Adherence to the Mediterranean Diet in Paediatric Patients with Inflammatory Bowel Disease and Functional Abdominal Pain Disorders—Comparative Study
Abstract
1. Introduction
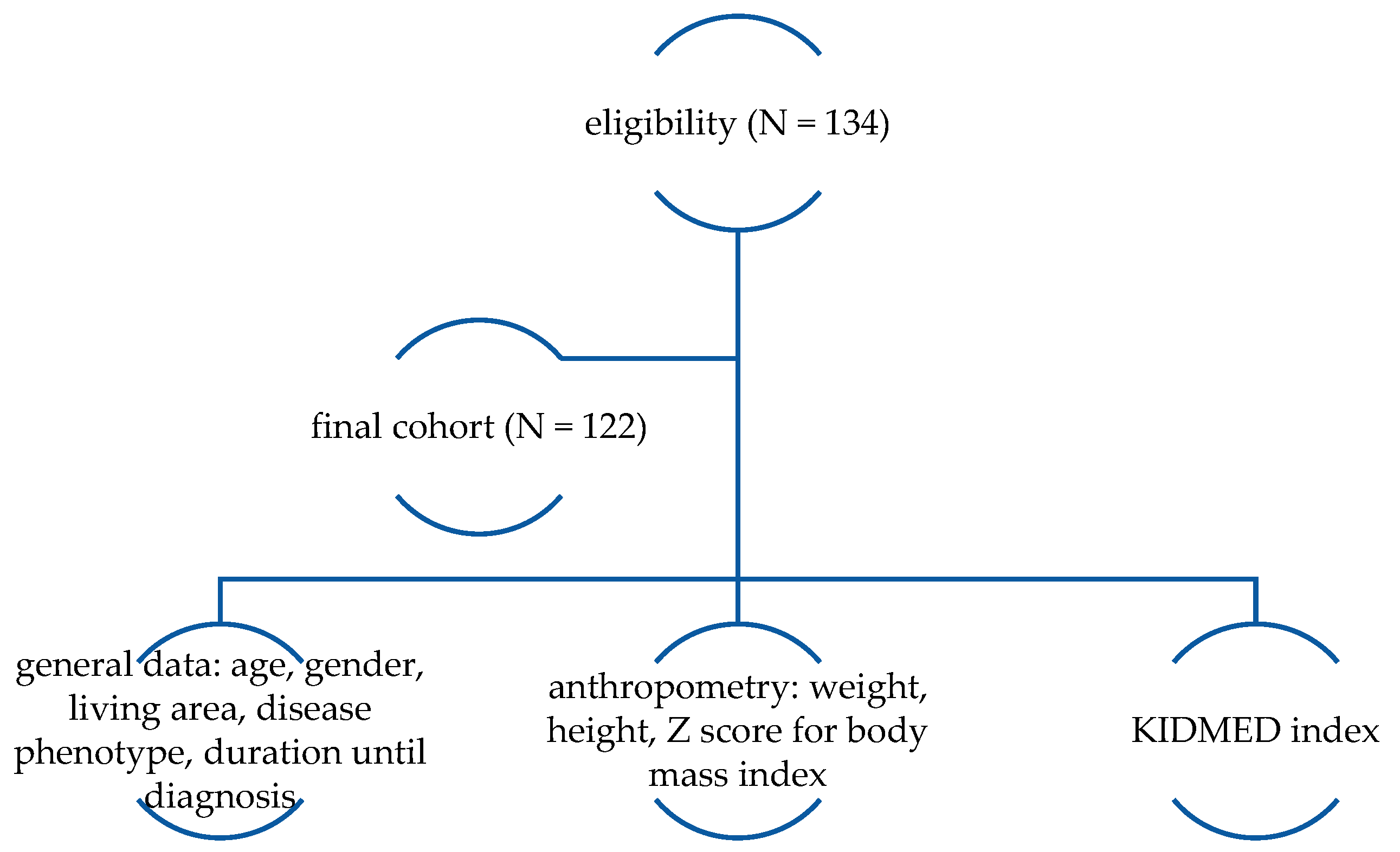
2. Materials and Methods
Study Population
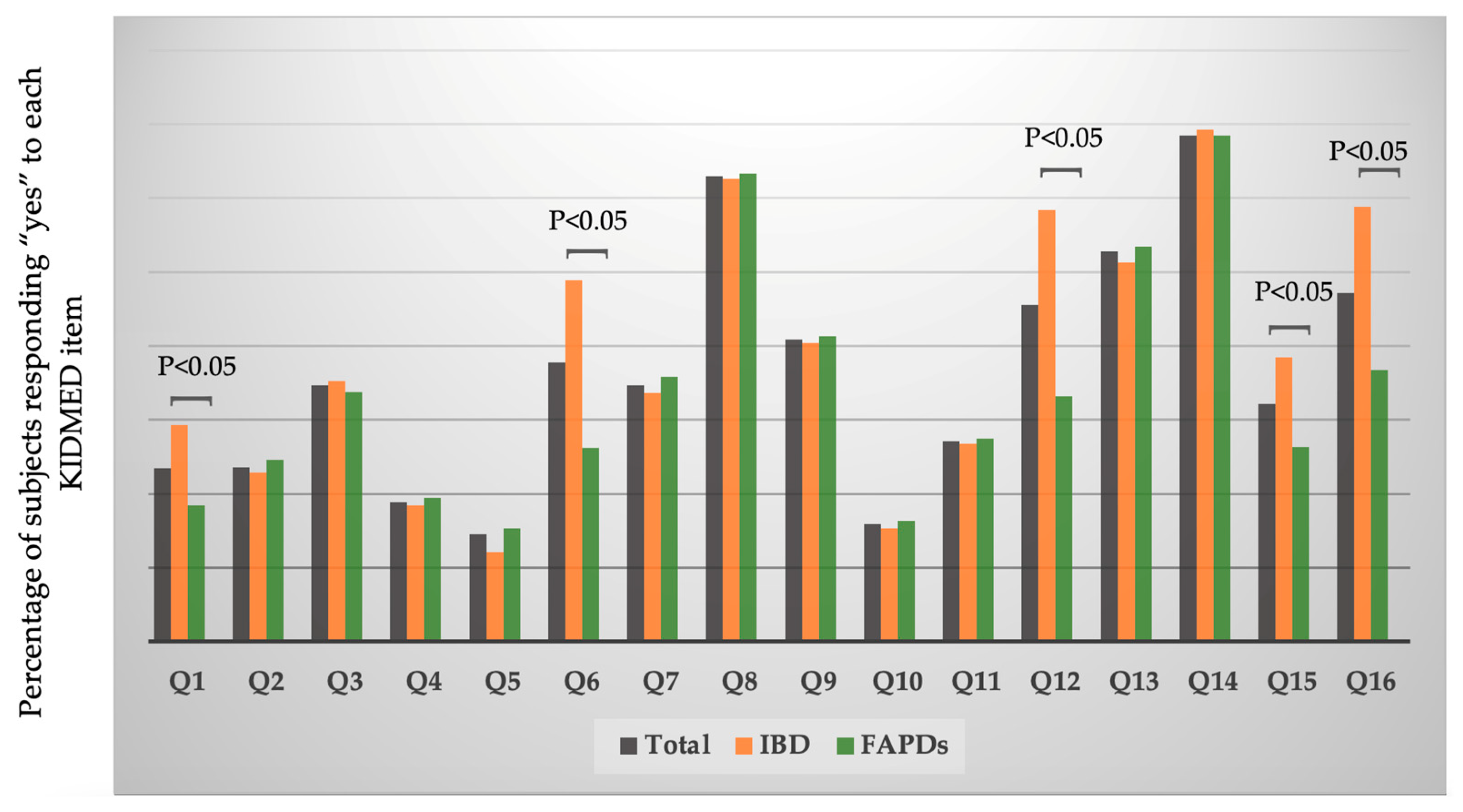
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| IBD | Inflammatory bowel disorder |
| FAPDs | Functional abdominal pain disorders |
| MD | Mediterranean diet |
| GI | Gastrointestinal |
References
- Schreiner, P.; Martinho-Grueber, M.; Studerus, D.; Vavricka, S.R.; Tilg, H.; Biedermann, L. On behalf of Swiss IBDnet, an official working group of the Swiss Society of Gastroenterology Nutrition in Inflammatory Bowel Disease. Digestion 2020, 101, 120–135. [Google Scholar] [CrossRef] [PubMed]
- Forbes, A.; Escher, J.; Hébuterne, X.; Kłęk, S.; Krznaric, Z.; Schneider, S.; Shamir, R.; Stardelova, K.; Wierdsma, N.; Wiskin, A.E.; et al. ESPEN guideline: Clinical nutrition in inflammatory bowel disease. Clin. Nutr. 2017, 36, 321–347. [Google Scholar] [CrossRef]
- Cucinotta, U.; Romano, C.; Dipasquale, V. Diet and Nutrition in Pediatric Inflammatory Bowel Diseases. Nutrients 2021, 13, 655. [Google Scholar] [CrossRef] [PubMed]
- Strisciuglio, C.; Cenni, S.; Serra, M.R.; Dolce, P.; Martinelli, M.; Staiano, A.; Miele, E. Effectiveness of Mediterranean Diet’s Adherence in children with Inflammatory Bowel Diseases. Nutrients 2020, 12, 3206. [Google Scholar] [CrossRef] [PubMed]
- Geerling, B.J.; Badart-Smook, A.; Stockbrügger, R.W.; Brummer, R.J. Comprehensive nutritional status in recently diagnosed patients with inflammatory bowel disease compared with population controls. Eur. J. Clin. Nutr. 2000, 54, 521. [Google Scholar] [CrossRef]
- Vrdoljak, J.; Vilović, M.; Živković, P.; Hadjina, I.T.; Rušić, D.; Bukić, J.; Borovac, J.; Božić, J. Mediterranean Diet Adherence and Dietary Attitudes in Patients with Inflammatory Bowel Disease. Nutrients 2020, 12, 3429. [Google Scholar] [CrossRef] [PubMed]
