Postoperative Outcomes of One-Step Implant-Based Breast and Ovarian Surgery in High-Penetrance Gene Mutation: A Single-Center Experience
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Inclusion and Exclusion Criteria
2.2. Data Collection and Statistical Analysis
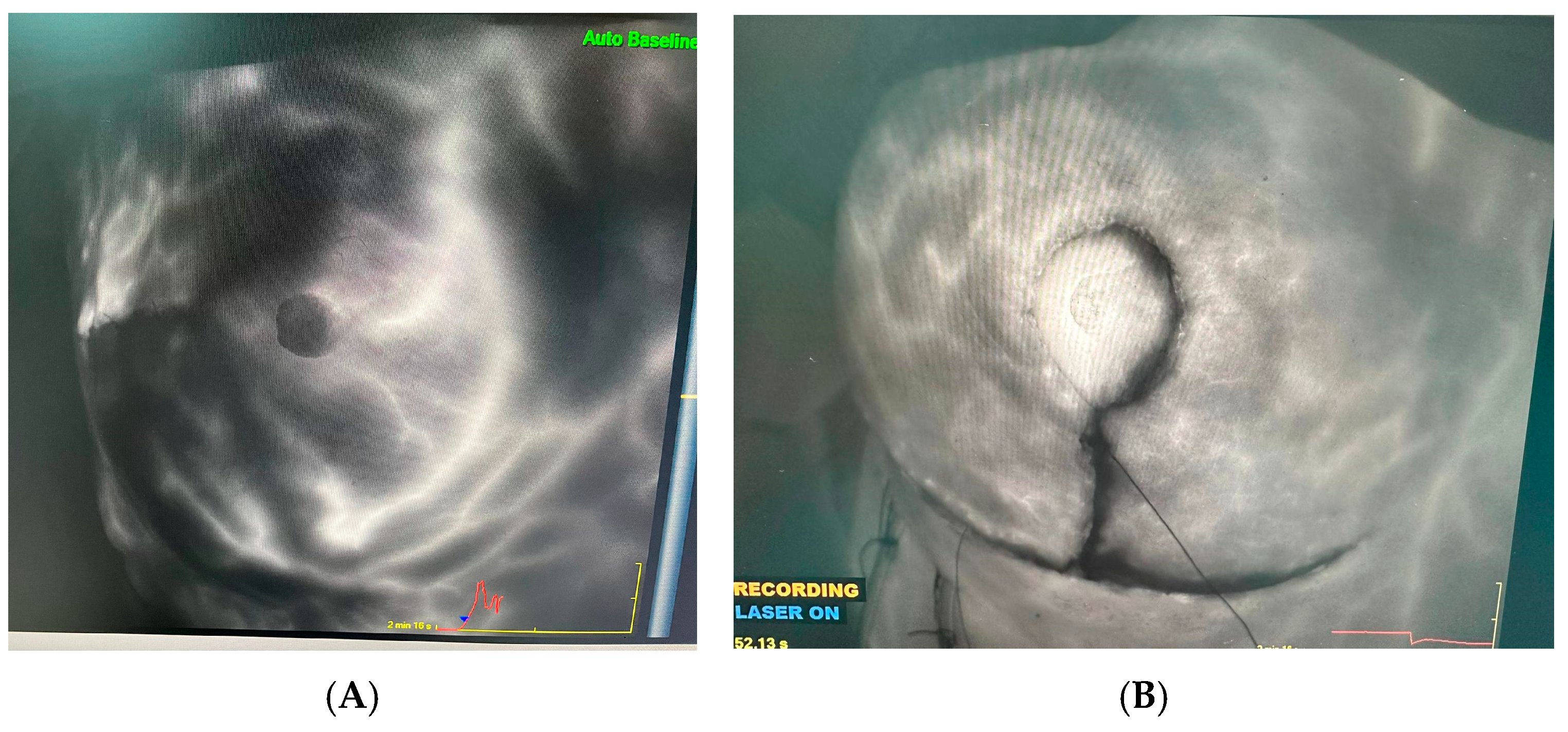
2.3. Surgical Technique
3. Results
3.1. General Features
3.2. Surgical Technique
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| RT | Radiotherapy |
| CT | Chemotherapy |
| RRSO | Risk-reducing salpingo-oophorectomy |
| RRBM | Risk-reducing bilateral mastectomy |
| NCCN | National Comprehensive Cancer Network |
| NACT | Neoadjuvant chemotherapy |
| SSMI | Skin-sparing mastectomy with implant reconstruction |
| TLH | Total laparoscopic hysterectomy |
| BSO | Bilateral salpingo-oophorectomy |
| BMI | Body mass index |
| ER | Estrogen receptor |
| PR | Progesteron receptor |
References
- Breast Cancer Association Consortium. Breast Cancer Risk Genes—Association Analysis in More than 113,000 Women. N. Engl. J. Med. 2021, 384, 428–436. [Google Scholar] [CrossRef] [PubMed]
- Düzkale, N.; Gökçe, A.; Eren, T.; İmamoğlu, G.İ.; Altinbaş, M. Investigation of genotype-phenotype relationship in women with BRCA1/2 normal breast cancer: A single-center experience from Turkey. Turk. J. Clin. Lab. 2021, 3, 346–355. [Google Scholar]
- Valencia, O.M.; Samuel, S.E.; Viscusi, R.K.; Riall, T.S.; Neumayer, L.A.; Aziz, H. The Role of Genetic Testing in Patients With Breast Cancer: A Review. JAMA Surg. 2017, 152, 589–594. [Google Scholar] [CrossRef]
- Saccardi, C.; Spagnol, G.; Saibene, T.; De Lorenzo, L.S.; Marchetti, M.; Bonaldo, G.; Michieletto, S.; Toffanin, M.C.; Noventa, M.; Tozzi, R. Risk-Reducing Salpingo-Oophorectomy (RRSO) Combined with Simultaneous Mastectomy in Women with BRCA 1-2 Mutation Carriers: The Surgical Technique, the Feasibility and Patients’ Satisfaction of Multiple Surgeries. J. Clin. Med. 2022, 11, 7502. [Google Scholar] [CrossRef]
