Axial Length Stabilization or Reduction in over 40% of Patients Wearing Extended Depth-of-Focus Contact Lenses
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Study Populations
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Changes in the AL, SE, and CT After Wearing EDOF CLs
3.3. Patient Factors Involved in AL Shortening After Wearing EDOF CLs
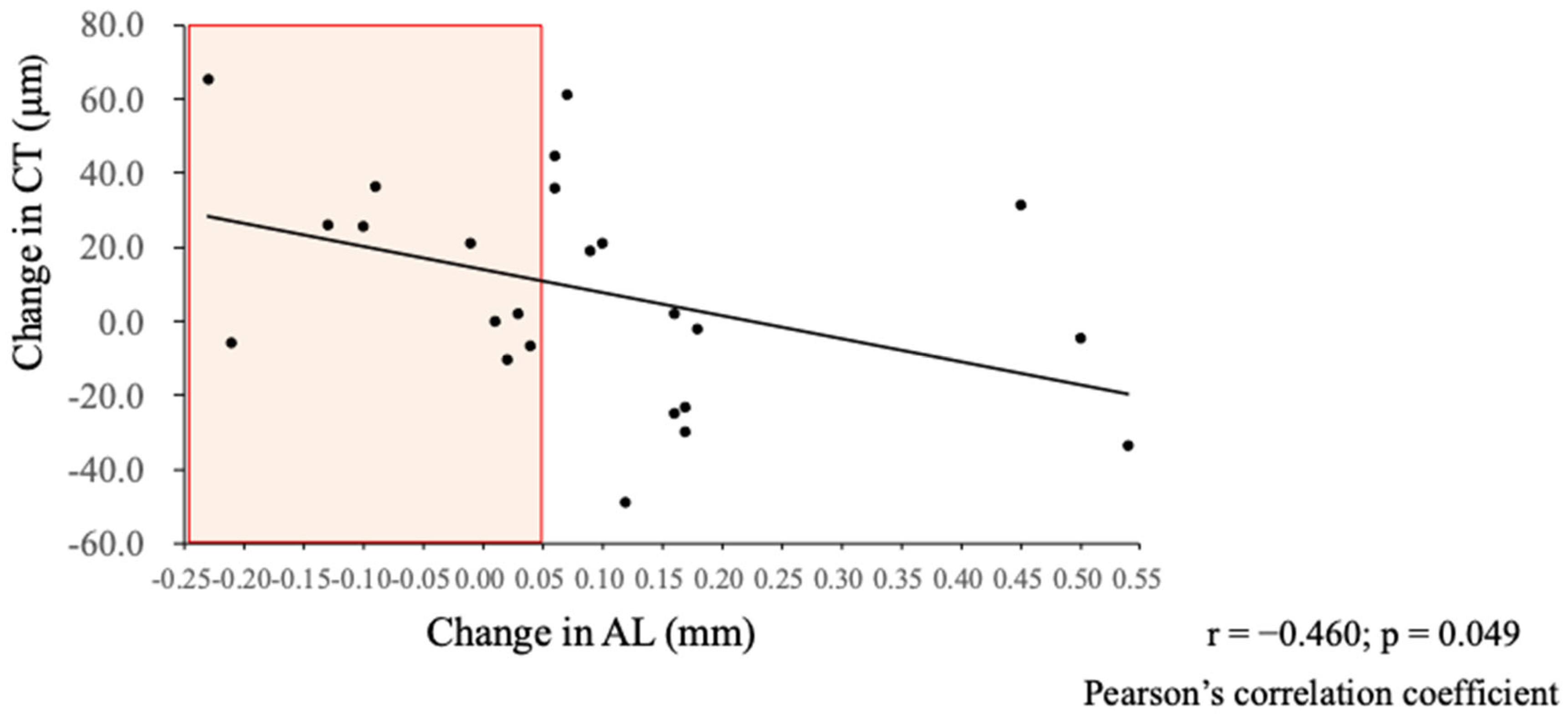
3.4. Associations Between Changes in AL and Changes in CT After Wearing EDOF CLs
3.5. Investigation of Factors Associated with the Changes in AL
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Axial length | AL |
| Spherical equivalent | SE |
| Choroidal thickness | CT |
| Orthokeratology | OK |
| Contact lenses | CL |
| Multifocal contact lenses | MFCL |
| Extended depth-of-focus | EDOF |
| Low-level red light | LLRL |
| Optical coherence tomography | OCT |
| Violet light | VL |
References
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Xiang, Z.Y.; Zou, H.D. Recent Epidemiology Study Data of Myopia. J. Ophthalmol. 2020, 4395278. [Google Scholar] [CrossRef] [PubMed]
- Yotsukura, E.; Torii, H.; Inokuchi, M.; Tokumura, M.; Uchino, M.; Nakamura, K.; Hyodo, M.; Mori, K.; Jiang, X.; Ikeda, S.I.; et al. Current Prevalence of Myopia and Association of Myopia with Environmental Factors among Schoolchildren in Japan. JAMA Ophthalmol. 2019, 137, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Yotsukura, E.; Torii, H.; Mori, K.; Ogawa, M.; Hanyuda, A.; Negishi, K.; Kurihara, T.; Tsubota, K. Slowing of Greater Axial Length Elongation Stemming from the Coronavirus Disease 2019 Pandemic with Increasing Time Outdoors: The Tokyo Myopia Study. Ophthalmol. Sci. 2024, 4, 100491. [Google Scholar] [CrossRef]
- Wong, T.Y.; Ferreira, A.; Hughes, R.; Carter, G.; Mitchell, P. Epidemiology and Disease Burden of Pathologic Myopia and Myopic Choroidal Neovascularization: An Evidence-Based Systematic Review. Am. J. Ophthalmol. 2014, 157, 9–25.e12. [Google Scholar] [CrossRef]
- Łazarczyk, J.B.; Urban, B.; Konarzewska, B.; Szulc, A.; Bakunowicz-Łazarczyk, A.; Żmudzka, E.; Kowzan, U.; Waszkiewicz, N.; Juszczyk-Zajkowska, K. The Differences in Level of Trait Anxiety among Girls and Boys Aged 13–17 Years with Myopia and Emmetropia. BMC Ophthalmol. 2016, 16, 201. [Google Scholar] [CrossRef]
- Jones, L.A.; Sinnott, L.T.; Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Zadnik, K. Parental History of Myopia, Sports and Outdoor Activities, and Future Myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3524–3532. [Google Scholar] [CrossRef]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Children’s Refractive Error. Investig. Ophthalmol. Vis. Sci. 2002, 43, 3633–3640. [Google Scholar]
- Deng, L.; Pang, Y. Effect of Outdoor Activities in Myopia Control: Meta-Analysis of Clinical Studies. Optom. Vis. Sci. 2019, 96, 276–282. [Google Scholar] [CrossRef]
