Coronary Artery Calcium Is Independently Associated with Arterial Stiffness and LDL Cholesterol Burden in Patients with Familial Hypercholesterolemia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Parameters, Traditional CV Risk Factors, and Therapy Management
2.3. CT Scan Parameters
2.4. Carotid Intima-Media Thickness Assessment
2.5. Arterial Stiffness Evaluation
2.6. Lipid Analysis and Genetic Assessment
2.7. Cholesterol Burden Calculation
2.8. Statistical Analysis
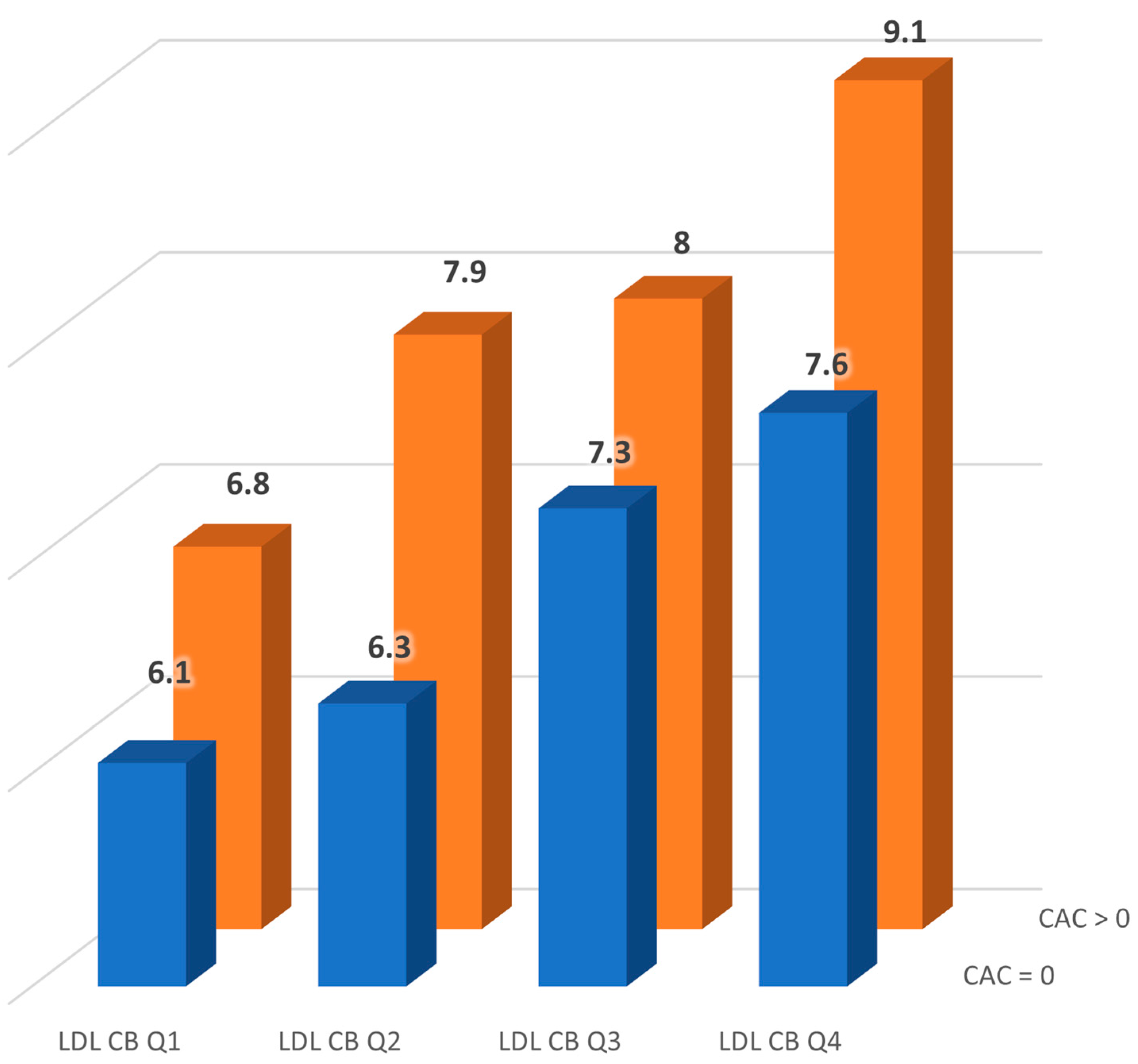
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abera, A.; Worede, A.; Hirigo, A.T.; Alemayehu, R.; Ambachew, S. Dyslipidemia and Associated Factors among Adult Cardiac Patients: A Hospital-Based Comparative Cross-Sectional Study. Eur. J. Med. Res. 2024, 29, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 5 February 2025).
