Abstract
Background/Objectives: The clinical impact of neutrophil-to-lymphocyte ratio (NLR) and right ventricular (RV) dysfunction on clinical outcomes in COVID-19 remains understudied in the Indonesian population. This study aims to investigate their prognostic value in hospitalized Indonesian adults with COVID-19. Methods: A retrospective cohort study was conducted at a COVID-19 referral hospital in Indonesia. We included all consecutive adults hospitalized between April 2020 and April 2021 who underwent transthoracic echocardiography (TTE) during admission. Clinical information was extracted from electronic medical records. TTE variables were defined according to the American Society of Echocardiography criteria. Statistical analyses were performed using SPSS. Ethical approval was obtained from the Institutional Review Board of Universitas Indonesia (#2022-01-135). Results: A total of 488 patients were included in this study—29 with and 459 without RV dysfunction. The mean age of the population was 54.8, with 42% being female. An NLR >4.793 was considered elevated. Elevated NLR was independently associated with RV dysfunction (OR: 3.38, p = 0.02). Older age (HR: 1.02, p = 0.01), obesity (HR: 1.85, p < 0.01), chronic kidney disease (HR: 1.69, p = 0.01), high NLR (HR: 2.75, p < 0.001), and RV dysfunction (HR: 2.07, p = 0.02) independently increased the risk of 30-day mortality by multivariate Cox regression analysis. Conclusions: In adult Indonesian patients hospitalized with COVID-19, an elevated NLR was associated with RV dysfunction, and both of these parameters increased the risk of 30-day mortality. This retrospective cohort study highlights the prognostic importance of NLR and RV dysfunction in hospitalized COVID-19 patients, providing physicians with tools to identify high-risk patients.
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first identified in December 2019. Its clinical presentation ranges from asymptomatic infection to critical illness characterized by acute respiratory distress syndrome (ARDS), septic shock, and multi-organ failure. Several prognostic markers have been identified, including the neutrophil-to-lymphocyte ratio (NLR), an inflammatory marker associated with disease severity and mortality [1]. Additionally, cardiovascular comorbidities have been shown to predict worse clinical outcomes in COVID-19 patients [2]. Therefore, beyond NLR, assessing both pre-existing and de novo cardiovascular abnormalities may provide valuable prognostic information.
The American Society of Echocardiography (ASE) has highlighted the importance of echocardiographic evaluation in COVID-19 patients [3]. Studies have demonstrated that RV dilation and dysfunction are common in severe COVID-19, and are associated with increased mortality [4,5,6]. Transthoracic echocardiography (TTE) is a non-invasive and accessible tool for assessing cardiac structure and function, including RV performance. In a global study of 1216 COVID-19 patients, TTE findings influenced clinical management decisions in 33% of the patients, demonstrating the value of this modality [7].
Given the rising burden of cardiovascular disease in Indonesia [8], assessment of NLR and RV dysfunction via TTE could provide valuable prognostic information. However, the prognostic value of these markers remains unexplored in the Indonesian population. Such prognostic information is tremendously valuable as it would allow for risk stratification and efficient resource allocation, especially in low-resource settings. This retrospective study aims to evaluate the prognostic value of NLR and RV dysfunction in hospitalized Indonesian adults with confirmed COVID-19. Additionally, we seek to determine whether an association exists between these markers, which could provide mechanistic insights.
2. Materials and Methods
2.1. Study Population and Design
This single-center retrospective cohort study was conducted at Universitas Indonesia Hospital, a designated COVID-19 referral hospital in Indonesia. All consecutive hospitalized adult patients with confirmed COVID-19 who underwent TTE assessment between 3 April 2020 and 6 April 2021 were included in this study. A confirmed case of COVID-19 was defined by a positive real-time reverse-transcriptase polymerase chain reaction (RT-PCR) test for SARS-CoV-2. Patients under the age of 18 or with negative real-time RT-PCR results were excluded. This retrospective study was performed in line with the principles of the Declaration of Helsinki, and ethical approval was granted by the Institutional Review Board (IRB) of Universitas Indonesia Hospital (Ref: 2022-01-135).