- Sherwin, J.C.; Reacher, M.H.; Keogh, R.H.; Khawaja, A.P.; MacKey, D.A.; Foster, P.J. The Association between Time Spent Outdoors and Myopia in Children and Adolescents: A Systematic Review and Meta-Analysis. Ophthalmology 2012, 119, 2141–2151. [Google Scholar] [CrossRef]
- Sánchez-Tena, M.Á.; Ballesteros-Sánchez, A.; Martinez-Perez, C.; Alvarez-Peregrina, C.; De-Hita-Cantalejo, C.; Sánchez-González, M.C.; Sánchez-González, J.M. Assessing the Rebound Phenomenon in Different Myopia Control Treatments: A Systematic Review. Ophthalmic Physiol. Opt. 2024, 44, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Sankaridurg, P. Contact Lenses to Slow Progression of Myopia. Clin. Exp. Optom. 2017, 100, 432–437. [Google Scholar] [CrossRef]
- Yam, J.C.; Zhang, X.J.; Zhang, Y.; Yip, B.H.K.; Tang, F.; Wong, E.S.; Bui, C.H.T.; Kam, K.W.; Ng, M.P.H.; Ko, S.T.; et al. Effect of Low-Concentration Atropine Eyedrops vs Placebo on Myopia Incidence in Children: The LAMP2 Randomized Clinical Trial. JAMA 2023, 329, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Yam, J.C.; Jiang, Y.; Lee, J.; Li, S.; Zhang, Y.; Sun, W.; Yuan, N.; Wang, Y.M.; Yip, B.H.K.; Kam, K.W.; et al. The Association of Choroidal Thickening by Atropine with Treatment Effects for Myopia: Two-Year Clinical Trial of the Low-Concentration Atropine for Myopia Progression (LAMP) Study. Am. J. Ophthalmol. 2022, 237, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, M.; San, S.; Bian, L.; Li, H. Orthokeratology in Controlling Myopia of Children: A Meta-Analysis of Randomized Controlled Trials. BMC Ophthalmol. 2023, 23, 441. [Google Scholar] [CrossRef]
- Torii, H.; Mori, K.; Okano, T.; Kondo, S.; Yang, H.-Y.; Yotsukura, E.; Hanyuda, A.; Ogawa, M.; Negishi, K.; Kurihara, T.; et al. Short-Term Exposure to Violet Light Emitted from Eyeglass Frames in Myopic Children: A Randomized Pilot Clinical Trial. J. Clin. Med. 2022, 11, 6000. [Google Scholar] [CrossRef]
- Mori, K.; Torii, H.; Fujimoto, S.; Jiang, X.; Ikeda, S.-I.; Yotsukura, E.; Koh, S.; Kurihara, T.; Nishida, K.; Tsubota, K. The Effect of Dietary Supplementation of Crocetin for Myopia Control in Children: A Randomized Clinical Trial. J. Clin. Med. 2019, 8, 1179. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, Y.; Zhu, Z.; Zhang, S.; Xuan, M.; Tan, X.; Kong, X.; Zhong, H.; Bulloch, G.; Xiong, R.; et al. Axial Shortening in Myopic Children after Repeated Low-Level Red-Light Therapy: Post Hoc Analysis of a Randomized Trial. Ophthalmol. Ther. 2023, 12, 1223–1237. [Google Scholar] [CrossRef]
- Wang, W.; Jiang, Y.; Zhu, Z.; Zhang, S.; Xuan, M.; Chen, Y.; Xiong, R.; Bulloch, G.; Zeng, J.; Morgan, I.G.; et al. Clinically Significant Axial Shortening in Myopic Children After Repeated Low-Level Red Light Therapy: A Retrospective Multicenter Analysis. Ophthalmol. Ther. 2023, 12, 999–1011. [Google Scholar] [CrossRef]