- Daly, M.B.; Pal, T.; Berry, M.P.; Buys, S.S.; Dickson, P.; Domchek, S.M.; Elkhanany, A.; Friedman, S.; Goggins, M.; Hutton, M.L.; et al. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2021, 19, 77–102. [Google Scholar] [CrossRef]
- Patel, M.M.; Adrada, B.E. Hereditary Breast Cancer: BRCA Mutations and Beyond. Radiol. Clin. N. Am. 2024, 62, 627–642. [Google Scholar] [CrossRef] [PubMed]
- Comeaux, J.G.; Culver, J.O.; Lee, J.E.; Dondanville, D.; McArthur, H.L.; Quinn, E.; Gorman, N.; Ricker, C.; Li, M.; Lerman, C. Risk-reducing mastectomy decisions among women with mutations in high- and moderate- penetrance breast cancer susceptibility genes. Mol. Genet. Genom. Med. 2022, 10, e2031. [Google Scholar] [CrossRef]
- Decker, M.R.; Greenblatt, D.Y.; Havlena, J.; Wilke, L.G.; Greenberg, C.C.; Neuman, H.B. Impact of neoadjuvant chemotherapy on wound complications after breast surgery. Surgery 2012, 152, 382–388. [Google Scholar] [CrossRef]
- Lorentzen, T.; Heidemann, L.N.; Möller, S.; Bille, C. Impact of neoadjuvant chemotherapy on surgical complications in breast cancer: A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2022, 48, 44–52. [Google Scholar] [CrossRef]
- Huang, N.; Liu, L.; Qin, Y.; Xie, Y. Effect of radiation therapy during surgery on postoperative wound complications after breast reconstruction in patients with breast cancer: A meta-analysis. Int. Wound J. 2023, 21, e14473. [Google Scholar] [CrossRef]
- Fasola, C.E.; Sharp, H.J.; Clavin, N.W.; Sha, W.; Schepel, C.R.; Trufan, S.J.; Graham, E.; Hecksher, A.; White, R.L., Jr.; Hadzikadic-Gusic, L. Effect of Delayed Oncoplastic Reduction Mammoplasty on Radiation Treatment Delay Following Breast-Conserving Surgery for Breast Cancer. Ann. Surg. Oncol. 2023, 30, 8362–8370. [Google Scholar] [CrossRef] [PubMed]
- Bogdan, R.G.; Helgiu, A.; Cimpean, A.M.; Ichim, C.; Todor, S.B.; Iliescu-Glaja, M.; Bodea, I.C.; Crainiceanu, Z.P. Assessing Fat Grafting in Breast Surgery: A Narrative Review of Evaluation Techniques. J. Clin. Med. 2024, 13, 7209. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, R.; Andersson, M.N.; Svensson, J.; Rosén, A.; Koch, F.; Björkgren, A.; Sund, M. Prophylactic Mastectomy: Postoperative Skin Flap Thickness Evaluated by MRT, Ultrasound and Clinical Examination. Ann. Surg. Oncol. 2020, 27, 2221–2228. [Google Scholar] [CrossRef] [PubMed]