- Hovingh, G.K.; Davidson, M.H.; Kastelein, J.J.P.P.; O’Connor, A.M. Diagnosis and Treatment of Familial Hypercholesterolaemia. Eur. Heart J. 2013, 34, 962–971. [Google Scholar] [CrossRef] [PubMed]
- Cuchel, M.; Bruckert, E.; Ginsberg, H.N.; Raal, F.J.; Santos, R.D.; Hegele, R.A.; Kuivenhoven, J.A.; Nordestgaard, B.G.; Descamps, O.S.; Steinhagen-Thiessen, E.; et al. Homozygous Familial Hypercholesterolaemia: New Insights and Guidance for Clinicians to Improve Detection and Clinical Management. A Position Paper from the Consensus Panel on Familial Hypercholesterolaemia of the European Atherosclerosis Society. Eur. Heart J. 2014, 35, 2146–2157. [Google Scholar] [CrossRef] [PubMed]
- Benn, M.; Watts, G.F.; Tybjærg-Hansen, A.; Nordestgaard, B.G. Mutations Causative of Familial Hypercholesterolaemia: Screening of 98 098 Individuals from the Copenhagen General Population Study Estimated a Prevalence of 1 in 217. Eur. Heart J. 2016, 37, 1384–1394. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef]
- Kroon, A.A.; Ajubi, N.; van Asten, W.N.; Stalenhoef, A.F. The Prevalence of Peripheral Vascular Disease in Familial Hypercholesterolaemia. J. Intern. Med. 1995, 238, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Tonstad, S.; Joakimsen, O.; Stensland-Bugge, E.; Ose, L.; Bønaa, K.H.; Leren, T.P. Carotid Intima-Media Thickness and Plaque in Patients with Familial Hypercholesterolaemia Mutations and Control Subjects. Eur. J. Clin. Investig. 1998, 28, 971–979. [Google Scholar] [CrossRef]
- Cocciolone, A.J.; Hawes, J.Z.; Staiculescu, M.C.; Johnson, E.O.; Murshed, M.; Wagenseil, J.E. Elastin, Arterial Mechanics, and Cardiovascular Disease. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H189–H205. [Google Scholar] [CrossRef] [PubMed]
- Zieman, S.J.; Melenovsky, V.; Kass, D.A. Mechanisms, Pathophysiology, and Therapy of Arterial Stiffness. Arter. Thromb. Vasc. Biol. 2005, 25, 932–943. [Google Scholar] [CrossRef] [PubMed]
- Scioli, M.G.; Storti, G.; D’amico, F.; Guzmán, R.R.; Centofanti, F.; Doldo, E.; Miranda, E.M.C.; Orlandi, A. Oxidative Stress and New Pathogenetic Mechanisms in Endothelial Dysfunction: Potential Diagnostic Biomarkers and Therapeutic Targets. J. Clin. Med. 2020, 9, 1995. [Google Scholar] [CrossRef]
- Laurent, S.; Cockcroft, J.; Van Bortel, L.; Boutouyrie, P.; Giannattasio, C.; Hayoz, D.; Pannier, B.; Vlachopoulos, C.; Wilkinson, I.; Struijker-Boudier, H.; et al. Expert Consensus Document on Arterial Stiffness: Methodological Issues and Clinical Applications. Eur. Heart J. 2006, 27, 2588–2605. [Google Scholar] [CrossRef] [PubMed]
- Levisianou, D.; Foussas, S.; Skopelitis, E.; Adamopoulou, E.; Xenopoulou, T.; Destounis, A.; Koukoulis, G.; Skoularigis, I.; Melidonis, A.; Triposkiadis, F. Arterial Stiffness Predicts Risk for Long-Term Recurrence in Patients with Type 2 Diabetes Admitted for Acute Coronary Event. Diabetes Res. Clin. Pract. 2013, 99, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Sequí-Domínguez, I.; Cavero-Redondo, I.; Álvarez-Bueno, C.; Pozuelo-Carrascosa, D.P.; Nuñez de Arenas-Arroyo, S.; Martínez-Vizcaíno, V. Accuracy of Pulse Wave Velocity Predicting Cardiovascular and All-Cause Mortality. A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2080. [Google Scholar] [CrossRef] [PubMed]
