Sleep Quality and Cognitive Impairments in Children and Adolescents with Post Traumatic Stress Disorder and/or Depressive Symptoms
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Children’s Depression Inventory (CDI)
2.2.2. Neurocognitive Symptomatology Associated with Child Trauma Based on DSM-5 (NeuroTrauma-DSM5)
2.2.3. The Pittsburgh Sleep Quality Index (PSQI)
2.3. Procedure
2.4. Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Downey, C.; Crummy, A. The impact of childhood trauma on children’s wellbeing and adult behavior. Eur. J. Trauma Dissociation 2022, 6, 100237. [Google Scholar] [CrossRef]
- Melamed, D.M.; Botting, J.; Lofthouse, K.; Pass, L.; Meiser-Stedman, R. The relationship between negative self-concept, trauma, and maltreatment in children and adolescents: A meta-analysis. Clin. Child Fam. Psychol. Rev. 2024, 27, 220–234. [Google Scholar] [CrossRef]
- Hart, H.; Lim, L.; Mehta, M.A.; Simmons, A.; Mirza, K.A.H.; Rubia, K. Altered fear processing in adolescents with a history of severe childhood maltreatment: An fMRI study. Psychol. Med. 2018, 48, 1092–1101. [Google Scholar] [CrossRef]
- Jovanovic, T. 6.3 Effects of Trauma Exposure on Fear Inhibition Circuitry in the Developing Brain. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, S309. [Google Scholar] [CrossRef]
- UNICEF. The State of the World’s Children. In The Future of Childhood in a Changing World Statistical Compendium; UNICEF: New York, NY, USA, 2024. [Google Scholar]
- Save the Children. Children in Conflict. Available online: https://data.stopwaronchildren.org (accessed on 19 January 2025).
- Instituto Nacional de Medicina Legal y Ciencias Forenses. Grupo Centro de Referencia Nacional Sobre Violencia-GCERN. Boletín Estadístico de Julio de 2023. Available online: https://www.medicinalegal.gov.co/cifras-estadisticas/boletines-estadisticos-mensuales (accessed on 12 October 2024).
- McLaughlin, K.A.; Lambert, H.K. Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Curr. Opin. Psychol. 2017, 14, 29–34. [Google Scholar] [CrossRef]
- Humphreys, K.L.; LeMoult, J.; Wear, J.G.; Piersiak, H.A.; Lee, A.; Gotlib, I.H. Child maltreatment and depression: A meta-analysis of studies using the Childhood Trauma Questionnaire. Child Abus. Negl. 2020, 102, 104361. [Google Scholar] [CrossRef]
