Impact of Education on Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Southern Italy Cohort-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Lifestyle, Clinical, and Dietary Assessments
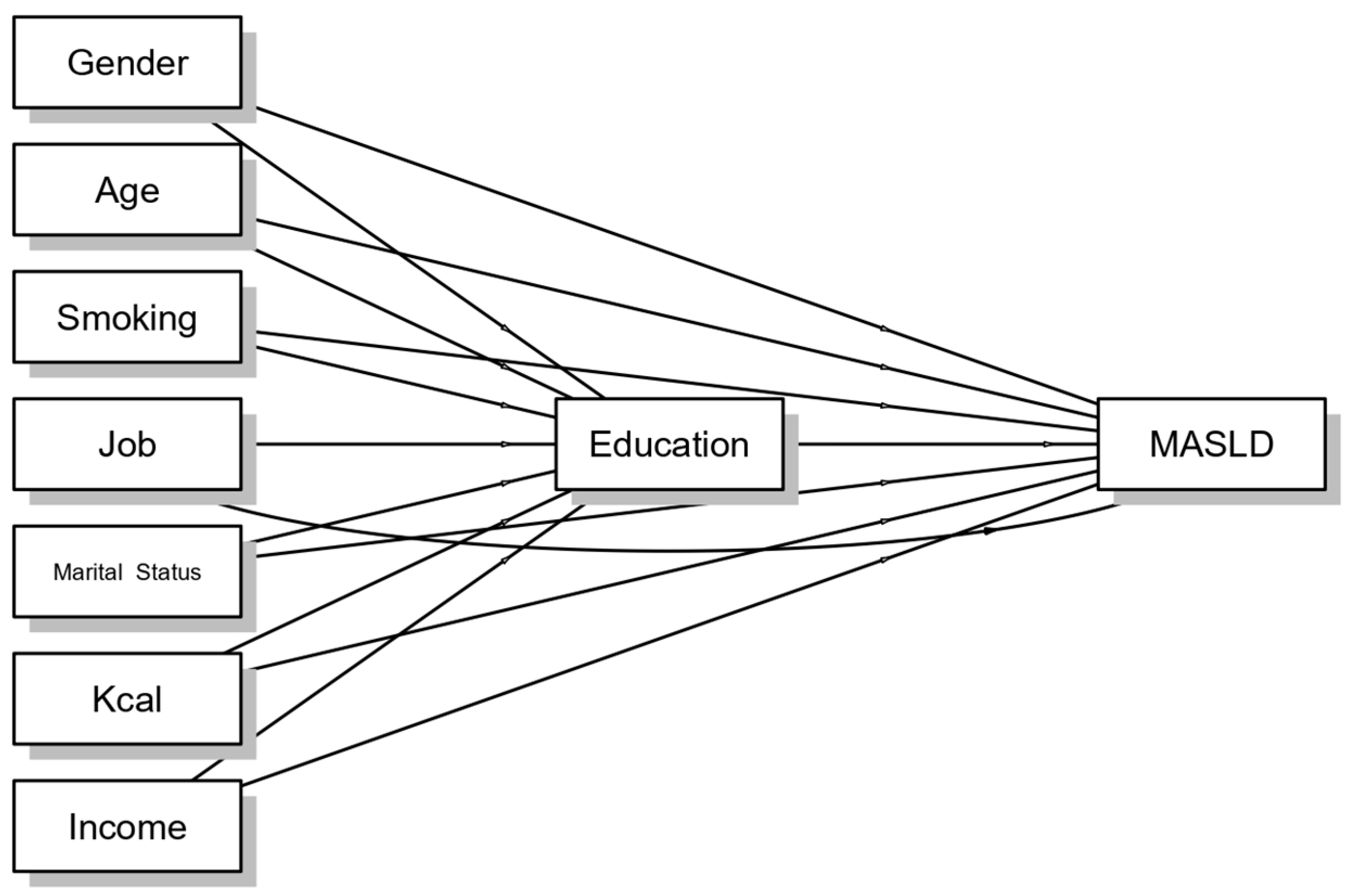
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Devarbhavi, H.; Asrani, S.K.; Arab, J.P.; Nartey, Y.A.; Pose, E.; Kamath, P.S. Global burden of liver disease: 2023 update. J. Hepatol. 2023, 79, 516–537. [Google Scholar] [CrossRef] [PubMed]
- Cotter, T.G.; Charlton, M. Nonalcoholic Steatohepatitis After Liver Transplantation. Liver Transpl. 2020, 26, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; Geroge, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef]
- Estes, C.; Anstee, Q.M.; Arias-Loste, M.; Bantel, H.; Bellentani, S.; Caballeria, J.; Colombo, M.; Craxi, A.; Crespo, J.; Day, C.P.; et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016–2030. J. Hepatol. 2018, 69, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Estes, C.; Razavi, H.; Loomba, R.; Younossi, Z.; Sanyal, A.J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018, 67, 123–133. [Google Scholar] [CrossRef]
- Younossi, Z.M.; Golabi, P.; Paik, J.M.; Henry, A.; Van Dongen, C.; Henry, L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): A systematic review. Hepatology 2023, 77, 1335–1347. [Google Scholar] [CrossRef]
- Chan, W.K.; Chuah, K.H.; Rajaram, R.B.; Lim, L.L.; Ratnasingam, J.; Vethakkan, S.R. Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review. J. Obes. Metab. Syndr. 2023, 32, 197–213. [Google Scholar] [CrossRef]
- Powell, E.E.; Wong, V.W.S.; Rinella, M. Non-alcoholic fatty liver disease. Lancet 2021, 397, 2212–2224. [Google Scholar] [CrossRef]
- Giammarino, A.M.; Qiu, H.; Bulsara, K.; Khan, S.; Jiang, Y.; Da, B.L.; Bernstein, D.E.; Satapathy, S.K. Community Socioeconomic Deprivation Predicts Nonalcoholic Steatohepatitis. Hepatol. Commun. 2022, 6, 550–560. [Google Scholar] [CrossRef]
- Ratziu, V.; Bellentani, S.; Cortez-Pinto, H.; Day, C.; Marchesini, G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J. Hepatol. 2010, 53, 372–384. [Google Scholar] [CrossRef]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 2023, 78, 1966–1986. [Google Scholar] [CrossRef] [PubMed]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zalber-Sagi, S.; Wong, V.W.S.; Dufour, J.F.; Schattneberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef]