2.2. Transthoracic Echocardiography
Patients with appropriate indications for TTE, such as a clinical suspicion of congestive heart failure, a history of coronary artery disease, and new onset dyspnea, underwent focused TTE assessments during hospitalization. The decision as to whether a TTE study was needed was made by a clinical cardiologist as a part of the multidisciplinary team. All TTE assessments were conducted by cardiologists experienced in this technique. In accordance with recommendations from the ASE [9], the TTE assessments were focused as necessary to aid management decisions, and other appropriate infection control and protective precautions were taken. All TTE findings were recorded on a standardized echocardiography reporting form. The following TTE parameters were extracted for this study: left atrial (LA) dilation, left ventricle (LV) hypertrophy, LV ejection fraction, LV systolic function, right ventricle (RV) function, wall motion abnormalities (WMAs), and LV diastolic function. LA dilation was defined as an anteroposterior LA diameter > 40 mm measured in the parasternal long-axis view, as an LA volume index > 34 mL/m2, or by visual estimation. LV measurements were made in the parasternal long-axis view; LV hypertrophy (LVH) was defined as an LV mass > 95 g/m2 for women and >115 g/m2 for men. LV ejection fraction (LVEF) was measured by Simpson’s biplane method, measured by the TEICHOLZ quantification method on M-Mode, or estimated visually when image quality did not allow for accurate quantification. LV systolic dysfunction was defined as an LVEF < 50%. RV dysfunction was defined by an abnormal tricuspid annular plane systolic excursion (TAPSE) (<17 mm) or RV dilation (RV basal diameter > 41 mm or visual estimation). LV diastolic dysfunction was defined according to the structural and functional criteria set by the ASE [10]. Any WMAs were also recorded.
2.3. Data Collection
All data were extracted from the hospital’s secure electronic medical records (EMR) system. The extracted data included demographic information, peak severity of COVID-19 during hospitalization, final outcome of disease (survival or death), and presence of comorbidities, including obesity, hypertension, diabetes, dyslipidemia, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), congestive heart failure (CHF), coronary artery disease (CAD), and malignancy. The severity of COVID-19 was graded as mild, moderate, severe, or critical, as defined by the National Institutes of Health. TTE parameters were extracted from the patients’ standardized echocardiography report forms, also available on the EMR system.
2.4. Clinical Outcomes and Statistical Analysis
To determine the cut-off value for elevated NLR, a Receiver Operating Characteristics (ROC) curve was made for prediction of severe–critical COVID-19 disease. Youden’s J statistic was used to determine the optimal cut-off value. The normality of continuous variables was assessed using the Shapiro–Wilk test. Continuous variables were compared using Student’s t-test when normally distributed, or the Mann–Whitney U-test when non-normally distributed. Categorical variables were compared using the chi-square test or Fisher’s exact test. Multivariate logistic regression analysis was conducted to determine the factors associated with RV dysfunction in the cohort. Data for 30-day survival were extracted from the EMR. Survival analysis was conducted by formulating the Kaplan–Meier curve and by univariate and multivariate Cox regression analyses. A p-value of <0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS Statistics 26 (IBM Corporations, Armonk, NY, USA).
3. Results
A total of 488 patients met the inclusion criteria, of which 459 patients had no RV dysfunction and 29 patients had RV dysfunction. More than half of the entire cohort developed severe–critical COVID-19, and approximately a quarter did not survive beyond 30 days of admission. The full characteristics of the patients included in the study are presented in Table 1.

Table 1.
Population characteristics.
3.1. Defining an Elevated NLR
Youden’s J index was calculated for each co-ordinate of the Receiver Operating Characteristics (ROC) curve (Figure 1). The co-ordinate with the highest J index was used to determine the optimal cut-off for the NLR, which was 4.793. This cut-off had a sensitivity of 70.6% and a specificity of 80.6% in predicting severe–critical COVID-19.
