The Effect of Osteopathic Visceral Manipulation on Quality of Life and Postural Stability in Women with Endometriosis and Women with Pelvic Organ Prolapse: A Non-Controlled Before–After Clinical Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Type of Study and Participants
2.2. Visceral Manipulation
2.3. Outcome Measures: Quality of Life and Postural Stability
2.4. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parsons, J.; Marcer, N. Osteopathy: Models for Diagnosis, Treatment and Practice; Churchill Livingstone: Edinburgh, UK, 2005; pp. 135–167. [Google Scholar]
- Orrock, P. Profile of members of the Australian Osteopathic Association: Part 1—The practitioners. Int. J. Osteopath. Med. 2009, 12, 14–24. [Google Scholar] [CrossRef]
- Ruffini, N.; D’Alessandro, G.; Pimpinella, A.; Galli, M.; Galeotti, T.; Cerritelli, F.; Tramontano, M. The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review. Healthcare 2022, 10, 1566. [Google Scholar] [CrossRef]
- Tramontano, O.; Tamburella, F.; Dal Farra, F.; Bergna, A.; Lunghi, C.; Innocenti, M.; Cavera, F.; Savini, F.; Manzo, V.; D’Alessandro, G. International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare 2022, 10, 28. [Google Scholar] [CrossRef]
- Available online: https://www.aacom.org/docs/default-source/publications/glossary2017.pdf (accessed on 7 January 2025).
- Novack, J.C.; Whitton, E.L.; Smith, R.N.; Sciarretta, J.D.; Nguyen, J. Abdominal Wall Evisceration Coupled with Iliac Vascular Injury after Blunt Trauma. Cureus 2023, 15, e34917. [Google Scholar] [CrossRef]
- Jeong, H.; Jung, S.; Heo, T.G.; Choi, P.W.; Kim, J.I.; Jung, S.M.; Jun, H.; Shin, Y.C.; Um, E. Could the Injury Severity Score be a new indicator for surgical treatment in patients with traumatic splenic injury? J. Trauma Inj. 2022, 35, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Brandner, E.D.; Wu, A.; Chen, H.; Heron, D.; Kalnicki, S.; Komanduri, K.; Gerszten, K.; Burton, S.; Ahmed, I.; Shou, Z. Abdominal organ motion measured using 4D CT. Int. J. Radiat. Oncol. Biol. Phys. 2006, 65, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Bove, G.M.; Chapelle, S.L. Visceral mobilization can lyse and prevent peritoneal adhesions in a rat model. J. Bodyw. Mov. Ther. 2021, 16, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Lamblin, G.; Delorme, E.; Cosson, M.; Rubod, C. Cystocele and functional anatomy of the pelvic floor: Review and update of the various theories. Int. Urogynecol. J. 2016, 27, 1297–1305. [Google Scholar] [CrossRef] [PubMed]
- Hedley, G. Notes on visceral adhesions as fascial pathology. J. Bodyw. Mov. Ther. 2010, 14, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Schleip, R.; Findley, T.; Chaitow, L.; Huijing, P.A.J.B.M. Fascia: The Tensional Network of the Human Body: The Science and Clinical Applications in Manual and Movement Therapy; Elsevier Health Sciences imprint Churchill Livingstone: London, UK, 2012; pp. 245–266. [Google Scholar]
- Bordoni, B.; Zanier, E. Skin, fascias, and scars: Symptoms and systemic connections. J. Multidiscip. Healthc. 2014, 7, 11–24. [Google Scholar] [CrossRef]
- Craig, A.D. How do you feel? Interoception: The sense of the physiological condition of the body. Nat. Rev. Neurosci. 2002, 3, 655–666. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, G.; Cerritelli, F.; Cortelli, P. Sensitization and Interoception as Key Neurological Concepts in Osteopathy and Other Manual Medicines. Front. Neurosci. 2016, 10, 100. [Google Scholar] [CrossRef] [PubMed]
- McMahon, S.B.; Abel, C. A model for the study of visceral pain states: Chronic inflammation of the chronic decerebrate rat urinary bladder by irritant chemicals. Pain 1987, 28, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Wesselmann, U.; Lai, J. Mechanisms of referred visceral pain: Uterine inflammation in the adult virgin rat results in neurogenic plasma extravasation in the skin. Pain 1997, 73, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Collebrusco, L.; Lombardini, R.; Censi, G. An Alternative Approach to the Gastroesophageal Reflux Disease: Manual Techniques and Nutrition. Open J. Ther. Rehabil. 2017, 5, 98–106. [Google Scholar] [CrossRef]
- Gershon, M.D. The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and Intestine; HarperPerennial: New York, NY, USA, 1999; pp. 145–196. [Google Scholar]
- Binnebösel, M.; Klinge, U.; Rosch, R.; Junge, K.; Lynen-Jansen, P.; Schumpelick, V. Morphology, quality, and composition in mature human peritoneal adhesions. Langenbeck’s Arch. Surg. 2008, 393, 59–66. [Google Scholar] [CrossRef]
