Perioperative Outcomes and Trends of Surgical Correction of Male Urethral Strictures: Results from the GRAND Study
Abstract
1. Introduction
2. Methods
2.1. Data Source: German Nationwide Inpatient Data (GRAND)
2.2. Study Population and Outcomes
2.3. Statistical Analysis
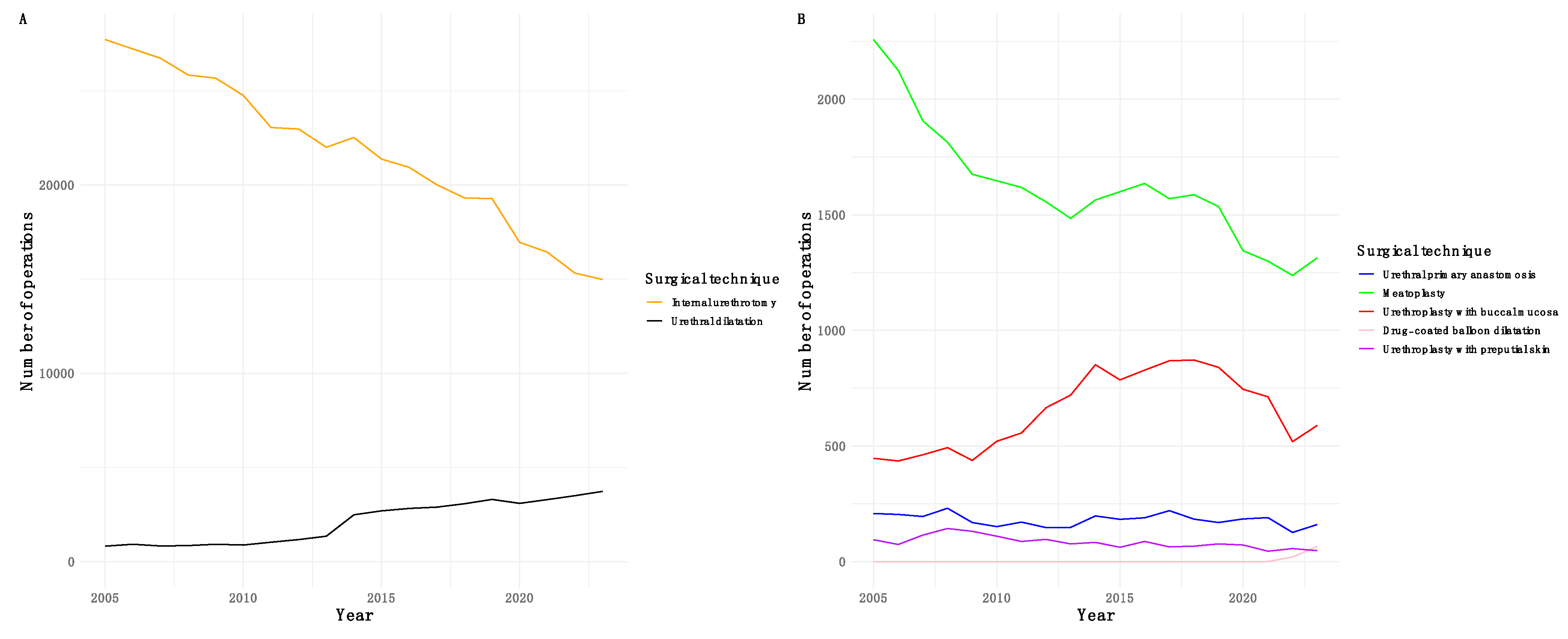
3. Results
3.1. Baseline Characteristics
3.2. Comparison of Outcomes: Urethroplasty with Buccal Mucosa Versus Preputial Skin
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Latini, J.M.; McAninch, J.W.; Brandes, S.B.; Chung, J.Y.; Rosenstein, D. SIU/ICUD Consultation On Urethral Strictures: Epidemiology, etiology, anatomy, and nomenclature of urethral stenoses, strictures, and pelvic fracture urethral disruption injuries. Urology 2014, 83 (Suppl. 3), S1–S7. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.M.; Thum, D.J.; Barbagli, G.; Kulkarni, S.; Sansalone, S.; Pardeshi, A.; Gonzalez, C.M. A geographic analysis of male urethral stricture aetiology and location. BJU Int. 2013, 112, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Alwaal, A.; Blaschko, S.D.; McAninch, J.W.; Breyer, B.N. Epidemiology of urethral strictures. Transl. Androl. Urol. 2014, 3, 209–213. [Google Scholar] [CrossRef]
- Palminteri, E.; Berdondini, E.; Verze, P.; De Nunzio, C.; Vitarelli, A.; Carmignani, L. Contemporary urethral stricture characteristics in the developed world. Urology 2013, 81, 191–196. [Google Scholar] [CrossRef]
- Patel, H.V.; Li, K.D.; Rourke, K.F.; Smith, T.G.; Voelzke, B.B.; Myers, J.B.; Broghammer, J.A.; Alsikafi, N.F.; Buckley, J.C.; Zhao, L.C.; et al. The Impact of Social Deprivation on Anterior Urethral Stricture Recurrence After Urethroplasty: A Trauma and Urologic Reconstructive Network of Surgeons Analysis. J. Urol. 2024, 212, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Purohit, R.S.; Golan, R.; Copeli, F.; Weinberger, J.; Benedon, M.; Mekel, G.; Blaivas, J.G. Natural History of Low-stage Urethral Strictures. Urology 2017, 108, 180–183. [Google Scholar] [CrossRef]
- Lumen, N.; Campos-Juanatey, F.; Greenwell, T.; Martins, F.E.; Osman, N.I.; Riechardt, S.; Waterloos, M.; Barratt, R.; Chan, G.; Esperto, F.; et al. European Association of Urology Guidelines on Urethral Stricture Disease (Part 1): Management of Male Urethral Stricture Disease. Eur. Urol. 2021, 80, 190–200. [Google Scholar] [CrossRef]
- Jackson, M.J.; Sciberras, J.; Mangera, A.; Brett, A.; Watkin, N.; N’Dow, J.M.; Chapple, C.R.; Andrich, D.E.; Pickard, R.S.; Mundy, A.R. Defining a patient-reported outcome measure for urethral stricture surgery. Eur. Urol. 2011, 60, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Campos-Juanatey, F.; Osman, N.I.; Greenwell, T.; Martins, F.E.; Riechardt, S.; Waterloos, M.; Barratt, R.; Chan, G.; Esperto, F.; Ploumidis, A.; et al. European Association of Urology Guidelines on Urethral Stricture Disease (Part 2): Diagnosis, Perioperative Management, and Follow-up in Males. Eur. Urol. 2021, 80, 201–212. [Google Scholar] [CrossRef]
