Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Variables
2.3. Statistical Analysis
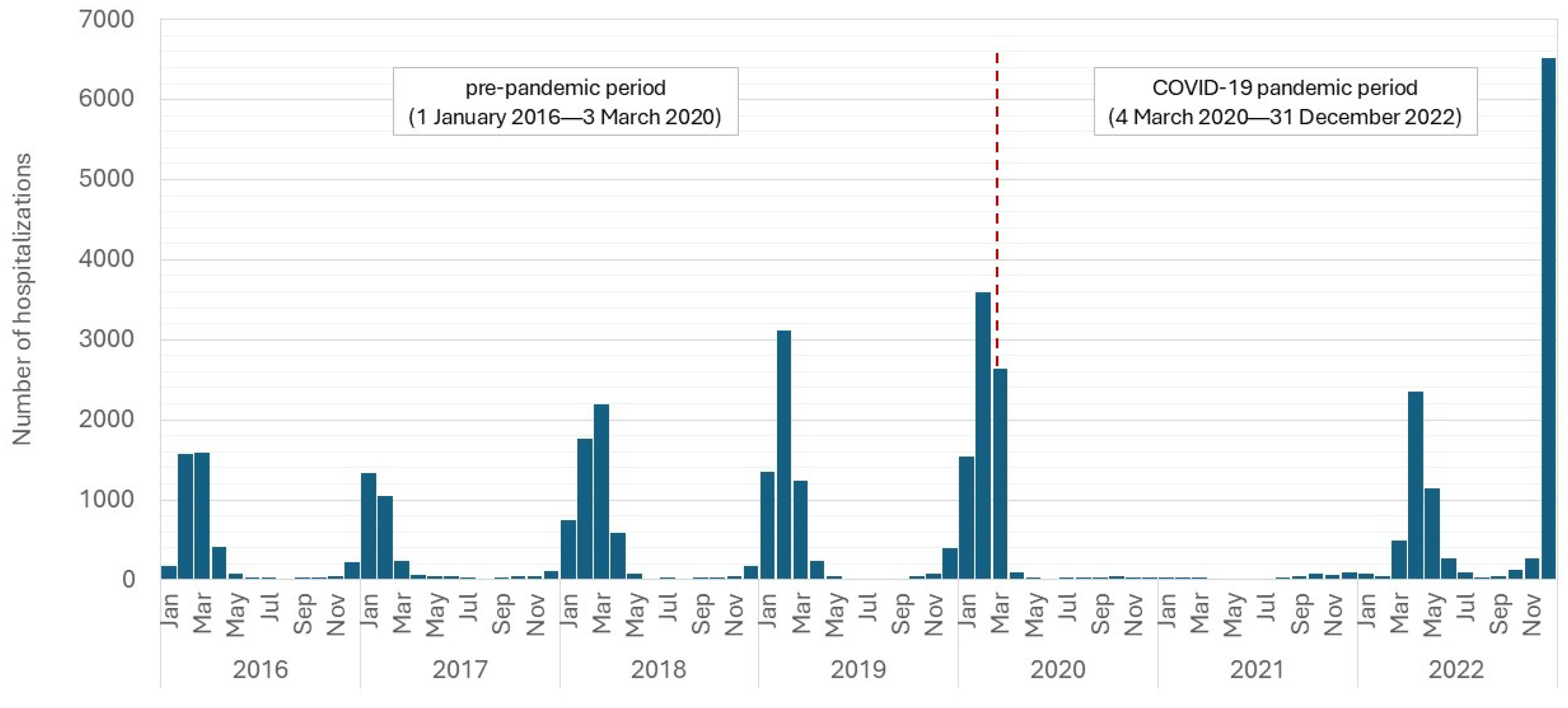
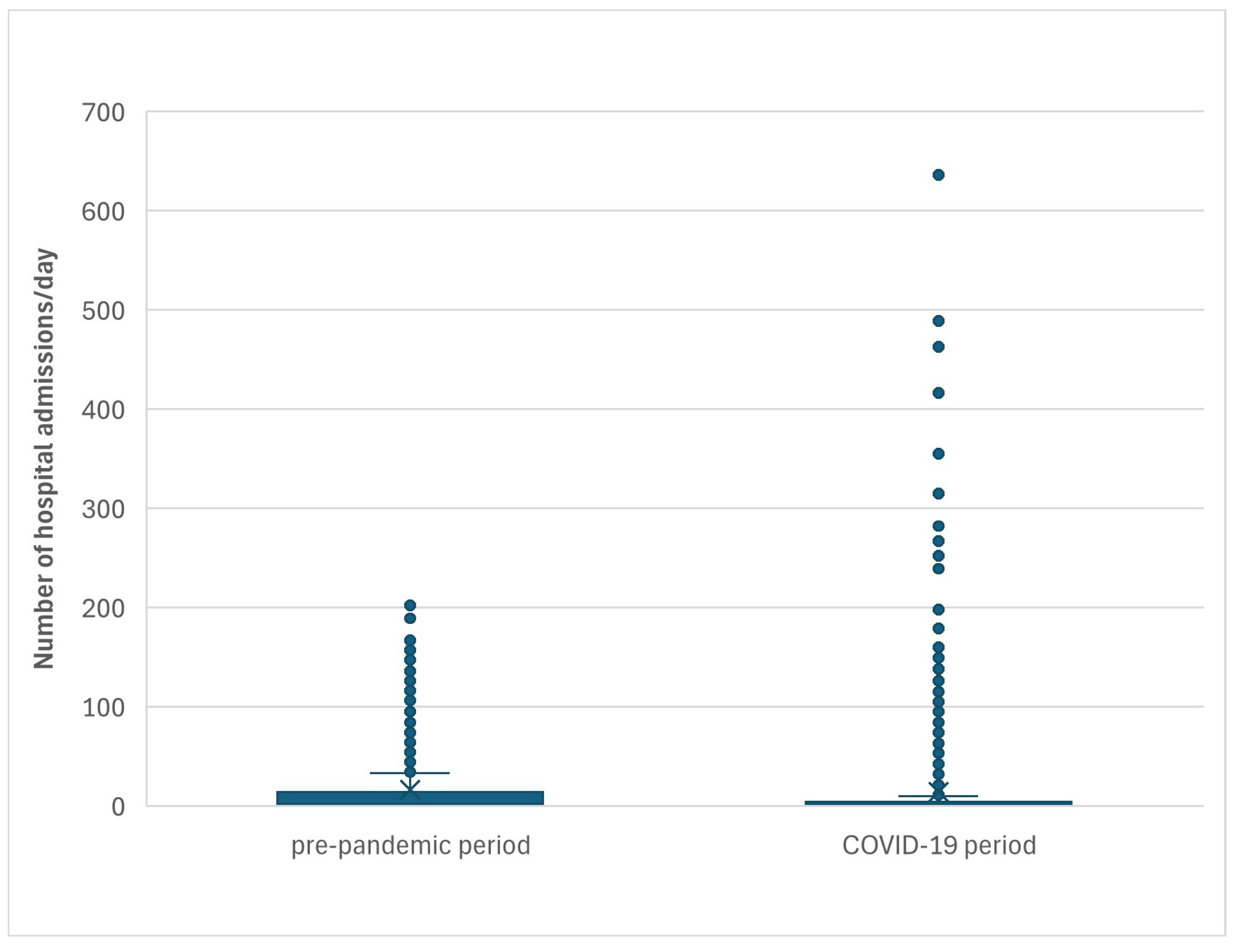
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ryu, S.; Cowling, B.J. Human Influenza Epidemiology. Cold Spring Harb. Perspect. Med. 2021, 11, a038356. [Google Scholar] [CrossRef] [PubMed]
- Talbot, H.K. Influenza in Older Adults. Infect. Dis. Clin. N. Am. 2017, 31, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Maleki, F.; Welch, V.; Lopez, S.M.C.; Cane, A.; Langer, J.; Enstone, A.; Markus, K.; Wright, O.; Hewitt, N.; Whittle, I. Understanding the Global Burden of Influenza in Adults Aged 18–64 years: A Systematic Literature Review from 2012 to 2022. Adv. Ther. 2023, 40, 4166–4188. [Google Scholar] [CrossRef] [PubMed]
- McElhaney, J.E.; Andrew, M.K.; Haynes, L.; Kuchel, G.A.; McNeil, S.A.; Pawelec, G. Influenza Vaccination: Accelerating the Process for New Vaccine Development in Older Adults. Interdiscip. Top. Gerontol. Geriatr. 2020, 43, 98–112. [Google Scholar]
- Doyon-Plourde, P.; Fakih, I.; Tadount, F.; Tadount, F.; Fortin, É.; Quach, C. Impact of influenza vaccination on healthcare utilization—A systematic review. Vaccine 2019, 37, 3179–3189. [Google Scholar] [CrossRef]
