Impact of Combined Neuromuscular Electrical Stimulation (Comb-NMES) on Glucose Signaling and Muscle Myofiber Distribution in a Patient with Acute Spinal Cord Injury and Lower Motor Neuron Lesion
Abstract
1. Introduction
2. Case Presentation
3. Clinical and Laboratory Procedures
Blood Glucose, Insulin, and Lipid Measurements
4. Statistical Analysis
5. Results
5.1. Fasting Insulin and Glucose Levels
5.2. Fasting Lipid Profile
5.3. Skeletal Muscle Intracellular Signaling
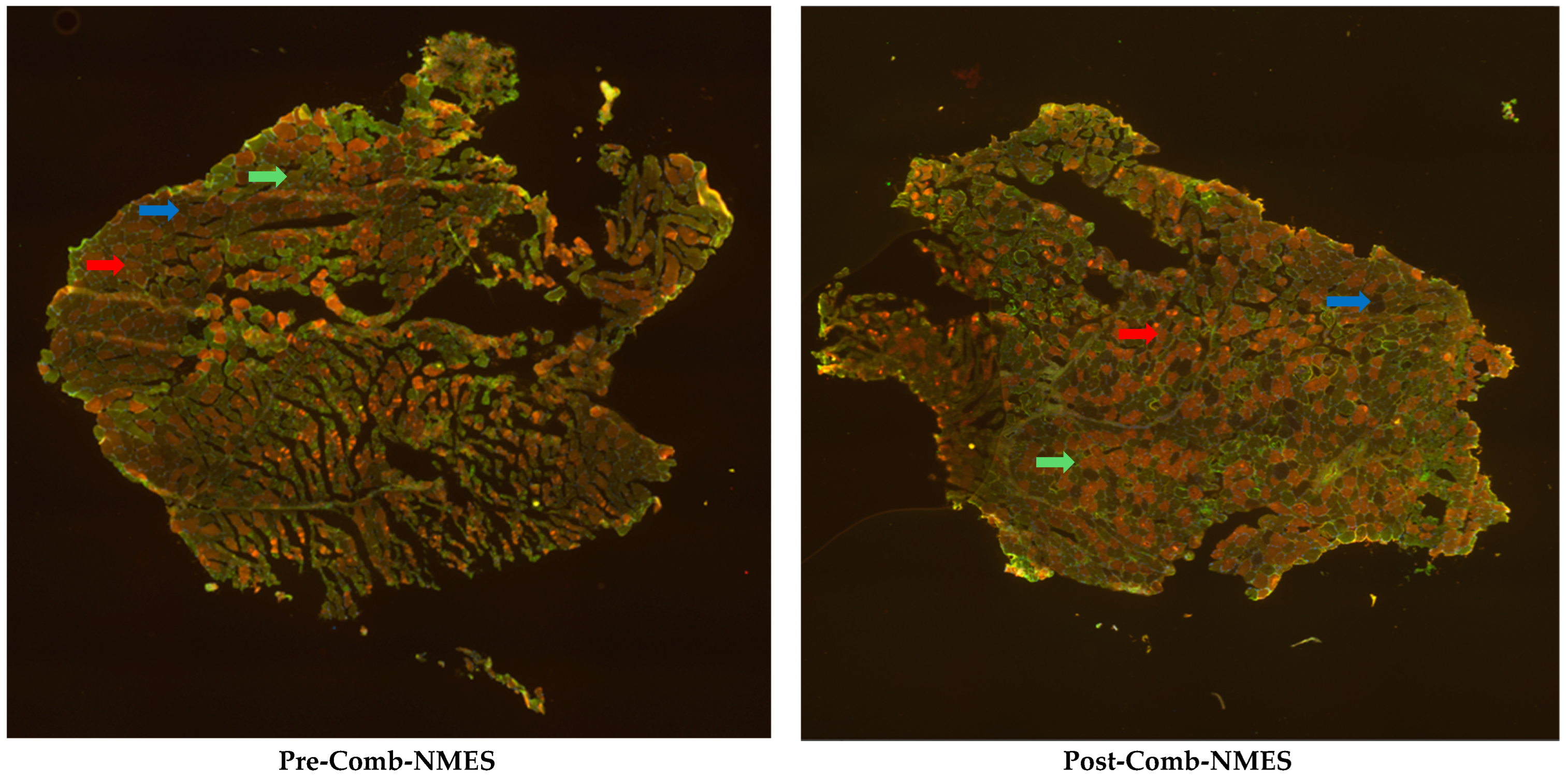
5.4. Myofiber-Type Distribution
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Baligand, C.; Chen, Y.-W.; Ye, F.; Pandey, S.N.; Lai, S.-H.; Liu, M.; Vandenborne, K. Transcriptional Pathways Associated with Skeletal Muscle Changes after Spinal Cord Injury and Treadmill Locomotor Training. BioMed Res. Int. 2015, 2015, 387090. [Google Scholar] [CrossRef]
- Budd, M.A.; Gater Jr, D.R.; Channell, I. Psychosocial consequences of spinal cord injury: A narrative review. J. Pers. Med. 2022, 12, 1178. [Google Scholar] [CrossRef]
- Drasites, K.P.; Shams, R.; Zaman, V.; Matzelle, D.; Shields, D.C.; Garner, D.P.; Sole, C.J.; Haque, A.; Banik, N.L. Pathophysiology, biomarkers, and therapeutic modalities associated with skeletal muscle loss following spinal cord injury. Brain Sci. 2020, 10, 933. [Google Scholar] [CrossRef]
- Jackman, R.W.; Cornwell, E.W.; Wu, C.L.; Kandarian, S.C. Nuclear factor-κB signalling and transcriptional regulation in skeletal muscle atrophy. Exp. Physiol. 2013, 98, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, I.; Ijaz, S.; Gholaminejhad, M.; Hassanzadeh, G. Clinical Complications Associated with Spinal Cord Injury: A Narrative Review. J. Contemp. Med. Sci. 2021, 7, 264–271. [Google Scholar] [CrossRef]
- Kern, H.; Carraro, U.; Adami, N.; Biral, D.; Hofer, C.; Forstner, C.; Mödlin, M.; Vogelauer, M.; Pond, A.; Boncompagni, S.; et al. Home-based functional electrical stimulation rescues permanently denervated muscles in paraplegic patients with complete lower motor neuron lesion. Neurorehabilit. Neural Repair 2010, 24, 709–721. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, S.; Davis, J.; Bersch, I.; Goldberg, G.; Gorgey, A.S. Electrical stimulation and denervated muscles after spinal cord injury. Neural Regen. Res. 2020, 15, 1397–1407. [Google Scholar]
- Doherty, J.G.; Burns, A.S.; O’Ferrall, D.M.; Ditunno, M., Jr; John, F. Prevalence of upper motor neuron vs lower motor neuron lesions in complete lower thoracic and lumbar spinal cord injuries. J. Spinal Cord Med. 2002, 25, 289–292. [Google Scholar] [CrossRef]
- Franz, S.; Eck, U.; Schuld, C.; Heutehaus, L.; Wolf, M.; Wilder-Smith, E.; Schulte-Mattler, W.; Weber, M.-A.; Rupp, R.; Weidner, N. Lower motoneuron dysfunction impacts spontaneous motor recovery in acute cervical spinal cord injury. J. Neurotrauma 2023, 40, 862–875. [Google Scholar] [CrossRef]
