Assessment of Safety and Efficacy of Expanded Hemodialysis with Medium Cut-Off Dialyzer Compared to Haemodiafiltration
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
- Group 1, HDx with Asahi Kasei Medical ViE-X
- Group 2, HDx Baxter Theranova 400;
- Group 3, HDF with Fresenius CorDiax Fx80.
2.2. Patients’ Selection
2.3. Laboratory Sampling
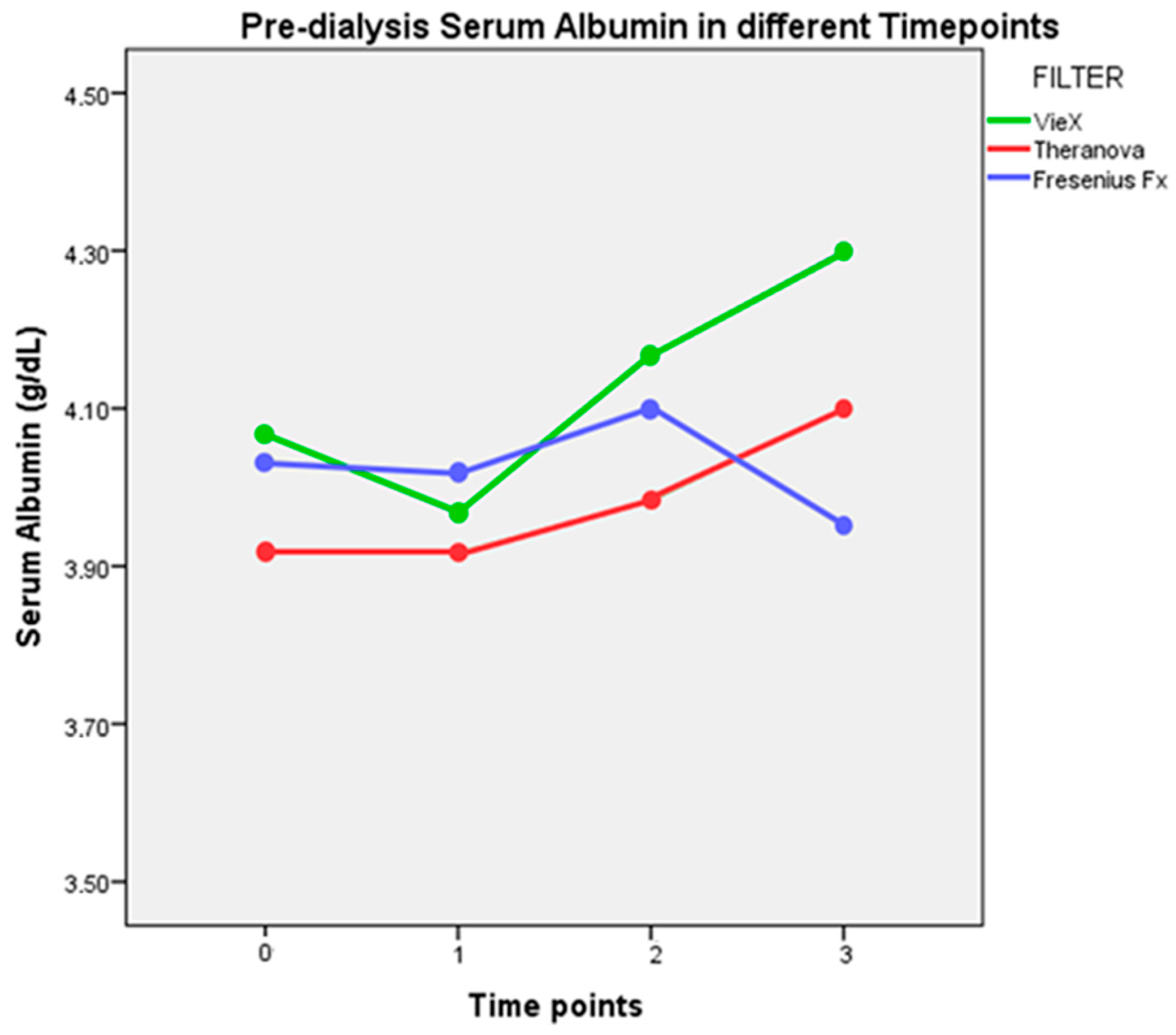
- T0. First HD session analysed and first use of ViE-X dialyzer in Group 1;
- T1. After one month from the first HD session;
- T2. After two months from the first HD session;
- T3. After three months from the first HD session.