- Lafond, K.E.; Porter, R.M.; Whaley, M.J.; Suizan, Z.; Ran, Z.; Aleem, M.A.; Thapa, B.; Sar, B.; Proschle, V.S.; Peng, Z.; et al. Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: A systematic review and meta-analysis. PLoS Med. 2021, 18, e1003550. [Google Scholar] [CrossRef]
- Tanner, A.R.; Dorey, R.B.; Brendish, N.J.; Clark, T.W. Influenza vaccination: Protecting the most vulnerable. Eur. Respir. Rev. 2021, 30, 200258. [Google Scholar] [CrossRef]
- Behrouzi, B.; Bhatt, D.L.; Cannon, C.P.; Vardeny, O.; Lee, D.S.; Solomon, S.D.; Udell, J.A. Association of Influenza Vaccination With Cardiovascular Risk: A Meta-analysis. JAMA Netw. Open 2022, 5, e228873. [Google Scholar] [CrossRef]
- Liu, R.; Fan, Y.; Patel, A.; Liu, H.; Du, X.; Liu, B.; Di Tanna, G.L. The association between influenza vaccination, cardiovascular mortality and hospitalization: A living systematic review and prospective meta-analysis. Vaccine 2024, 42, 1034–1041. [Google Scholar] [CrossRef]
- Wpływ Pandemii COVID-19 na Potrzeby Zdrowotne w Polsce. Available online: https://basiw.mz.gov.pl/mapy-informacje/mapa-2022-2026/analizy/dodatkowe-analizy/ (accessed on 15 February 2025).
- Available online: https://covid19.who.int (accessed on 15 February 2025).
- Available online: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2 (accessed on 15 February 2025).
- Available online: https://wwwold.pzh.gov.pl/oldpage/epimeld/index_p.html (accessed on 28 May 2024).
