Abstract
Background/Objectives: Identifying key psychological well-being factors in morbid obesity is crucial for designing effective mental health and weight management interventions. This study explores the interconnections between the dimensions of psychological well-being in a large sample of adults with morbid obesity enrolled in an inpatient nutritional rehabilitation program. Methods: A sample of 3212 participants (F = 58%; mean age = 57.18 years; mean Body Mass Index = 43.40 kg/m2) completed the Psychological General Well-Being Index (PGWBI) upon admission to the clinic. A network analysis approach examined the relationships among the PGWBI dimensions (anxiety, depression, positive well-being, self-control, vitality, and general health). Results: Network analysis revealed that vitality and positive well-being exhibited the highest values across closeness (1.432; 0.353), strength (0.853; 0.917), and expected influence (0.853; 0917), indicating their key role in psychological well-being. Depression also demonstrated moderate relevance, suggesting its connection to other well-being factors, though it was not the primary determinant. In contrast, self-control and general health had negative strength and expected influence values (−0.660; −1.641), indicating a less central role in the network. Additionally, anxiety and depression displayed negative betweenness (−0.645), reinforcing their more peripheral position. Conversely, positive well-being and vitality showed the highest betweenness (1.291), highlighting their role as key connecting nodes within the well-being network. Conclusions: Findings suggest interventions targeting positive well-being and vitality may most effectively enhance psychological well-being in morbid obesity, emphasizing strength-based approaches that foster positive affect, motivation, and resilience rather than focusing solely on reducing distress or weight-related concerns.
1. Introduction
The prevalence of morbid obesity has steadily increased worldwide, posing significant challenges to public health and economic stability due to its substantial healthcare costs [1,2]. Defined as a Body Mass Index (BMI) ≥ 40 or ≥35 kg/m2 with obesity-related health conditions, this complex metabolic disorder is associated with severe comorbidities, including cardiovascular disease, type 2 diabetes, sleep apnea, osteoarthritis, and various types of cancer [3]. Furthermore, obesity is a chronic, relapsing condition that often persists despite multiple interventions [4,5,6].
Beyond its well-documented physical burdens, obesity has a profound impact on mental health. Individuals with severe obesity experience higher rates of depression [7], anxiety [8,9,10], and reduced self-esteem and overall well-being [11,12,13]. Stigmatization is also pervasive across various aspects of life [14,15,16], including interpersonal relationships [17,18,19], education, employment [20], healthcare settings [21,22], and even everyday activities, such as being able to fit into public seating [23]. This social marginalization further deteriorates psychological well-being [24]. Additionally, psychological distress can hinder adherence to dietary recommendations and behavioral changes essential for weight management [25,26]. Despite the clear connection between obesity and mental health, healthcare systems often prioritize acute medical conditions and weight loss over comprehensive well-being, leading to fragmented and insufficient care that leaves many patients dissatisfied [27,28].
Psychological well-being is a crucial construct in health research, encompassing emotional, cognitive, and social dimensions of life [29,30]. It is recognized as an independent predictor of morbidity and mortality, both in healthy individuals and clinical populations, and includes those with severe obesity [31,32,33].
Traditionally, mental health research has treated psychopathology (e.g., depression and anxiety) and subjective well-being (e.g., life satisfaction and positive emotion) as distinct domains. However, emerging evidence suggests they are interrelated and should be examined together for a more comprehensive understanding of mental health [34,35].
Existing research often explores linear relationships between psychological factors and weight-related outcomes [36]. Such approaches may overlook the intricate and dynamic interplay between these variables. Identification of the most influential aspects of psychological well-being in individuals with morbid obesity is essential for the development of targeted interventions that enhance both mental health and weight management. This calls for innovative analytical frameworks that capture these complexities [37].
Network analysis provides a novel approach by mapping interconnections between psychological dimensions, offering deeper insight into how different aspects of well-being influence each other in individuals with morbid obesity. Unlike traditional analyses, which primarily examine isolated pairwise associations, network analysis identifies central psychological components, distinguishes direct from indirect relationships, and visually represents interactions, enhancing interpretability of results [38,39]. By revealing key nodes and pathways within the psychological network, this methodology helps clarify how dimensions of well-being interact and reinforce one another.
This study applies network analysis to explore the interconnections between the dimensions of psychological well-being (anxiety, depression, positive well-being, self-control, vitality, and general health) in adults with morbid obesity enrolled in an intensive inpatient nutritional rehabilitation program. By identifying the most influential psychological factors within this population, we aim to contribute to a more nuanced understanding of well-being in the context of severe obesity and inform the design of more effective, patient-centered interventions.
2. Materials and Methods
2.1. Participants and Procedures
Participants were individuals with morbid obesity who were enrolled in a 4-week multidisciplinary nutritional rehabilitation program at the IRCCS, Istituto Auxologico Italiano in Verbania, Italy.
The program included individualized nutritional intervention, psychological support, and supervised physical activity. Each patient received a balanced, hypocaloric Mediterranean diet consisting of three meals a day with 18–20% protein, 27–30% fat (of which <8% was saturated fat), and 50–55% carbohydrates (<15% simple sugars), and 30 g of fiber from fresh vegetables. Under the supervision of a physiotherapist, they performed 60-min physiotherapy sessions twice a day comprising aerobic training, postural control exercises, and strengthening exercises. Additionally, they attended weekly individual and group psychological support sessions.
Subjects were eligible for the study if they met the following criteria: age ≥ 18 years; BMI greater than 40 kg/m2 or above 35 kg/m2 with obesity-related health conditions; ability to understand the study’s purpose and sign an informed consent for research participation; and completion of the Psychological General Well-Being Index (PGWBI) [40,41]. Exclusion criteria included the presence of mental, cognitive, or visual impairments that could interfere with completing the questionnaire.
The data used in this research were obtained from archival records. During their initial consultation with a physician, patients provided informed consent to participate in the rehabilitation program, which also included explicit approval for the use of their data for research purposes. This standard procedure ensured ethical compliance and transparency in the collection and use of patient information.
On the same day as the initial consultation, a clinical psychologist assessed the inclusion and exclusion criteria and administered the PGWBI as part of a routine clinical evaluation. Data were collected from January 2018 to December 2022. This study was approved by the Ethical Committee of Istituto Auxologico Italiano, IRCCS, in Milan, Italy (approval number: 03C020; date of approval: 18 February 2020). Research was carried out according to the Declaration of Helsinki and its advancements.