- Hampson, L.A.; McAninch, J.W.; Breyer, B.N. Male urethral strictures and their management. Nat. Rev. Urol. 2014, 11, 43–50. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kluth, L.A.; Ernst, L.; Vetterlein, M.W.; Meyer, C.P.; Reiss, C.P.; Fisch, M.; Rosenbaum, C.M. Direct Vision Internal Urethrotomy for Short Anterior Urethral Strictures and Beyond: Success Rates, Predictors of Treatment Failure, and Recurrence Management. Urology 2017, 106, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.S.W.; Aboumarzouk, O.M.; Narahari, R.; O’Riordan, A.; Pickard, R. Simple urethral dilatation, endoscopic urethrotomy, and urethroplasty for urethral stricture disease in adult men. Cochrane Database Syst. Rev. 2012, 12, CD006934. [Google Scholar] [CrossRef]
- DeLong, J.; Virasoro, R.; Pichardo, M.; Estrella, R.; Rodríguez Lay, R.; Espino, G.; Elliott, S. Long-Term Outcomes of Recurrent Bulbar Urethral Stricture Treatment With the Optilume Drug-Coated Balloon: Five-Year Results From the ROBUST I Study. J. Urol. 2025, 213, 90–98. [Google Scholar] [CrossRef]
- Pang, K.H.; Chapple, C.R.; Chatters, R.; Downey, A.P.; Harding, C.K.; Hind, D.; Watkin, N.; Osman, N.I. A Systematic Review and Meta-analysis of Adjuncts to Minimally Invasive Treatment of Urethral Stricture in Men. Eur. Urol. 2021, 80, 467–479. [Google Scholar] [CrossRef]
- Nilsen, O.J.; Holm, H.V.; Ekerhult, T.O.; Lindqvist, K.; Grabowska, B.; Persson, B.; Sairanen, J. To Transect or Not Transect: Results from the Scandinavian Urethroplasty Study, A Multicentre Randomised Study of Bulbar Urethroplasty Comparing Excision and Primary Anastomosis Versus Buccal Mucosal Grafting. Eur. Urol. 2022, 81, 375–382. [Google Scholar] [CrossRef]
- Wessells, H.; Morey, A.; Souter, L.; Rahimi, L.; Vanni, A. Urethral Stricture Disease Guideline Amendment (2023). J. Urol. 2023, 210, 64–71. [Google Scholar] [CrossRef] [PubMed]
- McGeorge, S.; Chung, A.; Desai, D.J. Trends in urethral stricture management over two decades. BJU Int. 2019, 124 (Suppl. 1), 37–41. [Google Scholar] [CrossRef]
- Johnsen, N.V.; Holt, S.K.; Wingate, J.T. National Trends in the Management of Urethral Stricture Disease. Urol. Pract. 2020, 7, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Naud, E.; Rourke, K. Recent Trends and Advances in Anterior Urethroplasty. Urol. Clin. N. Am. 2022, 49, 371–382. [Google Scholar] [CrossRef]