- Barrera-Valencia, M.; Calderón-Delgado, L.; Trejos-Castillo, E.; O’boyle, M. Cognitive profiles of Post-traumatic stress disorder and depression in children and adolescents. Int. J. Clin. Heal. Psychol. 2017, 17, 242–250. [Google Scholar] [CrossRef]
- Panagioti, M.; Gooding, P.A.; Tarrier, N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: The role of comorbid depression. Compr. Psychiatry 2012, 53, 915–930. [Google Scholar] [CrossRef]
- Carrión, V.G.; Weems, C. Neuroscience of Pediatric PTSD; Oxford University Press: Oxford, UK, 2017. [Google Scholar]
- Giannakopoulos, G.; Kolaitis, G. Sleep problems in children and adolescents following traumatic life events. World J. Psychiatry 2021, 11, 27–34. [Google Scholar] [CrossRef]
- Rolling, J.; Rabot, J.; Reynaud, E.; Kolb, O.; Bourgin, P.; Schroder, C.M. Nightmares and sleep disturbances in children with PTSD: A polysomnographic and actigraphy approach evaluation. J. Clin. Med. 2023, 12, 6570. [Google Scholar] [CrossRef]
- Wylie, M.S. The limits of talk. Psychother. Networker 2004, 28, 30–36. [Google Scholar]
- Van der Bij, J.; Den Kelder, R.O.; Montagne, B.; Hagenaars, M.A. Inhibitory control in trauma-exposed youth: A systematic review. Neurosci. Biobehav. Rev. 2020, 118, 451–462. [Google Scholar] [CrossRef] [PubMed]
- Calderon-Delgado, L.; Barrera-Valencia, M.; Noriega, I.; Al-Khalil, K.; Trejos-Castillo, E.; Mosi, J.; Chavez, B.; Galvan, M.; O’Boyle, M. Implicit processing of emotional words by children with Post-Traumatic Stress Disorder: An fMRI investigation. Int. J. Clin. Heal. Psychol. 2020, 20, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Germain, A. Sleep disturbances as the hallmark of PTSD: Where are we now? Am. J. Psychiatry 2013, 170, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Vlemincx, E.; Vantieghem, I.; Dhar, M.; Dong, D.; Vandekerckhove, M. Bottom-up and cognitive top-down emotion regulation: Experiential emotion regulation and cognitive reappraisal on stress relief and follow-up sleep physiology. Int. J. Environ. Res. Public Health 2022, 19, 7621. [Google Scholar] [CrossRef]
- Liu, S.; Ahemaitijiang, N.; Xu, J.; Liu, Y.; Chen, L.; Han, Z.R. Patterns of childhood maltreatment influence sleep quality: The role of emotion regulation. Dev. Psychopathol. 2024, 36, 1388–1398. [Google Scholar] [CrossRef]
- Baum, K.T.; Desai, A.; Field, J.; Miller, L.E.; Rausch, J.; Beebe, D.W. Sleep restriction worsens mood and emotion regulation in adolescents. J. Child Psychol. Psychiatry 2014, 55, 180–190. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; text rev.; American Psychiatric Publishing: Arlington, VA, USA, 2022. [Google Scholar]