- Riazi, K.; Azhari, H.; Charette, J.H.; Underwood, F.E.; King, J.A.; Afshar, E.E.; Swain, M.G.; Congly, S.E.; Kaplan, G.G.; Shaheen, A.A. The prevalence and incidence of NAFLD worldwide: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 851–861. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Zheng, L.; Wang, M.; Du, Y.; Jiang, J. Prevalence trends in non-alcoholic fatty liver disease at the global, regional and national levels, 1990-2017: A population-based observational study. NMJ Open 2020, 10, e036663. [Google Scholar] [CrossRef]
- Attili, A.F.; Capocaccia, R.; Carulli, N.; Festi, D.; Roda, E.; Barbara, L.; Capocaccia, L.; Menotti, A.; Okolicsanyi, L.; Ricci, G.; et al. Factors associated with gallstone disease in the MICOL experience. Multicenter Italian Study on Epidemiology of Cholelithiasis. Hepatology 1997, 26, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Chiloiro, M.; Caruso, M.G.; Cisternino, A.M.; Inguaggiato, R.; Reddavide, R.; Bonfiglio, C.; Guerra, V.; Notarnicola, M.; De Michele, G.; Correale, M.; et al. Ultrasound evaluation and correlates of fatty liver disease: A population study in a Mediterranean area. Metab. Syndr. Relat. Disord. 2013, 11, 349–358. [Google Scholar] [CrossRef]
- Sever, P. New hypertension guidelines from the National Institute for Health and Clinical Excellence and the British Hypertension Society. J. Renin-Angiotensin-Aldosterone Syst. 2006, 7, 61–63. [Google Scholar] [CrossRef]
- Cozzolongo, R.; Osella, A.R.; Elba, S.; Petruzzi, J.; Buongiorno, G.; Giannuzzi, V.; Leone, G.; Bonfiglio, C.; Lanzilotta, E.; Manghisi, O.G.; et al. Epidemiology of HCV infection in the general population: A survey in a southern Italian town. Am. J. Gastroenterol. 2009, 104, 2740–2746. [Google Scholar] [CrossRef]
- Olmedo-Requena, R.; González-Donquiles, C.; Dávila-Batista, V.; Romaguera, D.; Castelló, A.; de la Torre, A.J.; Amiano, P.; Dierssen-Sotos, T.; Guevara, M.; Fernández-Tardón, G.; et al. Agreement among Mediterranean Diet Pattern Adherence Indexes: MCC-Spain Study. Nutrients 2019, 11, 488. [Google Scholar] [CrossRef]