- Pyrgidis, N.; Moschini, M.; Tzelves, L.; Somani, B.K.; Juliebø-Jones, P.; Del Giudice, F.; Mertens, L.S.; Pichler, R.; Volz, Y.; Ebner, B.; et al. Perioperative Outcomes and Trends in Transurethral Resection of Bladder Tumors with Photodynamic Diagnosis: Results from the GeRmAn Nationwide Inpatient Data Study. J. Clin. Med. 2024, 13, 3531. [Google Scholar] [CrossRef]
- Ostrovsky, A.M.; Prebay, Z.J.; Chung, P.H. Trends in Male and Female Urethral Endoscopic Management and Urethroplasty Using the TriNetX Database. J. Clin. Med. 2023, 12, 2137. [Google Scholar] [CrossRef]
- Hillary, C.J.; Osman, N.I.; Chapple, C.R. Current trends in urethral stricture management. Asian J. Urol. 2014, 1, 46–54. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Elliott, S.P.; Coutinho, K.; Robertson, K.J.; D’Anna, R.; Chevli, K.; Carrier, S.; Aube-Peterkin, M.; Cantrill, C.H.; Ehlert, M.J.; Te, A.E.; et al. One-Year Results for the ROBUST III Randomized Controlled Trial Evaluating the Optilume® Drug-Coated Balloon for Anterior Urethral Strictures. J. Urol. 2022, 207, 866–875. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.L.; García-Perdomo, H.A.; Robayo, J.A. Alternatives to oral mucosa grafts for urethral reconstruction. Nat. Rev. Urol. 2023, 20, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Sterling, J.; Simhan, J.; Flynn, B.J.; Rusilko, P.; França, W.A.; Ramirez, E.A.; Angulo, J.C.; Martins, F.E.; Patel, H.V.; Higgins, M.; et al. Multi-Institutional Outcomes of Dorsal Onlay Buccal Mucosal Graft Urethroplasty in Patients With Postprostatectomy, Postradiation Anastomotic Stenosis. J. Urol. 2024, 211, 596–604. [Google Scholar] [CrossRef]
- Ayangbesan, A.; Koch, G.E.; Dagostino, C.; Proctor, J.M.; Gambrah, H.; Bhalla, R.G.; Bonnet, K.; Schlundt, D.; Johnsen, N.V. Qualitative Analysis of Patient Experiences Reaching Urethroplasty for Recurrent Urethral Stricture Disease. J. Urol. 2024, 211, 153–162. [Google Scholar] [CrossRef]
- Tyagi, S.; Parmar, K.M.; Singh, S.K.; Sharma, A.; Shukla, M.; Sharma, A.P.; Devana, S.K.; Sharma, G.; Kumar, S.; Mandal, A.K. ’Pee’BuSt Trial: A single-centre prospective randomized study comparing functional and anatomic outcomes after augmentation urethroplasty with penile skin graft versus buccal mucosa graft for anterior urethral stricture disease. World J. Urol. 2022, 40, 475–481. [Google Scholar] [CrossRef]
- Sharma, A.K.; Chandrashekar, R.; Keshavamurthy, R.; Nelvigi, G.G.; Kamath, A.J.; Sharma, S.; Venkatesh, G.K. Lingual versus buccal mucosa graft urethroplasty for anterior urethral stricture: A prospective comparative analysis. Int. J. Urol. 2013, 20, 1199–1203. [Google Scholar] [CrossRef]
- Sharma, G.; Sharma, S.; Parmar, K. Buccal mucosa or penile skin for substitution urethroplasty: A systematic review and meta-analysis. Indian J. Urol. 2020, 36, 81–88. [Google Scholar] [CrossRef]