- Rickenbacher, E.; Baez, M.A.; Hale, L.; Leiser, S.C.; Zderic, S.A.; Valentino, R.J. Impact of overactive bladder on the brain: Central sequelae of a visceral pathology. Proc. Natl. Acad. Sci. USA 2008, 105, 10589–10594. [Google Scholar] [CrossRef] [PubMed]
- González-Muñoz, A.; Pruimboom, L.; Navarro-Ledesma, S. The Relationship Between the Elastic Properties and Pain Pressure Threshold in Cesarean Scar Tissue-An Observational Study. Healthcare 2024, 12, 2166. [Google Scholar] [CrossRef]
- Oliveira Souza Lima, S.R.; Kanemitsu, K.; Rashid, M.; Patel, V.K.; Ali, M. Long-Term Efficacy and Safety of Adhesion Prevention Agents in Abdominal and Pelvic Surgeries: A Systematic Review. Cureus 2024, 16, e71280. [Google Scholar] [CrossRef]
- Erdi, M.; Rozyyev, S.; Balabhadrapatruni, M.; Saruwatari, M.S.; Daristotle, J.L.; Ayyub, O.B.; Sandler, A.D.; Kofinas, P. Sprayable tissue adhesive with biodegradation tuned for prevention of postoperative abdominal adhesions. Bioeng. Transl. Med. 2022, 8, e10335. [Google Scholar] [CrossRef]
- Audebert, A.; Darai, E.; Bénifla, J.L.; Yazbeck, C.; Déchaud, H.; Wattiez, A.; Crowe, A.; Pouly, J.L. Postoperative abdominal adhesions and their prevention in gynaecological surgery: I. What should you know? Gynecol. Obstet. Fertil. 2012, 40, 365–370. [Google Scholar] [CrossRef] [PubMed]
- Carranco, R.C.; Zomer, M.T.; Berg, C.F.; Smith, A.V.; Koninckx, P.; Kondo, W. Peritoneal Retraction Pocket Defects and Their Important Relationship with Pelvic Pain and Endometriosis. J. Minim. Invasive Gynecol. 2021, 28, 168–169. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, W.V.B.; Blanco, C.R.; Politti, F.; de Cordoba Lanza, F.; Lucareli, P.R.G.; Corrêa, J.C.F. The effect of a six-week osteopathic visceral manipulation in patients with non-specific chronic low back pain and functional constipation: Study protocol for a randomized controlled trial. Trials 2018, 19, 151. [Google Scholar] [CrossRef]
- Stone, C.; Redakcja Szkolinicki, M. Osteopatia Wisceralna i Położnicza; MedPharm: Wrocław, Poland, 2021; pp. 219–230. [Google Scholar]
- Yang, C.; Du, Y.K.; Wu, J.B.; Wang, J.; Luan, P.; Yang, Q.L.; Yuan, L. Fascia and Primo Vascular System. Evid. Based Complement. Altern. Med. 2015, 2015, 303769. [Google Scholar] [CrossRef]
- Wójcik, M.; Szczepaniak, R.; Placek, K. Physiotherapy Management in Endometriosis. Int. J. Environ. Res. Public Health 2022, 19, 16148. [Google Scholar] [CrossRef] [PubMed]
- Horton, R.C. The Anatomy, Biological Plausibility and Efficacy of Visceral Mobilization in the Treatment of Pelvic Floor Dysfunction. J. Pelvic Obstet. Gynaecol. Physiother. 2015, 117, 5–18. [Google Scholar]
- Della Corte, L.; Di Filippo, C.; Gabrielli, O.; Reppuccia, S.; La Rosa, V.L.; Ragusa, R.; Fichera, M.; Commodari, E.; Bifulco, G.; Giampaolino, P. The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int. J. Environ. Res. Public Health 2020, 17, 4683. [Google Scholar] [CrossRef]
- Lawson, S.; Sacks, A. Pelvic Floor Physical Therapy and Women’s Health Promotion. J. Midwifery Womens Health 2018, 63, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Wójcik, M.; Placek, K. Application Physiotherapy and Balneoclimatology in Gynaecology. Acta Balneol. 2023, 65, 253–262. [Google Scholar] [CrossRef]
- Koninckx, P.R.; Fernandes, R.; Ussia, A.; Schindler, L.; Wattiez, A.; Al-Suwaidi, S.; Amro, B.; Al-Maamari, B.; Hakim, Z.; Tahlak, M. Pathogenesis Based Diagnosis and Treatment of Endometriosis. Front. Endocrinol. 2021, 12, 745548. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Holtz, D.N.; Schmidt, N.; Kolipaka, S.; Hata, E.; Sutton, M.; Znayenko-Miller, T.; Hazen, N.D.; Cobb, C.; Kahleova, H. Nutrition in the prevention and treatment of endometriosis: A review. Front. Nutr. 2023, 10, 1089891. [Google Scholar] [CrossRef] [PubMed]
- Bø, K.; Anglès-Acedo, S.; Batra, A.; Brækken, I.H.; Chan, Y.L.; Jorge, C.H.; Kruger, J.; Yadav, M.; Dumoulin, C. Are hypopressive and other exercise programs effective for the treatment of pelvic organ prolapse? Int. Urogynecol. J. 2023, 34, 43–52. [Google Scholar] [CrossRef]
- Espiño-Albela, A.; Castaño-García, C.; Díaz-Mohedo, E.; Ibáñez-Vera, A.J. Effects of Pelvic-Floor Muscle Training in Patients with Pelvic Organ Prolapse Approached with Surgery vs. Conservative Treatment: A Systematic Review. J. Pers. Med. 2022, 12, 806. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Hernández, M.; López-Fando, L.; Sánchez-Guerrero, C.; Sánchez-González, Á.; Artiles-Medina, A.; Santiago-González, M.; Jiménez-Cidre, M.Á.; Burgos-Revilla, F.J. Combined laparoscopic surgery for the treatment of pelvic organ prolapse and recurrent urinary incontinence. Actas Urol. Esp. 2021, 45, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, B. The Five Diaphragms In Osteopathic Manipulative Medicine: Neurological Relationships, Part 1. Cureus 2020, 12, e8697. [Google Scholar]