- Initial part of HD session (I), taken 15 min after the beginning of HD session;
- Final part of HD session (F), taken 15 min from the end of HD session.
2.4. Calculations
2.5. Statistical Analysis
3. Results
3.1. Primary Endpoint
3.2. Secondary Endpoint
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Locatelli, F.; Gauly, A.; Czekalski, S.; Hannedouche, T.; Jacobson, S.H.; Loureiro, A.; Martin-Malo, A.; Papadimitriou, M.; Passlick-Deetjen, J.; Ronco, C.; et al. The MPO Study: Just a European HEMO Study or something very different? Blood Purif. 2008, 26, 100–104. [Google Scholar] [CrossRef]
- Kuragano, T.; Kida, A.; Furuta, M.; Nanami, M.; Otaki, Y.; Hasuike, Y.; Nonoguchi, H.; Nakanishi, T. The impact of beta2-microglobulin clearance on the risk factors of cardiovascular disease in hemodialysis patients. ASAIO J. 2010, 56, 326–332. [Google Scholar] [CrossRef]
- Nakano, T.; Matsui, M.; Inoue, I.; Awata, T.; Katayama, S.; Murakoshi, T. Free immunoglobulin light chain: Its biology and implications in diseases. Clin. Chim. Acta 2011, 412, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Ronco, C. The Rise of Expanded Hemodialysis. Blood Purif. 2017, 44, I–VIII. [Google Scholar] [CrossRef]
- Sakurai, K. Biomarkers for evaluation of clinical outcomes of hemodiafiltration. Blood Purif. 2013, 35 (Suppl. 1), 64–68. [Google Scholar] [CrossRef] [PubMed]
- Scholze, A.; Jankowski, J.; Pedraza-Chaverri, J.; Evenepoel, P. Oxidative Stress in Chronic Kidney Disease. Oxidative Med. Cell. Longev. 2016, 2016, 8375186. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.T.; Ahmed, F.A.; Hamm, L.L.; Teran, F.J.; Chen, C.-S.; Liu, Y.; Shah, K.; Rifai, N.; Batuman, V.; Simon, E.E.; et al. Association of C-reactive protein, tumor necrosis factor-alpha, and interleukin-6 with chronic kidney disease. BMC Nephrol. 2015, 16, 77. [Google Scholar] [CrossRef]
- Kaltsatou, A.; Sakkas, G.K.; Poulianiti, K.P.; Koutedakis, Y.; Tepetes, K.; Christodoulidis, G.; Stefanidis, I.; Karatzaferi, C. Uremic myopathy: Is oxidative stress implicated in muscle dysfunction in uremia? Front. Physiol. 2015, 6, 102. [Google Scholar] [CrossRef]
- Aucella, F.; Gesuete, A.; Vigilante, M.; Prencipe, M. Adsorption dialysis: From physical principles to clinical applications. Blood Purif. 2013, 35, 42–47. [Google Scholar] [CrossRef]
- Canaud, B.; Barbieri, C.; Marcelli, D.; Bellocchio, F.; Bowry, S.; Mari, F.; Amato, C.; Gatti, E. Optimal convection volume for improving patient outcomes in an international incident dialysis cohort treated with online hemodiafiltration. Kidney Int. 2015, 88, 1108–1116. [Google Scholar] [CrossRef]
- Tattersall, J.E.; Ward, R.A. Online haemodiafiltration: Definition, dose quantification and safety revisited. Nephrol. Dial. Transplant. 2013, 28, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, A.H.; Lyko, R.; Nilsson, L.-G.; Beck, W.; Amdahl, M.; Lechner, P.; Schneider, A.; Wanner, C.; Rosenkranz, A.R.; Krieter, D.H. Performance of hemodialysis with novel medium cut-off dialyzers. Nephrol. Dial. Transplant. 2017, 32, 165–172. [Google Scholar] [CrossRef]