- Liu, G.; Li, B.; Rong, H.; Du, B.; Wang, B.; Hu, J.; Zhang, B.; Wei, R. Axial Length Shortening and Choroid Thickening in Myopic Adults Treated with Repeated Low-Level Red Light. J. Clin. Med. 2022, 11, 7498. [Google Scholar] [CrossRef]
- Anstice, N.S.; Phillips, J.R. Effect of Dual-Focus Soft Contact Lens Wear on Axial Myopia Progression in Children. Ophthalmology 2011, 118, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Fujikado, T.; Ninomiya, S.; Kobayashi, T.; Suzaki, A.; Nakada, M.; Nishida, K. Effect of Low-Addition Soft Contact Lenses with Decentered Optical Design on Myopia Progression in Children: A Pilot Study. Clin. Ophthalmol. 2014, 8, 1947–1956. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.S.Y.; Tang, W.C.; Tse, D.Y.Y.; Tang, Y.Y.; To, C.H. Defocus Incorporated Soft Contact (DISC) Lens Slows Myopia Progression in Hong Kong Chinese Schoolchildren: A 2-Year Randomised Clinical Trial. Br. J. Ophthalmol. 2014, 98, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Aller, T.A.; Liu, M.; Wildsoet, C.F. Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial. Optom. Vis. Sci. 2016, 93, 344–352. [Google Scholar] [CrossRef]
- Chamberlain, P.; Peixoto-de-Matos, S.C.; Logan, N.S.; Ngo, C.; Jones, D.; Young, G. A 3-Year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom. Vis. Sci. 2019, 96, 556–567. [Google Scholar] [CrossRef]
- Li, S.-M.; Kang, M.-T.; Wu, S.-S.; Meng, B.; Sun, Y.-Y.; Wei, S.-F.; Liu, L.; Peng, X.; Chen, Z.; Zhang, F.; et al. Studies Using Concentric Ring Bifocal and Peripheral Add Multifocal Contact Lenses to Slow Myopia Progression in School-Aged Children: A Meta-Analysis. Ophthalmic Physiol. Opt. 2017, 37, 51–59. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Bakaraju, R.C.; Naduvilath, T.; Chen, X.; Weng, R.; Tilia, D.; Xu, P.; Li, W.; Conrad, F.; Smith, E.L.; et al. Myopia Control with Novel Central and Peripheral plus Contact Lenses and Extended Depth of Focus Contact Lenses: 2 Year Results from a Randomised Clinical Trial. Ophthalmic Physiol. Opt. 2019, 39, 294–307. [Google Scholar] [CrossRef]
- Shen, E.P.; Chu, H.-S.; Cheng, H.-C.; Tsai, T.-H. Center-for-Near Extended-Depth-of-Focus Soft Contact Lens for Myopia Control in Children: 1-Year Results of a Randomized Controlled Trial. Ophthalmol. Ther. 2022, 11, 1577–1588. [Google Scholar] [CrossRef]
- Manoharan, M.K.; Verkicharla, P.K. Randomised Clinical Trial of Extended Depth of Focus Lenses for Controlling Myopia Progression: Outcomes from SEED LVPEI Indian Myopia Study. Br. J. Ophthalmol. 2024, 108, 1292–1298. [Google Scholar] [CrossRef]
- Department of Ophthalmology, Keio University School of Medicine. Opt Out of the Retrospective Study. Available online: https://www.ctr.hosp.keio.ac.jp/patients/optout/index.html (accessed on 16 August 2021).