- Hyams, J.S.; Di Lorenzo, C.; Saps, M.; Shulman, R.J.; Staiano, A.; van Tilburg, M. Functional Disorders: Children and Adolescents. Gastroenterology 2016, S0016-5085, 00181-5. [Google Scholar]
- Black, C.J.; Drossman, D.A.; Talley, N.J.; Ruddy, J.; Ford, A.C. Functional gastrointestinal disorders: Advances in understanding and management. Lancet 2020, 396, 1664–1674. [Google Scholar] [CrossRef]
- de Bruijn, C.M.; Rexwinkel, R.; Gordon, M.; Sinopoulou, V.; Benninga, M.A.; Tabbers, M.M. Dietary interventions for functional abdominal pain disorders in children: A systematic review and meta-analysis. Expert Rev. Gastroenterol. Hepatol. 2022, 16, 359–371. [Google Scholar] [CrossRef]
- Defrees, D.N.; Bailey, J. Irritable Bowel Syndrome: Epidemiology, Pathophysiology, Diagnosis, and Treatment. Prim. Care Clin. Off. Pract. 2017, 44, 655–671. [Google Scholar] [CrossRef]
- Radovanovic-Dinic, B.; Tesic-Rajkovic, S.; Grgov, S.; Petrovic, G.; Zivković, V. Irritable bowel syndrome—From etiopathogenesis to therapy. Biomed. Pap. 2018, 162, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Alfaro Cruz, L.; Minard, C.; Guffey, D.; Chumpitazi, B.P.; Shulman, R.J. Does a Minority of Children with Functional Gastrointestinal Disorders Receive Formal Diet Advice? J. Parenter. Enter. Nutr. 2020, 44, 1525–1529. [Google Scholar] [CrossRef]
- Chumpitazi, B.P. Update on Dietary Management of Childhood Functional Abdominal Pain Disorders. Gastroenterol. Clin. N. Am. 2018, 47, 715–726. [Google Scholar]
- van Lanen, A.S.; de Bree, A.; Greyling, A. Efficacy of a low-FODMAP diet in adult irritable bowel syndrome: A systematic review and meta-analysis. Eur. J. Nutr. 2021, 60, 3505–3522. [Google Scholar] [CrossRef] [PubMed]