- Erickson, B.A.; Tuong, M.N.; Zorn, A.N.; Schlaepfer, C.H.; Alsikafi, N.F.; Breyer, B.N.; Broghammer, J.A.; Buckley, J.C.; Elliott, S.P.; Myers, J.B.; et al. Development and Validation of the Length, Segment, and Etiology Anterior Urethral Stricture Disease Staging System Using Longitudinal Urethroplasty Outcomes Data From the Trauma and Urologic Reconstruction Network of Surgeons. J. Urol. 2025, 213, 512–523. [Google Scholar] [CrossRef]
- Anderson, K.T.; Vanni, A.J.; Erickson, B.A.; Myers, J.B.; Voelzke, B.; Breyer, B.N.; Broghammer, J.A.; Buckley, J.C.; Zhao, L.C.; Smith, T.G.; et al. Defining Success after Anterior Urethroplasty: An Argument for a Universal Definition and Surveillance Protocol. J. Urol. 2022, 208, 135–143. [Google Scholar] [CrossRef]
- Frankiewicz, M.; Cocci, A.; Vetterlein, M.W.; Verla, W.; Campos-Juanatey, F.; Castiglione, F.; Mantica, G.; Rosenbaum, C.M.; Waterloos, M.; Adamowicz, J.; et al. Urethroscopic Findings Following Urethroplasty Predict the Need for Secondary Intervention in the Long Term: A Multi-Institutional Study From Trauma and Urologic Reconstructive Network of Surgeons. Letter. J. Urol. 2022, 208, 957–958. [Google Scholar] [CrossRef] [PubMed]
- Cotter, K.J.; Hahn, A.E.; Voelzke, B.B.; Myers, J.B.; Smith, T.G.; Elliott, S.P.; Alsikafi, N.F.; Breyer, B.N.; Vanni, A.J.; Buckley, J.C.; et al. Trends in Urethral Stricture Disease Etiology and Urethroplasty Technique From a Multi-institutional Surgical Outcomes Research Group. Urology 2019, 130, 167–174. [Google Scholar] [CrossRef]
- Babu, P.; Nayak, A.; Javali, T.D.; Joshi, P.; Nagaraj, H.K.; Aggarwal, K. Evaluation of Jordan’s meatoplasty for the treatment of fossa navicularis strictures. A retrospective study. Cent. Eur. J. Urol. 2017, 70, 103–106. [Google Scholar] [CrossRef]
- Shakir, N.A.; Fuchs, J.S.; Haney, N.; Viers, B.R.; Cordon, B.H.; McKibben, M.; Scott, J.; Armenakas, N.A.; Morey, A.F. Excision and Primary Anastomosis Reconstruction for Traumatic Strictures of the Pendulous Urethra. Urology 2019, 125, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Zhao, W.; Yang, M.; Fang, W.; Gao, G.; Wang, Y.; Fu, Q. Cell-Based Therapy for Urethral Regeneration: A Narrative Review and Future Perspectives. Biomedicines 2023, 11, 2366. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hoare, D.T.; Doiron, R.C.; Rourke, K.F. The evolution of urethral stricture and urethroplasty practice over 15 years: A single-center, single-surgeon, 1319 urethroplasty analysis. Can. Urol. Assoc. J. 2022, 16, 289–293. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guo, Y.; Ma, N.; Zhang, J.; Chen, S.; Liu, P.; Yang, Z.; Li, Y. Surgical Management of Anterior Urethral Stricture: A 23-year Single-Center Study. Res. Rep. Urol. 2025, 17, 31–42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Characteristic | Urethral Primary Anastomosis, n = 3428 | Urethral Dilatation, n = 39,619 | Meatoplasty, n = 30,774 | Urethroplasty with Buccal Mucosa, n = 12,351 | Drug-coated Balloon Dilatation, n = 85 | Urethroplasty with Preputial Skin, n = 1585 | Internal Urethrotomy, n = 413,095 |