- Fiore, G.B.; Ronco, C. Principles and practice of internal hemodiafiltration. Contrib. Nephrol. 2007, 158, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Ronco, C.; Marchionna, N.; Brendolan, A.; Neri, M.; Lorenzin, A.; Rueda, A.J.M. Expanded haemodialysis: From operational mechanism to clinical results. Nephrol. Dial. Transplant. 2018, 33 (Suppl. 3), iii41–iii47. [Google Scholar] [CrossRef]
- Maduell, F. Hemodiafiltration versus conventional hemodialysis: Should “conventional” be redefined? Semin. Dial. 2018, 31, 625–632. [Google Scholar] [CrossRef]
- Weiner, D.E.; Falzon, L.; Skoufos, L.; Bernardo, A.; Beck, W.; Xiao, M.; Tran, H. Efficacy and Safety of Expanded Hemodialysis with the Theranova 400 Dialyzer A Randomized Controlled Trial. Clin. J. Am. Soc. Nephrol. 2020, 15, 1310–1319. [Google Scholar] [CrossRef] [PubMed]
- Lowrie, E.G.; Lew, N.L. Death risk in hemodialysis patients: The predictive value of commonly measured variables and an evaluation of death rate differences between facilities. Am. J. Kidney Dis. 1990, 15, 458–482. [Google Scholar] [CrossRef]
- Van Gelder, M.K.; Abrahams, A.C.; Joles, J.A.; Kaysen, G.A.; Gerritsen, K.G.F. Albumin handling in different hemodialysis modalities. Nephrol. Dial. Transplant. 2018, 33, 906–913. [Google Scholar] [CrossRef]
- Cozzolino, M.; Magagnoli, L.; Ciceri, P.; Conte, F.; Galassi, A. Effects of a medium cut-off (Theranova®) dialyser on haemodialysis patients: A prospective, cross-over study. Clin. Kidney J. 2021, 14, 382–389. [Google Scholar] [CrossRef]
- Krishnasamy, R.; Hawley, C.M.; Jardine, M.J.; Roberts, M.A.; Cho, Y.; Wong, M.; Heath, A.; Nelson, C.L.; Sen, S.; Mount, P.F.; et al. A tRial Evaluating Mid Cut-Off Value Membrane Clearance of Albumin and Light Chains in HemoDialysis Patients: A Safety Device Study. Blood Purif. 2020, 49, 468–478. [Google Scholar] [CrossRef]
- Rocco, M.V.; Daugirdas, J.T.; Depner, T.A.; Inrig, J.; Mehrotra, R.; Suri, R.S.; Weiner, D.E.; Greer, N.; Ishani, A.; MacDonald, R.; et al. KDOQI Clinical Practice Guideline for Hemodialysis Adequacy: 2015 Update. Am. J. Kidney Dis. 2015, 66, 884–930. [Google Scholar] [CrossRef]
- Pstras, L.; Ronco, C.; Tattersall, J. Basic physics of hemodiafiltration. Semin. Dial. 2022, 35, 390–404. [Google Scholar] [CrossRef] [PubMed]
- Lorenzin, A.; Neri, M.; Lupi, A.; Todesco, M.; Santimaria, M.; Alghisi, A.; Brendolan, A.; Ronco, C. Quantification of Internal Filtration in Hollow Fiber Hemodialyzers with Medium Cut-Off Membrane. Blood Purif. 2018, 46, 196–204. [Google Scholar] [CrossRef]
- Maduell, F.; Broseta, J.J.; Rodas, L.; Montagud-Marrahi, E.; Rodriguez-Espinosa, D.; Hermida, E.; Arias-Guillén, M.; Fontseré, N.; Vera, M.; Gómez, M.; et al. Comparison of Solute Removal Properties Between High-Efficient Dialysis Modalities in Low Blood Flow Rate. Ther. Apher. Dial. 2020, 24, 387–392. [Google Scholar] [CrossRef]