- Morariu, I.-D.; Avasilcai, L.; Vieriu, M.; Lupu, V.V.; Morariu, B.-A.; Lupu, A.; Morariu, P.-C.; Pop, O.-L.; Starcea, I.M.; Trandafir, L. Effects of a Low-FODMAP Diet on Irritable Bowel Syndrome in both Children and Adults—A Narrative Review. Nutrients 2023, 15, 2295. [Google Scholar] [CrossRef] [PubMed]
- Zito, F.P.; Polese, B.; Vozzella, L.; Gala, A.; Genovese, D.; Verlezza, V.; Medugno, F.; Santini, A.; Barrea, L.; Cargiolli, M.; et al. Good adherence to mediterranean diet can prevent gastrointestinal symptoms: A survey from Southern Italy. World J. Gastrointest. Pharmacol. Ther. 2016, 7, 564–571. [Google Scholar] [CrossRef]
- Al-Biltagi, M.; El Amrousy, D.; El Ashry, H.; Maher, S.; Mohammed, M.A.; Hasan, S. Effects of adherence to the Mediterranean diet in children and adolescents with irritable bowel syndrome. World J. Clin. Pediatr. 2022, 11, 330–340. [Google Scholar] [CrossRef]
- Grosso, G.; Buscemi, S.; Galvano, F.; Mistretta, A.; Marventano, S.; Vela, V.L.; Drago, F.; Gangi, S.; Basile, F.; Biondi, A. Mediterranean diet and cancer: Epidemiological evidence and mechanism of selected aspects. BMC Surg. 2013, 13, S14. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [CrossRef]
- Donini, L.M.; Serra-Majem, L.; Bulló, M.; Gil, Á.; Salas-Salvadó, J. The Mediterranean diet: Culture, health and science. Br. J. Nutr. 2015, 113 (Suppl. S2), S1–S3. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Dietary patterns, mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014, 25, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Ros, E.; Martínez-González, M.A.; Estruch, R.; Salas-Salvadó, J.; Fitó, M.; Martínez, J.A.; Corella, D. Mediterranean diet and cardiovascular health: Teachings of the predimed study. Adv. Nutr. 2014, 5, 330S–336S. [Google Scholar] [CrossRef] [PubMed]
- Bacopoulou, F.; Landis, G.; Rentoumis, A.; Tsitsika, A.; Efthymiou, V. Mediterranean diet decreases adolescent waist circumference. Eur. J. Clin. Investig. 2017, 47, 447–455. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the mediterranean diet in Spain. Development of kidmed, mediterranean diet quality index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar]