- Pfaff, A.; Jud, A.; Schlarb, A. Systematic review on the association between sleep-related hyperarousal and child maltreatment. Sleep Med. 2021, 84, 219–226. [Google Scholar] [CrossRef]
- Harb, F.; Wart, A.G.-V.; Brzezinski, J.; Deroon-Cassini, T.A.; Larson, C.L. Subtypes of childhood maltreatment and posttraumatic stress disorder symptoms in an adult trauma sample: The mechanistic role of sleep. Psychol. Trauma Theory Res. Primary Policy, 2024; online ahead of print. [Google Scholar] [CrossRef]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef]
- Schønning, V.; Sivertsen, B.; Hysing, M.; Dovran, A.; Askeland, K.G. Childhood maltreatment and sleep in children and adolescents: A systematic review and meta-analysis. Sleep Med. Rev. 2022, 63, 101617. [Google Scholar] [CrossRef]
- Kovacs, M. Children’s Depression Inventory; CDI, Manual/Multi-Health Systems Inc.: Toronto, ON, Canada, 1992. [Google Scholar]
- Segura Camacho, S.; Posada Gómez, S.; Ospina, M.L.; Ospina Gómez, H.A. Estandarización del Inventario CDI en niños y adolescente entre 12 y 17 años de edad, del Municipio de Sabaneta del Departamento de Antioquia-Colombia. Int. J. Psychol. Res. 2010, 3, 63–73. [Google Scholar] [CrossRef][Green Version]
- Barrera-Valencia, M.; Calderón-Delgado, L.; Acevedo-Mesa, C.N. Preliminary validation of PTSD scale and cognitive symptoms associated in a sample of children and adolescents. Rev. Suma Psicol. 2025; in press. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Escobar-Córdoba, F.; Eslava-Schmalbach, J. Validación colombiana del índice de calidad de sueño de Pittsburgh. Rev. Neurol. 2005, 40, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Bartholomew, M.E.; Heller, W.; Miller, G.A. Inhibitory control of emotional processing: Theoretical and empirical considerations. Int. J. Psychophysiol. 2021, 163, 5–10. [Google Scholar] [CrossRef]
- Noriega, I.; Trejos-Castillo, E.; Chae, Y.; Calderon-Delgado, L.; Barrera-Valencia, M.; Al-Khalil, K.; O’Boyle, M.W. Emotional memory processing in post-traumatic stress disorder affected Colombian youth. Int. J. Psychol. 2021, 56, 387–393. [Google Scholar] [CrossRef]
- Guassi Moreira, J.F.; McLaughlin, K.A.; Silvers, J.A. Characterizing the network architecture of emotion regulation neurodevelopment. Cereb. Cortex 2021, 31, 4140–4150. [Google Scholar] [CrossRef]