- Maduell, F.; Broseta, J.J.; Gómez, M.; Racionero, P.; Montagud-Marrahi, E.; Rodas, L.; Arias-Guillén, M.; Fontseré, N.; Vera, M.; Rico, N. Determining factors for hemodiafiltration to equal or exceed the performance of expanded hemodialysis. Artif. Organs 2020, 44, E448–E458. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Jang, M.-J.; Jeon, J.; Lee, J.E.; Huh, W.; Choi, B.S.; Park, C.W.; Chin, H.J.; Kang, C.L.; Kim, D.K.; et al. Cardiovascular Risk Comparison between Expanded Hemodialysis Using Theranova and Online Hemodiafiltration (CARTOON): A Multicenter Randomized Controlled Trial. Sci. Rep. 2021, 11, 10807. [Google Scholar] [CrossRef]
- Yang, S.-K.; Xiao, L.; Xu, B.; Xu, X.-X.; Liu, F.-Y.; Sun, L. Effects of vitamin E-coated dialyzer on oxidative stress and inflammation status in hemodialysis patients: A systematic review and meta-analysis. Ren. Fail. 2014, 36, 722–731. [Google Scholar] [CrossRef]
- Rodríguez-Ribera, L.; Corredor, Z.; Silva, I.; Díaz, J.M.; Ballarín, J.; Marcos, R.; Pastor, S.; Coll, E. Vitamin E-coated dialysis membranes reduce the levels of oxidative genetic damage in hemodialysis patients. Mutat. Res. Toxicol. Environ. Mutagen. 2017, 815, 16–21. [Google Scholar] [CrossRef]
- Girndt, M.; Lengler, S.; Kaul, H.; Sester, U.; Sester, M.; Köhler, H. Prospective crossover trial of the influence of vitamin E–coated dialyzer membranes on T-cell activation and cytokine induction. Am. J. Kidney Dis. 2000, 35, 95–104. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions, and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |
| HDx | HDF | p-Value | ||
|---|---|---|---|---|
| Group | 1 | 2 | 3 | |
| Filter | ViE-X | Theranova | Fresenius CorDiax | |
| Nr of patients (n/%) | 6/25 | 6/25 | 6/25 | |
| AGE (mean ± SD) | 67.6 ± 4.1 | 65.17 ± 7.73 | 70.33 ± 10.1 | ns |
| SEX (male) (n/%) | 4/66.7 | 4/66.7 | 3/50 | ns |
| BMI (mean ± SD) | 27.3 ± 4.3 | 24.67 ± 5.68 | 22.82 ± 1.64 | ns |
| URINE OUTPUT (n/%) | ns | |||
| <100 mL | 1/16.7 | 1/16.7 | 5/83.3 | |
| <500 mL | 3/50 | 4/66.7 | 1/16.7 | |
| >500 mL | 2/33.3 | 1/16.7 | 0 | |
| DIABETES (n/%) | 2/33.3 | 1/16.7 | 3/50 | ns |
| CHARLSON > 6 (n/%) | 3/50 | 2/33.3 | 3/50 | ns |
| CHARLSON (mean ± SD) | 7.1 ± 0.9 | 5.67 ± 2.16 | 6.83 ± 2.99 | ns |
| CKD CAUSE (n/%) | ns | |||
| UNKNOWN | 4/66.7 | 1/16.7 | 5/83.3 | |
| GLOMERULAR | 2/33.3 | 3/50 | 0 | |
| OBSTRUCTIVE | 0 | 1/16.7 | 1/16.7 | |
| ADPKD | 0 | 1/16.7 | 0 | |
| DIALISYS VINTAGE (months) (median/IQR) | 15 [2.5–42.5] | 91 [18.5–113.2] | 149.8 [37–100] | 0.042 |
| VASCULAR ACCESS (n/%) | ns | |||
| AVF | 5/83.3 | 3/50 | 5/83.3 | |
| CVC | 1/16.7 | 3/50 | 1/16.7 | |
| Qb (mL/min) (median/IQR) | 290 [281–300] | 300 [287–300] | 300 [300–350] | <0.001 |
| Qf (mL/min) (median/IQR) | 13.15 [12.3–14] | 11.8 [7.9–14.3] | 99.1 [85.9–108.2] | <0.001 |
| Mean Albumin Loss (g) | |
|---|---|
| Vie-X | 2.9 |
| Theranova | 3.7 |
| Fresenius-Fx | 2.5 |
| Vie-X | Theranova | Fresenius Fx | p-Value | |
|---|---|---|---|---|
| RR Creatinine (Mean ± SD) | 65.5 ± 6.3 | 66.3 ± 6.3 | 66.9 ± 5.1 | ns |