2.2. Measures
Weight and height were measured on the second day of admission to calculate BMI. Standing height was determined by a Harpenden Stadiometer (Holstein Limited, Crymych, Dyfed, UK). Weight was measured to the nearest 0.1 kg using an electronic scale (RoWU 150, Wunder Sa.bi., Trezzo sull’Adda, Italy). Demographics (gender and age) were also collected, and the Italian version of the PGWBI was used to measure psychological well-being.
The Psychological General Well-Being Index (PGWBI) [40,41] is a widely used self-report measure designed to assess a person’s level of subjective psychological well-being. In detail, it assesses self-representations of intrapersonal affective or emotional states reflecting a sense of subjective well-being or distress, and thus captures what we could call a subjective perception of well-being. The PGWBI consists of 22 standardized items rated on a 6-point Likert scale, with responses ranging from 0 (indicating severe distress or negative feelings) to 5 (indicating positive feelings or well-being). The tool produces a single measure of psychological well-being and also provides subscales to assess the following domains: Anxiety (5 items) assesses levels of tension, worry, and nervousness. Higher scores indicate lower anxiety and a greater sense of calm (“Have you felt tense and nervous?”). Depression (3 items) evaluates feelings of sadness, discouragement, and hopelessness. A higher score reflects a more positive mood and fewer depressive symptoms (“Have you felt downhearted and unhappy?”). Positive well-being (4 items)measures feelings of happiness, life satisfaction, and optimism. A higher score suggests a greater sense of overall well-being and emotional positivity (“Have you felt happy, satisfied with life?”). Self-control (3 items) examines an individual’s ability to regulate emotions and behavior, reflecting stability and resilience. Higher scores indicate better emotional regulation and perceived control over one’s life (“Have you felt in control of yourself?). General health (3 items) assesses self-perceived physical health and vitality, including the impact of psychological distress on overall well-being. Higher scores suggest a stronger perception of good health (“How would you rate your health status?”). Vitality (4 items) captures energy levels and fatigue, reflecting overall vigor and enthusiasm for daily activities. Higher scores indicate greater energy and lower fatigue (“Have you felt full of energy?”).
The PGWBI is structured so that higher scores reflect lower levels of psychological distress and better emotional well-being. This means that higher scores on the anxiety and depression subscales indicate lower levels of anxiety and depression, respectively (no reverse scoring required). The total score is calculated by summing the responses across all items. The possible score range is between 0 and 110, with higher scores indicating better psychological well-being. PGWBI total scores are typically categorized into four well-being levels: severe distress, 0–60; moderate distress, 61–72; no distress/marginal well-being, 73–82; and positive well-being, ≥83. These cut-off points are used to classify individuals based on their psychological well-being, with lower scores indicating higher levels of psychological distress.
The PGWBI has been widely used across the world with both clinical and nonclinical samples [42,43,44]. The Italian-adapted version, developed by Grossi and colleagues [40], has shown strong internal consistency, with Cronbach’s alpha values between 0.94 and 0.96, confirming its reliability.
Similarly, in the present study, Cronbach’s alpha coefficients demonstrated strong internal consistency across all dimensions (total score: α = 0.94, anxiety: α = 0.91, depressed mood: α = 0.90, positive well-being: α = 0.92, self-control: α = 0.89, general health: α = 0.88, and vitality: α = 0.90).
2.3. Statistical Analysis
Data analyses were conducted using IBM SPSS Statistics for Windows, Version 23.0 [45]. Descriptive statistics were computed to summarize participant characteristics and the dimensions of the Psychological General Well-Being Index (PGWBI), and were presented as means and standard deviations or frequencies and percentages, as appropriate.
Moreover, given the normal distribution of the variables, the relationships between the six dimensions of the PGWBI (anxiety, depression, positive well-being, self-control, general health, and vitality) were examined using Pearson’s correlation coefficients and interpreted as weak (r = 0.1–0.3), moderate (r = 0.3–0.5), or strong (r > 0.5) [46]. The strength and direction of the correlations were analyzed to identify significant associations between dimensions and corresponding p-values were calculated. A significance level of p < 0.05 was used for all statistical tests.
In addition, a psychometric network analysis was performed using JASP (Version 0.19.0) [47] to disentangle the relationships among the six dimensions of the PGWBI. The analysis was performed using a Gaussian Graphical Model (GGM) with pairwise partial correlations representing the edges (relationships) between nodes (PGWBI dimensions) [48]. To minimize the presence of spurious connections, the network model was estimated using the Graphical Least Absolute Shrinkage and Selection Operator (GLASSO) regularization algorithm [49,50,51].
This approach constrains low correlation values to zero, resulting in a sparse network, by eliminating likely spurious connections. The GLASSO algorithm employs a tuning parameter (λ) to control the sparsity of the network, where higher λ values lead to greater sparsity [49,50,52]. Then, the Extended Bayesian Information Criterion (EBIC) was employed as a model-selection criterion to identify and retrieve the most optimal network structure. A γ hyperparameter was set to 0.5 to balance sensitivity and specificity in edge detection [53].
This EBIC–GLASSO approach has been recognized for its effectiveness in accurately reconstructing true network structures [54,55] in cases where the network is inherently sparse (i.e., contains relatively few connections). This method also demonstrates high specificity, effectively preventing the estimation of non-existent edges, though its sensitivity (i.e., accuracy in detecting existing connections) can vary.
Furthermore, the stability of the network model was assessed [56] using the correlation stability coefficient (CS-coefficient). CS-coefficient values higher or equal to 0.5 indicate optimal stability and values higher than 0.25 indicate moderate stability [56,57].
In addition, centrality measures were computed, including strength, closeness, betweenness, and expected influence. Strength centrality indicates the number of edges (relationships) connected to a node. Closeness centrality measures the proximity of a node to all other nodes, reflecting its level of accessibility within the network. Betweenness centrality measures interactions between nodes, depending on the other nodes that lie on the same path [58,59,60,61,62]. Last, expected influence accounts for the sum of all positive and negative connections of a node, providing insight into its overall impact on the network.
3. Results
3.1. Characteristics of the Sample
The study included 3.212 adult inpatients diagnosed with morbid obesity, with women representing 58% of the sample (n = 1.863). The participants had an average age of 57.18 years (SD = 14.11) and a mean BMI of 43.40 kg/m2 (SD = 5.66). Descriptive statistics of the sample are shown in Table 1 below.

Table 1.
Descriptive statistics of the sample.
3.2. Correlation Analysis
Table 2 presents the results of a correlation analysis exploring relationships among the six variables (depression, anxiety, positive well-being, self-control, general health, and vitality) that constitute the PGWBI. All correlations are positive and significant at the 0.01 level, indicating robust relationships across dimensions.