- He, M.; Xiang, F.; Zeng, Y.; Mai, J.; Chen, Q.; Zhang, J.; Smith, W.; Rose, K.; Morgan, I.G. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China A Randomized Clinical Trial. JAMA 2021, 314, 1142–1148. [Google Scholar] [CrossRef]
- Montés-Micó, R.; Pastor-Pascual, F.; Ruiz-Mesa, R.; Tañá-Rivero, P. Ocular Biometry with Swept-Source Optical Coherence Tomography. J. Cataract Refract. Surg. 2021, 47, 802–814. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Cui, L.; Kong, M.; Li, Q.; Feng, X.; Feng, K.; Zhu, H.; Cui, H.; Shi, C.; Zhang, J.; et al. Repeated Low-Level Red Light Therapy for Myopia Control in High Myopia Children and Adolescents: A Randomized Clinical Trial. Ophthalmology. 2024, 131, 1314–1323. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Liu, L.; Rong, H.; Li, L.; Liu, X.; Jia, Z.; Zhang, H.; Wang, B.; Song, D.; Hu, J.; et al. Axial Shortening Effects of Repeated Low-Level Red-Light Therapy in Children with High Myopia: A Multicenter Randomized Controlled Trial. Am. J. Ophthalmol. 2025, 270, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, R.; Read, S.A.; Collins, M.J. Diurnal Variations in Axial Length, Choroidal Thickness, Intraocular Pressure, and Ocular Biometrics. Investig. Ophthalmol. Vis. Sci. 2011, 52, 5121–5129. [Google Scholar] [CrossRef]
- Li, Z.; Hu, Y.; Cui, D.; Long, W.; He, M.; Yang, X. Change in Subfoveal Choroidal Thickness Secondary to Orthokeratology and Its Cessation: A Predictor for the Change in Axial Length. Acta Ophthalmol. 2019, 97, e454–e459. [Google Scholar] [CrossRef]
- Lau, J.K.; Wan, K.; Cheung, S.-W.; Vincent, S.J.; Cho, P. Weekly Changes in Axial Length and Choroidal Thickness in Children During and Following Orthokeratology Treatment with Different Compression Factors. Transl. Vis. Sci. Technol. 2019, 8, 9. [Google Scholar] [CrossRef]
- Hu, Y.; Ding, X.; Jiang, J.; Yu, M.; Chen, L.; Zhai, Z.; Zhang, H.; Fang, B.; Wang, H.; Yu, S.; et al. Long-Term Axial Length Shortening in Myopic Orthokeratology: Incident Probability, Time Course, and Influencing Factors. Investig. Ophthalmol. Vis. Sci. 2023, 64, 37. [Google Scholar] [CrossRef]
- Wang, A.; Yang, C.; Shen, L.; Wang, J.; Zhang, Z.; Yang, W. Axial Length Shortening after Orthokeratology and Its Relationship with Myopic Control. BMC Ophthalmol. 2022, 22, 243. [Google Scholar] [CrossRef]
- Ofuji, Y.; Torii, H.; Yotsukura, E.; Mori, K.; Kurihara, T.; Negishi, K.; Tsubota, K. Axial Length Shortening in a Myopic Child with Anisometropic Amblyopia after Wearing Violet Light-Transmitting Eyeglasses for 2 Years. Am. J. Ophthalmol. 2020, 20, 101002. [Google Scholar] [CrossRef]
- Tang, X.-H.; Yu, M.-T.; Hu, Y.; He, M.-G.; Yang, X. Axial Length Shortening in Myopic Children with Stickler Syndrome after Repeated Low-Level Red-Light Therapy. Int. J. Ophthalmol. 2023, 16, 1712–1717. [Google Scholar] [CrossRef]