- Maggi, S.; Veronese, N.; Burgio, M.; Cammarata, G.; Ciuppa, M.E.; Ciriminna, S.; Di Gennaro, F.; Smith, L.; Trott, M.; Dominguez, L.J.; et al. Rate of Hospitalizations and Mortality of Respiratory Syncytial Virus Infection Compared to Influenza in Older People: A Systematic Review and Meta-Analysis. Vaccines 2022, 10, 2092. [Google Scholar] [CrossRef]
- de-Miguel-Díez, J.; Lopez-de-Andres, A.; Hernandez-Barrera, V.; Jimenez-Trujillo, I.; Mendez-Bailon, M.; de Miguel-Yanes, J.M.; Muñoz-Rivas, N.; Romero-Maroto, M.; Jimenez-Garcia, R. Retrospective observational analysis of hospital discharge database to characterize primary pulmonary hypertension and its outcomes in Spain from 2004 to 2015. Medicine 2019, 98, e15518. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Baz, I.; Navascués, A.; Trobajo-Sanmartín, C.; Pozo, F.; Fernández-Huerta, M.; Olazabal-Arruiz, M.; Argente-Colas, L.; Ezpeleta, G.; Echeverria, A.; Casado, I.; et al. Effectiveness of influenza vaccination in preventing confirmed influenza cases and hospitalizations in Northern Spain, 2023/24 season: A population-based test-negative case-control study. Int. J. Infect. Dis. 2025, 151, 107364. [Google Scholar] [CrossRef] [PubMed]
- Statistics Poland. Available online: https://stat.gov.pl (accessed on 24 May 2024).
- TIBCO Software Inc. Statistica (Data Analysis Software System), Version 13. Available online: https://www.statistica.com/en/software/tibco-data-science-/-tibco-statistica (accessed on 1 October 2020).