|---|---|---|---|---|---|---|---|
| Age (years) | 53 (35–68) | 71 (61–79) | 65 (44–74) | 55 (40–68) | 71 (58–77) | 56 (40–69) | 71 (62–78) |
| Benign prostatic hyperplasia | 160 (4.7%) | 11,299 (29%) | 8849 (29%) | 451 (3.7%) | XXX | XXX | 130,556 (32%) |
| Diabetes | 312 (9.1%) | 8044 (20%) | 4582 (15%) | 1316 (11%) | 11 (13%) | 175 (11%) | 73,292 (18%) |
| Chronic heart failure | 66 (1.9%) | 2898 (7.3%) | 1048 (3.4%) | 199 (1.6%) | 6 (7.1%) | 25 (1.6%) | 21,236 (5.1%) |
| Chronic kidney disease | 162 (4.7%) | 5235 (13%) | 1947 (6.3%) | 481 (3.9%) | 10 (12%) | 61 (3.8%) | 38,767 (9.4%) |
| Hypertension | 1013 (30%) | 20,517 (52%) | 11,343 (37%) | 4225 (34%) | 33 (39%) | 522 (33%) | 199,048 (48%) |
| Obesity | 181 (5.3%) | 2554 (6.4%) | 1623 (5.3%) | 666 (5.4%) | 3 (3.5%) | 83 (5.2%) | 22,861 (5.5%) |
| Hospital stay (days) | 7 (5–11) | 4.0 (2–7) | 4 (2–6) | 7 (6–11) | 3 (2–4) | 7 (6–10) | 4 (3–7) |
| Reimbursement (EUR) | 4789 (4583–5331) | 2245 (1821–3250) | 6856 (5884–7336) | 2001 (1920–2191) | 4711 (4363–5316) | 2239 (1904–3045) | 4789 (4583–5331) |
| Age group | |||||||
| <50 | 1491 (43%) | 4636 (12%) | 8570 (28%) | 4710 (38%) | 12 (14%) | 601 (38%) | 39,245 (9.5%) |
| 50–59 | 552 (16%) | 3943 (10%) | 3336 (11%) | 2278 (18%) | 11 (13%) | 256 (16%) | 40,169 (9.7%) |
| 60–69 | 587 (17%) | 7875 (20%) | 6328 (21%) | 2448 (20%) | 16 (19%) | 294 (19%) | 89,700 (22%) |
| 70–79 | 604 (18%) | 12,597 (32%) | 8197 (27%) | 2409 (20%) | 26 (31%) | 329 (21%) | 148,164 (36%) |
| Year of surgery | |||||||
| 2005 | 208 (6.1%) | 821 (2.1%) | 2258 (7.3%) | 447 (3.6%) | 0 (0%) | 94 (5.9%) | 27,718 (6.7%) |
| 2006 | 204 (6.0%) | 921 (2.3%) | 2124 (6.9%) | 435 (3.5%) | 0 (0%) | 74 (4.7%) | 27,229 (6.6%) |
| 2007 | 195 (5.7%) | 829 (2.1%) | 1906 (6.2%) | 462 (3.7%) | 0 (0%) | 115 (7.3%) | 26,736 (6.5%) |
| 2008 | 231 (6.7%) | 849 (2.1%) | 1814 (5.9%) | 493 (4.0%) | 0 (0%) | 143 (9.0%) | 25,843 (6.3%) |
| 2009 | 169 (4.9%) | 918 (2.3%) | 1676 (5.4%) | 438 (3.5%) | 0 (0%) | 131 (8.3%) | 25,676 (6.2%) |
| 2010 | 151 (4.4%) | 878 (2.2%) | 1647 (5.4%) | 521 (4.2%) | 0 (0%) | 110 (6.9%) | 24,759 (6.0%) |
| 2011 | 171 (5.0%) | 1030 (2.6%) | 1619 (5.3%) | 556 (4.5%) | 0 (0%) | 87 (5.5%) | 23,051 (5.6%) |
| 2012 | 147 (4.3%) | 1167 (2.9%) | 1556 (5.1%) | 666 (5.4%) | 0 (0%) | 96 (6.1%) | 22,971 (5.6%) |
| 2013 | 148 (4.3%) | 1347 (3.4%) | 1485 (4.8%) | 720 (5.8%) | 0 (0%) | 77 (4.9%) | 22,006 (5.3%) |