- Konstantinidou, E.; Sakalis, V.; Kalaitzi, M.; Charalampous, I.; Konstantinos-Vaios, M.; Themistoklis, M.; Hatzichristou, D.; Apostolidis, A. The role of abdominal muscle training in combination with pelvic floor muscle training to treat female urinary incontinence—A pilot 12-week study. Cent. Eur. J. Urol. 2024, 77, 218–224. [Google Scholar] [CrossRef]
- Awad, E.; Ahmed, H.; Yousef, A.; Abbas, R. Efficacy Of Exercise On Pelvic Pain And Posture Associated With Endometriosis: Within Subject Design. J. Phys. Ther. Sci. 2017, 29, 2112–2115. [Google Scholar] [CrossRef] [PubMed]
- Goyal, K.; Goyal, M.; Narkeesh, K.; Samuel, A.J.; Sharma, S.; Chatterjee, S.; Arumugam, N. The effectiveness of osteopathic manipulative treatment in an abnormal uterine bleeding related pain and health related quality of life (HR-QoL)—A case report. J. Bodyw. Mov. Ther. 2017, 21, 569–573. [Google Scholar] [CrossRef]
- Sillem, M.; Juhasz-Böss, I.; Klausmeier, I.; Mechsner, S.; Siedentopf, F.; Solomayer, E. Osteopathy for Endometriosis and Chronic Pelvic Pain—A Pilot Study. Geburtshilfe Frauenheilkd 2016, 76, 960–963. [Google Scholar] [CrossRef] [PubMed]
- Ott, S. Osteopathische Ansätze bei Endometriose. Osteopat. Med. 2017, 18, 4–9. [Google Scholar] [CrossRef]
- Daraï, C.; Bendifallah, S.; Foulot, H.; Ballester, M.; Chabbert-Buffet, N.; Daraï, E. Intérêt clinique du traitement ostéopathique chezles patientes ayant une endométriose colorectale: Classification fondée sur les symptômes et la qualité de vie. Gynécologie Obs. Fertil. Sénologie 2017, 45, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Daraï, C.; Deboute, O.; Zacharopoulou, C.; Laas, E.; Canlorbe, G.; Belghiti, J.; Zilberman, S.; Ballester, M.; Daraï, E. Impact of osteopathic manipulative therapy on quality of life of patients with deep infiltrating endometriosis with colorectal involvement: Results of a pilot study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 188, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Liem, T.; Dobler, T.K.; Puylaert, M. Redaktor Wydania I Polskiego Majchrzycki M. Przewodnik po Osteopatii Wisceralnej; MedPharm Polska: Wrocław, Poland, 2017; pp. 499, 502, 504, 535, 536, 539, 658. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 12 November 2024).
- Available online: https://www.who.int/tools/whoqol/whoqol-bref (accessed on 27 December 2024).
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256. [Google Scholar] [CrossRef]
- Wang, B.; Chen, Y.; Zhu, X.; Wang, T.; Li, M.; Huang, Y.; Xue, L.; Zhu, Q.; Gao, X.; Wu, M. Global burden and trends of pelvic organ prolapse associated with aging women: An observational trend study from 1990 to 2019. Front. Public Health 2022, 10, 975829. [Google Scholar] [CrossRef]
- Tamburella, F.; Piras, F.; Piras, F.; Spanò, B.; Tramontano, M.; Gili, T. Cerebral Perfusion Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Front. Physiol. 2019, 10, 403. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Cerritelli, F.; Piras, F.; Spanò, B.; Tamburella, F.; Piras, F.; Caltagirone, C.; Gili, T. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020, 10, 969. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, F.; Chiacchiaretta, P.; Gambi, F.; Perrucci, M.G.; Barassi, G.; Visciano, C.; Bellomo, R.G.; Saggini, R.; Ferretti, A. Effect of manual approaches with osteopathic modality on brain correlates of interoception: An fMRI study. Sci. Rep. 2020, 10, 3214. [Google Scholar] [CrossRef] [PubMed]
- Ponzo, V.; Cinnera, A.M.; Mommo, F.; Caltagirone, C.; Koch, G.; Tramontano, M. Osteopathic Manipulative Therapy Potentiates Motor Cortical Plasticity. J. Am. Osteopat. Assoc. 2018, 118, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Gershon, M.D.; Margolis, K.G. The gut, its microbiome, and the brain: Connections and communications. J. Clin. Investig. 2021, 131, e143768. [Google Scholar] [CrossRef] [PubMed]
- Brookes, S.; Chen, N.; Humenick, A.; Spencer, N.J.; Costa, M. Extrinsic sensory innervation of the gut: Structure and function. Adv. Exp. Med. Biol. 2016, 891, 63–69. [Google Scholar]
- Beal, M.C. Viscerosomatic reflexes: A review. J. Am. Osteopath. Assoc. 1985, 85, 53–68. [Google Scholar] [CrossRef]
- Bath, M.; Owens, J. Physiology, Viscerosomatic Reflexes. Available online: https://www.ncbi.nlm.nih.gov/sites/books/NBK559218/ (accessed on 27 December 2024).