- Abramson, J.H. WINPEPI Updated: Computer Programs for Epidemiologists, and Their Teaching Potential. Epidemiol. Perspect. 2011, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Lumley, T.; Diehr, P.; Emerson, S.; Chen, L. The Importance of the Normality Assumption in Large Public Health Data Sets. Annu. Rev. Public Health 2002, 23, 151–169. [Google Scholar] [CrossRef]
- Lin, F.; Liang, J.L.; Guan, Z.X.; Wu, M.; Yang, L.Y. Hospitalized children with influenza A before, during and after COVID-19 pandemic: A retrospective cohort study. BMC Pediatr. 2024, 24, 828. [Google Scholar] [CrossRef]
- Alsallakh, M.; Adeloye, D.; Vasileiou, E.; Sivakumaran, S.; Akbari, A.; Lyons, R.A.; Robertson, C.; Rudan, I.; Davies, G.A.; Sheikh, A. Impact of the COVID-19 Pandemic on Influenza Hospital Admissions and Deaths in Wales: Descriptive National Time Series Analysis. JMIR Public Health Surveill. 2024, 10, e43173. [Google Scholar] [CrossRef]
- Ramos-Rincón, J.M.; Pinargote-Celorio, H.; González-de-la-Aleja, P.; Sánchez-Payá, J.; Reus, S.; Rodríguez-Díaz, J.C.; Merino, E. Impact of influenza related hospitalization in Spain: Characteristics and risk factor of mortality during five influenza seasons (2016 to 2021). Front. Public Health 2024, 12, 1360372. [Google Scholar] [CrossRef]
- Pivette, M.; Nicolay, N.; de Lauzun, V.; Hubert, B. Characteristics of hospitalizations with an influenza diagnosis, France, 2012–2013 to 2016–2017 influenza seasons. Influenza Other Respir. Viruses 2020, 14, 340–348. [Google Scholar] [CrossRef]
- Froes, F.; Carmo, M.; Lopes, H.; Bizouard, G.; Gomes, C.; Martins, M.; Bricout, H.; de Courville, C.; de Sousa, J.C.; Rabaçal, C.; et al. Excess hospitalizations and mortality associated with seasonal influenza in Portugal, 2008–2018. BMC Infect. Dis. 2022, 22, 726. [Google Scholar] [CrossRef]
- Hauge, S.H.; Bakken, I.J.; de Blasio, B.F.; Håberg, S.E. Burden of medically attended influenza in Norway 2008–2017. Influenza Other Respir. Viruses 2019, 13, 240–247. [Google Scholar] [CrossRef]
- Matias, G.; Taylor, R.J.; Haguinet, F.; Schuck-Paim, C.; Lustig, R.L.; Fleming, D.M. Modelling estimates of age-specific influenza-related hospitalisation and mortality in the United Kingdom. BMC Public Health 2016, 16, 481. [Google Scholar] [CrossRef] [PubMed]
- Paget, J.; Staadegaard, L.; Wang, X.; Li, Y.; van Pomeren, T.; van Summeren, J.; Dückers, M.; Chaves, S.S.; Johnson, E.K.; Mahé, C.; et al. Global and national influenza-associated hospitalisation rates: Estimates for 40 countries and administrative regions. J. Glob. Health 2023, 13, 04003. [Google Scholar] [CrossRef] [PubMed]
- Fattore, G.; Pongiglione, B.; Vezzosi, L. Excess hospitalizations and in-hospital mortality associated with seasonal influenza in Italy: A 11-year retrospective study. BMC Infect. Dis. 2024, 24, 227. [Google Scholar] [CrossRef]