- Wallman, J.; Wildsoet, C.; Xu, A.; Gottlieb, M.D.; Nickla, D.L.; Marran, L.; Krebs, W.; Christensen, A.M. Moving the Retina: Choroidal Modulation of Refractive State. Vis. Res. 1995, 35, 37–50. [Google Scholar] [CrossRef] [PubMed]
- Wildsoet, C.; Wallman, J. Choroidal and Scleral Mechanisms of Compensation for Spectacle Lenses in Chicks. Vis. Res. 1995, 35, 1175–1194. [Google Scholar] [CrossRef] [PubMed]
- Hung, L.F.; Wallman, J.; Smith, E.L. Vision-Dependent Changes in the Choroidal Thickness of Macaque Monkeys. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1259–1269. [Google Scholar]
- Troilo, D.; Nickla, D.L.; Wildsoet, C.F. Choroidal Thickness Changes during Altered Eye Growth and Refractive State in a Primate. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1249–1258. [Google Scholar]
- Nickla, D.L.; Wallman, J. The Multifunctional Choroid. Prog. Retin. Eye Res. 2010, 29, 144–168. [Google Scholar] [CrossRef]
- Flores-Moreno, I.; Lugo, F.; Duker, J.S.; Ruiz-Moreno, J.M. The Relationship between Axial Length and Choroidal Thickness in Eyes with High Myopia. Am. J. Ophthalmol. 2013, 155, 314–319. [Google Scholar] [CrossRef]
- Sogawa, K.; Nagaoka, T.; Takahashi, A.; Tanano, I.; Tani, T.; Ishibazawa, A.; Yoshida, A. Relationship between Choroidal Thickness and Choroidal Circulation in Healthy Young Subjects. Am. J. Ophthalmol. 2012, 153, 1129–1132.e1. [Google Scholar] [CrossRef]
- Torii, H.; Kurihara, T.; Seko, Y.; Negishi, K.; Ohnuma, K.; Inaba, T.; Kawashima, M.; Jiang, X.; Kondo, S.; Miyauchi, M.; et al. Violet Light Exposure Can Be a Preventive Strategy Against Myopia Progression. eBioMedicine 2017, 15, 210–219. [Google Scholar] [CrossRef]
- Mori, K.; Torii, H.; Hara, Y.; Hara, M.; Yotsukura, E.; Hanyuda, A.; Negishi, K.; Kurihara, T.; Tsubota, K. Effect of Violet Light-Transmitting Eyeglasses on Axial Elongation in Myopic Children: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 5462. [Google Scholar] [CrossRef]
- Jiang, X.; Pardue, M.T.; Mori, K.; Ikeda, S.-I.; Torii, H.; D’Souza, S.; Lang, R.A.; Kurihara, T.; Tsubota, K. Violet Light Suppresses Lens-Induced Myopia via Neuropsin (OPN5) in Mice. Proc. Natl. Acad. Sci. USA 2021, 118, e2018840118. [Google Scholar] [CrossRef]

| Parameter | Mean ± SD (Range) |
|---|---|
| Gender | Male 13 (54.2%); female 11 (45.8%) |
| Age (years) | 13.9 ± 2.8 (8–19) |
| Prescribed CL (D) | −5.45 ± 2.07 (−1.00 to 10.00) |
| Outdoor activity time (minutes) | 146.0 ± 80.8 (30–369) |
| Involvement in outdoor club activities | 33.3% |
| Near work time (minutes) | 93.0 ± 43.5 (20–174) |
| Parental history of myopia (either or both) | 95.8% |
| Parameters | Baseline Mean ± SD | After Wearing EDOF CLs Mean ± SD | Change Mean ± SD | p Value |
|---|---|---|---|---|
| Non-cycloplegic objective refraction (D) | −6.38 ± 2.47 | −6.61 ± 2.48 | −0.23 ± 0.53 | 0.054 |