- De Marco, M.; Arbieto, E.R.; Da Roza, T.H.; Resende, A.P.; Santos, G.M. Effects of visceral manipulation associated with pelvic floor muscles training in women with urinary incontinence: A randomized controlled trial. Neurourol. Urodyn. 2022, 41, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Yosri, M.M.; Hamada, H.A.; Yousef, A.M. Effect of visceral manipulation on menstrual complaints in women with polycystic ovarian syndrome. J. Osteopath. Med. 2022, 122, 411–422. [Google Scholar] [CrossRef] [PubMed]
- Lagrange, A.; Decoux, D.; Briot, N.; Hennequin, A.; Coudert, B.; Desmoulins, I.; Bertaut, A. Visceral osteopathic manipulative treatment reduces patient reported digestive toxicities induced by adjuvant chemotherapy in breast cancer: A randomized controlled clinical study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 241, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Tamer, S.; Öz, M.; Ülger, Ö. The effect of visceral osteopathic manual therapy applications on pain, quality of life and function in patients with chronic nonspecific low back pain. J. Back Musculoskelet. Rehabil. 2017, 30, 419–425. [Google Scholar] [CrossRef]
- Panagopoulos, J.; Hancock, M.J.; Ferreira, P.; Hush, J.; Petocz, P. Does the addition of visceral manipulation alter outcomes for patients with low back pain? A randomized placebo controlled trial. Eur. J. Pain 2015, 19, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Eguaras, N.; Rodríguez-López, E.S.; Lopez-Dicastillo, O.; Franco-Sierra, M.Á.; Ricard, F.; Oliva-Pascual-Vaca, Á. Effects of Osteopathic Visceral Treatment in Patients with Gastroesophageal Reflux: A Randomized Controlled Trial. J. Clin. Med. 2019, 8, 1738. [Google Scholar] [CrossRef]