Table 2.
Correlations among the six dimensions of the PGWBI.
The strongest association was observed between positive well-being and vitality (r = 0.768). In addition, positive well-being showed high correlations with depression (r = 0.757) and anxiety (r = 0.720), which were also strongly related to each other (r = 0.746).
General health showed the lowest correlation indices with all the other variables; the weakest relationship was observed with self-control (r = 0.483).
3.3. Psychometric Network Analysis
3.3.1. Network Structure and Edge Weights
The network model estimated by the EBIC–GLASSO algorithm was constructed using network weights. The matrix of these weights is presented in Table 3 and includes only positive-edge weights across all connections. The strongest edge was observed between positive well-being and vitality (0.394), followed by the relationships between vitality and general health (0.385), and the edge between anxiety and depression (0.342). Moreover, a solid edge was observed between positive well-being and depression (0.298) and a moderately strong correlation was also identified between depression and self-control (0.246). Conversely, the weakest connection was found between general health and self-control (0.023), with the next weakest link being between vitality and depression (0.037). The results are reported in Table 3 and Figure 1.

Table 3.
Undirected weights matrix of the EBIC–GLASSO network model.
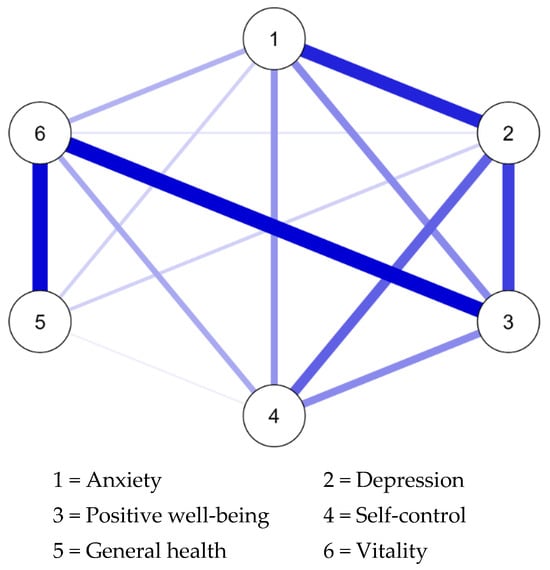
Figure 1.
Network visualization of the PGWBI dimensions.
3.3.2. Network Stability
Stability analyses indicated that the network model had excellent stability, with a CS coefficient of 0.75 for the edges. This implies that even if up to 75% of the participants were removed from the sample, the structure of the edges would remain stable (Figure 2).
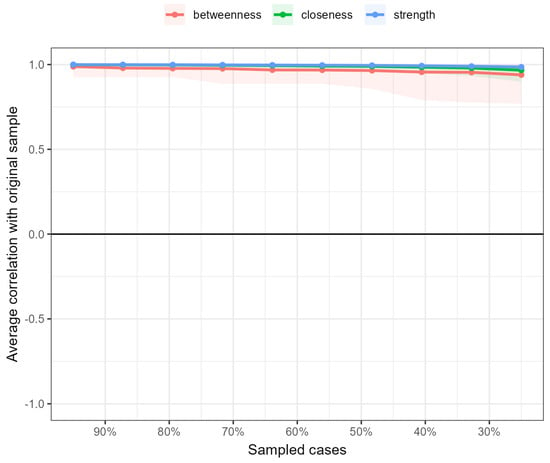
Figure 2.
Bootstrap stability analysis of centrality measures in the network.
Centrality indices indicated that vitality and positive well-being exhibited the highest values across all centrality measures, particularly in closeness, strength, and expected influence. Depression also demonstrated notable relevance, with moderate values in closeness, strength, and expected influence. In contrast, self-control and general health showed negative values for strength and expected influence. Along with anxiety and depression, they also displayed negative betweenness, suggesting a more peripheral role in the network. Moreover, positive well-being and vitality had the highest betweenness. The results are reported in Table 4 and Figure 3.

Table 4.
Centrality indices of PGWBI dimensions in the network model.
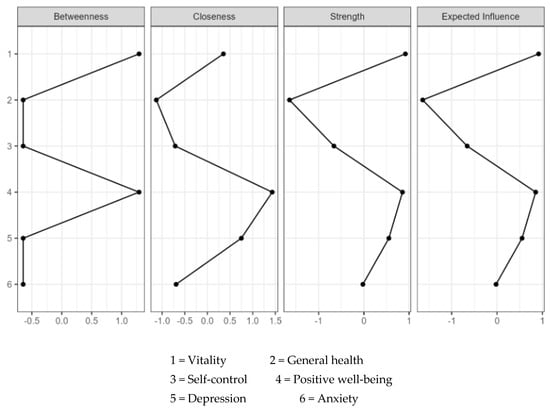
Figure 3.
Plots of the standardized centrality indices of the network analysis.
4. Discussion
Psychological well-being is increasingly acknowledged as a key determinant in morbid obesity, shaping both immediate and long-term health outcomes [29,63,64,65]. However, despite its well-established significance, its multifaceted nature makes it a complex and not-yet-fully-understood phenomenon. The present study aims to explore the psychological well-being of a sample of inpatients with morbid obesity through psychometric network analysis. This approach was used to reveal distinctive and potentially significant connections between different dimensions of psychological well-being assessed with the PGWBI.
A high association between the variables in this network is expected, as well-being encompasses closely related dimensions. This expectation is confirmed by the high number of non-zero edges (14 out of 15), suggesting strong interconnections among the measured constructs. Particularly noteworthy relationships emerged between positive well-being and vitality, reinforcing their theoretical and empirical link. Indeed, in the positive psychology literature, two distinct forms of positive well-being have been conceptualized: hedonic well-being and eudaimonic well-being. The first refers to positive emotions and overall life satisfaction and typically assesses the presence, frequency, and intensity of positive affect, offering insight into an individual’s subjective emotional experience. In contrast, eudaimonic well-being is associated with a sense of purpose, personal growth, and self-actualization. It reflects the emotions that arise when an individual moves toward their full potential, often assessed through indicators such as vitality, curiosity, and engagement [66]. Accordingly, the findings of the present study suggest that positive well-being and vitality exhibited the highest number of connections (strength), the greatest impact (expected influence), and were also more centrally positioned (higher closeness) within the network, thus functioning as core components of psychological well-being in individuals with morbid obesity.
