Moore, D. Effectiveness of upper limb functional electrical stimulation after stroke for the improvement of activities of daily living and motor function: A systematic review and meta-analysis. Syst. Rev. 2017, 6, 40. [Google Scholar] [CrossRef]
- Ahmed, I.; Mustafaoglu, R.; Rossi, S.; Cavdar, F.A.; Agyenkwa, S.K.; Pang, M.Y.C.; Straudi, S. Non-invasive brain stimulation techniques for the improvement of upper limb motor function and performance in activities of daily living after stroke: A systematic review and network meta-analysis. Arch. Phys. Med. Rehabil. 2023, 104, 1683–1697. [Google Scholar] [CrossRef]
- Gao, Y.; Qiu, Y.; Yang, Q.; Tang, S.; Gong, J.; Fan, H.; Wu, Y.; Lu, X. Repetitive Transcranial Magnetic Stimulation Combined with Cognitive Training for Cognitive Function and Activities of Daily Living in Patients with Post-Stroke Cognitive Impairment: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2023, 87, 101919. [Google Scholar] [CrossRef]
- Leong, S.C.; Tang, Y.M.; Toh, F.M.; Fong, K.N.K. Examining the effectiveness of virtual, augmented, and mixed reality (VAMR) therapy for upper limb recovery and activities of daily living in stroke patients: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2022, 19, 93. [Google Scholar] [CrossRef]
- Chen, X.; Liu, F.; Lin, S.; Yu, L.; Lin, R. Effects of virtual reality rehabilitation training on cognitive function and activities of daily living of patients with poststroke cognitive impairment: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2022, 103, 1422–1435. [Google Scholar] [CrossRef]
- O’Donoghue, M.; Leahy, S.; Boland, P.; Galvin, R.; McManus, J.; Hayes, S. Rehabilitation of cognitive deficits poststroke: Systematic review and meta-analysis of randomized controlled trials. Stroke 2022, 53, 1700–1710. [Google Scholar] [CrossRef]
- Loetscher, T.; Potter, K.J.; Wong, D.; das Nair, R. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst. Rev. 2019, 2019, CD002842. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Yang, H.; Zhou, Q.; Pan, H. Effects of cognitive motor dual-task training on stroke patients: A RCT-based meta-analysis. J. Clin. Neurosci. 2021, 92, 175–182. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Yang, L.; Zhou, J.; Yao, L.; Pang, M.Y.C. Dual-task training effects on motor and cognitive functional abilities in individuals with stroke: A systematic review. Clin. Rehabil. 2018, 32, 865–877. [Google Scholar] [CrossRef] [PubMed]
| Category | Inclusion | Exclusion |
|---|---|---|
| Population | Studies that were conducted in the chronic stroke population with a mean age of 45 years or more. | Studies with populations whose central pathology is other than a CVA (brain injury, multiple sclerosis, ALS, or other neurological or neurodegenerative condition) and under 45 years of age. |
| Intervention | Studies involving interventions or programs of OT from 4 weeks onwards. | Studies whose focus of intervention was not related to OT interventions |
| Comparison | Interventions with active or inactive control groups. | Lack of reference and/or follow-up data. Absence of control group. |
| Outcome | At least one assessment of ADLs or cognitive function or physical function. | Does not present any follow-up assessment. |
| Study design | Randomized controlled trial studies. | Non-randomized, cross-sectional, retrospective, and prospective controlled studies. |
| Authors | Country or Multicenter | Groups (n) |
Mean Age (Years) | Type of Intervention and Control Group | Training Volume |
Training Intensity | Assessments | Main Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Weeks | Frequency (Sessions/Week) |
Session Duration (Minutes) | ||||||||
| [21] | South Korea | Total: 43 EG: 20 CG: 23 | 52.6 years old | EG: CO-OP approach CG: Conventional occupational therapy | 5 | NR | NR | NR | COPM and PQRS | COPM-Performance: ↑ p < 0.001 COPM-Satisfaction: ↑ p < 0.001 PQRS: ↑ p < 0.001 |
| [22] | Japan | Total: 30 EG: 15 CG: 15 | 61.2 years old | EG: received training with the HAL in combination with occupational therapy CG: received only occupational therapy without the HAL | 2 | 5 | 40 min | NR | Br-stage, FIM and MAL | Both groups: ↔ Upper Limb Motor Function (Br-stage) (p = 0.003) EG: ↑ Dressing of Upper Body (FIM) (p = 0.046) ↑ Amount of Use-Putting Arm Through Sleeve (MAL) (p = 0.023) ↑ Quality of Movement (p = 0.043) ↑ Motor Sub score (FIM) (p = 0.009) CG: ↔ No significant changes in ADL assessments (p > 0.05) |