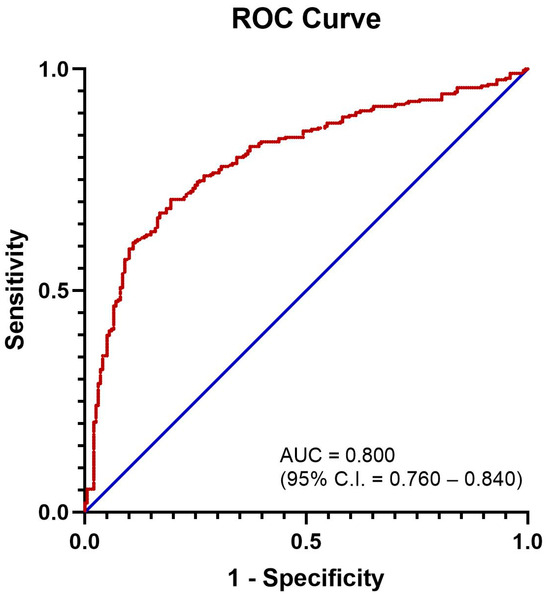
Figure 1.
ROC curve for NLR in predicting severe–critical COVID-19. Area under curve = 0.800 (95% C.I. = 0.760–0.840).
3.2. Factors Associated with RV Dysfunction
A logistic regression was performed to ascertain the effects of covariates on the likelihood that subjects have RV dysfunction (Table 2). The logistic regression model was statistically significant, χ2 = 64.48, p < 0.001. A high NLR (OR: 3.38, p = 0.02) and LV systolic dysfunction (OR: 9.76, p < 0.01) were independently associated with RV dysfunction.

Table 2.
Logistic regression analysis for RV dysfunction.
3.3. Analysis of 30-Day Survival
The 30-day survival curves by presence of RV dysfunction and elevated NLR were plotted (Figure 2). Patients with RV dysfunction and an elevated NLR experienced lower rates of 30-day survival.
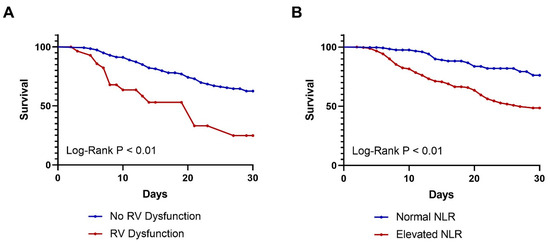
Figure 2.
Kaplan–Meier 30-day survival curves by (A) presence of RV dysfunction (p < 0.01) and (B) presence of elevated NLR (p < 0.01).
Next, a univariate Cox regression analysis was performed (Table 3). Older age (HR: 1.03, p < 0.001), obesity (HR: 1.71, p = 0.004), diabetes (HR: 1.85, p = 0.001), CKD (HR: 2.39, p < 0.001), CAD (HR: 1.57, p = 0.014), high NLR (HR: 3.38, p < 0.001), RV dysfunction (HR: 3.13, p < 0.001), and LV systolic dysfunction (HR: 1.08, p = 0.002) increased the risk of 30-day mortality.

Table 3.
Univariate Cox regression analysis (30-day survival).
Next, a multivariate Cox regression analysis was performed, incorporating the significant variables from the univariate analysis (Table 4). Older age (HR: 1.02, p = 0.01), obesity (HR: 1.85, p < 0.01), CKD (HR: 1.69, p = 0.01), high NLR (HR: 2.75, p < 0.001), and RV dysfunction (HR: 2.07, p = 0.017) independently increased the risk of 30-day mortality.

Table 4.
Multivariate Cox regression analysis (30-day survival).
4. Discussion
Our study confirmed that both an elevated NLR and RV dysfunction are independently associated with mortality in COVID-19. We also showed that an elevated NLR is independently associated with RV dysfunction, highlighting the interplay between inflammation and cardiovascular dysfunction in this condition.