These two dimensions may have differential effects on overall well-being; while positive well-being contributes to immediate emotional gratification, vitality may play a more sustained role in long-term psychological resilience and life satisfaction. This aligns with previous research indicating that positive well-being and vitality play a critical role in maintaining adherence to therapeutic programs, particularly in individuals with obesity, who often face challenges such as demotivation, stigma, and emotional distress [67,68]. Improving positive well-being could help sustain motivation and encourage active participation in treatment, thereby enhancing both psychological and physical health outcomes. Additionally, interventions that emphasize behavioral activation can boost, with wide-ranging effects, multiple aspects of psychological well-being. Indeed, vitality plays a pivotal role as a bridge connecting other dimensions within the network.
Another key result of this study is the moderate centrality of depression, which shows positive closeness, strength, and expected influence. This suggests that while depressive symptoms are connected to other well-being dimensions, they do not dominate the network. In other words, depression does not appear to be the primary driver of overall well-being in this model but, rather, interacts with other factors in a secondary role. These findings contrast with traditional models, where depression is often conceptualized as a core determinant of mental health [69,70], and suggest that reducing depressive symptoms alone may not be sufficient to enhance the overall well-being of a person. This aligns with the results of a meta-analysis of 26 studies [71] that suggest positive affect exerts a protective influence on health beyond the mere absence of emotional distress. In other words, well-being does not solely stem from the absence of negative emotions but also the presence of positive experiences and engagement [72,73,74]. These insights reinforce the importance of integrating positive psychological interventions that promote positive experiences, rather than solely reduce negative emotions, to enhance long-term well-being in individuals with morbid obesity.
Conversely, self-control and general health exhibited negative strength and expected influence values, suggesting that these dimensions play a less central role within the well-being network, potentially exerting their effects in more indirect or context-dependent ways. The peripheral position of general health is particularly noteworthy, indicating that perceived physical health may not be a primary driver of psychological well-being. These findings align with research highlighting that subjective health perception does not always directly influence psychological well-being [75,76,77] and reinforce the importance of integrating psychological interventions into obesity treatment programs, rather than focusing exclusively on weight reduction or medical management. Indeed, self-control displayed negative centrality values, suggesting that it does not function as a key integrative component within the well-being network in this population. This contrasts with studies that have highlighted the role of self-regulation in weight management and emotional well-being [78,79]. One possible explanation is that in individuals with morbid obesity, self-control may not be a primary determinant of psychological well-being, particularly if emotional distress, stigma, or learned helplessness mechanisms play a stronger role [80,81]. Moreover, the moderate connection between anxiety and depression is consistent with well-established findings that these two affective states frequently co-occur and share underlying cognitive and emotional mechanisms [82,83]. However, the network suggests that depression has stronger links to well-being factors like positive well-being and vitality, whereas anxiety appears to be less integrated into the overall well-being structure. This distinction may have implications for tailoring psychological interventions, as strategies aimed at reducing depression may also enhance well-being, whereas the impact of anxiety reduction on the broader well-being network might be less integrative than expected, possibly due to individual differences in coping mechanisms or resilience [84,85]. Interventions targeting these areas may, therefore, need a more individualized approach, rather than expecting a widespread impact on well-being.
The present study has notable strengths but also limitations that warrant discussion. The main strength of this study is the use of network analysis to investigate the interconnections between well-being dimensions in a large group of inpatients seeking treatment for morbid obesity. This methodology sheds light on how variables within the same construct interact and reinforce one another, offering deeper insight into the complex interplay between psychological processes involved in morbid obesity [38].
However, some limitations should be acknowledged. First, only one measure of psychological well-being was included. Additionally, the integration of additional variables, such as measures of eating disorders, body image, or self-efficacy, would have allowed for a more comprehensive understanding of the complex interrelationship between psychological factors in inpatients with morbid obesity. Furthermore, the inclusion of BMI would have allowed for the exploration of potential associations between psychological well-being and weight-related factors. Still, BMI is an external factor that does not function as a psychological dimension within the PGWBI structure, making it less suitable for inclusion in a network analysis designed to map relationships between psychological constructs, and should be investigated in further studies. Moreover, the cross-sectional nature of this study design hinders its ability to establish causality between relationships observed in the network and the lack of longitudinal data restricts its capacity to monitor changes in psychological well-being over time, including before and after the rehabilitation program. In addition, data were obtained from a single clinical center, requiring caution when generalizing the findings to other populations or settings. Specifically, these findings may not be generalizable to individuals with morbid obesity who are not actively seeking treatment for weight reduction and rehabilitation or to patients treated in different settings (i.e., outpatient or bariatric surgery). Future research should explore whether similar psychological well-being patterns emerge in non-treatment-seeking populations and across various clinical and community-based interventions to enhance the applicability of these results. Last, the study design does not permit us to draw conclusions about clinical implications, only to propose hypotheses that should be tested in future studies.
Despite these limitations, the findings of this study provide valuable insight for the implementation of tailored interventions targeting psychological well-being in morbid obesity.
Indeed, the strong interconnectedness of positive well-being and vitality suggests that targeting these dimensions in psychological interventions could yield widespread benefits across the well-being structure.
Depression plays a role, but it is not the primary driver of psychological well-being in this population. This underscores the importance of moving beyond a symptom-reduction model—which primarily focuses on mitigating distress—toward a broader framework that actively cultivates positive psychological states. To this aim, strategies such as positive psychology interventions [86] have been shown to reduce depressive symptoms while simultaneously enhancing overall well-being and resilience [87,88]. Additionally, exercise-based programs [89] have been associated with enhanced emotional regulation, increased self-efficacy, and reduced symptoms of depression and anxiety [90,91].
Mindfulness techniques [92], including meditation, body awareness, and acceptance-based strategies, may be particularly beneficial for individuals with obesity-related distress, as they have been found to reduce emotional distress and promote adaptive coping mechanisms [93,94]. In addition, interventions based on motivational interviewing (MI) [12,95] could further strengthen the ability to regulate behavior and emotion. MI has been widely applied in weight management and obesity treatment, demonstrating efficacy in enhancing intrinsic motivation for lifestyle changes, encouraging self-efficacy and autonomy in goal-setting, and addressing ambivalence toward behavior modification [96]. Additionally, MI techniques align with research on self-regulation and emotional competence, which suggests that greater behavioral control is associated with better emotional resilience and psychological well-being [97]. This makes MI an ideal complement to positive psychology interventions, ensuring that individuals not only experience greater positive affect and vitality, but also develop the cognitive and behavioral tools to sustain long-term improvement.