- Albert, J.M.; Nelson, S. Generalized causal mediation analysis. Biometrics 2011, 67, 1028–1038. [Google Scholar] [CrossRef]
- Asrani, S.K.; Devarbhavi, H.; Eaton, J.; Kamath, P.S. Burden of liver diseases in the world. J. Hepatol. 2019, 70, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Kong, L.; Ye, C.; Dou, C.; Zheng, J.; Xu, M.; Xu, Y.; Li, M.; Zhao, Z.; Lu, J.; et al. Causal impacts of educational attainment on chronic liver diseases and the mediating pathways: Mendelian randomization study. Liver Int. 2023, 43, 2379–2392. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Gomez, E.; Nephew, L.D.; Vuppalanchi, R.; Gawrieh, S.; Mladenovic, A.; Pike, F.; Samala, N.; Chalasani, N. High-quality diet, physical activity, and college education are associated with low risk of NAFLD among the US population. Hepatology 2022, 75, 1491–1506. [Google Scholar] [CrossRef]
- Xie, J.; Huang, H.; Liu, Z.; Yu, C.; Xu, L.; Xu, C. The associations between modifiable risk factors and nonalcoholic fatty liver disease: A comprehensive Mendelian randomization study. Hepatology 2023, 77, 949–964. [Google Scholar] [CrossRef]
- Zhao, Q.; Deng, Y. Education and income are associated with long-term outcome in the metabolic dysfunction-associated steatotic liver disease population. Geriatr. Gerontol. Int. 2023, 23, 975–976. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.S.; Choy, R.W.; Zhang, Y.; Chu, W.K.; Chen, L.J.; Pang, C.P.; Yam, Y.C. Global retinoblastoma survival and globe preservation: A systematic review and meta-analysis of associations with socioeconomic and health-care factors. Lancet Glob. Health 2022, 10, e380–e389. [Google Scholar] [CrossRef]
- Zajacova, A.; Lawrence, E.M. The Relationship Between Education and Health: Reducing Disparities Through a Contextual Approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef]
- Liberatos, P.; Link, B.G.; Kelsey, J.L. The measurement of social class in epidemiology. Epidemiol. Rev. 1988, 10, 87–121. [Google Scholar] [CrossRef]