- Ma, I.T.; Gray, R.J.; Wasif, N.; Butler, K.A.; Cornella, J.L.; Magrina, J.F.; Magtibay, P.M.; Casey, W.J.; Mahabir, R.; Rebecca, A.M.; et al. Outcomes of Concurrent Breast and Gynecologic Risk Reduction Surgery. Ann. Surg. Oncol. 2017, 24, 77–83. [Google Scholar] [CrossRef]
- Batista, L.I.; Lu, K.H.; Beahm, E.K.; Arun, B.K.; Bodurka, D.C.; Meric-Bernstam, F. Coordinated prophylactic surgical management for women with hereditary breast-ovarian cancer syndrome. BMC Cancer 2008, 8, 101. [Google Scholar] [CrossRef]
- Casey, W.J., 3rd; Rebecca, A.M.; Andres, L.A.; Craft, R.O.; Smith, A.A.; Pockaj, B.A.; Kho, R.M.; Magtibay, P.M. Safety and efficacy of perforator flap breast reconstruction with combined intraabdominal procedures. Ann. Plast. Surg. 2010, 64, 144–150. [Google Scholar] [CrossRef]
- Warren Peled, A.; Itakura, K.; Foster, R.D.; Hamolsky, D.; Tanaka, J.; Ewing, C.; Alvarado, M.; Esserman, L.J.; Hwang, E.S. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch. Surg. 2010, 145, 880–885. [Google Scholar] [CrossRef]
- Singer, R.; Krant, S.M. Intravenous fluorescein for evaluating the dusky nipple-areola during reduction mammaplasty. Plast. Reconstr. Surg. 1981, 67, 534–535. [Google Scholar] [CrossRef]
- Ooi, A.; Song, D.H. Reducing infection risk in implant-based breast-reconstruction surgery: Challenges and solutions. Breast Cancer: Targets Ther. 2016, 8, 161–172. [Google Scholar] [CrossRef]
- Azouz, V.; Mirhaidari, S.; Wagner, D.S. Defining Infection in Breast Reconstruction: A Literature Review. Ann. Plast. Surg. 2018, 80, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Gardani, M.; Cocconi, A.; Palli, D. Skin-reducing mastectomy and pre-pectoral breast reconstruction using the Braxon® ADM: A single-center experience. Minerva Surg. 2022, 77, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Payne, S.H.; Ballesteros, S.; Brown, O.H.; Razavi, S.A.; Carlson, G.W. Skin Reducing Mastectomy and Immediate Tissue Expander Reconstruction: A Critical Analysis. Ann. Plast. Surg. 2022, 88, 485–489. [Google Scholar] [CrossRef] [PubMed]