- Iaccarino Idelson, P.; Scalfi, L.; Valerio, G. Adherence to the Mediterranean Diet in children and adolesents: A systematic review. Nutr. Metab. Cardiovasc Dis. 2017, 27, 283–299. [Google Scholar] [CrossRef]
- Alibabaei, Z.; Jazayeri, S.; Vafa, M.; Feizy, Z.; Sajadi Hezaveh, Z. The association between dietary patterns and quality and duration of sleep in children and adolescents: A systematic review. Clin. Nutr. ESPEN 2021, 45, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Romero-Robles, M.A.; Ccami-Bernal, F.; Ortiz-Benique, Z.N.; Pinto-Ruiz, D.F.; Benites-Zapata, V.A.; Casas Patiño, D. Adherence to Mediterranean diet associated with health-related quality of life in children and adolescents: A systematic review. BMC Nutr. 2022, 8, 57. [Google Scholar] [CrossRef]
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; De Ridder, L.; Kolho, K.L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. ESPGHAN revised portocriteriafor the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806. [Google Scholar] [CrossRef]
- Altavilla, C.; Caballero-Pérez, P. An update of the KIDMED questionnaire, a Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2019, 22, 2543–2547. [Google Scholar] [CrossRef]
- El Amrousy, D.; Elashry, H.; Salamah, A.; Maher, S.; Abd-Elsalam, S.M.; Hasan, S. Adherence to the Mediterranean Diet Improved Clinical Scores and Inflammatory Markers in Children with Active Inflammatory Bowel Disease: A Randomized Trial. J. Inflamm. Res. 2022, 15, 2075–2086. [Google Scholar] [CrossRef]
- Kwon, Y.-J.; Park, Y.-H.; Lee, Y.-J.; Lim, L.-R.; Lee, J.-W. Development and Validation of a Questionnaire to Measure Adherence to a Mediterranean-Type Diet in Youth. Nutrients 2024, 16, 2754. [Google Scholar] [CrossRef]