- Woolf, S.H.; Braveman, P. Where health disparities begin: The role of social and economic determinants—And why current policies may make matters worse. Health Aff. 2011, 30, 1852–1859. [Google Scholar] [CrossRef]
- Kilander, L.; Berglund, L.; Boberg, M.; Vessby, B.; Lithell, H. Education, lifestyle factors and mortality from cardiovascular disease and cancer. A 25-year follow-up of Swedish 50-year-old men. Int. J. Epidemiol. 2001, 30, 1119–1126. [Google Scholar] [CrossRef]
- Alexander, M.; Loomis, A.K.; van der Lei, J.; Duarte-Salles, T.; Prieto-Alhambra, D.; Ansell, D.; Pasqua, A.; Lapi, F.; Rijnbeek, P.; Mosseveld, M.; et al. Risks and clinical predictors of cirrhosis and hepatocellular carcinoma diagnoses in adults with diagnosed NAFLD: Real-world study of 18 million patients in four European cohorts. BMC Med. 2019, 17, 95. [Google Scholar] [CrossRef] [PubMed]
- Djojosoeparto, S.K.; Kamphuis, C.B.; Harrington, J.M.; Løvhaug, A.L.; Roos, G.; Sawyer, A.D.M.; Stronks, K.; Terragni, L.; Torheim, L.E.; Vandervijvere, S.; et al. How theory can help to understand the potential impact of food environment policies on socioeconomic inequalities in diet: An application of Bourdieu’s capital theory and the scarcity theory. Eur. J. Public Health 2022, 32, iv66–iv70. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, S.A.; Paik, J.M.; Biswas, R.; Arshad, T.; Henry, L.; Younossi, Z.M. Poor Awareness of Liver Disease Among Adults with NAFLD in the United States. Hepatol. Commun. 2021, 5, 1833–1847. [Google Scholar] [CrossRef]


| Parameters * | Total Cohort (n = 2909) | Primary School (n = 847) | Middle School (n = 874) | High School (n = 892) | Graduate (n = 296) | p ^ |
|---|---|---|---|---|---|---|
| Age (yrs) | 59.69 ± 13.74 | 71.46 ± 8.09 | 58.79 ± 11.19 | 52.59 ± 12.57 | 50.01 ± 13.34 | 0.0001 |
| Gender (%) | <0.001 ¥ | |||||
| Male | 1467 (50.43) | 381 (44.98) | 477 (54.58) | 467 (52.35) | 142 (47.97) | |
| Female | 1442 (49.57) | 466 (55.02) | 397 (45.42) | 425 (47.65) | 154 (52.03) | |
| Marital Status (%) | <0.001 ¥ | |||||
| Single | 230 (8.52) | 25 (3.10) | 40 (4.92) | 111 (13.74) | 54 (19.85) | |
| Married or Cohabiting | 2193 (81.25) | 649 (80.52) | 705 (86.72) | 638 (78.96) | 201 (73.90) | |