- Kern, H.; Hofer, C.; Mödlin, M.; Mayr, W.; Vindigni, V.; Zampieri, S.; Boncompagni, S.; Protasi, F.; Carraro, U. Stable muscle atrophy in long-term paraplegics with complete upper motor neuron lesion from 3-to 20-year SCI. Spinal Cord 2008, 46, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Dulhunty, A.F.; Gage, P.W. Excitation-contraction coupling and charge movement in denervated rat extensor digitorum longus and soleus muscles. J. Physiol. 1985, 358, 75–89. [Google Scholar] [CrossRef]
- Kern, H.; Boncompagni, S.; Rossini, K.; Mayr, W.; Fanò, G.; Zanin, M.E.; Podhorska-Okolow, M.; Protasi, F.; Carraro, U. Long-term denervation in humans causes degeneration of both contractile and excitation-contraction coupling apparatus, which is reversible by functional electrical stimulation (FES): A role for myofiber regeneration? J. Neuropathol. Exp. Neurol. 2004, 63, 919–931. [Google Scholar] [CrossRef] [PubMed]
- Biral, D.; Kern, H.; Adami, N.; Boncompagni, S.; Protasi, F.; Carraro, U. Atrophy-resistant fibers in permanent peripheral denervation of human skeletal muscle. Neurol. Res. 2008, 30, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Bochkezanian, V.; Newton, R.U.; Trajano, G.S.; Blazevich, A.J. Effects of neuromuscular electrical stimulation in people with spinal cord injury. Med. Sci. Sports Exerc. 2018, 50, 1733–1739. [Google Scholar] [CrossRef] [PubMed]
- Erickson, M.L.; Ryan, T.E.; Backus, D.; McCully, K.K. Endurance neuromuscular electrical stimulation training improves skeletal muscle oxidative capacity in individuals with motor-complete spinal cord injury. Muscle Nerve 2017, 55, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Yarar-Fisher, C.; Polston, K.F.; Eraslan, M.; Henley, K.Y.; Kinikli, G.I.; Bickel, C.S.; Windham, S.T.; McLain, A.B.; Oster, R.A.; Bamman, M.M. Paralytic and nonparalytic muscle adaptations to exercise training versus high-protein diet in individuals with long-standing spinal cord injury. J. Appl. Physiol. 2018, 125, 64–72. [Google Scholar] [CrossRef]
- Frostell, A.; Hakim, R.; Thelin, E.P.; Mattsson, P.; Svensson, M. A review of the segmental diameter of the healthy human spinal cord. Front. Neurol. 2016, 7, 238. [Google Scholar] [CrossRef]
- Alharbi, A.; Li, J.; Womack, E.; Farrow, M.; Yarar-Fisher, C. The Effect of Lower Limb Combined Neuromuscular Electrical Stimulation on Skeletal Muscle Signaling for Glucose Utilization, Myofiber Distribution, and Metabolic Function after Spinal Cord Injury. Int. J. Environ. Res. Public Health 2023, 20, 6958. [Google Scholar] [CrossRef]
- Carnevale Schianca, G.P.; Rossi, A.; Sainaghi, P.P.; Maduli, E.; Bartoli, E. The significance of impaired fasting glucose versus impaired glucose tolerance: Importance of insulin secretion and resistance. Diabetes Care 2003, 26, 1333–1337. [Google Scholar] [CrossRef] [PubMed]
- Röckl, K.S.; Witczak, C.A.; Goodyear, L.J. Signaling mechanisms in skeletal muscle: Acute responses and chronic adaptations to exercise. IUBMB Life 2008, 60, 145–153. [Google Scholar] [CrossRef]