| RR Phosphate (Mean ± SD) | 58.2 ± 11.2 | 56.1 ± 9.4 | 60.2 ± 7.3 | ns |
| RR Urea (Mean ± SD) | 72.9 ± 5.1 | 72.1 ± 6.2 | 75.0 ± 4.4 | ns |
| Kt/V (ID) ∗ (Mean ± SD) | 1.30 ± 0.16 | 1.27 ± 0.17 | 1.29 ± 0.10 | ns |
| ViE-X | Theranova | Fresenius | p-Value | ||
|---|---|---|---|---|---|
| InterLeukin-6 (Mean ± SD) | Pre | 6.93 ± 0.15 | 6.96 ± 0.17 | 6.88 ± 0.16 | ns |
| Post | 6.86 ± 0.28 | 6.90 ± 0.17 | 6.88 ± 0.07 | ns | |
| RR | 0.9 ± 3.7 | 0.9 ± 2.6 | −0.05 ± 2.9 | ns | |
| β2-microglobulin (Mean ± SD) | Pre | 13.7 ± 2.8 | 16.0 ± 2.9 | 16.5 ± 3.6 | ns |
| Post | 6.9 ± 1.1 | 7.2 ± 2.2 | 7.5 ± 1.8 | ns | |
| RR | 48.2 ± 8.9 | 55.9 ± 9.3 | 55.7 ± 13.2 | ns | |
| α1-microglobulin (Mean ± SD) | Pre | 222.4 ± 54.1 | 212.7 ± 25.0 | 264.5 ± 22.0 | <0.001 |
| Post | 232.4 ± 57.9 | 211.7 ± 33.1 | 254.0 ± 46.8 | 0.012 | |
| RR | −4.5 ± 5.8 | 0.7 ± 13.2 | 4.5 ± 12.9 | 0.024 | |
| Myoglobin (Mean ± SD) | Pre | 196.4 ± 86.2 | 266.6 ± 121 | 198.2 ± 73.8 | 0.005 |
| Post | 118.9 ± 46.5 | 135.2 ± 47.1 | 123.2 ± 73.5 | ns | |
| RR | 38.1 ± 8.6 | 47.1 ± 9 | 38.6 ± 23.1 | 0.07 |
| Uraemic Toxins (Mean ± SD) | ViE-X | Theranova | Fresenius | p-Value |
|---|---|---|---|---|
| Urea | 258 ± 16 | 258 ± 15 | 277 ± 29 | 0.003 |
| Creatinine | 133 ± 15 | 145 ± 13 | 151 ± 20 | 0.001 |
| Interleukin-6 | 23.1 ± 17.4 | 12.8 ± 8 | 107.0 ± 28.1 | <0.001 |
| β2-microglobulin | 75.4 ± 12.6 | 86.9 ±10.1 | 128.5 ± 32.4 | <0.001 |
| α1-microglobulin | 8.8 ± 5.3 | 8.0 ± 7.3 | 101.6 ± 42.1 | <0.001 |
| Myoglobin | 58.3 ± 9.8 | 69.7 ± 11.9 | 94.5 ± 46.1 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcello, M.; Simonini, M.; Lorenzin, A.; Corradi, V.; Virzì, G.M.; Caprara, C.; Brendolan, A.; Benedetti, C.; Lentini, P.; Zanella, M.; et al. Assessment of Safety and Efficacy of Expanded Hemodialysis with Medium Cut-Off Dialyzer Compared to Haemodiafiltration. J. Clin. Med. 2025, 14, 1798. https://doi.org/10.3390/jcm14061798
Marcello M, Simonini M, Lorenzin A, Corradi V, Virzì GM, Caprara C, Brendolan A, Benedetti C, Lentini P, Zanella M, et al. Assessment of Safety and Efficacy of Expanded Hemodialysis with Medium Cut-Off Dialyzer Compared to Haemodiafiltration. Journal of Clinical Medicine. 2025; 14(6):1798. https://doi.org/10.3390/jcm14061798
Chicago/Turabian StyleMarcello, Matteo, Marco Simonini, Anna Lorenzin, Valentina Corradi, Grazia Maria Virzì, Carlotta Caprara, Alessandra Brendolan, Claudia Benedetti, Paolo Lentini, Monica Zanella, and et al. 2025. "Assessment of Safety and Efficacy of Expanded Hemodialysis with Medium Cut-Off Dialyzer Compared to Haemodiafiltration" Journal of Clinical Medicine 14, no. 6: 1798. https://doi.org/10.3390/jcm14061798
APA StyleMarcello, M., Simonini, M., Lorenzin, A., Corradi, V., Virzì, G. M., Caprara, C., Brendolan, A., Benedetti, C., Lentini, P., Zanella, M., & Ronco, C. (2025). Assessment of Safety and Efficacy of Expanded Hemodialysis with Medium Cut-Off Dialyzer Compared to Haemodiafiltration. Journal of Clinical Medicine, 14(6), 1798. https://doi.org/10.3390/jcm14061798