- Detrano, R.; Guerci, A.D.; Carr, J.J.; Bild, D.E.; Burke, G.; Folsom, A.R.; Liu, K.; Shea, S.; Szklo, M.; Bluemke, D.A.; et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. N. Engl. J. Med. 2008, 358, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Gallo, A.; De Isla, L.P.; Charrière, S.; Vimont, A.; Alonso, R.; Muñiz-Grijalvo, O.; Díaz-Díaz, J.L.; Zambón, D.; Moulin, P.; Bruckert, E.; et al. The Added Value of Coronary Calcium Score in Predicting Cardiovascular Events in Familial Hypercholesterolemia. JACC Cardiovasc. Imaging 2021, 14, 2414–2424. [Google Scholar] [CrossRef]
- Hussain, B.; Mahmood, A.; Flynn, M.G.; Alexander, T. Coronary Artery Calcium Scoring in Asymptomatic Patients. HCA Healthc. J. Med. 2023, 4, 341. [Google Scholar] [CrossRef]
- Cheng, H.M.; Ye, Z.X.; Chiou, K.R.; Lin, S.J.; Charng, M.J. Vascular Stiffness in Familial Hypercholesterolaemia Is Associated with C-Reactive Protein and Cholesterol Burden. Eur. J. Clin. Investig. 2007, 37, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Gallo, A.; Giral, P.; Carrié, A.; Carreau, V.; Béliard, S.; Bittar, R.; Maranghi, M.; Arca, M.; Cluzel, P.; Redheuil, A.; et al. Early Coronary Calcifications Are Related to Cholesterol Burden in Heterozygous Familial Hypercholesterolemia. J. Clin. Lipidol. 2017, 11, 704–711.e2. [Google Scholar] [CrossRef] [PubMed]
- Reiner, Z.; Capatano, A.; De Backer, G.; Graham, I. ESC/EAS Guidelines for the Management of Dyslipidemias. Eur. Hear. J. 2011, 32, 1769–1818. [Google Scholar] [CrossRef]
- Touboul, P.J.; Hennerici, M.G.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Fatar, M.; et al. Mannheim Carotid Intima-Media Thickness Consensus (2004–2006). An Update on Behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006. Cerebrovasc. Dis. 2007, 23, 75–80. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, I.B.; McEniery, C.M.; Schillaci, G.; Boutouyrie, P.; Segers, P.; Donald, A.; Chowienczyk, P.J. ARTERY Society Guidelines for Validation of Non-Invasive Haemodynamic Measurement Devices: Part 1, Arterial Pulse Wave Velocity. Artery Res. 2010, 4, 34–40. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the Concentration of Low-Density Lipoprotein Cholesterol in Plasma, without Use of the Preparative Ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Spina, R.; Noto, D.; Barbagallo, C.M.; Monastero, R.; Ingrassia, V.; Valenti, V.; Baschi, R.; Pipitone, A.; Giammanco, A.; La Spada, M.P.; et al. Genetic Epidemiology of Autosomal Recessive Hypercholesterolemia in Sicily: Identification by next-Generation Sequencing of a New Kindred. J. Clin. Lipidol. 2018, 12, 145–151. [Google Scholar] [CrossRef]
- Bertolini, S.; Pisciotta, L.; Rabacchi, C.; Cefalù, A.B.; Noto, D.; Fasano, T.; Signori, A.; Fresa, R.; Averna, M.; Calandra, S. Spectrum of Mutations and Phenotypic Expression in Patients with Autosomal Dominant Hypercholesterolemia Identified in Italy. Atherosclerosis 2013, 227, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Hoeg, J.M.; Feuerstein, I.M.; Tucker, E.E. Detection and Quantitation of Calcific Atherosclerosis by Ultrafast Computed Tomography in Children and Young Adults with Homozygous Familial Hypercholesterolemia. Arterioscler. Thromb. A J. Vasc. Biol. Am. Heart Assoc. 1994, 14, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Smilde, T.J.; van den Berkmortel, F.W.; Boers, G.H.; Wollersheim, H.; de Boo, T.; van Langen, H.; Stalenhoef, A.F. Carotid and Femoral Artery Wall Thickness and Stiffness in Patients at Risk for Cardiovascular Disease, with Special Emphasis on Hyperhomocysteinemia. Arter. Thromb. Vasc. Biol. 1998, 18, 1958–1963. [Google Scholar] [CrossRef]