- Yarar-Fisher, C.; Bickel, C.S.; Windham, S.T.; McLain, A.B.; Bamman, M.M. Skeletal muscle signaling associated with impaired glucose tolerance in spinal cord-injured men and the effects of contractile activity. J. Appl. Physiol. 2013, 115, 756–764. [Google Scholar] [CrossRef]
- Sylow, L.; Kleinert, M.; Richter, E.A.; Jensen, T.E. Exercise-stimulated glucose uptake—Regulation and implications for glycaemic control. Nat. Rev. Endocrinol. 2017, 13, 133–148. [Google Scholar] [CrossRef]
- Richter, E.A. Novel regulatory mechanisms in muscle metabolism during exercise. Exp. Physiol. 2014, 99, 1559–1561. [Google Scholar] [CrossRef]
- Long, Y.C.; Kostovski, E.; Boon, H.; Hjeltnes, N.; Krook, A.; Widegren, U. Differential expression of metabolic genes essential for glucose and lipid metabolism in skeletal muscle from spinal cord injured subjects. J. Appl. Physiol. 2011, 110, 1204–1210. [Google Scholar] [CrossRef] [PubMed]
- Dudley-Javoroski, S.; Shields, R.K. Muscle and bone plasticity after spinal cord injury: Review of adaptations to disuse and to electrical muscle stimulation. J. Rehabil. Res. Dev. 2008, 45, 283. [Google Scholar] [CrossRef] [PubMed]
- Mukund, K.; Subramaniam, S. Skeletal muscle: A review of molecular structure and function, in health and disease. Wiley Interdiscip. Rev. Syst. Biol. Med. 2020, 12, e1462. [Google Scholar] [CrossRef] [PubMed]
- Ryan, T.E.; Erickson, M.L.; Young, H.-J.; McCully, K.K. Case report: Endurance electrical stimulation training improves skeletal muscle oxidative capacity in chronic spinal cord injury. Arch. Phys. Med. Rehabil. 2013, 94, 2559–2561. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alharbi, A.; Womack, E.; Yarar-Fisher, C. Impact of Combined Neuromuscular Electrical Stimulation (Comb-NMES) on Glucose Signaling and Muscle Myofiber Distribution in a Patient with Acute Spinal Cord Injury and Lower Motor Neuron Lesion. J. Clin. Med. 2025, 14, 876. https://doi.org/10.3390/jcm14030876
Alharbi A, Womack E, Yarar-Fisher C. Impact of Combined Neuromuscular Electrical Stimulation (Comb-NMES) on Glucose Signaling and Muscle Myofiber Distribution in a Patient with Acute Spinal Cord Injury and Lower Motor Neuron Lesion. Journal of Clinical Medicine. 2025; 14(3):876. https://doi.org/10.3390/jcm14030876
Chicago/Turabian StyleAlharbi, Amal, Erika Womack, and Ceren Yarar-Fisher. 2025. "Impact of Combined Neuromuscular Electrical Stimulation (Comb-NMES) on Glucose Signaling and Muscle Myofiber Distribution in a Patient with Acute Spinal Cord Injury and Lower Motor Neuron Lesion" Journal of Clinical Medicine 14, no. 3: 876. https://doi.org/10.3390/jcm14030876
APA StyleAlharbi, A., Womack, E., & Yarar-Fisher, C. (2025). Impact of Combined Neuromuscular Electrical Stimulation (Comb-NMES) on Glucose Signaling and Muscle Myofiber Distribution in a Patient with Acute Spinal Cord Injury and Lower Motor Neuron Lesion. Journal of Clinical Medicine, 14(3), 876. https://doi.org/10.3390/jcm14030876