| BRCA1 (n: 24) | BRCA2 (n: 28) | Other High Penetrant Gene Group (n: 9) | |||
|---|---|---|---|---|---|
| Age | 42.28 ± 7.82 (30–58) | ||||
| BMI | 25.08 ± 4.19 (17.3–39.1) | ||||
| Surgery Duration, min | 150.33 ± 53.75 (60–300) | ||||
| Relative Comorbidity | No | 21 | 21 | 9 | |
| (87.5%) | (75%) | (100%) | |||
| Yes | 2 | 4 | 0 | ||
| (8.33%) | (14.28%) | (0%) | |||
| Hormone Receptor Expression; (n: %) | ER (+) | 6 | 15 | 5 | |
| (25%) | (53.57%) | (55.5%) | |||
| PR (+) | 6 | 13 | 3 | ||
| (25%) | (46.42%) | (33.33%) | |||
| HER2 (n: %) | HER2 (+) | 2 | 3 | 2 | |
| (8.33%) | (10.71%) | (22.22%) | |||
| HER2 (−) | 21 | 22 | 7 | ||
| (87.5%) | (78.57%) | (77.77%) | |||
| Previously RT (n: %) | No | 20 | 16 | 7 | |
| (83.33%) | (57.14%) | (77.77%) | |||
| Yes | 3 | 9 | 2 | ||
| (12.5%) | (32.14%) | (22.22%) | |||
| Neoadjuvant CT (n: %) | No | 10 | 19 | 4 | |
| (41.66%) | (67.85%) | (44.44%) | |||
| Yes | 13 | 6 | 5 | ||
| (54.16%) | (21.42%) | (55.55%) | |||
| Clinical Stage; (n: %) | T | T1 | 9 (37.5%) | 9 (32.14%) | 3 (33.33%) |
| T2 | 8 (33.33%) | 9 (32.14%) | 4 (44.44%) | ||
| T3 | 1 (4.16%) | 0 (0%) | 0 (0%) | ||
| N | N0 | 7 (29.16%) | 8 (28.57%) | 5 (55.55%) | |
| N1 | 1 (4.16%) | 2 (7.14%) | 1 (11.11%) | ||
| N2 | 8 (33.33%) | 8 (28.57%) | 1 (11.11%) | ||
| N3 | 2 (8.33%) | 0 (0%) | 0 (0%) | ||
| Pathologycal Stage; (n: %) | T | T0 | 9 (37.5%) | 3 (10.71%) | 2 (22.22%) |
| T1 | 7 (29.16%) | 8 (28.57%) | 3 (33.33%) | ||
| T2 | 2 (8.33%) | 6 (21.42%) | 2 (22.22%) | ||
| T3 | 1 (4.16%) | 0 (0%) | 0 (0%) | ||
| N | N0 | 7 (29.16%) | 9 (32.14%) | 5 (55.55%) | |
| N1 | 1 (4.16%) | 2 (7.14%) | 1 (11.11%) | ||
| N2 | 8 (33.33%) | 8 (28.57%) | 1 (11.11%) | ||
| N3 | 2 (8.33%) | 0 (0%) | 0 (0%) | ||
| Skin-Reducing Mastectomy; (n: %) | 4 | 4 | 1 | ||
| (16.66%) | (14.28%) | (11.11%) | |||
| Groups (n, %) | p Value | |||
|---|---|---|---|---|