- Messina, I.; Grecucci, A.; Viviani, R. Neurobiological models of emotion regulation: A meta-analysis of neuroimaging studies of acceptance as an emotion regulation strategy. Soc. Cogn. Affect. Neurosci. 2021, 16, 257–267. [Google Scholar] [CrossRef]
- Jenness, J.L.; Peverill, M.; Miller, A.B.; Heleniak, C.; Robertson, M.M.; Sambrook, K.A.; Sheridan, M.A.; McLaughlin, K.A. Alterations in neural circuits underlying emotion regulation following child maltreatment: A mechanism underlying trauma-related psychopathology. Psychol. Med. 2021, 51, 1880–1889. [Google Scholar] [CrossRef]
- Manti, F.; Giovannone, F.; Aceti, F.; Giacchetti, N.; Fioriello, F.; Maugeri, A.; Sogos, C. Unraveling the Relationship between Sleep Problems, Emotional Behavior Disorders, and Stressful Life Events in Preschool Children. J. Clin. Med. 2022, 11, 5419. [Google Scholar] [CrossRef]
- Wamser-Nanney, R.; Chesher, R.E. Trauma characteristics and sleep impairment among trauma-exposed children. Child Abus. Negl. 2018, 76, 469–479. [Google Scholar] [CrossRef]
- Rho, Y.-A.; Sherfey, J.; Vijayan, S. Emotional Memory Processing during REM Sleep with Implications for Post-Traumatic Stress Disorder. J. Neurosci. 2023, 43, 433–446. [Google Scholar] [CrossRef] [PubMed]
- Ten Brink, M.; Dietch, J.R.; Tutek, J.; Suh, S.A.; Gross, J.J.; Manber, R. Sleep and affect: A conceptual review. Sleep Med. Rev. 2022, 65, 101670. [Google Scholar] [CrossRef] [PubMed]
- Messa, R.M.; Benfica, M.A.; Ribeiro, L.F.; Williams, C.M.; Davidson, S.R.; Alves, E.S. The effect of total sleep deprivation on autonomic nervous system and cortisol responses to acute stressors in healthy individuals: A systematic review. Psychoneuroendocrinology 2024, 168, 107114. [Google Scholar] [CrossRef] [PubMed]
- Brewin, C.R.; Atwoli, L.; Bisson, J.I.; Galea, S.; Koenen, K.; Lewis-Fernández, R. Post-traumatic stress disorder: Evolving conceptualization and evidence, and future research directions. World Psychiatry 2025, 24, 52–80. [Google Scholar] [CrossRef]
| Variable | PTSD+ n = 28 | DEP+ n = 15 | PTSD+/DEP+ n = 43 | CONTROLS n = 44 | p-Value (Levene Test) |
|---|---|---|---|---|---|
| Age | 13.3 ± 1.5 | 12.7 ± 1.4 | 13 ± 0.9 | 12.9 ± 1.6 | 0.480 (0.045) |
| Educational level | 7.1 ± 0.8 | 7.1 ± 0.9 | 7.2 ± 0.7 | 6.7 ± 0.9 | 0.06 (0.057) |