- Mattina, A.; Rosenbaum, D.; Bittar, R.; Bonnefont-Rousselot, D.; Noto, D.; Averna, M.; Bruckert, E.; Giral, P. Lipoprotein-Associated Phospholipase A2 Activity Is Increased in Patients with Definite Familial Hypercholesterolemia Compared with Other Forms of Hypercholesterolemia. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 517–523. [Google Scholar] [CrossRef]
- Cernes, R.; Zimlichman, R.; Shargorodsky, M. Arterial Elasticity in Cardiovascular Disease: Focus on Hypertension, Metabolic Syndrome and Diabetes. In Cardiovascular Diabetology: Clinical, Metabolic and Inflammatory Facets; KARGER: Basel, Switzerland, 2008; Volume 45, pp. 65–81. [Google Scholar]
- Wang, X.; Keith, J.C.; Struthers, A.D.; Feuerstein, G.Z. Assessment of Arterial Stiffness, a Translational Medicine Biomarker System for Evaluation of Vascular Risk. Cardiovasc. Ther. 2008, 26, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Smilde, T.J.; van den Berkmortel, F.W.; Wollersheim, H.; van Langen, H.; Kastelein, J.J.; Stalenhoef, A.F. The Effect of Cholesterol Lowering on Carotid and Femoral Artery Wall Stiffness and Thickness in Patients with Familial Hypercholesterolaemia. Eur. J. Clin. Investig. 2000, 30, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Giallauria, F.; Milaneschi, Y.; Tanaka, T.; Maggio, M.; Canepa, M.; Elango, P.; Vigorito, C.; Lakatta, E.G.; Ferrucci, L.; Strait, J. Arterial Stiffness and Vitamin D Levels: The Baltimore Longitudinal Study of Aging. J. Clin. Endocrinol. Metab. 2012, 97, 3717–3723. [Google Scholar] [CrossRef] [PubMed]
- Giallauria, F.; Ling, S.M.; Schreiber, C.; Maggio, M.; Shetty, V.; Muller, D.; Vigorito, C.; Ferrucci, L.; Najjar, S.S. Arterial Stiffness and Bone Demineralization: The Baltimore Longitudinal Study of Aging. Am. J. Hypertens. 2011, 24, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Reiner, Ž.; Simental-Mendía, L.E.; Ruscica, M.; Katsiki, N.; Banach, M.; Al Rasadi, K.; Jamialahmadi, T.; Sahebkar, A. Pulse Wave Velocity as a Measure of Arterial Stiffness in Patients with Familial Hypercholesterolemia: A Systematic Review and Meta-Analysis. Arch. Med. Sci. 2019, 15, 1365–1374. [Google Scholar] [CrossRef]
- Plana, N.; Ferré, R.; Merino, J.; Aragonès, G.; Girona, J.; Heras, M.; Masana, L. Heterozygous Familial Hypercholesterolaemic Patients Have Increased Arterial Stiffness, as Determined Using the Augmentation Index. J. Atheroscler. Thromb. 2011, 18, 1110–1116. [Google Scholar] [CrossRef][Green Version]
- Martinez, L.R.C.; Miname, M.H.; Bortolotto, L.A.; Chacra, A.P.M.; Rochitte, C.E.; Sposito, A.C.; Santos, R.D. No Correlation and Low Agreement of Imaging and Inflammatory Atherosclerosis’ Markers in Familial Hypercholesterolemia. Atherosclerosis 2008, 200, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Tada, H.; Kawashiri, M.-A.; Nohara, A.; Inazu, A.; Mabuchi, H.; Yamagishi, M. Assessment of Arterial Stiffness in Patients with Familial Hypercholesterolemia. J. Clin. Lipidol. 2017, 12, 397–402.e2. [Google Scholar] [CrossRef]