- Mariscal-Arcas, M.; Rivas, A.; Velasco, J.; Ortega, M.; Caballero, A.M.; Olea-Serrano, F. Evaluation of the mediterranean diet quality index (kidmed) in children and adolescents in Southern Spain. Public Health Nutr. 2009, 12, 1408–1412. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Marventano, S.; Buscemi, S.; Scuderi, A.; Matalone, M.; Platania, A.; Giorgianni, G.; Rametta, S.; Nolfo, F.; Galvano, F.; et al. Factors associated with adherence to the mediterranean diet among adolescents living in sicily, Southern Italy. Nutrients 2013, 5, 4908–4923. [Google Scholar] [CrossRef]
- Deslippe, A.L.; Bergeron, C.; Cohen, T.R. Boys and girls differ in their rationale behind eating: A systematic review of intrinsic and extrinsic motivations in dietary habits across countries. Front Nutr. 2023, 10, 1256189. [Google Scholar] [CrossRef] [PubMed]
- Pop, T.L.; Maniu, D.; Rajka, D.; Lazea, C.; Cismaru, G.; Ştef, A.; Căinap, S.S. Prevalence of Underweight, Overweight and Obesity in School-Aged Children in the Urban Area of the Northwestern Part of Romania. Int. J. Environ. Res. Public Health 2021, 18, 5176. [Google Scholar] [CrossRef]
- Stan-Ilie, M.; Sandru, V.; Constantinescu, G.; Plotogea, O.-M.; Rinja, E.M.; Tincu, I.F.; Jichitu, A.; Carasel, A.E.; Butuc, A.C.; Popa, B. Artificial Intelligence—The Rising Star in the Field of Gastroenterology and Hepatology. Diagnostics 2023, 13, 662. [Google Scholar] [CrossRef]
- Zahid, M.; Sughra, U.; Mumtaz, S.; Hassan, M. Improving nutritional status of children using artificial intelligence-based mobile application postsurgery: Randomised controlled trial. BMJ Nutr. Prev. Health 2023, 6, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Bučan Nenadić, D.; Kolak, E.; Selak, M.; Smoljo, M.; Radić, J.; Vučković, M.; Dropuljić, B.; Pijerov, T.; Babić Cikoš, D. Anthropometric parameters and mediterranean diet adherence in preschool children in split-dalmatia county, croatia-are they related? Nutrients 2021, 13, 4252. [Google Scholar] [CrossRef]