- Neto, H.P.; Borges, R.A. Visceral mobilization and functional constipation in stroke survivors: A randomized, controlled, double-blind, clinical trial. Cureus 2020, 12, e8058. [Google Scholar]
- Abd El-Azeim, A.S.; Mahmoud, A.G.; Mohamed, M.T.; El-Khateeb, Y.S. Impact of adding scapular stabilization to postural correctional exercises on symptomatic forward head posture: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2022, 58, 757–766. [Google Scholar] [CrossRef]
- Lin, G.; Zhao, X.; Wang, W.; Wilkinson, T. The relationship between forward head posture, postural control and gait: A systematic review. Gait Posture 2022, 98, 316–329. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Zeng, M.; Cui, Y.; Fu, J.; Li, Y.; Yao, Y.; Shen, F.; Sun, Y.; Wang, Z.; Deng, D. Aquatic strength training improves postural stability and walking function in stroke patients. Physiother. Theory Pract. 2023, 39, 1626–1635. [Google Scholar] [CrossRef] [PubMed]
- Goffredo, M.; Baglio, F.; DE Icco, R.; Proietti, S.; Maggioni, G.; Turolla, A.; Pournajaf, S.; Jonsdottir, J.; Zeni, F.; Federico, S.; et al. Efficacy of non-immersive virtual reality-based telerehabilitation on postural stability in Parkinson’s disease: A multicenter randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2023, 59, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Gorji, S.M.; Samakosh, H.M.N.; Watt, P.; Marchetti, H.P.; Oliveira, R. Pain Neuroscience Education and Motor Control Exercises versus Core Stability Exercises on Pain, Disability, and Balance in Women with Chronic Low Back Pain. Int. J. Environ. Res. Public Health 2022, 19, 2694. [Google Scholar] [CrossRef] [PubMed]