We observed that an elevated NLR nearly triples the risk of 30-day mortality (HR 2.75), which is consistent with the meta-analysis by Simadibrata et al. [1] and other studies from various geographical regions [11,12,13,14]. Previous Indonesian studies have also demonstrated that an elevated NLR is associated with disease severity in this population [15,16]. Severe COVID-19 is characterized by an exaggerated immune response and hyperinflammation, which drive disease progression [17]. This immune response leads to increased neutrophil production and recruitment, causing tissue damage via oxidative stress, elevated neutrophil elastase activity, and neutrophil extracellular trap (NET) formation [18]. Our study, along with others in the literature, reinforces that inflammation, as reflected by an elevated NLR, correlates with worse clinical outcomes in COVID-19.
Next, we found that RV dysfunction doubles the risk of mortality in COVID-19 patients (HR 2.07), which is consistent with prior studies [4,5,6,19]. Several mechanisms explain this association. First, severe COVID-19 often leads to acute respiratory distress syndrome (ARDS), increasing pulmonary vascular resistance (PVR) directly and through ventilatory strategies like positive-pressure ventilation [20]. Additionally, a well-known feature of COVID-19 is increased risk of venous thromboembolism (VTE), including pulmonary emboli, which contribute to PVR elevation and RV strain [6]. Elevated PVR and RV afterload results in distension of the highly compliant ‘afterload-sensitive’ RV, resulting in increased oxygen demand and reduced oxygen supply [20]. Additionally, direct myocardial damage from COVID-19 may contribute to RV dysfunction [6]. In critically ill patients, RV dysfunction is often the primary cause of cardiovascular insufficiency, resulting in worse outcomes. Furthermore, RV dilation may result in shifting of the septum to the left, impairing left ventricular (LV) filling and cardiac output [20].
Another important finding from our study is the independent association between elevated NLR and RV dysfunction. Patients with an elevated NLR had more than three times the odds (OR 3.38) of having RV dysfunction than those with a normal NLR. Inflammation can drive RV dysfunction in COVID-19 through various mechanisms. Systemic inflammation in COVID-19 triggers the release of pro-inflammatory cytokines (IL-6, TNF-α, IL-1β), impairing cardiac function directly and by promoting inflammatory cell infiltration [21]. Inflammation also causes endothelial dysfunction, leading to vasoconstriction, hypercoagulation (with increased risk of VTEs), and microvascular thrombi, all of which contribute to elevated PVR and RV strain. Furthermore, systemic inflammation exacerbates ARDS and pulmonary injury, compounding RV dysfunction.
Our study has various limitations that must be addressed. Firstly, the TTEs performed were focused, rather than comprehensive, to minimize the risk of infection. Secondly, the retrospective design introduces a higher risk of bias and reduced control over data availability. Thirdly, the timing of TTEs varied among patients, introducing variability in disease progression at the time of assessment. Abnormalities on TTE could develop at different stages of COVID-19 disease progression, and hence, the variability in TTE timing could confound the observed association between abnormal TTE findings and clinical outcomes. Fourthly, we did not differentiate patients by SARS-CoV-2 variants, and so the effect of different variants on TTE findings and clinical outcomes is unknown. Finally, since TTE was only performed once, we could not determine whether RV dysfunction was pre-existing or developed during hospitalization. Future studies should explore whether pre-existing RV dysfunction leads to inflammation, whether inflammation drives RV dysfunction, or whether the relationship is bidirectional. Nevertheless, our study aimed to evaluate the prognostic value of NLR and TTE findings during hospitalization, regardless of when abnormalities developed.
Despite these limitations, this was a real-world study on a large population, and hence provides important insights. If feasible and safe, TTE must be conducted in hospitalized COVID-19 patients with appropriate indications, as this non-invasive modality can provide valuable prognostic information. Together with abnormal inflammatory indices such as an elevated NLR, the presence of TTE abnormalities, especially RV dysfunction, can alert physicians to possible deterioration in patients. Future prospective studies should standardize the timing of measurements (e.g., within 72 h of admission) to improve consistency. Additionally, a risk scoring system could be developed, incorporating the five independent predictors of 30-day mortality from our study: older age, obesity, chronic kidney disease (CKD), high NLR, and RV dysfunction. This would better reflect real-world clinical scenarios where multiple risk factors interact.