- Sahingoz, S.A.; Sanlier, N. Compliance with mediterranean diet quality index (kidmed) and nutrition knowledge levels in adolescents. A case study from Turkey. Appetite 2011, 57, 272–277. [Google Scholar] [CrossRef]
- Godala, M.; Gaszyńska, E.; Walczak, K.; Małecka-Wojciesko, E. Habitual Dietary Intake and Adherence to Dietary Guidelines of Patients with Inflammatory Bowel Diseases. Gastroenterol. Insights 2024, 15, 69–86. [Google Scholar] [CrossRef]
- Fiorindi, C.; Russo, E.; Balocchini, L.; Amedei, A.; Giudici, F. Inflammatory Bowel Disease and Customized Nutritional Intervention Focusing on Gut Microbiome Balance. Nutrients 2022, 14, 4117. [Google Scholar] [CrossRef] [PubMed]
- Laing, B.B.; Lim, A.G.; Ferguson, L.R. A Personalised Dietary Approach—A Way Forward to Manage Nutrient Deficiency, Effects of the Western Diet, and Food Intolerances in Inflammatory Bowel Disease. Nutrients 2019, 11, 1532. [Google Scholar] [CrossRef] [PubMed]
- Lane, E.R.; Zisman, T.L.; Suskind, D.L. The microbiota in inflammatory bowel disease: Current and therapeutic insights. J. Inflamm. Res. 2017, 10, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Mentella, M.C.; Scaldaferri, F.; Pizzoferrato, M.; Gasbarrini, A.; Miggiano, G.A.D. Nutrition, IBD and Gut Microbiota: A Review. Nutrients 2020, 12, 944. [Google Scholar] [CrossRef]
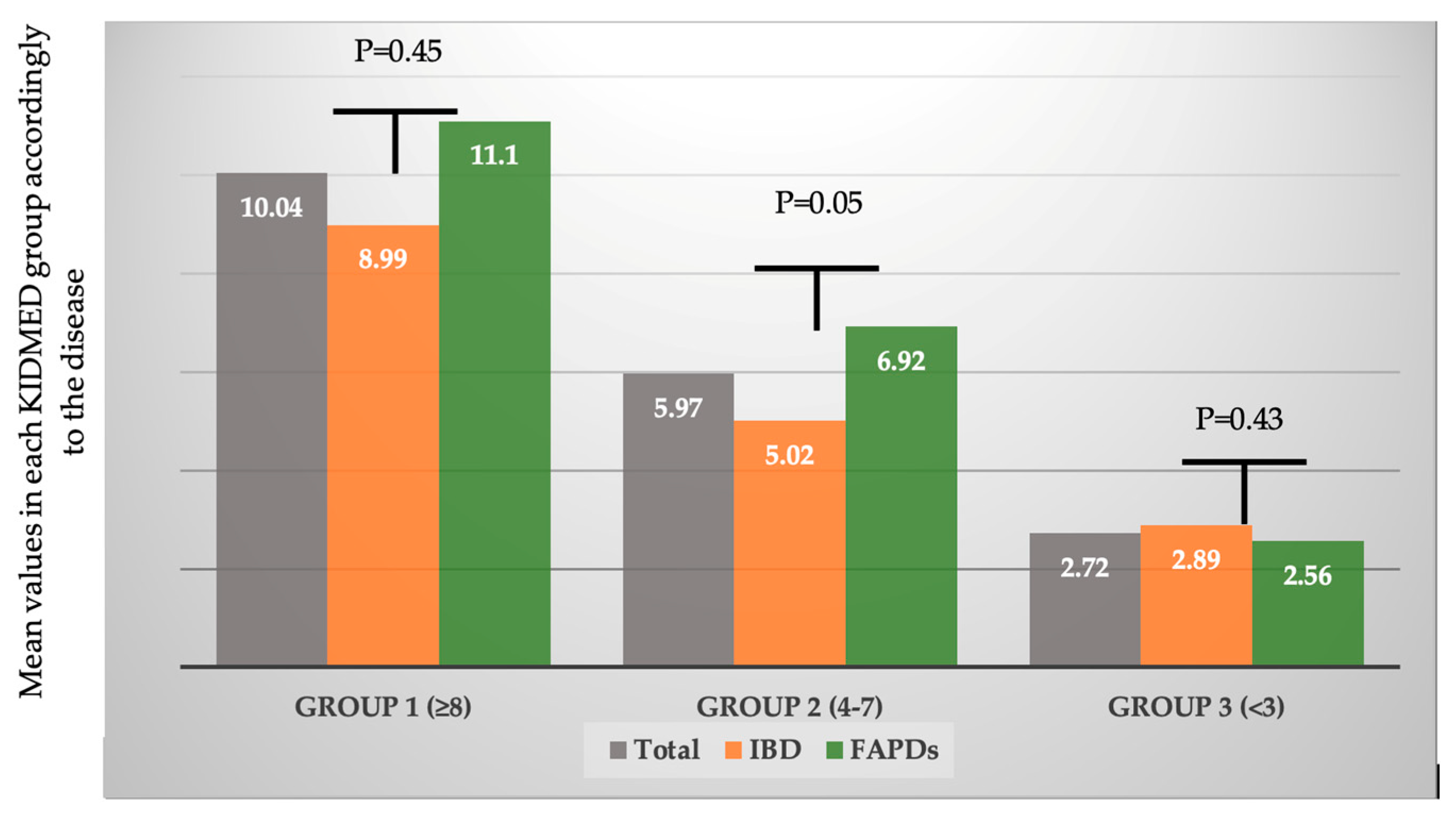
| KIDMED | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | Group 1 (Score ≥ 8) | Group 2 (Score 4–7) | Group 3 (Score < 3) | p | |||||
| IBD | FAPDs | IBD | FAPDs | IBD | FAPDs | IBD | FAPDs | ||
| n | 57 | 65 | 8 (14.03) | 10 (15.38) | 12 (21.05) | 14 (21.53) | 37 (64.91) | 41 (63.07) | 0.05 |
| Sex, n (%) | 0.03 | ||||||||
| Male, n (%) | 20 (35.09) | 23 (35.38) | 2 (3.58) | 3 (4.61) | 2 (3.58) | 4 (6.15) | 16 (28.07) | 16 (24.61) | NS |