- Kienberger, Y.; Sassmann, R.; Rieder, F.; Johansson, T.; Kässmann, H.; Pirich, C.; Wicker, A.; Niebauer, J. Effects of whole body vibration in postmenopausal osteopenic women on bone mineral density, muscle strength, postural control and quality of life: The T-bone randomized trial. Eur. J. Appl. Physiol. 2022, 122, 2331–2342. [Google Scholar] [CrossRef] [PubMed]
- Reinmann, A.; Bruyneel, A.V.; Gligorov, J.; Mesure, S.; Combescure, C.; Koessler, T.; Bodmer, A. Influence of chemotherapy on postural control and quality of life in women with gynaecological cancer: A protocol of a prospective observational study. BMJ Open 2022, 12, e061664. [Google Scholar] [CrossRef]
- Bula, A.; Tatar, K.; Wysocka, R.; Chyrek, K.; Piejko, L.; Nawrat-Szołtysik, A.; Polak, A. Effect of Physical Activity on Static and Dynamic Postural Balance in Women Treated for Breast Cancer: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 3722. [Google Scholar] [CrossRef]
- Buscemi, A.; Cannatella, M.; Lutrario, P.; Rapisarda, A.; Di Gregorio, G.; Coco, M. Effects of Osteopathic Treatment on Postural Equilibrium Evaluated through a Stabilometric Platform: A Randomized and Controlled Study. J. Funct. Morphol. Kinesiol. 2017, 2, 18. [Google Scholar] [CrossRef]
- Park, J.Y.; Cho, B.W.; Kwon, H.M.; Park, K.K.; Lee, W.S. Knee Extension Is Related to the Posteriorly Deviated Gravity Line to the Pelvis in Young Adults: Radiographic Analysis Using Low-Dose Biplanar X-ray. Yonsei Med. J. 2022, 63, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.; Gaboury, I. Osteopathic empirical research: A bibliometric analysis from 1966 to 2018. BMC Complement. Med. Ther. 2021, 21, 196. [Google Scholar] [CrossRef]