| Previousl RT (16, 26.2%) | Neoadjuvant CT (26, 42.6%) | Not Receiving Any Neoadjuvant Treatment (19, 31.2%) | ||
| Age, Years, Mean ± SD | 44 ± 7.51 | 39.42 ± 8.14 | 44.74 ± 6.62 | 0.044 F |
| BMI, Median, Distribution | 24.25 (20.8–38.8) | 23.9 (19.2–39.1) | 25 (17.3–32) | 0.711 H |
| Gene Profile, n (%) | 0.098 X2 | |||
| BRCA1 | 3 (12.5%) | 14 (58.3%) | 7 (29.2%) | |
| BRCA2 | 11 (39.3%) | 7 (25%) | 10 (35.7%) | |
| Other High Penetrant | 2 (22.2%) | 5 (55.6%) | 2 (22.2%) | |
| Nipple Ssparing Mastectomy, n (%) | 0.846 X2 | |||
| No | 2 (20%) | 5 (50%) | 3 (30%) | |
| Yes | 14 (27.5%) | 21 (41.2%) | 16 (31.3%) | |
| Skin Reducing Mastectomy, n (%) | 0.270 X2 | |||
| No | 15 (28.8%) | 20 (38.5%) | 17 (32.7%) | |
| Yes | 1 (11.1%) | 6 (66.7%) | 2 (22.2%) | |
| Comorbidities *, n (%) | 0.569 X2 | |||
| No | 14 (25.9%) | 22 (40.8%) | 18 (33.3%) | |
| Yes | 2 (28.6%) | 4 (57.1%) | 1 (14.3%) | |
| Skin-Sparing Mastectomy With Implant Reconstruction Surgery Time, min, median, Distribution | 160 (90–240) | 125 (60–180) | 180 (80–300) | 0.089 H |
| Total (n: =61) | |
|---|---|
| Mean Operative Time SSMI + TLH + BSO | 240 ± 52.37 (120–360) |
| Mean Operative Time SSMI | 150.33 ± 53.75 (60–300) |
| Mean Operative Time TLH + BSO | 75.55 ± 31.96 (30–150) |
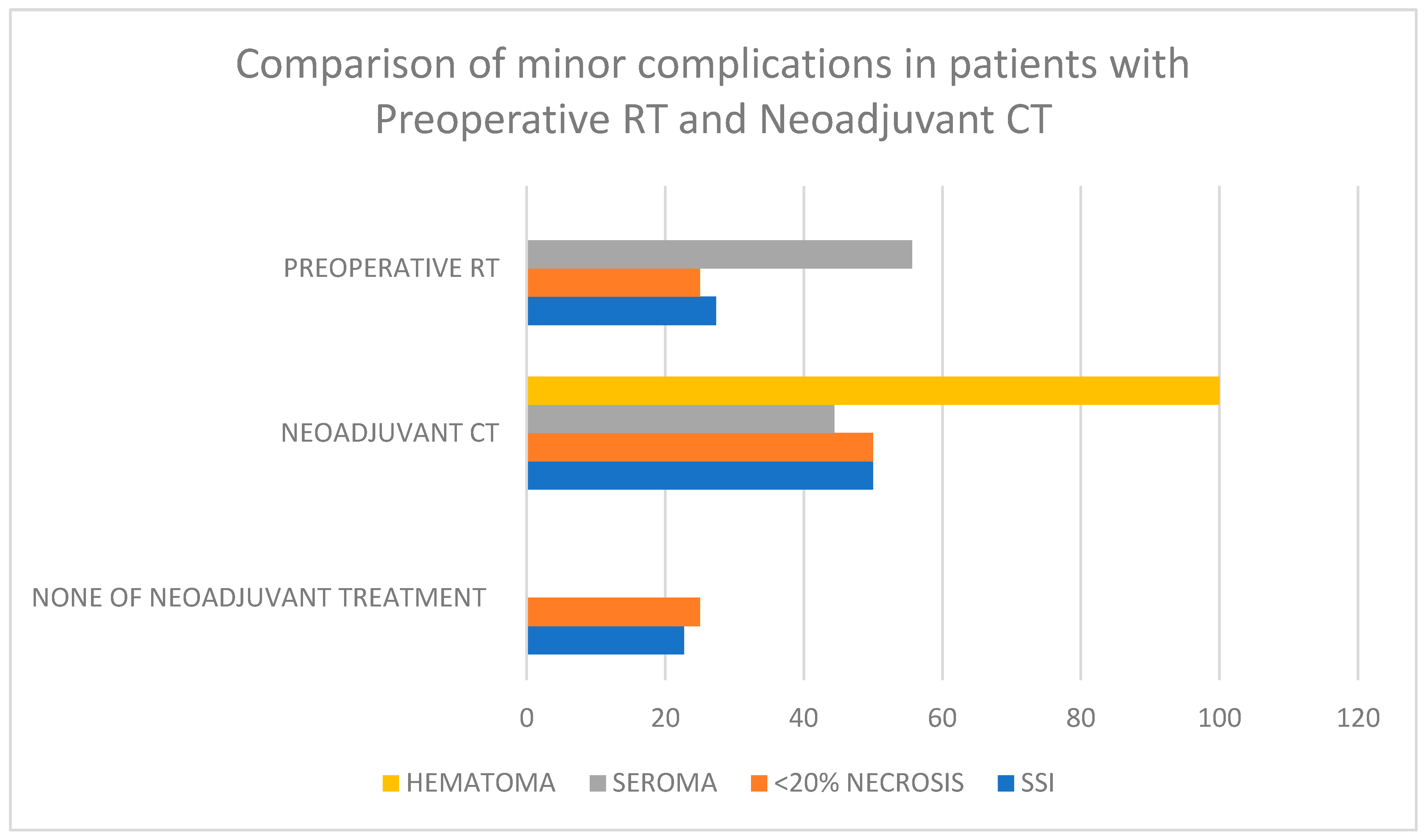
| Preoperative RT (16, 26.2%) | Neoadjuvant CT (26, 42.6%) | None of Neoadjuvant Treatment (19, 31.2%) | p | ||
|---|---|---|---|---|---|
| Major Complications; n (%) | Active Bleeding | 0.504 X2 | |||
| No | 16 (26.7%) | 25 (41.7%) | 19 (31.6%) | ||
| Yes | 0 (0%) | 1 (100%) | 0 (0%) | ||
| Wound Dehiscence | 0.273 X2 | ||||
| No | 12 (25.5%) | 18 (38.3%) | 17 (36.2%) | ||
| Yes | 4 (28.6%) | 8 (57.1%) | 2 (14.3%) | ||
| Minor Complicaitons; n (%) | SSI | 0.539 X2 | |||
| No | 10 (25.6%) | 15 (38.5%) | 14 (35.9%) | ||
| Yes | 6 (27.3%) | 11 (50%) | 5 (22.7%) | ||
| <20% Skin Necrosis | 0.759 X2 | ||||
| No | 12 (26.7%) | 18 (40%) | 15 (33.3%) | ||
| Yes | 4 (25%) | 8 (50%) | 4 (25%) | ||
| Seroma | 0.034 X2 | ||||
| No | 11 (21.2%) | 22 (42.3%) | 19 (36.5%) | ||
| Yes | 5 (55.6%) | 4 (44.4%) | 0 (0%) | ||