- Pumarola, T.; Díez-Domingo, J.; Martinón-Torres, F.; Redondo Margüello, E.; de Lejarazu Leonardo, R.O.; Carmo, M.; Bizouard, G.; Drago, G.; López-Belmonte, J.L.; Bricout, H.; et al. Excess hospitalizations and mortality associated with seasonal influenza in Spain, 2008–2018. BMC Infect. Dis. 2023, 23, 86. [Google Scholar] [CrossRef] [PubMed]
- Naquin, A.; O’Halloran, A.; Ujamaa, D.; Sundaresan, D.; Masalovich, S.; Cummings, C.N.; Noah, K.; Jain, S.; Kirley, P.D.; Alden, N.B.; et al. Laboratory-Confirmed Influenza-Associated Hospitalizations Among Children and Adults—Influenza Hospitalization Surveillance Network, United States, 2010–2023. MMWR Surveill. Summ. 2024, 73, 1–18. [Google Scholar] [CrossRef]
- Lin, F.; Chen, M.T.; Zhang, L.; Wu, M.; Xie, H.; Guan, Z.X.; Yang, Z.; Cai, Z.X.; Wen, J.Z.; Yang, L.Y. Resurgence of influenza A after SARS-CoV-2 omicron wave and comparative analysis of hospitalized children with COVID-19 and influenza A virus infection. Front. Med. 2024, 10, 1289487. [Google Scholar] [CrossRef]
- Bai, Y.; Tao, X. Comparison of COVID-19 and influenza characteristics. J. Zhejiang Univ. Sci. B 2021, 22, 87–98. [Google Scholar] [CrossRef]
- de Courville, C.; Bricout, H.; Alvarez, F.P.; Clouting, J.; Patel, S.; Mohamed, H.; Giblin, S.; Coles, B. Secondary healthcare resource utilization and related costs associated with influenza-related hospital admissions in adult patients, England 2016–2020. Expert Rev. Pharmacoecon. Outcomes Res. 2024, 25, 385–397. [Google Scholar] [CrossRef]
- Hu, T.; Miles, A.C.; Pond, T.; Boikos, C.; Maleki, F.; Alfred, T.; Lopez, S.M.C.; McGrath, L. Economic burden and secondary complications of influenza-related hospitalization among adults in the US: A retrospective cohort study. J. Med. Econ. 2024, 27, 324–336. [Google Scholar] [CrossRef]
- Sakamoto, H.; Ishikane, M.; Ueda, P. Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Japan. JAMA 2020, 323, 1969–1971. [Google Scholar] [CrossRef]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Lu, J.; Liu, Y.; Zhang, Z.; Luo, L. Positive effects of COVID-19 control measures on influenza prevention. Int. J. Infect. Dis. 2020, 95, 345–346. [Google Scholar] [CrossRef] [PubMed]
- Lagacé-Wiens, P.; Sevenhuysen, C.; Lee, L.; Nwosu, A.; Smith, T. Impact of nonpharmaceutical interventions on laboratory detections of influenza A and B in Canada. Can. Commun. Dis. Rep. 2021, 47, 142–148. [Google Scholar] [CrossRef]
- Su, Y.; Guo, Z.; Gu, X.; Sun, S.; Wang, K.; Xie, S.; Zhao, S. Influenza vaccine effectiveness against influenza A during the delayed 2022/23 epidemic in Shihezi, China. Vaccine 2023, 41, 5683–5686. [Google Scholar] [CrossRef]
- UK Health Security Agency. Surveillance of Influenza and Other Seasonal Respiratory Viruses in the UK, Winter 2022 to 2023. 2023. Available online: https://www.gov.uk/government/statistics/annual-flu-reports/surveillance-of-influenza-and-other-seasonal-respiratory-viruses-in-the-uk-winter-2022-to-2023 (accessed on 22 February 2025).