| [23] | China | Total: 52 EG: 25 CG: 27 | 53 years old | EG: VR training using the Doctor Kinetic system CG: Standard rehabilitation without VR | 3 | 5 | 45 min | NR | MBI and FMA-UE | Both groups: ↔ ADL (MBI) (p = 0.030) EG: ↑ MBI (p < 0.000) ↑ FMA-UE (p < 0.000) CG: ↑ MBI (p < 0.000) ↑ FMA-UE (p < 0.000) |
| [24] | Canada | Total: 21 EG: 10 CG: 11 | 57.4 years old | Determine the potential effectiveness of OPC-Stroke. EC: OPC–Stroke plus usual care. CG: Usual care only. | 16 | 10 | NR | NR | COPM, GSAB-DFI, MoCA and RNLI | EG: ↑ COPM Performance (p < 0.001) ↑ COPM Satisfaction (p < 0.001) ↔ GSAB–DFI (p = 0.731) ↔ MoCA (p = 0.070) ↔ RNLI (p = 0.231) CG: ↑ COPM-Performance (p < 0.001) ↑ COPM-Satisfaction (p < 0.001) ↔ GSAB–DFI (p = 0.819) ↔ MoCA (p = 0.065) ↔ RNLI (p = 0.212) |
| [25] | South Korea | Total: 48 EG: 24 CG: 24 | 58.3 years old | EG: SG using the RAPAEL Smart Glove™ for distal upper extremity rehabilitation CG: CON involving standard range of motion and strengthening exercises, tabletop activities, and training for ADLs | 4 | 5 | 30 min | No reported | FM, JTT and SIS | EG: ↔ FM-total (T0: 53.4 ± 1.8, T2: 58.3 ± 1.7, p < 0.001) ↑ FM-total (T3: 58.5 ± 1.7, p = 0.001) ↑ FM-prox (T2: 32.5 ± 0.9, p = 0.001) ↑ FM-prox (T3: 32.7 ± 0.9, p = 0.001) ↑ JTT-total (p = 0.032) ↑ JTT-gross (p = 0.025) ↑ Composite SIS (T2: 36.7 ± 10.0, p = 0.001) CG: ↔ FM-total (T0: 48.2 ± 2.6, T2: 49.6 ± 2.7, p = 0.512) ↔ FM-total (T3: 49.5 ± 2.7, p = 0.592) ↔ FM-prox (T2: 28.9 ± 1.4, p = 0.538) ↔ JTT-total ↔ JTT-gross ↔ Composite SIS (T2: 1.9 ± 10.5, p = 0.856) |
| [26] | Portugal | Total: 18 EG: 9 CG: 9 | 55.1 years old | EG: VR training simulation of activities of daily living (Reh@City) CG: Time-matched conventional cognitive training (paper-and-pencil tasks). | 4–6 | 3–4 | 20 min | NR | ACE, MMSE and SIS | Both groups: ↔ ADL (SIS) (p = does not specify) EG: ↑ Global cognitive functioning (ACE) (p = 0.014) ↑ Attention (p = 0.040) ↑ Memory (p = does not specify) ↑ Visuo-spatial abilities (p = does not specify) ↑ Physical domain (Strength) (p = 0.017) ↑ Physical domain (Mobility) (p = 0.012) ↑ MMSE (p = 0.050) CG: ↓ Verbal fluency (p = does not specify) ↔ Memory self-report (p = does not specify) ↔ Social participation (p = does not specify) ↔ MMSE (p = does not specify) |
| [27] | Spain | Total: 29 EG: 15 CG: 14 | 66.4 years old | EG: VR training WiiG CG: CPTG | 8 | 3 | 60 | Moderate | BBS, BI, FAI, POMA, and TUG | BBS: ↑ p < 0.01 BI: ↑ p < 0.01 FAI: ↑ p < 0.001 POMA-Total: ↑ p < 0.001 POMA-Gait: ↑ p < 0.01 POMA-Balance: ↑ p < 0.01 TUG: ↑ p < 0.001 |
| [28] | South Korea | Total: 33 EG: 15 CG: 15 | Middle age: 52.6 years old | EG: CO-OP approach CG: Conventional occupational therapy | 8 | 5 | 45 | Moderate | K-MBI and MFT | K-MBI: ↑ p < 0.001 MFT: ↑ p = 0.050 |
| [29] | Israel | Total: 66 EG: 33 CG: 33 | Mean age: 64.6 years old | EG: FaCoT intervention CG: Standard care | 12 | 3 | 60 | Moderate | COPM | COPM-Performance: ↑ p < 0.001 COPM-Satisfaction: ↑ p < 0.001 |
| Certainty of Evidence | Nº of Patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nº of Studies | Study Design | Risk Assessment | Inconsistency | Indirect Evidence | Vagueness | Other Considerations | [Conventional Therapy Plus Virtual Reality] | [Conventional Therapy] | Relative (95% CI) | Absolute (95% CI) | ||
| Comparison of cognitive orientation to daily occupational performance and conventional occupational therapy on occupational performance in individuals with stroke: A randomized controlled trial | ||||||||||||
| 1 | RCT | Very serious | It is not serious | It is not serious | It is not serious | None | 20/43 (46.5%) | 23/43 (53.5%) | Not estimable | ++ Go down | IMPORTANT | |
| Combination of Exoskeletal Upper Limb Robot and Occupational Therapy Improve Activities of Daily Living Function in Acute Stroke Patients | ||||||||||||
| 1 | RCT | Serious | It is not serious | It is not serious | It is not serious | None | 15/30 (50.0%) | 15/30 (50.0%) | Not estimable | +++ Moderate | IMPORTANT | |