| 2014 | 198 (5.8%) | 2480 (6.3%) | 1564 (5.1%) | 852 (6.9%) | 0 (0%) | 83 (5.2%) | 22,519 (5.5%) |
| 2015 | 183 (5.3%) | 2692 (6.8%) | 1600 (5.2%) | 786 (6.4%) | 0 (0%) | 62 (3.9%) | 21,377 (5.2%) |
| 2016 | 189 (5.5%) | 2821 (7.1%) | 1636 (5.3%) | 828 (6.7%) | 0 (0%) | 87 (5.5%) | 20,935 (5.1%) |
| 2017 | 220 (6.4%) | 2888 (7.3%) | 1570 (5.1%) | 869 (7.0%) | 0 (0%) | 63 (4.0%) | 20,009 (4.8%) |
| 2018 | 184 (5.4%) | 3076 (7.8%) | 1587 (5.2%) | 872 (7.1%) | 0 (0%) | 67 (4.2%) | 19,317 (4.7%) |
| 2019 | 169 (4.9%) | 3297 (8.3%) | 1536 (5.0%) | 840 (6.8%) | 0 (0%) | 76 (4.8%) | 19,275 (4.7%) |
| 2020 | 185 (5.4%) | 3089 (7.8%) | 1344 (4.4%) | 745 (6.0%) | 0 (0%) | 72 (4.5%) | 16,947 (4.1%) |
| 2021 | 190 (5.5%) | 3295 (8.3%) | 1300 (4.2%) | 713 (5.8%) | 0 (0%) | 45 (2.8%) | 16,434 (4.0%) |
| 2022 | 126 (3.7%) | 3495 (8.8%) | 1238 (4.0%) | 519 (4.2%) | 20 (24%) | 56 (3.5%) | 15,318 (3.7%) |
| 2023 | 160 (4.7%) | 3723 (9.4%) | 1314 (4.3%) | 589 (4.8%) | 65 (76%) | 47 (3.0%) | 14,975 (3.6%) |
| Outcome | Urethroplasty with Buccal Mucosa | Urethroplasty with Preputial Skin | ||
|---|---|---|---|---|
| Cases | Estimate (95% CI), p-Value | Cases | Estimate (95% CI), p-Value | |
| Transfusion | 52 (0.4%) | — | 12 (0.8%) | 1.81 (0.92, 3.29), 0.07 |
| Sepsis | 27 (0.2%) | — | 4 (0.3%) | 1.2 (0.34, 3), 0.8 |
| Length of hospital stay | 7 (6–11) | — | 7 (6–10) | −0.4 (−0.7, −0.05), 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bischoff, R.; Marcon, J.; Schulz, G.B.; Stief, C.G.; Keller, P.; Eismann, L.; Weinhold, P.; Pyrgidis, N. Perioperative Outcomes and Trends of Surgical Correction of Male Urethral Strictures: Results from the GRAND Study. J. Clin. Med. 2025, 14, 2171. https://doi.org/10.3390/jcm14072171
Bischoff R, Marcon J, Schulz GB, Stief CG, Keller P, Eismann L, Weinhold P, Pyrgidis N. Perioperative Outcomes and Trends of Surgical Correction of Male Urethral Strictures: Results from the GRAND Study. Journal of Clinical Medicine. 2025; 14(7):2171. https://doi.org/10.3390/jcm14072171
Chicago/Turabian StyleBischoff, Robert, Julian Marcon, Gerald Bastian Schulz, Christian G. Stief, Patrick Keller, Lennert Eismann, Philipp Weinhold, and Nikolaos Pyrgidis. 2025. "Perioperative Outcomes and Trends of Surgical Correction of Male Urethral Strictures: Results from the GRAND Study" Journal of Clinical Medicine 14, no. 7: 2171. https://doi.org/10.3390/jcm14072171
APA StyleBischoff, R., Marcon, J., Schulz, G. B., Stief, C. G., Keller, P., Eismann, L., Weinhold, P., & Pyrgidis, N. (2025). Perioperative Outcomes and Trends of Surgical Correction of Male Urethral Strictures: Results from the GRAND Study. Journal of Clinical Medicine, 14(7), 2171. https://doi.org/10.3390/jcm14072171