- Xu, D.; Chen, Z.; Zhu, G. Change of epidemiological characteristics of four respiratory viral infections in children before and during COVID-19 pandemic. Infect. Dis. Now 2024, 54, 104858. [Google Scholar] [CrossRef]
- Leung, C.; Konya, L.; Su, L. Postpandemic immunity debt of influenza in the USA and England: An interrupted time series study. Public Health 2024, 227, 239–242. [Google Scholar] [CrossRef]
- Jensen, A.; Stensballe, L.G. Impact of COVID-19 on testing, positive cases, patient characteristics, and hospital contacts for respiratory syncytial virus, influenza, and pneumococcus in Danish children. J. Infect. Public Health 2025, 18, 102660. [Google Scholar] [CrossRef]
- Cohen, P.R.; Rybak, A.; Werner, A.; Béchet, S.; Desandes, R.; Hassid, F.; André, J.M.; Gelbert, N.; Thiebault, G.; Kochert, F.; et al. Trends in pediatric ambulatory community acquired infections before and during COVID-19 pandemic: A prospective multicentric surveillance study in France. Lancet Reg. Health Eur. 2022, 22, 100497. [Google Scholar] [CrossRef]
- Huh, K.; Kim, Y.E.; Ji, W.; Kim, D.W.; Lee, E.J.; Kim, J.H.; Kang, J.M.; Jung, J. Decrease in hospital admissions for respiratory diseases during the COVID-19 pandemic: A nationwide claims study. Thorax 2021, 76, 939–941. [Google Scholar] [CrossRef]
- Taniguchi, Y.; Kuno, T.; Komiyama, J.; Adomi, M.; Suzuki, T.; Abe, T.; Ishimaru, M.; Miyawaki, A.; Saito, M.; Ohbe, H.; et al. Comparison of patient characteristics and in-hospital mortality between patients with COVID-19 in 2020 and those with influenza in 2017–2020: A multicenter, retrospective cohort study in Japan. Lancet Reg. Health West. Pac. 2022, 20, 100365. [Google Scholar] [CrossRef]
- McDonald, S.A.; Teirlinck, A.C.; Hooiveld, M.; van Asten, L.; Meijer, A.; de Lange, M.; van Gageldonk-Lafeber, A.B.; Wallinga, J. Inference of age-dependent case-fatality ratios for seasonal influenza virus subtypes a(H3N2) and a(H1N1)pdm09 and B lineages using data from the Netherlands. Influenza Other Respir. Viruses 2023, 17, e13146. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.; Kelly, H.; Cheung, C.-M.M.; Shiu, E.Y.; Wu, P.; Ni, M.Y.; Ip, D.K.; Cowling, B.J. Hospitalization Fatality Risk of Influenza A(H1N1)pdm09: A Systematic Review and Meta-Analysis. Am. J. Epidemiol. 2015, 182, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Lemaitre, M.; Fouad, F.; Carrat, F.; Crépey, P.; Gaillat, J.; Gavazzi, G.; Launay, O.; Mosnier, A.; Levant, M.-C.; Uhart, M. Estimating the burden of influenza-related and associated hospitalizations and deaths in France: An eight-season data study, 2010–2018. Influenza Other Respir. Viruses 2022, 16, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Cohen, L.E.; Hansen, C.L.; Andrew, M.K.; McNeil, S.A.; Vanhems, P.; Kyncl, J.; Domingo, J.D.; Zhang, T.; Dbaibo, G.; Laguna-Torres, V.A.; et al. Predictors of Severity of Influenza-Related Hospitalizations: Results From the Global Influenza Hospital Surveillance Network (GIHSN). J. Infect. Dis. 2024, 229, 999–1009. [Google Scholar] [CrossRef]