5. Conclusions
This is one of few studies available in the literature exploring psychological well-being in a large sample of adult inpatients with morbid obesity using a network analysis approach. Network analysis proves to be a valuable approach to personalize clinical intervention and identify critical areas for targeted action. By analyzing the interconnections among various dimensions of well-being, the findings provide valuable insight into the complex relationships that shape psychological well-being in this population. Overall, these findings highlight the dominance of positive well-being and vitality in shaping psychological health, emphasizing their importance in both theoretical models of well-being and practical intervention strategies. At the same time, the relatively peripheral roles of general health perception and anxiety suggest that well-being cannot be fully explained through physical health status or distress-related factors alone. Instead, a holistic strength-based approach that prioritizes positive emotional and behavioral engagement may be the most effective pathway to improving well-being in individuals with morbid obesity.
Author Contributions
Conceptualization, G.P.; methodology, G.P.; formal analysis, G.P.; data curation, A.B.; writing—original draft preparation, G.P., A.G.-U. and A.B.; writing—review and editing, A.B., V.V., G.C. and A.S. All authors have read and agreed to the published version of the manuscript.
Funding
The present work was funded by the Italian Ministry of Health—Ricerca Corrente.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Istituto Auxologico Italiano (approval number: 2020_02_18_04 on the date 18 April 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Phelps, N.H.; Singleton, R.K.; Zhou, B.; Heap, R.A.; Mishra, A.; Bennett, J.E.; Paciorek, C.J.; Lhoste, V.P.F.; Carrillo-Larco, R.M.; Stevens, G.A.; et al. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Nagi, M.A.; Ahmed, H.; Rezq, M.A.A.; Sangroongruangsri, S.; Chaikledkaew, U.; Almalki, Z.; Thavorncharoensap, M. Economic costs of obesity: A systematic review. Int. J. Obes. 2024, 48, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Cummings, D.E.; Eckel, R.H.; Cohen, R.V.; Wilding, J.P.; Brown, W.A.; Stanford, F.C.; Batterham, R.L.; Farooqi, I.S.; Farpour-Lambert, N.J.; et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025, 13, 221–262. [Google Scholar] [CrossRef]
- Burki, T. European Commission classifies obesity as a chronic disease. Lancet Diabetes Endocrinol. 2021, 9, 418. [Google Scholar] [CrossRef]
- Castelnuovo, G.; Capodaglio, P.; De Amicis, R.; Gilardini, L.; Mambrini, S.P.; Pietrabissa, G.; Cavaggioni, L.; Piazzolla, G.; Galeone, C.; Garavaglia, G.; et al. Study protocol of a clinical randomized controlled trial on the efficacy of an innovative Digital thErapy to proMote wEighT loss in patients with obesity by incReasing their Adherence to treatment: The DEMETRA study. Front. Digit. Health 2023, 5, 1159744. [Google Scholar] [CrossRef]
- Cattivelli, R.; Castelnuovo, G.; Musetti, A.; Varallo, G.; Spatola, C.A.M.; Riboni, F.V.; Usubini, A.G.; Tosolin, F.; Manzoni, G.M.; Capodaglio, P.; et al. ACTonHEALTH study protocol: Promoting psychological flexibility with activity tracker and mHealth tools to foster healthful lifestyle for obesity and other chronic health conditions. Trials 2018, 19, 659. [Google Scholar] [CrossRef]
- Debski, J.; Przybylowski, J.; Skibiak, K.; Czerwinska, M.; Waledziak, M.; Rozanska-Waledziak, A. Depression and Obesity-Do We Know Everything about It? A Narrative Review. Nutrients 2024, 16, 3383. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Bertuzzi, V.; Simpson, S.; Guerrini Usubini, A.; Cattivelli, R.; Bertoli, S.; Mozzi, E.; Roviaro, G.; Castelnuovo, G.; Molinari, E. Psychological Aspects of Treatment with Intragastric Balloon for Management of Obesity: A Systematic Review of the Literature. Obes. Facts 2022, 15, 1–18. [Google Scholar] [CrossRef]
- Amiri, S.; Behnezhad, S. Obesity and anxiety symptoms: A systematic review and meta-analysis. Neuropsychiatrie 2019, 33, 72–89. [Google Scholar] [CrossRef]
- Gomez-de-Regil, L.; Avila-Nava, A.; Gutierrez-Solis, A.L.; Lugo, R. Mobile Apps for the Management of Comorbid Overweight/Obesity and Depression/Anxiety: A Systematic Review. J. Healthc. Eng. 2020, 2020, 9317179. [Google Scholar] [CrossRef]
- Kokkinos, P.; Faselis, C.; Franklin, B.; Lavie, C.J.; Sidossis, L.; Moore, H.; Karasik, P.; Myers, J. Cardiorespiratory fitness, body mass index and heart failure incidence. Eur. J. Heart Fail. 2019, 21, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Pietrabissa, G.; Manzoni, G.M.; Rossi, A.; Castelnuovo, G. The MOTIV-HEART Study: A Prospective, Randomized, Single-Blind Pilot Study of Brief Strategic Therapy and Motivational Interviewing among Cardiac Rehabilitation Patients. Front. Psychol. 2017, 8, 83. [Google Scholar] [CrossRef] [PubMed]
- Sarwer, D.B.; Polonsky, H.M. The Psychosocial Burden of Obesity. Endocrinol. Metab. Clin. North. Am. 2016, 45, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Ryan, L.; Quigley, F.; Birney, S.; Crotty, M.; Conlan, O.; Walsh, J.C. ’Beyond the Scale’: A Qualitative Exploration of the Impact of Weight Stigma Experienced by Patients With Obesity in General Practice. Health Expect. 2024, 27, e14098. [Google Scholar] [CrossRef]
- Rao, A.; Puhl, R.; Farrar, K. Weight Stigma in Online News Images: A Visual Content Analysis of Stigma Communication in the Depictions of Individuals with Obesity in U.S. and U.K. News. J. Health Commun. 2024, 29, 95–106. [Google Scholar] [CrossRef]
- Rossi, A.A.; Manzoni, G.M.; Pietrabissa, G.; Di Pauli, D.; Mannarini, S.; Castelnuovo, G. Weight stigma in patients with overweight and obesity: Validation of the Italian Weight Self-Stigma Questionnaire (WSSQ). Eat. Weight Disord. 2022, 27, 2459–2472. [Google Scholar] [CrossRef]
- Puhl, R.M.; Himmelstein, M.S.; Pearl, R.L. Weight stigma as a psychosocial contributor to obesity. Am. Psychol. 2020, 75, 274–289. [Google Scholar] [CrossRef]
- Albano, G.; Rowlands, K.; Baciadonna, L.; Coco, G.L.; Cardi, V. Interpersonal difficulties in obesity: A systematic review and meta-analysis to inform a rejection sensitivity-based model. Neurosci. Biobehav. Rev. 2019, 107, 846–861. [Google Scholar] [CrossRef]