- Baroni, F.; Ruffini, N.; D’Alessandro, G.; Consorti, G.; Lunghi, C. The role of touch in osteopathic practice: A narrative review and integrative hypothesis. Complement. Ther. Clin. Pract. 2021, 42, 101277. [Google Scholar] [CrossRef]
- Consorti, G.; Castagna, C.; Tramontano, M.; Longobardi, M.; Castagna, P.; Di Lernia, D.; Lunghi, C. Reconceptualizing Somatic Dysfunction in the Light of a Neuroaesthetic Enactive Paradigm. Healthcare 2023, 11, 479. [Google Scholar] [CrossRef] [PubMed]
- Bicalho, E.; Vieira, L.; Makita, D.K.; Rivas, L. Inhibitory Tests as Assessment Tools for Somatic Dysfunctions: Mechanisms and Practical Applications. Cureus 2020, 12, e7700. [Google Scholar] [CrossRef] [PubMed]
- Castagna, C.; Consorti, G.; Turinetto, M.; Lunghi, C. Osteopathic Models Integration Radar Plot: A Proposed Framework for Osteopathic Diagnostic Clinical Reasoning. J. Chiropr. Humanit. 2021, 28, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Lunghi, C.; Baroni, F. Cynefin Framework for Evidence-Informed Clinical Reasoning and Decision-Making. J. Osteopath. Med. 2019, 119, 312. [Google Scholar] [CrossRef]
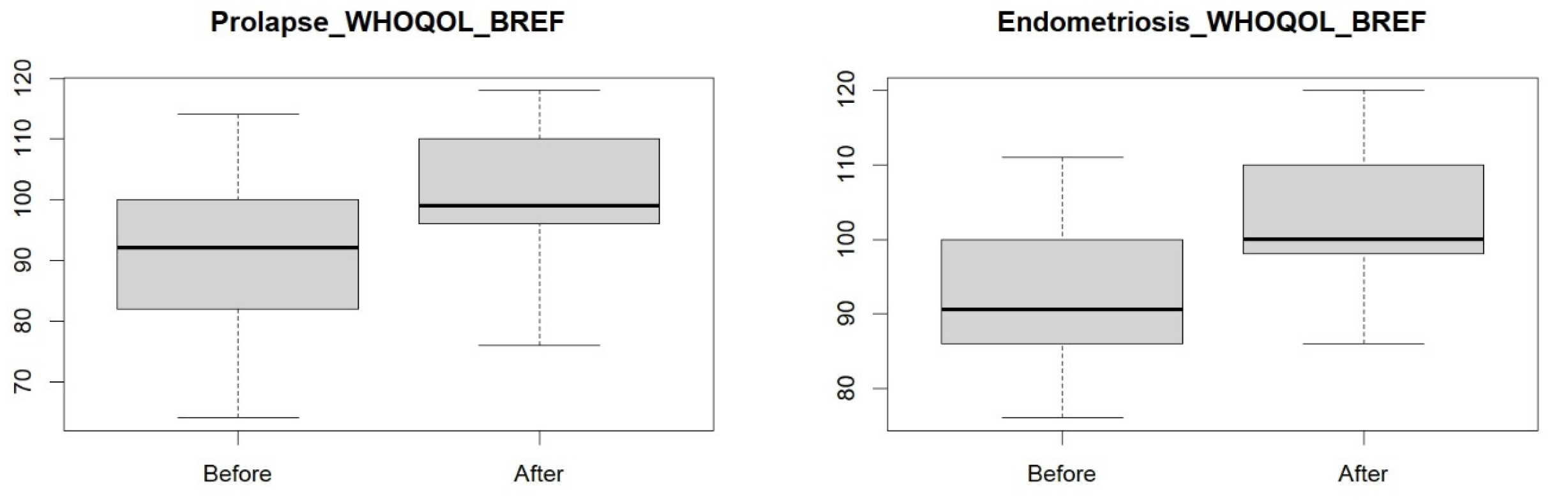
| Group | p-Value |
|---|---|
| endometriosis WHOQOL BREF | 0.0001 |
| pelvic organ prolapse WHOQOL BREF | 0.0093 |
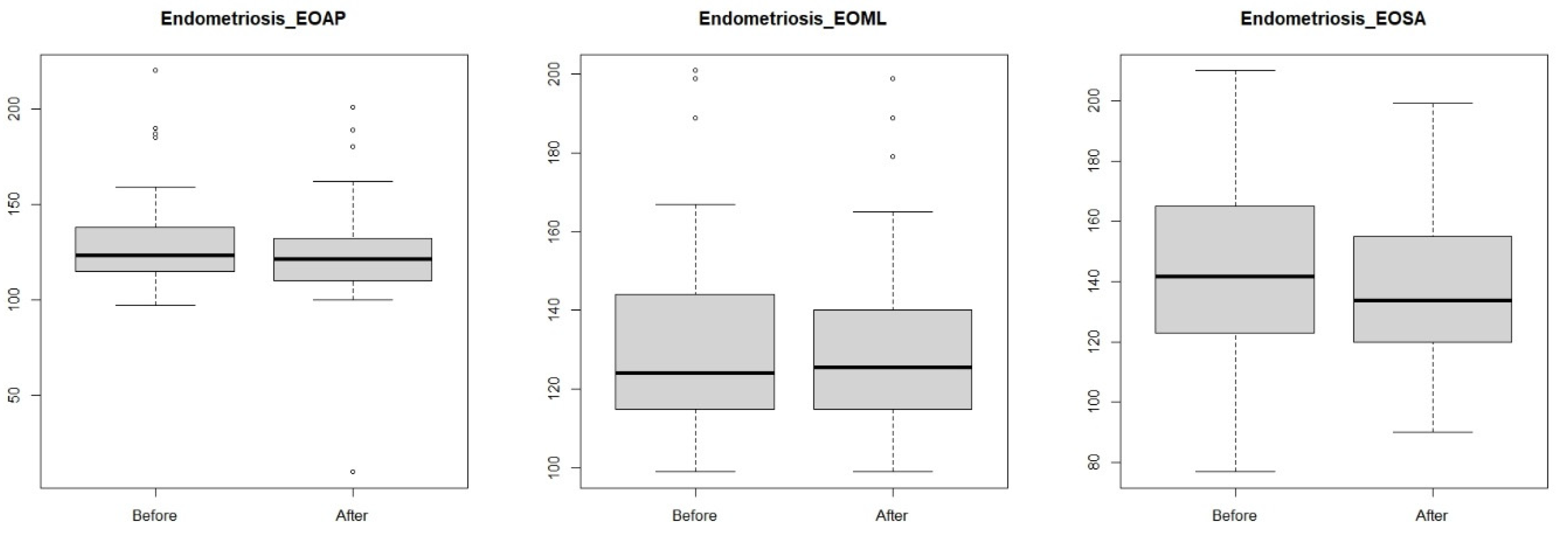
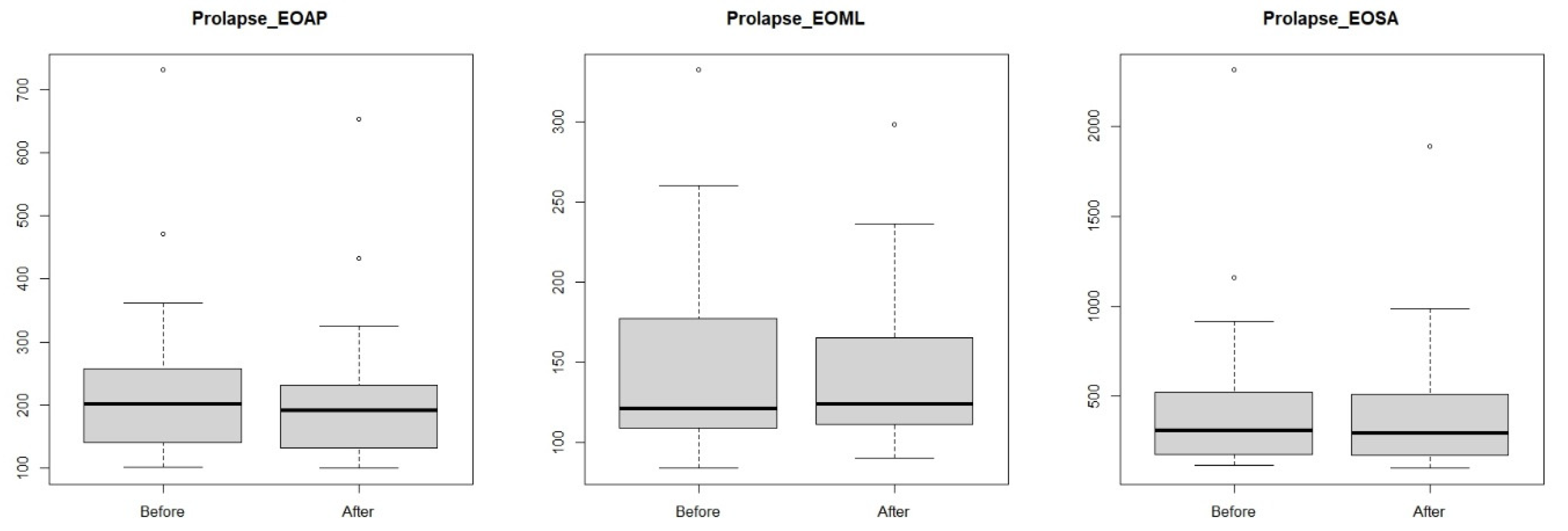
| Group | p-Value |
|---|---|
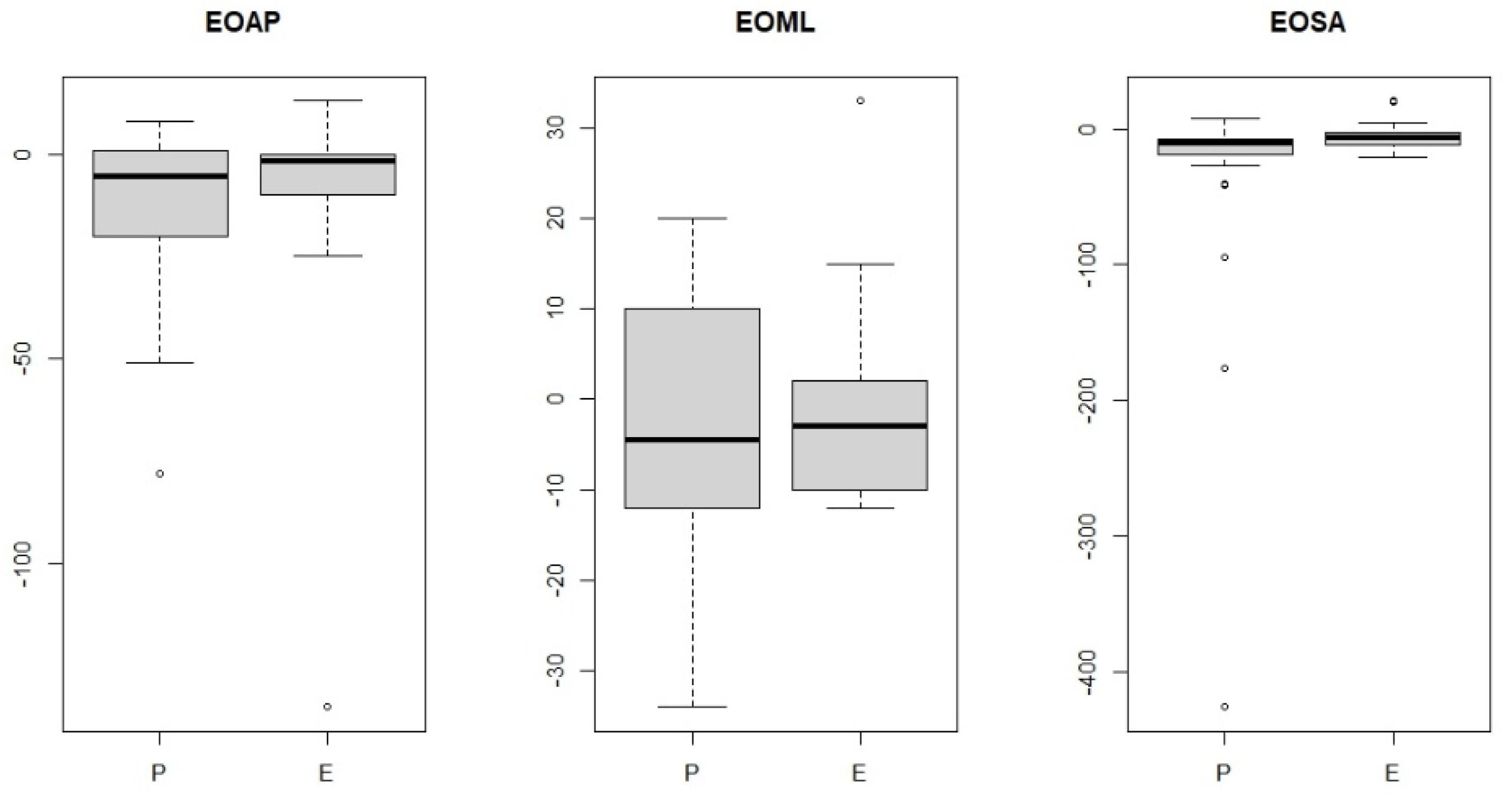
| endomertiosis EOAP | 0.4158 |
| endometriosis EOML | 0.9234 |
| endometriosis EOSA | 0.3827 |
| pelvic organ prolapse EOAP | 0.6152 |
| pelvic organ prolapse EOML | 0.9117 |
| pelvic organ prolapse EOSA | 0.6843 |
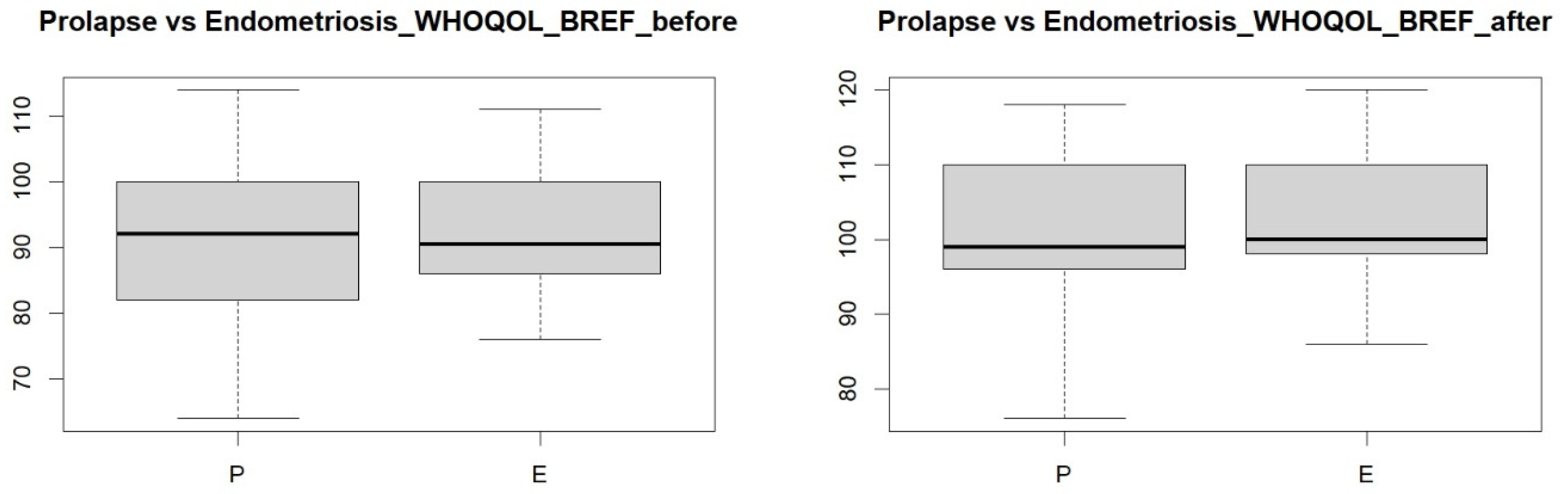
| Group | p-Value |
|---|---|
| endometriosis vs. pelvic organ prolapse EOAP | 0.558 |