- Ferdinands, J.M.; Thompson, M.G.; Blanton, L.; Spencer, S.; Grant, L.; Fry, A.M. Does influenza vaccination attenuate the severity of breakthrough infections? A narrative review and recommendations for further research. Vaccine 2021, 39, 3678–3695. [Google Scholar] [CrossRef]
- Regan, A.K.; Arriola, C.S.; Couto, P.; Duca, L.; Loayza, S.; Nogareda, F.; de Almeida, W.A.; Antman, J.; Araya, S.; Vigueras, M.A.A.; et al. Severity of influenza illness by seasonal influenza vaccination status among hospitalised patients in four South American countries, 2013–2019: A surveillance-based cohort study. Lancet Infect. Dis. 2023, 23, 222–232. [Google Scholar] [CrossRef]
- Bellino, S.; Piovesan, C.; Bella, A.; Bella, A.; Rizzo, C.; Pezzotti, P.; Ramigni, M. Determinants of vaccination uptake, and influenza vaccine effectiveness in preventing deaths and hospital admissions in the elderly population; Treviso, Italy, 2014/2015–2016/2017 seasons. Hum. Vaccines Immunother. 2020, 16, 301–312. [Google Scholar] [CrossRef]
- Fabiani, M.; Volpe, E.; Faraone, M.; Bella, A.; Pezzotti, P.; Chini, F. Effectiveness of influenza vaccine in reducing influenza-associated hospitalizations and deaths among the elderly population; Lazio region, Italy, season 2016–2017. Expert Rev. Vaccines 2020, 19, 479–489. [Google Scholar] [CrossRef]
- Kalligeros, M.; Shehadeh, F.; Mylona, E.K.; Dapaah-Afriyie, C.; van Aalst, R.; Chit, A.; Mylonakis, E. Influenza vaccine effectiveness against influenza-associated hospitalization in children: A systematic review and meta-analysis. Vaccine 2020, 38, 2893–2903. [Google Scholar] [CrossRef]
- Lee, J.K.H.; Lam, G.K.L.; Yin, J.K.; Loiacono, M.M.; Samson, S.I. High-dose influenza vaccine in older adults by age and seasonal characteristics: Systematic review and meta-analysis update. Vaccine X 2023, 14, 100327. [Google Scholar] [CrossRef]
- Lee, J.K.H.; Lam, G.K.L.; Shin, T.; Samson, S.I.; Greenberg, D.P.; Chit, A. Efficacy and effectiveness of high-dose influenza vaccine in older adults by circulating strain and antigenic match: An updated systematic review and meta-analysis. Vaccine 2021, 39 (Suppl. S1), A24–A35. [Google Scholar] [CrossRef]

| Gender/Age Groups | Pre-Pandemic Period | COVID-19 Pandemic Period | ||
|---|---|---|---|---|
| 1 January 2016–3 March 2020 | 4 March 2020–31 December 2022 | |||
| N | % | N | % | |
| Men | 13,484 | 100% | 7922 | 100% |
| 0–4 * | 4890 | 36.3% | 3588 | 45.3% |
| 5–19 * | 4311 | 32.0% | 2874 | 36.3% |
| 20–64 * | 2225 | 16.5% | 774 | 9.8% |
| ≥65 * | 2058 | 15.3% | 685 | 8.6% |
| Average age (SD) * | 22.8 (28.0) | 14.9 (22.9) | ||
| Women | 11,639 | 100.0% | 6558 | 100.0% |
| 0–4 * | 4117 | 35.4% | 2922 | 44.6% |
| 5–19 * | 3314 | 28.5% | 2221 | 33.9% |
| 20–64 * | 1982 | 17.0% | 662 | 10.1% |
| ≥65 * | 2226 | 19.1% | 753 | 11.5% |
| Average age (SD) * | 26.0 (30.3) | 17.1 (25.5) | ||
| Total | 25,123 | 100.0% | 14,480 | 100.0% |
| 0–4 * | 9007 | 35.9% | 6511 | 45.0% |
| 5–19 * | 7625 | 30.4% | 5095 | 35.2% |
| 20–64 * | 4207 | 16.7% | 1436 | 9.9% |
| ≥65 * | 4284 | 17.1% | 1438 | 9.9% |
| Average age (SD) * | 24.3 (29.2) | 15.9 (24.2) | ||
| 0–4 years | 5–19 years | 20–64 years | ≥65 years | Total | ||
|---|---|---|---|---|---|---|
| 2016 | N | 1293 | 1320 | 1062 | 554 | 4229 |
| rate | 68.7 | 22.7 | 4.3 | 9.0 | 11.0 | |