- Côté, M.; Bégin, C. Review of the Experience of Weight-Based Stigmatization in Romantic Relationships. Curr. Obes. Rep. 2020, 9, 280–287. [Google Scholar] [CrossRef]
- Täuber, S.; Mulder, L.B.; Flint, S.W. The impact of workplace health promotion programs emphasizing individual responsibility on weight stigma and discrimination. Front. Psychol. 2018, 9, 2206. [Google Scholar] [CrossRef]
- Crompvoets, P.I.; Nieboer, A.P.; van Rossum, E.F.C.; Cramm, J.M. Perceived weight stigma in healthcare settings among adults living with obesity: A cross-sectional investigation of the relationship with patient characteristics and person-centred care. Health Expect. 2024, 27, e13954. [Google Scholar] [CrossRef] [PubMed]
- Ryan, L.; Coyne, R.; Heary, C.; Birney, S.; Crotty, M.; Dunne, R.; Conlan, O.; Walsh, J.C. Weight stigma experienced by patients with obesity in healthcare settings: A qualitative evidence synthesis. Obes. Rev. 2023, 24, e13606. [Google Scholar] [CrossRef] [PubMed]
- Stunkard, A.J.; Wadden, T.A. Psychological aspects of severe obesity. Am. J. Clin. Nutr. 1992, 55, 524s–532s. [Google Scholar] [CrossRef] [PubMed]
- Crompvoets, P.I.; Nieboer, A.P.; van Rossum, E.F.C.; Cramm, J.M. The relationship between person-centred care and well-being and satisfaction with care of patients living with obesity. Int. J. Qual. Health Care 2024, 36, mzae078. [Google Scholar] [CrossRef]
- Molina, K.; Baskin, M.L.; Long, D.; Carson, T.L. Psychological and behavioral pathways between perceived stress and weight change in a behavioral weight loss intervention. J. Behav. Med. 2021, 44, 822–832. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Cattivelli, R.; Giusti, E.M.; Riboni, F.V.; Varallo, G.; Pietrabissa, G.; Manzoni, G.M.; Consoli, S.; Bastoni, I.; Granese, V.; et al. The ACTyourCHANGE study protocol: Promoting a healthy lifestyle in patients with obesity with Acceptance and Commitment Therapy-a randomized controlled trial. Trials 2021, 22, 290. [Google Scholar] [CrossRef]
- Rand, K.; Vallis, M.; Aston, M.; Price, S.; Piccinini-Vallis, H.; Rehman, L.; Kirk, S.F. “It is not the diet; it is the mental part we need help with.” A multilevel analysis of psychological, emotional, and social well-being in obesity. Int. J. Qual. Stud. Health Well-Being 2017, 12, 1306421. [Google Scholar] [CrossRef]
- Alberga, A.S.; Edache, I.Y.; Forhan, M.; Russell-Mayhew, S. Weight bias and health care utilization: A scoping review. Prim. Health Care Res. Dev. 2019, 20, e116. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Castelnuovo, G.; Manzoni, G.M.; Cattivelli, R.; Molinari, E.; Gondoni, L.A. Psychological Well-Being as an Independent Predictor of Exercise Capacity in Cardiac Rehabilitation Patients With Obesity. Front. Psychol. 2019, 10, 2973. [Google Scholar] [CrossRef]
- Diener, E. Subjective well-being: The science of happiness and a proposal for a national index. Am. Psychol. 2000, 55, 34. [Google Scholar] [CrossRef]
- Boulon, L.; Prieur, F.; Gaget, O.; Martin, D.; Amichaud, R.; Al Naasan, I.; Hicter, M.-G.; Bossu Estour, C. Progression of quality of life in patients with grade 3 obesity after a 36 months care pathway with and without bariatric surgery. Nutr. Clin. Métab. 2022, 36, 203–209. [Google Scholar] [CrossRef]
- Phyo, A.Z.Z.; Freak-Poli, R.; Craig, H.; Gasevic, D.; Stocks, N.P.; Gonzalez-Chica, D.A.; Ryan, J. Quality of life and mortality in the general population: A systematic review and meta-analysis. BMC Public Health 2020, 20, 1596. [Google Scholar] [CrossRef] [PubMed]
- Rasyid, H.; Kasim, H.; Zatalia, S.R.; Sampebuntu, J. Quality of life in patients with renal failure undergoing hemodialysis. Acta Medica Indones. 2022, 54, 307–313. [Google Scholar]
- Greenspoon, P.J.; Saklofske, D.H. Toward an Integration of Subjective Well-Being and Psychopathology. Soc. Indic. Res. 2001, 54, 81–108. [Google Scholar] [CrossRef]
- Suldo, S.M.; Shaffer, E.J. Looking beyond psychopathology: The dual-factor model of mental health in youth. Sch. Psychol. Rev. 2008, 37, 52–68. [Google Scholar] [CrossRef]
- Calugi, S.; Dalle Grave, R. Psychological features in obesity: A network analysis. Int. J. Eat. Disord. 2020, 53, 248–255. [Google Scholar] [CrossRef]
- Borsboom, D.; Deserno, M.K.; Rhemtulla, M.; Epskamp, S.; Fried, E.I.; McNally, R.J.; Robinaugh, D.J.; Perugini, M.; Dalege, J.; Costantini, G.; et al. Network analysis of multivariate data in psychological science. Nat. Rev. Methods Prim. 2021, 1, 58. [Google Scholar] [CrossRef]
- Galderisi, S.; Rucci, P.; Kirkpatrick, B.; Mucci, A.; Gibertoni, D.; Rocca, P.; Rossi, A.; Bertolino, A.; Strauss, G.P.; Aguglia, E.; et al. Interplay Among Psychopathologic Variables, Personal Resources, Context-Related Factors, and Real-life Functioning in Individuals With Schizophrenia: A Network Analysis. JAMA Psychiatry 2018, 75, 396–404. [Google Scholar] [CrossRef]
- Hevey, D. Network analysis: A brief overview and tutorial. Health Psychol. Behav. Med. 2018, 6, 301–328. [Google Scholar] [CrossRef]
- Grossi, E.; Compare, A. Psychological General Well-Being Index (PGWB). In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 5152–5156. [Google Scholar]
- Dupuy, H.J. The psychological general well-being (PGWB) index. In Assessment of Quality of Life in clinical trials of cardiovascular therapies; Le Jacq Publishing: New York, NY, USA, 1984; pp. 170–183. [Google Scholar]
- Nilsson, G.; Ohrvik, J.; Lonnberg, I.; Hedberg, P. Low Psychological General Well-Being (PGWB) is associated with deteriorated 10-year survival in men but not in women among the elderly. Arch. Gerontol. Geriatr. 2011, 52, 167–171. [Google Scholar] [CrossRef]
- Talley, N.J.; Wiklund, I. Patient reported outcomes in gastroesophageal reflux disease: An overview of available measures. Qual. Life Res. 2005, 14, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Lundgren-Nilsson, Å.; Jonsdottir, I.H.; Ahlborg, G.; Tennant, A. Construct validity of the psychological general well being index (PGWBI) in a sample of patients undergoing treatment for stress-related exhaustion: A rasch analysis. Health Qual. Life Outcomes 2013, 11, 2. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows; Version 29.0.2.0; IBM Corp: Armonk, NY, USA, 2023. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 1988. [Google Scholar]
- JASP Team. JASP, Version 0.19.0; JASP: Amsterdam, The Netherlands, 2024.