| Hematoma | 0.249 X2 | ||||
| No | 16 (27.1%) | 24 (40.7%) | 19 (32.2%) | ||
| Yes | 0 (0%) | 2 (100%) | 0 (0%) | ||
| Reoperation; n (%) | No | 12 (25%) | 19 (39.6%) | 17 (35.4%) | 0.380 X2 |
| Yes | 4 (30.8%) | 7 (53.8%) | 2 (15.4%) | ||
| Skin Reducing Mammoplasty | p | |||
|---|---|---|---|---|
| Yes (n: 9) | No (n: 52) | |||
| Major Complications; n (%) | Active Bleeding | 0 (0%) | 1 (1.92%) | 0.675 |
| Wound Dehiscence | 3 (33.33%) | 11 (21.15%) | 0.412 | |
| Minor Complications; n (%) | SSI | 4 (44.44%) | 18 (34.61%) | 0.571 |
| <20% Skin Necrosis | 3 (33.33%) | 13 (25%) | 0.6 | |
| Seroma | 1 (11.11%) | 8 (15.38%) | 0.339 | |
| Hematoma | 0 (0%) | 2 (3.84%) | 0.55 | |
| Reoperation; n (%) | Due to Wound Dehiscence or Other Complications | 1 (11.11%) | 10 (19.23%) | 0.682 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koc, B.I.; Morkavuk, S.B.; Akyuz, S.; Aygun, G.; Ozdemir, O.; Gulcelik, M.A. Postoperative Outcomes of One-Step Implant-Based Breast and Ovarian Surgery in High-Penetrance Gene Mutation: A Single-Center Experience. J. Clin. Med. 2025, 14, 1784. https://doi.org/10.3390/jcm14061784
Koc BI, Morkavuk SB, Akyuz S, Aygun G, Ozdemir O, Gulcelik MA. Postoperative Outcomes of One-Step Implant-Based Breast and Ovarian Surgery in High-Penetrance Gene Mutation: A Single-Center Experience. Journal of Clinical Medicine. 2025; 14(6):1784. https://doi.org/10.3390/jcm14061784
Chicago/Turabian StyleKoc, Buse Irem, Sevket Barıs Morkavuk, Simay Akyuz, Guzin Aygun, Ozhan Ozdemir, and Mehmet Ali Gulcelik. 2025. "Postoperative Outcomes of One-Step Implant-Based Breast and Ovarian Surgery in High-Penetrance Gene Mutation: A Single-Center Experience" Journal of Clinical Medicine 14, no. 6: 1784. https://doi.org/10.3390/jcm14061784
APA StyleKoc, B. I., Morkavuk, S. B., Akyuz, S., Aygun, G., Ozdemir, O., & Gulcelik, M. A. (2025). Postoperative Outcomes of One-Step Implant-Based Breast and Ovarian Surgery in High-Penetrance Gene Mutation: A Single-Center Experience. Journal of Clinical Medicine, 14(6), 1784. https://doi.org/10.3390/jcm14061784