5. Conclusions
In adult Indonesian patients hospitalized with COVID-19, an elevated NLR (>4.793) at admission and RV dysfunction independently increased the risk of 30-day mortality. There was an independent association between an elevated NLR and RV dysfunction in this population. These parameters can aid physicians in identifying high-risk patients early on in the course of their disease, and allocating resources accordingly.
Author Contributions
Conceptualization, R.A. and H.S.M.; methodology, R.A., R.A.N. and H.S.M.; software, G.P., S.H., S.H.W., P.A. and D.Z.; validation, R.A. and H.S.M.; formal analysis, R.A.; investigation, G.P., S.H., S.H.W., P.A., D.Z. and H.S.M.; resources, G.P., S.H., S.H.W., P.A., D.Z. and H.S.M.; data curation, R.A.; writing—original draft preparation, R.A., S.I.K. and O.E.Y.; writing—review and editing, R.A., S.I.K., O.E.Y. and H.S.M.; visualization, R.A.; supervision, H.S.M.; project administration, R.A.N. and H.S.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This retrospective study was performed in line with the principles of the Declaration of Helsinki, and ethical approval was granted by the Institutional Review Board (IRB) of Universitas Indonesia Hospital on 27 January 2022 (Ref: 2022-01-135).
Informed Consent Statement
Not applicable, due to the retrospective nature of the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Conflicts of Interest
None declared for all authors.
References
- Simadibrata, D.M.; Calvin, J.; Wijaya, A.D.; Ibrahim, N.A.A. Neutrophil-to-lymphocyte ratio on admission to predict the severity and mortality of COVID-19 patients: A meta-analysis. Am. J. Emerg. Med. 2021, 42, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Ssentongo, P.; Ssentongo, A.E.; Heilbrunn, E.S.; Ba, D.M.; Chinchilli, V.M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0238215. [Google Scholar] [CrossRef]
- Kirkpatrick, J.N.; Swaminathan, M.; Adedipe, A.; Garcia-Sayan, E.; Hung, J.; Kelly, N.; Kort, S.; Nagueh, S.; Poh, K.K.; Sarwal, A.; et al. American Society of Echocardiography COVID-19 Statement Update: Lessons Learned and Preparation for Future Pandemics. J. Am. Soc. Echocardiogr. 2023, 36, 1127–1139. [Google Scholar] [CrossRef]
- Kim, J.; Volodarskiy, A.; Sultana, R.; Pollie, M.P.; Yum, B.; Nambiar, L.; Tafreshi, R.; Mitlak, H.W.; RoyChoudhury, A.; Horn, E.M.; et al. Prognostic Utility of Right Ventricular Remodeling Over Conventional Risk Stratification in Patients With COVID-19. J. Am. Coll. Cardiol. 2020, 76, 1965–1977. [Google Scholar] [CrossRef]
- Oweis, J.; Leamon, A.; Al-Tarbsheh, A.H.; Goodspeed, K.; Khorolsky, C.; Feustel, P.; Naseer, U.; Albaba, I.; Parimi, S.A.; Shkolnik, B.; et al. Influence of right ventricular structure and function on hospital outcomes in COVID-19 patients. Heart Lung 2023, 57, 19–24. [Google Scholar] [CrossRef]
- Corica, B.; Marra, A.M.; Basili, S.; Cangemi, R.; Cittadini, A.; Proietti, M.; Romiti, G.F. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 17774. [Google Scholar] [CrossRef]
- Dweck, M.R.; Bularga, A.; Hahn, R.T.; Bing, R.; Lee, K.K.; Chapman, A.R.; White, A.; Salvo, G.D.; Sade, L.E.; Pearce, K.; et al. Global evaluation of echocardiography in patients with COVID-19. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 949–958. [Google Scholar] [CrossRef] [PubMed]