- Lauritzen, S.L. Oxford Statistical Science Series. In Graphical Models; Oxford University Press: Oxford, UK; New York, NY, USA, 1996. [Google Scholar]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2007, 9, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Golino, H.F.; Epskamp, S. Exploratory graph analysis: A new approach for estimating the number of dimensions in psychological research. PLoS ONE 2017, 12, e0174035. [Google Scholar] [CrossRef]
- Costantini, G.; Epskamp, S.; Borsboom, D.; Perugini, M.; Mõttus, R.; Waldorp, L.J.; Cramer, A.O.J. State of the aRt personality research: A tutorial on network analysis of personality data in R. J. Res. Personal. 2015, 54, 13–29. [Google Scholar] [CrossRef]
- Epskamp, S.; Maris, G.; Waldorp, L.J.; Borsboom, D. Network Psychometrics. In The Wiley Handbook of Psychometric Testing: AnMultidisciplinary Reference on Survey, Scale and Test Development; University of Amsterdam: Amsterdam, The Netherlands, 2017; Volume 2, pp. 953–986. [Google Scholar]
- Chen, J.; Chen, Z. Extended Bayesian information criteria for model selection with large model spaces. Biometrika 2008, 95, 759–771. [Google Scholar] [CrossRef]
- van Borkulo, C.D.; Borsboom, D.; Epskamp, S.; Blanken, T.F.; Boschloo, L.; Schoevers, R.A.; Waldorp, L.J. A new method for constructing networks from binary data. Sci. Rep. 2014, 4, 5918. [Google Scholar] [CrossRef]
- Barber, R.F.; Drton, M. High-dimensional Ising model selection with Bayesian information criteria. Electron. J. Stat. 2015, 9, 567–607. [Google Scholar] [CrossRef]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Marchetti, I. Hopelessness: A network analysis. Cogn. Ther. Res. 2019, 43, 611–619. [Google Scholar] [CrossRef]
- Haslbeck, J.M.B.; Waldorp, L.J. How well do network models predict observations? On the importance of predictability in network models. Behav. Res. Methods 2018, 50, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, J.M.B.; Waldorp, L.J. mgm: Estimating Time-Varying Mixed Graphical Models in High-Dimensional Data. J. Stat. Softw. 2020, 93, 1–46. [Google Scholar] [CrossRef]
- Dalege, J.; Borsboom, D.; van Harreveld, F.; van der Maas, H.L.J. Network Analysis on Attitudes:A Brief Tutorial. Soc. Psychol. Personal. Sci. 2017, 8, 528–537. [Google Scholar] [CrossRef]
- McNally, R.J.; Mair, P.; Mugno, B.L.; Riemann, B.C. Co-morbid obsessive–compulsive disorder and depression: A Bayesian network approach. Psychol. Med. 2017, 47, 1204–1214. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Luo, X.; Ruan, Z.; Liu, L. The association between overweight and varying degrees of obesity with subjective well-being and depressive symptoms: A two sample Mendelian randomization study. J. Psychosom. Res. 2024, 187, 111940. [Google Scholar] [CrossRef]
- Putra, I.; Daly, M.; Sutin, A.; Steptoe, A.; Scholes, S.; Robinson, E. Obesity, psychological well-being related measures, and risk of seven non-communicable diseases: Evidence from longitudinal studies of UK and US older adults. Int. J. Obes. 2024, 48, 1283–1291. [Google Scholar] [CrossRef]
- Conradson, H.E.; Hayden, K.A.; Russell-Mayhew, S.; Raffin Bouchal, S.; King-Shier, K. Positive psychological well-being in women with obesity: A scoping review of qualitative and quantitative primary research. Obes. Sci. Pr. 2022, 8, 691–714. [Google Scholar] [CrossRef]
- Dockray, S.; Steptoe, A. Positive affect and psychobiological processes. Neurosci. Biobehav. Rev. 2010, 35, 69–75. [Google Scholar] [CrossRef]
- Guerrini Usubini, A.; Varallo, G.; Granese, V.; Cattivelli, R.; Consoli, S.; Bastoni, I.; Volpi, C.; Castelnuovo, G.; Molinari, E. The Impact of Psychological Flexibility on Psychological Well-Being in Adults With Obesity. Front. Psychol. 2021, 12, 636933. [Google Scholar] [CrossRef]
- Pietrabissa, G.; Volpi, C.; Bottacchi, M.; Bertuzzi, V.; Guerrini Usubini, A.; Löffler-Stastka, H.; Prevendar, T.; Rapelli, G.; Cattivelli, R.; Castelnuovo, G.; et al. The Impact of Social Isolation during the COVID-19 Pandemic on Physical and Mental Health: The Lived Experience of Adolescents with Obesity and Their Caregivers. Int. J. Env. Res. Public Health 2021, 18, 3026. [Google Scholar] [CrossRef] [PubMed]
- Helliwell, J.F. Determinants of well-being and their implications for health care. Ann. Nutr. Metab. 2019, 74, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Beekman, A.; Deeg, D.; Braam, A.; Smit, J.; Van Tilburg, W. Consequences of major and minor depression in later life: A study of disability, well-being and service utilization. Psychol. Med. 1997, 27, 1397–1409. [Google Scholar] [CrossRef]
- Chida, Y.; Steptoe, A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosom. Med. 2008, 70, 741–756. [Google Scholar] [CrossRef]
- Lundqvist, C.; Kenttä, G. Positive Emotions Are Not Simply the Absence of the Negative Ones: Development and Validation of the Emotional Recovery Questionnaire (EmRecQ). Sport Psychol. 2010, 24, 468–488. [Google Scholar] [CrossRef]
- Ruggeri, K.; Garcia-Garzon, E.; Maguire, Á.; Matz, S.; Huppert, F.A. Well-being is more than happiness and life satisfaction: A multidimensional analysis of 21 countries. Health Qual. Life Outcomes 2020, 18, 192. [Google Scholar] [CrossRef]