| Divorced or Separated | 78 (2.89) | 10 (1.24) | 26 (3.20) | 32 (3.96) | 10 (3.68) | |
| Widow/er | 198 (7.34) | 122 (15.14) | 42 (5.17) | 27 (3.34) | 7 (2.57) | |
| Job (%) | <0.001 ¥ | |||||
| Managers and Professionals | 180 (6.20) | 8 (0.94) | 27 (3.10) | 75 (8.45) | 70 (23.65) | |
| Craft, Agricultural, and Sales Workers | 904 (31.14) | 48 (5.67) | 259 (29.70) | 446 (50.23) | 151 (21.01) | |
| Elementary Occupations | 324 (11.16) | 53 (6.26) | 181 (20.76) | 89 (10.02) | 1 (0.34) | |
| Housewife | 219 (7.54) | 55 (6.49) | 95 (10.89) | 61 (6.87) | 8 (2.70) | |
| Retired Individuals | 1168 (40.23) | 677 (79.93) | 269 (30.85) | 168 (18.92) | 54 (18.24) | |
| Unemployed | 108 (3.72) | 6 (0.71) | 41 (4.70) | 49 (5.52) | 12 (4.05) | |
| Income (×year) (EUR) (%) | <0.001 ¥ | |||||
| <10,000 | 99 (3.40) | 19 (2.24) | 48 (5.49) | 26 (2.91) | 6 (2.03) | |
| 10,000–20,000 | 623 (21.42) | 180 (21.25) | 249 (28.49) | 169 (18.95) | 25 (8.45) | |
| 20,000–30,000 | 615 (21.14) | 83 (9.80) | 216 (24.71) | 245 (27.47) | 71 (23.99) | |
| 30,000–40,000 | 262 (9.01) | 9 (1.06) | 53 (6.06) | 135 (15.13) | 65 (21.96) | |
| >40,000 | 195 (6.70) | 3 (0.35) | 25 (2.86) | 100 (11.21) | 67 (22.64) | |
| No Response | 1115 (38.33) | 553 (65.29) | 283 (32.38) | 217 (24.33) | 62 (20.95) | |
| Smoking Habit (%) | <0.001 ¥ | |||||
| Never/Former | 2524 (86.85) | 771 (91.03) | 754 (86.27) | 732 (82.25) | 267 (90.51) | |
| Current | 382 (13.15) | 76 (8.97) | 120 (13.73) | 158 (17.75) | 28 (9.49) | |
| rMED (%) | 0.03 ¥ | |||||
| Low | 633 (26.07) | 135 (20.90) | 208 (28.42) | 223 (28.41) | 67 (25.28) | |
| Medium | 1414 (58.24) | 398 (61.61) | 411 (56.15) | 447 (56.94) | 158 (59.62) | |
| High | 381 (15.69) | 113 (17.49) | 113 (15.44) | 115 (14.65) | 40 (15.09) |
| Parameters * | Total Cohort (n = 2909) | Primary School (n = 847) | Middle School (n = 874) | High School (n = 892) | Graduate (n = 296) | p ^ |
|---|---|---|---|---|---|---|
| Systolic Blood Pressure (mmHg) | 124.52 ± 15.94 | 132.05 ± 14.30 | 124.96 ± 15.36 | 120.07 ± 15.35 | 115.19 ± 14.05 | 0.0001 |
| Diastolic Blood Pressure (mmHg) | 78.33 ± 8.03 | 78.55 ± 7.88 | 79.27 ± 8.02 | 77.83 ± 8.06 | 76.38 ± 7.99 | 0.0001 |