| Effects of Virtual Reality Training on Occupational Performance and Self-Efficacy of Patients with Stroke: A Randomized Controlled Trial | ||||||||||||
| 1 | RCT | Serious | It is not serious | It is not serious | It is not serious | None | 25/52 (48.1%) | 27/52 (51.9%) | Not estimable | +++ Moderate | IMPORTANT | |
| Occupational Performance Coaching for Stroke Survivors: A Pilot Randomized Controlled Trial | ||||||||||||
| 1 | RCT | Serious | It is not serious | It is not serious | It is not serious | None | 10/21 (47.6%) | 11/21 (52.4%) | Not estimable | +++ Moderate | IMPORTANT | |
| Effects of virtual reality-based rehabilitation on distal upper extremity function and health-related quality of life: a single-blinded, randomized controlled trial | ||||||||||||
| 1 | RCT | Serious | It is not serious | It is not serious | It is not serious | None | 24/48 (50.0%) | 24/48 (50.0%) | Not estimable | +++ Moderate | IMPORTANT | |
| Benefits of Virtual Reality-Based Cognitive Rehabilitation Through Simulated Activities of Daily Living: A Randomized Controlled Trial with Stroke Patients | ||||||||||||
| 1 | RCT | Very serious | It is not serious | It is not serious | It is not serious | None | 9/18 (50.0%) | 9/18 (50.0%) | Not estimable | ++ Go down | IMPORTANT | |
| Effectiveness of Nintendo Wii and Physical Therapy in Functionality, Balance, and Daily Activities in Chronic Stroke Patients | ||||||||||||
| 1 | RCT | It is not serious | It is not serious | It is not serious | It is not serious | None | 15/29 (51.7%) | 14/29 (48.3%) | Not estimable | ++++ High | IMPORTANT | |
| The Effect of Task-Oriented Activities Training on Upper-Limb Function, Daily Activities, and Quality of Life in Chronic Stroke Patients: A Randomized Controlled Trial | ||||||||||||
| 1 | RCT | Serious | It is not serious | It is not serious | It is not serious | None | 15/30 (50.0%) | 15/30 (50.0%) | Not estimable | +++ Moderate | IMPORTANT | |
| Effectiveness of the Functional and Cognitive Occupational Therapy (FaCoT) Intervention for Improving Daily Functioning and Participation of Individuals with Mild Stroke: A Randomized Controlled Trial | ||||||||||||
| 1 | RCT | Very serious | It is not serious | It is not serious | It is not serious | None | 33/66 (50.0%) | 33/66 (50.0%) | Not estimable | ++ Low | IMPORTANT | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vásquez-Carrasco, E.; Jamett-Oliva, P.; Hernandez-Martinez, J.; Riquelme-Hernández, C.; Villagrán-Silva, F.; Branco, B.H.M.; Sandoval, C.; Valdés-Badilla, P. Effectiveness of Occupational Therapy Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Middle-Aged and Older People with Chronic Stroke: A Systematic Review with Meta-Analysis. J. Clin. Med. 2025, 14, 2197. https://doi.org/10.3390/jcm14072197
Vásquez-Carrasco E, Jamett-Oliva P, Hernandez-Martinez J, Riquelme-Hernández C, Villagrán-Silva F, Branco BHM, Sandoval C, Valdés-Badilla P. Effectiveness of Occupational Therapy Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Middle-Aged and Older People with Chronic Stroke: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2025; 14(7):2197. https://doi.org/10.3390/jcm14072197
Chicago/Turabian StyleVásquez-Carrasco, Edgar, Pía Jamett-Oliva, Jordan Hernandez-Martinez, Cristóbal Riquelme-Hernández, Francisca Villagrán-Silva, Braulio Henrique Magnani Branco, Cristian Sandoval, and Pablo Valdés-Badilla. 2025. "Effectiveness of Occupational Therapy Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Middle-Aged and Older People with Chronic Stroke: A Systematic Review with Meta-Analysis" Journal of Clinical Medicine 14, no. 7: 2197. https://doi.org/10.3390/jcm14072197
APA StyleVásquez-Carrasco, E., Jamett-Oliva, P., Hernandez-Martinez, J., Riquelme-Hernández, C., Villagrán-Silva, F., Branco, B. H. M., Sandoval, C., & Valdés-Badilla, P. (2025). Effectiveness of Occupational Therapy Interventions on Activities of Daily Living, Cognitive Function, and Physical Function in Middle-Aged and Older People with Chronic Stroke: A Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 14(7), 2197. https://doi.org/10.3390/jcm14072197