- Park, C.L.; Kubzansky, L.D.; Chafouleas, S.M.; Davidson, R.J.; Keltner, D.; Parsafar, P.; Conwell, Y.; Martin, M.Y.; Hanmer, J.; Wang, K.H. Emotional Well-Being: What It Is and Why It Matters. Affect. Sci. 2023, 4, 10–20. [Google Scholar] [CrossRef]
- Diener, E.; Pressman, S.D.; Hunter, J.; Delgadillo-Chase, D. If, Why, and When Subjective Well-Being Influences Health, and Future Needed Research. Appl. Psychol. Health Well-Being 2017, 9, 133–167. [Google Scholar] [CrossRef]
- Lapin, B.; Mate, K.; Li, Y.; Thakore, N. Subjective health perception prioritizes psychological well-being over physical function in advanced ALS: A multigroup structural equation modeling analysis. J. Neurol. Sci. 2022, 442, 120442. [Google Scholar] [CrossRef]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Gao, Y.; Shabbir, A.; Lim, S.L.; Geetha, K.; Kim, G.; Chong, C.S.; Lomanto, D.; So, B.Y.J. Personal motivation, self-regulation barriers and strategies for weight loss in people with overweight and obesity: A thematic framework analysis. Public Health Nutr. 2022, 25, 2426–2435. [Google Scholar] [CrossRef] [PubMed]
- Lumeng, J.C.; Miller, A.L.; Horodynski, M.A.; Brophy-Herb, H.E.; Contreras, D.; Lee, H.; Sturza, J.; Kaciroti, N.; Peterson, K.E. Improving self-regulation for obesity prevention in head start: A randomized controlled trial. Pediatrics 2017, 139, e20162047. [Google Scholar] [CrossRef]
- Tomiyama, A.J.; Carr, D.; Granberg, E.M.; Major, B.; Robinson, E.; Sutin, A.R.; Brewis, A. How and why weight stigma drives the obesity ’epidemic’ and harms health. BMC Med. 2018, 16, 123. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, D.; Gillebaart, M. Lessons learned from trait self-control in well-being: Making the case for routines and initiation as important components of trait self-control. Health Psychol. Rev. 2017, 11, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Gariepy, G.; Nitka, D.; Schmitz, N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 407–419. [Google Scholar] [CrossRef]
- Dakanalis, A.; Mentzelou, M.; Papadopoulou, S.K.; Papandreou, D.; Spanoudaki, M.; Vasios, G.K.; Pavlidou, E.; Mantzorou, M.; Giaginis, C. The association of emotional eating with overweight/obesity, depression, anxiety/stress, and dietary patterns: A review of the current clinical evidence. Nutrients 2023, 15, 1173. [Google Scholar] [CrossRef]
- Bonanno, G.A.; Burton, C.L. Regulatory flexibility: An individual differences perspective on coping and emotion regulation. Perspect. Psychol. Sci. 2013, 8, 591–612. [Google Scholar] [CrossRef]
- Rademacher, L.; Kraft, D.; Eckart, C.; Fiebach, C.J. Individual differences in resilience to stress are associated with affective flexibility. Psychol. Res. 2023, 87, 1862–1879. [Google Scholar] [CrossRef]
- Seligman, M.E.P.; Steen, T.A.; Park, N.; Peterson, C. Positive Psychology Progress: Empirical Validation of Interventions. Am. Psychol. 2005, 60, 410–421. [Google Scholar] [CrossRef]
- Peters, M.L.; Smeets, E.; Feijge, M.; Van Breukelen, G.; Andersson, G.; Buhrman, M.; Linton, S.J. Happy despite pain: A randomized controlled trial of an 8-week internet-delivered positive psychology intervention for enhancing well-being in patients with chronic pain. Clin. J. Pain 2017, 33, 962–975. [Google Scholar] [CrossRef]
- Schotanus-Dijkstra, M.; Pieterse, M.E.; Drossaert, C.H.; Walburg, J.A.; Bohlmeijer, E.T. Possible mechanisms in a multicomponent email guided positive psychology intervention to improve mental well-being, anxiety and depression: A multiple mediation model. J. Posit. Psychol. 2019, 14, 141–155. [Google Scholar] [CrossRef]
- Reed, J.; Buck, S. The effect of regular aerobic exercise on positive-activated affect: A meta-analysis. Psychol. Sport Exerc. 2009, 10, 581–594. [Google Scholar] [CrossRef]
- Miller, K.J.; Mesagno, C.; McLaren, S.; Grace, F.; Yates, M.; Gomez, R. Exercise, mood, self-efficacy, and social support as predictors of depressive symptoms in older adults: Direct and interaction effects. Front. Psychol. 2019, 10, 2145. [Google Scholar] [CrossRef] [PubMed]
- Paluska, S.A.; Schwenk, T.L. Physical activity and mental health: Current concepts. Sports Med. 2000, 29, 167–180. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Ryan, R.M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Personal. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef]
- Ruffault, A.; Czernichow, S.; Hagger, M.S.; Ferrand, M.; Erichot, N.; Carette, C.; Boujut, E.; Flahault, C. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obes. Res. Clin. Pract. 2017, 11, 90–111. [Google Scholar] [CrossRef]
- Cotter, E.W.; Kelly, N.R. Stress-related eating, mindfulness, and obesity. Health Psychol. 2018, 37, 516. [Google Scholar] [CrossRef]
- Rapelli, G.; Pietrabissa, G.; Angeli, L.; Manzoni, G.M.; Tovaglieri, I.; Perger, E.; Garbarino, S.; Fanari, P.; Lombardi, C.; Castelnuovo, G. Study protocol of a randomized controlled trial of motivational interviewing-based intervention to improve adherence to continuous positive airway pressure in patients with obstructive sleep apnea syndrome: The MotivAir study. Front. Psychol. 2022, 13, 947296. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Annesi, J. Effects of exercise self-regulation on subsequent eating self-regulation: Implications for depletion vs. improvement based on behavioral treatment foci. Eur. Rev. Appl. Psychol. 2019, 69, 100472. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).