| Waist Circumference (cm) | 91.66 ± 13.45 | 96.35 ± 12.59 | 92.98 ± 13.25 | 88.77 ± 13.38 | 86.66 ± 12.18 | 0.0001 |
| Hip Circumference (cm) | 102.27 ± 10.24 | 105.71 ± 10.54 | 103.05 ± 10.34 | 100.11 ± 9.56 | 99.25 ± 8.77 | 0.0001 |
| BMI (kg/m2) | 28.07 ± 5.18 | 29.73 ± 5.64 | 28.41 ± 4.90 | 26.82 ± 4.72 | 26.07 ± 4.25 | 0.0001 |
| Dyslipidemia (Yes) (%) | 576 (23.18) | 256 (32.41) | 171 (23.17) | 117 (16.50) | 32 (12.90) | <0.001 ¥ |
| Hypertension (Yes) (%) | 1049 (42.18) | 509 (64.27) | 297 (40.24) | 201 (28.35) | 42 (16.94) | <0.001 ¥ |
| Diabetes (Yes) (%) | 241 (9.70) | 136 (17.17) | 65 (8.83) | 32 (4.51) | 8 (3.23) | <0.001 ¥ |
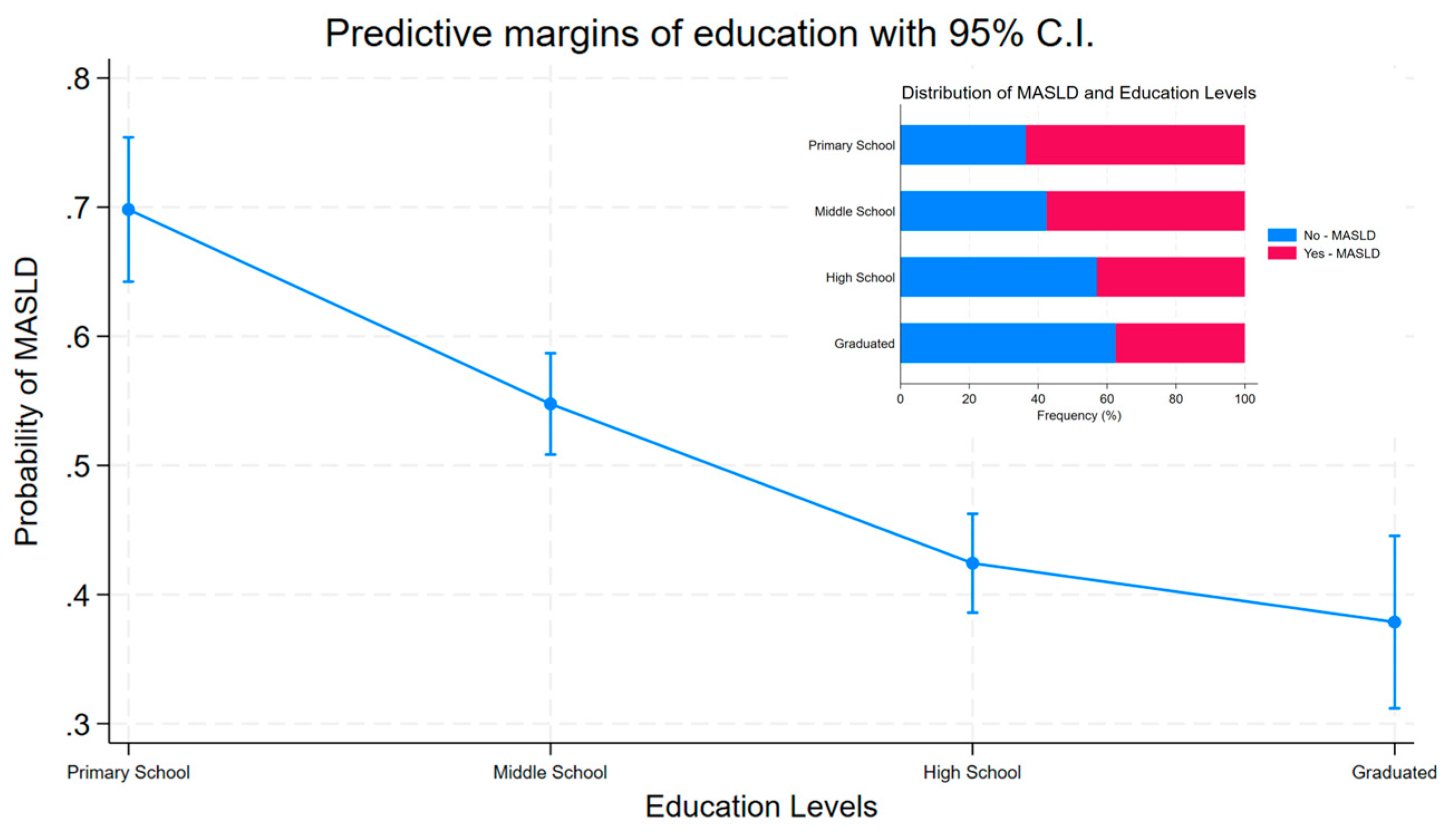
| MASLD (Yes) (%) | 1536 (52.80) | 539 (63.64) | 503 (57.55) | 383 (42.94) | 111 (37.50) | <0.001 ¥ |
| Blood | ||||||
| Triglycerides (mg/dL) | 103.01 ± 66.29 | 111.81 ± 67.58 | 101.52 ± 60.90 | 97.79 ± 67.79 | 98.79 ± 70.94 | 0.0001 |
| Total Cholesterol (mg/dL) | 191.76 ± 36.98 | 188.71 ± 38.41 | 192.16 ± 36.41 | 194.09 ± 36.23 | 192.28 ± 36.30 | 0.06 |
| HDL (mg/dL) | 50.16 ± 12.89 | 49.46 ± 12.76 | 49.77 ± 12.45 | 51.02 ± 13.42 | 50.74 ± 12.81 | 0.10 |
| Glucose (mg/dL) | 98.62 ± 22.17 | 105.01 ± 26.44 | 99.17 ± 21.03 | 94.28 ± 18.08 | 91.76 ± 17.91 | 0.0001 |
| Insulin (mmol/L) | 8.24 ± 6.28 | 8.61 ± 6.20 | 8.54 ± 6.81 | 7.94 ± 6.30 | 7.03 ± 4.19 | 0.0001 |
| HOMA | 2.12 ± 2.15 | 2.35 ± 2.30 | 2.21 ± 2.36 | 1.95 ± 1.96 | 1.67 ± 1.26 | 0.0001 |
| GOT (U/L) | 22.51 ± 14.82 | 22.65 ± 10.29 | 22.73 ± 14.74 | 22.49 ± 19.81 | 21.49 ± 5.61 | 0.86 |
| SGPT (IU/L) | 23.12 ± 16.68 | 21.97 ± 11.91 | 23.97 ± 19.59 | 23.61 ± 18.81 | 22.45 ± 11.11 | 0.003 |
| HbA1c (%) | 37.73 ± 7.17 | 40.17 ± 7.58 | 38.04 ± 7.45 | 36.88 ± 6.82 | 35.95 ± 5.74 | 0.0001 |
| Total Bilirubin (mg/dL) | 0.72 ± 0.37 | 0.70 ± 0.38 | 0.70 ± 0.35 | 0.72 ± 0.37 | 0.78 ± 10.91 | 0.01 |
| GGT (U/L) | 19.62 ± 17.62 | 20.26 ± 19.70 | 20.73 ± 20.88 | 18.56 ± 13.19 | 17.74 ± 10.91 | 0.07 |
| Alkaline Phosphatase (U/L) | 53.13 ± 16.07 | 57.12 ± 16.98 | 55.16 ± 15.94 | 50.46 ± 14.45 | 49.05 ± 16.86 | 0.0001 |
| Albumin (U/L) | 4.11 ± 0.27 | 4.04 ± 0.25 | 4.11 ± 0.26 | 4.14 ± 0.28 | 4.17 ± 0.26 | 0.0001 |