| AL (mm) | 26.31 ± 1.34 | 26.40 ± 1.33 | 0.09 ± 0.22 | 0.03 |
| CT (μm) | 235 ± 65 | 244 ± 72 | 8 ± 32 | 0.18 |
| Parameters | Increased Group (n = 14); Mean ± SD | Decreased Group (n = 5); Mean ± SD | p Value |
|---|---|---|---|
| Age at Prescription (year) | 12.9 ± 2.9 | 15.4 ± 2.1 | 0.14 |
| Objective Refraction at Prescription (diopter) | −6.65 ± 2.77 | −6.96 ± 2.16 | 0.71 |
| Axial Length at Prescription (mm) | 26.37 ± 1.35 | 26.88 ± 1.32 | 0.58 |
| Choroidal Thickness at Prescription (μm) | 216.68 ± 53.39 | 202.60 ± 67.87 | 0.46 |
| Outdoor Activities Time (minute) | 126.7 ± 62.6 | 200.6 ± 92.3 | 0.13 |
| Involvement in Outdoor Club Activities | 42.9% | 40.0% | 0.66 |
| Near Work Time (minute) | 86.0 ± 46.4 | 111.6 ± 18.0 | 0.21 |
| Parental History of Myopia (either or both) | 100.0% | 80.0% | 0.26 |
| Cases | Changes in Axial Length (mm/Year) | Changes in Choroidal Thickness (μm/Year) |
|---|---|---|
| 1 | −0.09 | +37 |
| 2 | −0.10 | +26 |
| 3 | −0.13 | +26 |
| 4 | −0.21 | −6 |
| 5 | −0.23 | +66 |
| Change in AL, (mm) (n = 24) | |||
|---|---|---|---|
| β | 95% CI | p Value | |
| Age (years) | −0.05 | −0.08 to −0.02 | 0.006 |
| Baseline AL (mm) | −0.02 | −0.08 to 0.05 | 0.59 |
| Near work time (minutes) | −0.00056 | −0.0033 to 0.0021 | 0.66 |
| Outdoor activity time (minutes) | 0.00017 | −0.0013 to 0.0016 | 0.80 |
| R2 | 0.48 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hazra, D.; Yotsukura, E.; Oyama, S.; Shigeno, Y.; Mori, K.; Takeuchi, R.; Nakajima, Y.; Hanyuda, A.; Ogawa, M.; Kurihara, T.; et al. Axial Length Stabilization or Reduction in over 40% of Patients Wearing Extended Depth-of-Focus Contact Lenses. J. Clin. Med. 2025, 14, 1750. https://doi.org/10.3390/jcm14051750
Hazra D, Yotsukura E, Oyama S, Shigeno Y, Mori K, Takeuchi R, Nakajima Y, Hanyuda A, Ogawa M, Kurihara T, et al. Axial Length Stabilization or Reduction in over 40% of Patients Wearing Extended Depth-of-Focus Contact Lenses. Journal of Clinical Medicine. 2025; 14(5):1750. https://doi.org/10.3390/jcm14051750
Chicago/Turabian StyleHazra, Debabrata, Erisa Yotsukura, Shihomi Oyama, Yuta Shigeno, Kiwako Mori, Rikako Takeuchi, Yurina Nakajima, Akiko Hanyuda, Mamoru Ogawa, Toshihide Kurihara, and et al. 2025. "Axial Length Stabilization or Reduction in over 40% of Patients Wearing Extended Depth-of-Focus Contact Lenses" Journal of Clinical Medicine 14, no. 5: 1750. https://doi.org/10.3390/jcm14051750
APA StyleHazra, D., Yotsukura, E., Oyama, S., Shigeno, Y., Mori, K., Takeuchi, R., Nakajima, Y., Hanyuda, A., Ogawa, M., Kurihara, T., Torii, H., & Negishi, K. (2025). Axial Length Stabilization or Reduction in over 40% of Patients Wearing Extended Depth-of-Focus Contact Lenses. Journal of Clinical Medicine, 14(5), 1750. https://doi.org/10.3390/jcm14051750