- Toikka, J.O.; Niemi, P.; Ahotupa, M.; Niinikoski, H.; Viikari, J.S.; Rönnemaa, T.; Hartiala, J.J.; Raitakari, O.T. Large-Artery Elastic Properties in Young Men: Relationships to Serum Lipoproteins and Oxidized Low-Density Lipoproteins. Arter. Thromb. Vasc. Biol. 1999, 19, 436–441. [Google Scholar] [CrossRef]
- Greenland, P.; Bonow, R.O.; Brundage, B.H.; Budoff, M.J.; Eisenberg, M.J.; Grundy, S.M.; Lauer, M.S.; Post, W.S.; Raggi, P.; Redberg, R.F.; et al. ACCF/AHA 2007 Clinical Expert Consensus Document on Coronary Artery Calcium Scoring By Computed Tomography in Global Cardiovascular Risk Assessment and in Evaluation of Patients With Chest Pain. J. Am. Coll. Cardiol. 2007, 49, 378–402. [Google Scholar] [CrossRef] [PubMed]
- Mattina, A.; Giammanco, A.; Giral, P.; Rosenbaum, D.; Carrié, A.; Cluzel, P.; Redheuil, A.; Bittar, R.; Béliard, S.; Noto, D.; et al. Polyvascular Subclinical Atherosclerosis in Familial Hypercholesterolemia: The Role of Cholesterol Burden and Gender. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, L.; Lee, R.T. Mechanisms of Plaque Rupture Mechanical and Biologic Interactions. Cardiovasc. Res. 1999, 41, 369–375. [Google Scholar] [CrossRef] [PubMed]
| Clinical Characteristics | Total Population | |
|---|---|---|
| n | 100 | |
| Age, years | 45.9 ± 16.2 | |
| Sex, male (%) | 50 (50) | |
| PWV, m/s | 7.44 ± 2.36 | |
| Xanthomas, n (%) | 21 (21) | |
| Age at start of treatment, years | 29.3 ± 14.2 | |
| Systolic BP, mmHg | 128.8 ± 21.4 | |
| Diastolic BP, mmHg | 73.2 ± 11.3 | |
| Mean BP, mmHg | 93.7 ± 13.0 | |
| Cardiovascular risk factors | ||
| Secondary prevention, n (%) | 13 (13) | |
| Current smoking, n (%) | 31 (31) | |
| Type 2 Diabetes, n (%) | 7 (7) | |
| BMI, kg2/h | 27.4 ± 4.9 | |
| Arterial hypertension, n (%) | 23 (23) | |
| Treatment | ||
| Antihypertensive treatment, n (%) | 24 (24) | |
| Statins, n (%) | 88 (88) | |
| Ezetimibe, n (%) | 45 (45) | |
| Alirocumab, n (%) | 8 (8) | |
| Lipid profile | ||
| Total cholesterol, mmol/L | 5.7 (4.8–7.1) | |
| LDL cholesterol, mmol/L | 3.7 (2.8–4.7) | |
| HDL cholesterol, mmol/L | 1.4 (1.2–1.6) | |
| Triglycerides, mmol/L | 1.0 (0.7–1.6) | |
| Non-HDL cholesterol, mmol/L | 4.2 (3.3–5.4) | |
| Lp(a), mg/dL | 18.8 (5.52–47) | |
| LDL-C burden | ||
| LDL cholesterol burden pre-treatment, mmol-years/L | 181.4 (133.7–286.6) | |
| LDL cholesterol burden post treatment, mmol-years/L | 70.9 (33.7–111.5) | |
| LDL cholesterol burden total, mmol-years/L | 259.7 (186.6–338.7) | |
| Carotid atherosclerosis | ||
| Maximum cIMT, mm | 0.8 (0.63–0.90) | |
| Mean cIMT, mm | 0.7 (0.60–0.85) | |
| CAC | ||
| Agatston calcium score, log | 2.14 ± 2.69 |
| logCAC | |||
|---|---|---|---|
| r | p | ||
| Characteristics | |||
| Age, years | 0.65 | <0.0001 | |
| Sex, male | 0.14 | 0.1803 | |
| PWV, m/s | 0.52 | <0.0001 | |
| Xanthomas | 0.26 | 0.0104 | |
| Cardiovascular risk factors | |||
| Secondary prevention | 0.45 | <0.0001 | |
| Current smoking | −0.05 | 0.6560 | |
| Type 2 Diabetes | 0.38 | <0.0001 | |