| Iron (mg/dL) | 89.93 ± 31.10 | 87.23 ± 27.99 | 89.32 ± 30.48 | 90.49 ± 32.36 | 93.64 ± 32.79 | 0.14 |
| Ferritin (ng/mL) | 100.80 ± 98.49 | 102.95 ± 91.77 | 105.69 ± 106.80 | 100.50 ± 99.50 | 85.75 ± 78.97 | 0.01 |
| CRP (mg/dL) | 0.26 ± 0.54 | 0.30 ± 0.49 | 0.28 ± 0.59 | 0.24 ± 0.52 | 0.21 ± 0.48 | 0.0001 |
| Ceruloplasmin (mg/dL) | 31.46 ± 7.44 | 32.06 ± 7.04 | 31.70 ± 7.04 | 31.45 ± 8.24 | 30.02 ± 6.28 | 0.0002 |
| α1AT (mg/dL) | 166.55 ± 36.34 | 172.32 ± 32.61 | 169.32 ± 35.66 | 164.31 ± 38.23 | 157.76 ± 35.38 | 0.0001 |
| OR | se (OR) | p | 95% C.I. | |
|---|---|---|---|---|
| Model 1 | ||||
| Education | ||||
| Primary School [Ref.] | -- | -- | -- | -- |
| Middle School | 0.88 | 0.09 | 0.24 | 0.72 to 1.08 |
| High School | 0.58 | 0.06 | <0.001 | 0.47 to 0.72 |
| Graduate | 0.52 | 0.08 | <0.001 | 0.38 to 0.70 |
| Model 2 | ||||
| Education | ||||
| Primary School [Ref.] | -- | -- | -- | -- |
| Middle School | 0.50 | 0.08 | <0.001 | 0.36 to 0.69 |
| High School | 0.29 | 0.05 | <0.001 | 0.21 to 0.41 |
| Graduate | 0.24 | 0.05 | <0.001 | 0.16 to 0.37 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Donghia, R.; Bonfiglio, C.; Giannelli, G.; Tatoli, R. Impact of Education on Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Southern Italy Cohort-Based Study. J. Clin. Med. 2025, 14, 1950. https://doi.org/10.3390/jcm14061950
Donghia R, Bonfiglio C, Giannelli G, Tatoli R. Impact of Education on Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Southern Italy Cohort-Based Study. Journal of Clinical Medicine. 2025; 14(6):1950. https://doi.org/10.3390/jcm14061950
Chicago/Turabian StyleDonghia, Rossella, Caterina Bonfiglio, Gianluigi Giannelli, and Rossella Tatoli. 2025. "Impact of Education on Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Southern Italy Cohort-Based Study" Journal of Clinical Medicine 14, no. 6: 1950. https://doi.org/10.3390/jcm14061950
APA StyleDonghia, R., Bonfiglio, C., Giannelli, G., & Tatoli, R. (2025). Impact of Education on Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A Southern Italy Cohort-Based Study. Journal of Clinical Medicine, 14(6), 1950. https://doi.org/10.3390/jcm14061950