- Mboi, N.; Syailendrawati, R.; Ostroff, S.M.; Elyazar, I.R.; Glenn, S.D.; Rachmawati, T.; Nugraheni, W.P.; Ali, P.B.; Trisnantoro, L.; Adnani, Q.E.S.; et al. The state of health in Indonesia’s provinces, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Glob. Health 2022, 10, e1632–e1645. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, J.N.; Mitchell, C.; Taub, C.; Kort, S.; Hung, J.; Swaminathan, M. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak: Endorsed by the American College of Cardiology. J. Am. Soc. Echocardiogr. 2020, 33, 648–653. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 277–314. [Google Scholar] [CrossRef]
- Citu, C.; Gorun, F.; Motoc, A.; Sas, I.; Gorun, O.M.; Burlea, B.; Tuta-Sas, I.; Tomescu, L.; Neamtu, R.; Malita, D.; et al. The Predictive Role of NLR, d-NLR, MLR, and SIRI in COVID-19 Mortality. Diagnostics 2022, 12, 122. [Google Scholar] [CrossRef] [PubMed]
- Cakirca, G.; Cakirca, T.D.; Bindal, A.; Olcen, M. Inflammation-based Indices Predicting Mortality in COVID-19. J. Coll. Physicians Surg. Pak. 2023, 33, 112–114. [Google Scholar] [PubMed]
- Seyfi, S.; Azadmehr, A.; Ezoji, K.; Nabipour, M.; Babazadeh, A.; Saleki, K.; Mahmoodi, M.; Pouladi, A.H. Mortality in ICU COVID-19 Patients Is Associated with Neutrophil-to-Lymphocyte Ratio (NLR): Utility of NLR as a Promising Immunohematological Marker. Interdiscip. Perspect. Infect. Dis. 2023, 2023, 9048749. [Google Scholar] [CrossRef] [PubMed]
- Regolo, M.; Vaccaro, M.; Sorce, A.; Stancanelli, B.; Colaci, M.; Natoli, G.; Russo, M.; Alessandria, I.; Motta, M.; Santangelo, N.; et al. Neutrophil-to-Lymphocyte Ratio (NLR) Is a Promising Predictor of Mortality and Admission to Intensive Care Unit of COVID-19 Patients. J. Clin. Med. 2022, 11, 2235. [Google Scholar] [CrossRef]
- Andiani, F.; Herawati, R.; Triyani, Y. Correlation between NLR and PLR with the Severity of COVID-19 Inpatients. Indones. J. Clin. Pathol. Med. Lab. 2023, 29, 47–53. [Google Scholar] [CrossRef]
- Arini, I.A.; Masyeni, S.; Widhidewi, N.W. Relationship between neutrophil-lymphocyte ratio and platelet-lymphocyte ratio with the severity of COVID-19. Narra J. 2024, 4, e262. [Google Scholar] [CrossRef]
- Tay, M.Z.; Poh, C.M.; Rénia, L.; MacAry, P.A.; Ng, L.F.P. The trinity of COVID-19: Immunity, inflammation and intervention. Nat. Rev. Immunol. 2020, 20, 363–374. [Google Scholar] [CrossRef]
- Cavalcante-Silva, L.H.A.; Carvalho, D.C.M.; Lima, É.d.A.; Galvão, J.G.F.M.; da Silva, J.S.d.F.; Sales-Neto, J.M.d.; Rodrigues-Mascarenhas, S. Neutrophils and COVID-19: The road so far. Int. Immunopharmacol. 2021, 90, 107233. [Google Scholar] [CrossRef]
- Soulat-Dufour, L.; Fauvel, C.; Weizman, O.; Barbe, T.; Pezel, T.; Mika, D.; Cellier, J.; Geneste, L.; Panagides, V.; Marsou, W.; et al. Prognostic value of right ventricular dilatation in patients with COVID-19: A multicentre study. Eur. Heart J. Cardiovasc. Imaging 2022, 13, 569–577. [Google Scholar] [CrossRef]
- Zochios, V.; Parhar, K.; Tunnicliffe, W.; Roscoe, A.; Gao, F. The Right Ventricle in ARDS. Chest 2017, 152, 181–193. [Google Scholar] [CrossRef]
- Adeghate, E.A.; Eid, N.; Singh, J. Mechanisms of COVID-19-induced heart failure: A short review. Heart Fail Rev. 2021, 26, 363–369. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).