| Female, n (%) | 37 (64.91) | 42 (64.62) | 6 (10.52) | 7 (10.76) | 10 (17.54) | 10 (15.38) | 21 (36.84) | 25 (38.46) | NS |
| Age, mean ± SD (years) | 13.1 ± 2.2 | 14.1 ± 2.6 | 12.5 ± 2.1 | 14.9 ± 3.3 | 13.0 ± 3.2 | 13.8 ± 2.8 | 10.1 ± 2.4 | 14.9 ± 3.5 | NS |
| Height, cm | 138.8 ± 16.2 | 144.4 ± 17.3 | 136.7 ± 16.1 | 145.2 ± 16.5 | 138.2 ± 16.7 | 143.8 ± 16.3 | 137.5 ± 15.4 | 144.6 ± 17.4 | NS |
| Body weight, kg | 35.4 ± 14.2 | 38.6 ± 15.3 | 36.5 ± 14.1 | 38.1 ± 15.3 | 34.4 ± 16.1 | 37.7 ± 12.3 | 35.1 ± 13.1 | 38.4 ± 15.2 | NS |
| Z score BMI mean ± SD | −2.19 ± 0.3 | 1.89 ± 0.5 | −1.89 ± 0.7 | 1.03 ± 0.3 | −2.08 ± 0.8 | 1.67 ± 0.5 | −2.21 ± 0.9 | 1.93 ± 0.9 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ţincu, I.F.; Chenescu, B.T.; Duchi, L.A.; Pleșca, D.A. Adherence to the Mediterranean Diet in Paediatric Patients with Inflammatory Bowel Disease and Functional Abdominal Pain Disorders—Comparative Study. J. Clin. Med. 2025, 14, 1971. https://doi.org/10.3390/jcm14061971
Ţincu IF, Chenescu BT, Duchi LA, Pleșca DA. Adherence to the Mediterranean Diet in Paediatric Patients with Inflammatory Bowel Disease and Functional Abdominal Pain Disorders—Comparative Study. Journal of Clinical Medicine. 2025; 14(6):1971. https://doi.org/10.3390/jcm14061971
Chicago/Turabian StyleŢincu, Iulia Florentina, Bianca Teodora Chenescu, Larisa Alexandra Duchi, and Doina Anca Pleșca. 2025. "Adherence to the Mediterranean Diet in Paediatric Patients with Inflammatory Bowel Disease and Functional Abdominal Pain Disorders—Comparative Study" Journal of Clinical Medicine 14, no. 6: 1971. https://doi.org/10.3390/jcm14061971
APA StyleŢincu, I. F., Chenescu, B. T., Duchi, L. A., & Pleșca, D. A. (2025). Adherence to the Mediterranean Diet in Paediatric Patients with Inflammatory Bowel Disease and Functional Abdominal Pain Disorders—Comparative Study. Journal of Clinical Medicine, 14(6), 1971. https://doi.org/10.3390/jcm14061971