| BMI, kg2/h | 0.28 | 0.0044 | |
| Arterial Hypertension | 0.51 | <0.0001 | |
| Systolic BP, mmHg | 0.46 | <0.0001 | |
| Diastolic BP, mmHg | 0.21 | 0.0381 | |
| Mean BP, mmHg | 0.37 | 0.0001 | |
| Treatment | |||
| Antihypertensive treatment | 0.49 | <0.0001 | |
| Statins | −0.09 | 0.3509 | |
| Ezetimibe | 0.28 | 0.0051 | |
| Alirocumab | 0.27 | 0.0059 | |
| Lipid profile | |||
| Total cholesterol, mmol/L | −0.10 | 0.3051 | |
| LDL cholesterol, mmol/L | −0.12 | 0.2420 | |
| HDL cholesterol, mmol/L | −0.07 | 0.4968 | |
| Triglycerides, mmol/L | 0.12 | 0.2536 | |
| Non-HDL cholesterol, mmol/L | −0.09 | 0.3564 | |
| Lp(a), mg/dL | −0.09 | 0.6342 | |
| LDL-C burden | |||
| LDL cholesterol burden pre-treatment, mmol-years/L | 0.49 | <0.0001 | |
| LDL cholesterol burden post treatment, mmol-years/L | 0.23 | 0.0228 | |
| LDL cholesterol burden total, mmol-years/L | 0.55 | <0.0001 | |
| Carotid atherosclerosis | |||
| Maximum cIMT, mm | 0.43 | <0.0001 | |
| Mean cIMT, mm | 0.48 | <0.0001 | |
| Log CAC | |||
|---|---|---|---|
| R2 | β (SE) | p | |
| Overall Model | 0.48 | <0.0001 | |
| PWV (m/s) | 0.337 (0.109) | 0.0026 | |
| Total LDL-C Burden (mmol/L) | 0.009 (0.002) | <0.0001 | |
| Sex (male) | 0.820 (0.486) | 0.0954 | |
| Mean Blood Pressure (mmHg) | 0.013 (0.019) | 0.5004 | |
| Smoking (yes = 1) | 0.200 (0.454) | 0.6597 | |
| LDL-C (mmol/L) | −0.007 (0.004 | 0.0993 | |
| HDL-C (mmol/L) | −0.018 (0.018) | 0.3205 | |
| Lipid-lowering drugs (yes = 1) | −1.057 (0.750) | 0.1622 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mattina, A.; Giammanco, A.; Noto, D.; Geraci, G.; Nardi, E.; Barbagallo, C.M.; Gagliardo, C.M.; Giusti, M.A.; D’Ignoto, F.; Giallauria, F.; et al. Coronary Artery Calcium Is Independently Associated with Arterial Stiffness and LDL Cholesterol Burden in Patients with Familial Hypercholesterolemia. J. Clin. Med. 2025, 14, 1245. https://doi.org/10.3390/jcm14041245
Mattina A, Giammanco A, Noto D, Geraci G, Nardi E, Barbagallo CM, Gagliardo CM, Giusti MA, D’Ignoto F, Giallauria F, et al. Coronary Artery Calcium Is Independently Associated with Arterial Stiffness and LDL Cholesterol Burden in Patients with Familial Hypercholesterolemia. Journal of Clinical Medicine. 2025; 14(4):1245. https://doi.org/10.3390/jcm14041245
Chicago/Turabian StyleMattina, Alessandro, Antonina Giammanco, Davide Noto, Giulio Geraci, Emilio Nardi, Carlo Maria Barbagallo, Carola Maria Gagliardo, Maria Ausilia Giusti, Francesco D’Ignoto, Francesco Giallauria, and et al. 2025. "Coronary Artery Calcium Is Independently Associated with Arterial Stiffness and LDL Cholesterol Burden in Patients with Familial Hypercholesterolemia" Journal of Clinical Medicine 14, no. 4: 1245. https://doi.org/10.3390/jcm14041245
APA StyleMattina, A., Giammanco, A., Noto, D., Geraci, G., Nardi, E., Barbagallo, C. M., Gagliardo, C. M., Giusti, M. A., D’Ignoto, F., Giallauria, F., Di Benedetto, C., Cardella, A. M., Toia, P., La Grutta, L., Cefalù, A. B., & Averna, M. (2025). Coronary Artery Calcium Is Independently Associated with Arterial Stiffness and LDL Cholesterol Burden in Patients with Familial Hypercholesterolemia. Journal of Clinical Medicine, 14(4), 1245. https://doi.org/10.3390/jcm14041245