| 2017 | N | 991 | 701 | 523 | 822 | 3037 |
| rate | 52.5 | 12.1 | 2.1 | 12.8 | 7.9 | |
| 2018 | N | 1666 | 1654 | 1052 | 1314 | 5686 |
| rate | 87.4 | 28.6 | 4.4 | 19.9 | 14.8 | |
| 2019 | N | 2611 | 1775 | 1094 | 1103 | 6583 |
| rate | 136.4 | 30.8 | 4.6 | 16.1 | 17.1 | |
| 2020 | N | 3218 | 2804 | 1085 | 1006 | 8113 |
| rate | 168.3 | 48.6 | 4.6 | 14.3 | 21.1 | |
| 2021 | N | 297 | 64 | 55 | 70 | 486 |
| rate | 15.8 | 1.1 | 0.2 | 1.0 | 1.3 | |
| 2022 | N | 5441 | 4401 | 771 | 857 | 11,470 |
| rate | 301.0 | 75.1 | 3.4 | 11.8 | 30.3 | |
| Age Group | 0–4 years | 5–19 years | 20–64 years | ≥65 years | Total | |
|---|---|---|---|---|---|---|
| 2016 | N | 4 | 3 | 75 | 84 | 166 |
| % | 2.4% | 1.8% | 45.2% | 50.6% | 100.0% | |
| CFR | 0.31 | 0.23 | 7.06 | 15.16 | 3.9 | |
| 2017 | N | 0 | 0 | 19 | 83 | 102 |
| % | 0.0% | 0.0% | 18.6% | 81.4% | 100.0% | |
| CFR | 0.00 | 0.00 | 3.63 | 10.10 | 3.4 | |
| 2018 | N | 1 | 2 | 56 | 119 | 178 |
| % | 0.6% | 1.1% | 31.5% | 66.9% | 100.0% | |
| CFR | 0.06 | 0.12 | 5.32 | 9.06 | 3.1 | |
| 2019 | N | 4 | 4 | 113 | 176 | 297 |
| % | 1.3% | 1.3% | 38.0% | 59.3% | 100.0% | |
| CFR | 0.15 | 0.23 | 10.33 | 15.96 | 4.5 | |
| 2020 | N | 3 | 6 | 45 | 161 | 215 |
| % | 1.4% | 2.8% | 20.9% | 74.9% | 100.0% | |
| CFR | 0.09 | 0.21 | 4.15 | 16.0 | 2.7 | |
| 2021 | N | 0 | 0 | 3 | 11 | 14 |
| % | 0.0% | 0.0% | 21.4% | 78.6% | 100.0% | |
| CFR | 0.00 | 0.00 | 5.45 | 15.71 | 2.9 | |
| 2022 | N | 0 | 2 | 33 | 139 | 174 |
| % | 0.0% | 1.1% | 19.0% | 79.9% | 0.0% | |
| CFR | 0.00 | 0.05 | 4.28 | 16.22 | 1.5 | |
| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | |
|---|---|---|---|---|---|---|---|
| All influenza cases | 4,316,823 | 5,043,491 | 5,239,293 | 4,790,033 | 3,160,711 | 2,973,793 | 4,703,128 |
| Incidence per 100,000 population | 11,233.9 | 13,126.5 | 13,639.3 | 12,478.4 | 8240.9 | 7792.5 | 12,433.1 |
| Number of people vaccinated against influenza | 857,029 | 945,869 | 1,009,285 | 1,013,706 | 1,046,633 | 1,293,653 | 1,107,351 |
| Percentage of people vaccinated against influenza | 2.2% | 2.5% | 2.6% | 2.6% | 2.7% | 3.4% | 2.9% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanecki, K.; Lewtak, K.; Tyszko, P.; Goryński, P.; Rząd, M.; Okręglicka, K.; Nitsch-Osuch, A. Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods. J. Clin. Med. 2025, 14, 1785. https://doi.org/10.3390/jcm14061785
Kanecki K, Lewtak K, Tyszko P, Goryński P, Rząd M, Okręglicka K, Nitsch-Osuch A. Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods. Journal of Clinical Medicine. 2025; 14(6):1785. https://doi.org/10.3390/jcm14061785
Chicago/Turabian StyleKanecki, Krzysztof, Katarzyna Lewtak, Piotr Tyszko, Paweł Goryński, Michał Rząd, Katarzyna Okręglicka, and Aneta Nitsch-Osuch. 2025. "Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods" Journal of Clinical Medicine 14, no. 6: 1785. https://doi.org/10.3390/jcm14061785
APA StyleKanecki, K., Lewtak, K., Tyszko, P., Goryński, P., Rząd, M., Okręglicka, K., & Nitsch-Osuch, A. (2025). Hospitalizations and In-Hospital Fatality Among Influenza Patients in the Pre-Pandemic and COVID-19 Pandemic Periods. Journal of Clinical Medicine, 14(6), 1785. https://doi.org/10.3390/jcm14061785