| endometriosis vs. pelvic organ prolapse EOML | 0.5385 |
| endometriosis vs. pelvic organ prolapse EOSA | 0.0221 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wójcik, M.; Kampioni, M.; Hudáková, Z.; Siatkowski, I.; Kędzia, W.; Jarząbek-Bielecka, G. The Effect of Osteopathic Visceral Manipulation on Quality of Life and Postural Stability in Women with Endometriosis and Women with Pelvic Organ Prolapse: A Non-Controlled Before–After Clinical Study. J. Clin. Med. 2025, 14, 767. https://doi.org/10.3390/jcm14030767
Wójcik M, Kampioni M, Hudáková Z, Siatkowski I, Kędzia W, Jarząbek-Bielecka G. The Effect of Osteopathic Visceral Manipulation on Quality of Life and Postural Stability in Women with Endometriosis and Women with Pelvic Organ Prolapse: A Non-Controlled Before–After Clinical Study. Journal of Clinical Medicine. 2025; 14(3):767. https://doi.org/10.3390/jcm14030767
Chicago/Turabian StyleWójcik, Małgorzata, Małgorzata Kampioni, Zuzana Hudáková, Idzi Siatkowski, Witold Kędzia, and Grażyna Jarząbek-Bielecka. 2025. "The Effect of Osteopathic Visceral Manipulation on Quality of Life and Postural Stability in Women with Endometriosis and Women with Pelvic Organ Prolapse: A Non-Controlled Before–After Clinical Study" Journal of Clinical Medicine 14, no. 3: 767. https://doi.org/10.3390/jcm14030767
APA StyleWójcik, M., Kampioni, M., Hudáková, Z., Siatkowski, I., Kędzia, W., & Jarząbek-Bielecka, G. (2025). The Effect of Osteopathic Visceral Manipulation on Quality of Life and Postural Stability in Women with Endometriosis and Women with Pelvic Organ Prolapse: A Non-Controlled Before–After Clinical Study. Journal of Clinical Medicine, 14(3), 767. https://doi.org/10.3390/jcm14030767