| Gender (%) | 0.015 | ||||
| Girls | 78.6 | 93.3 | 93 | 68.2 | |
| Boys | 21.4 | 6.7 | 7 | 31.9 | |
| PTSD | 25.35 ± 13.01 | 3.46 ± 9.84 | 34.67 ± 9.84 | 5.22 ± 7.71 | <0.001 (0.036) |
| Depression | 13.21 ± 3.37 | 23.8 ± 4.41 | 26.74 ± 5.52 | 11.15 ± 3.38 | <0.001 (0.004) |
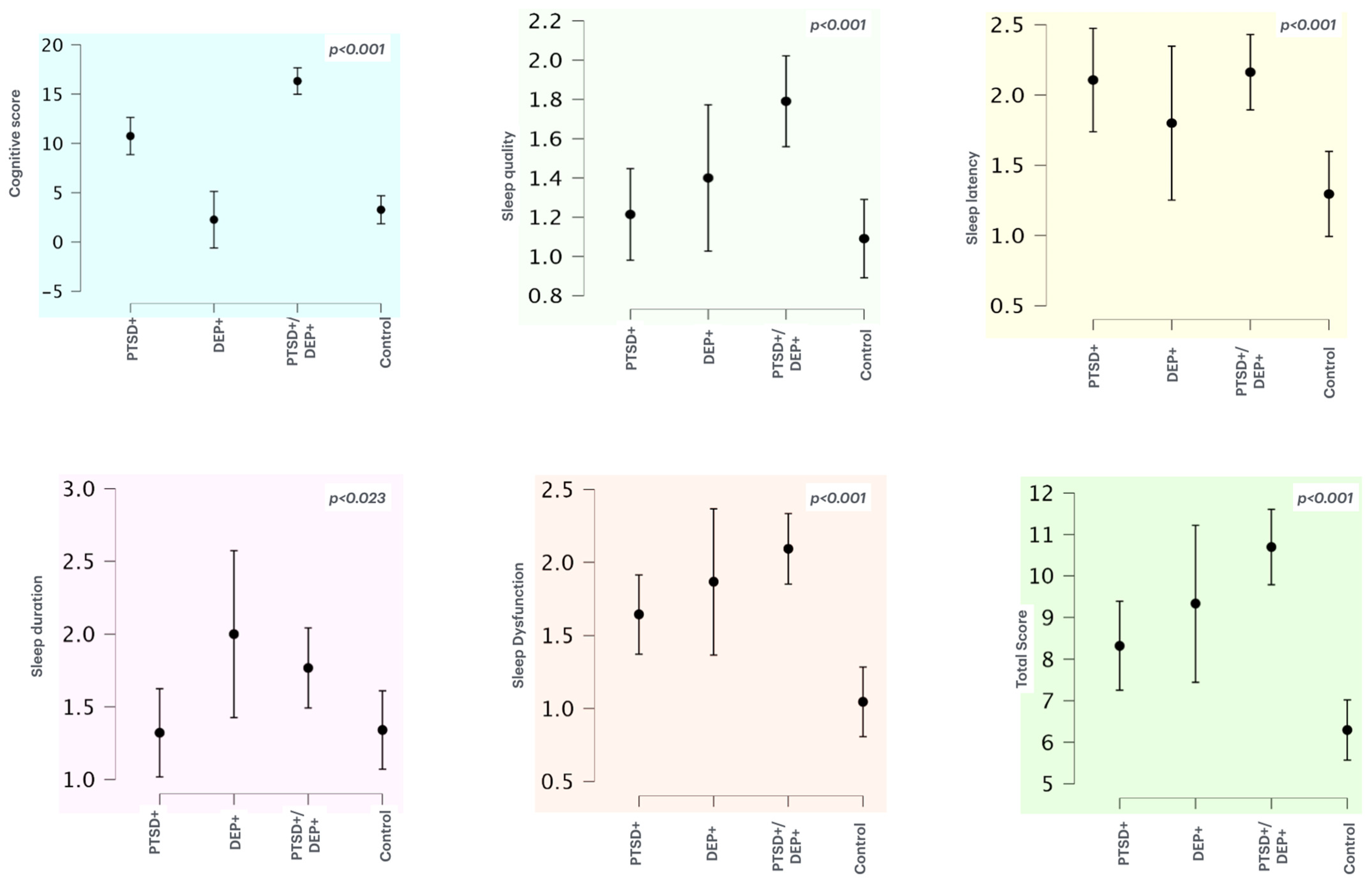
| Variable | Groups | Mean ± SD | F (3, 126) | p | ηp2 |
|---|---|---|---|---|---|
| Cognitive score | PTSD+ | 11.89 ± 5.71 | 63.97 | <0.001 | 0.604 |
| DEP+ | 2.46 ± 6.37 | ||||
| PTSD+/DEP+ | 17.74 ± 4.66 | ||||
| CONTROLS | 3.5 ± 5.22 | ||||
| Sleep quality | PTSD+ | 1.21 ± 0.63 | 7.793 | <0.001 | 0.157 |
| DEP+ | 1.4 ± 0.73 | ||||
| PTSD+/DEP+ | 1.79 ± 0.77 | ||||
| CONTROLS | 1.09 ± 0.67 | ||||
| Sleep latency | PTSD+ | 2.1 ± 0.99 | 6.698 | <0.001 | 0.138 |
| DEP+ | 1.8 ± 1.08 | ||||
| PTSD+/DEP+ | 2.16 ± 0.89 | ||||
| CONTROLS | 1.29 ± 1.02 | ||||
| Sleep duration | PTSD+ | 1.32 ± 0.81 | 3.298 | 0.023 | 0.073 |
| DEP+ | 2.0 ± 1.13 | ||||
| PTSD+/DEP+ | 1.76 ± 0.92 | ||||
| CONTROLS | 1.34 ± 0.92 | ||||
| Sleep efficiency | PTSD+ | 0.21 ± 0.63 | 2.335 | 0.077 | 0.053 |
| DEP+ | 0.4 ± 0.91 | ||||
| PTSD+/DEP+ | 0.41 ± 0.73 | ||||
| CONTROLS | 0.09 ± 0.29 | ||||
| Sleep disturbance | PTSD+ | 1.6 ± 0.62 | 10.24 | 0.196 | 0.196 |
| DEP+ | 1.73 ± 0.79 | ||||
| PTSD+/DEP+ | 2.07 ± 0.59 | ||||
| CONTROLS | 1.34 ± 0.56 | ||||
| Sleep medication | PTSD+ | 0.21 ± 0.63 | 1.964 | 0.0123 | 0.045 |
| DEP+ | 0.13 ± 0.51 | ||||
| PTSD+/DEP+ | 0.39 ± 0.82 | ||||
| CONTROLS | 0.09 ± 0.29 | ||||
| Daytime dysfunction | PTSD+ | 1.64 ± 0.73 | 12.580 | <0.001 | 0.230 |
| DEP+ | 1.86 ± 0.99 | ||||
| PTSD+/DEP+ | 2.09 ± 0.81 | ||||
| CONTROLS | 1.04 ± 0.8 | ||||
| Total Score | PTSD+ | 8.32 ± 2.88 | 16.987 | <0.001 | 0.288 |
| DEP+ | 9.33 ± 3,73 | ||||
| PTSD+/DEP+ | 10.69 ± 3.05 | ||||
| CONTROLS | 6.29 ± 2.45 |
| PSQI | p | ηp2 | PTSD+ DEP+ | PTSD+ PTSD+/DEP+ | PTSD+ Controls | DEP+ PTSD+/DEP+ | DEP+ Controls | PTSD+/DEP+ Controls |
|---|---|---|---|---|---|---|---|---|
| Sleep quality | <0.001 | 0.157 | 0.845 | 0.006 ** | 0.888 | 0.259 | 0.464 | <0.001 *** |
| Sleep latency | <0.001 | 0.138 | 0.764 | 0.996 | 0.005 ** | 0.610 | 0.321 | 0.001 *** |
| Sleep duration | 0.023 | 0.073 | 0.105 | 0.198 | 1.000 | 0.836 | 0.085 | 0.143 |
| Sleep disturbance | <0.001 | 0.196 | 0.920 | 0.013 * | 0.288 | 0.272 | 0.152 | <0.001 *** |
| Daytime dysfunction | <0.001 | 0.230 | 0.826 | 0.110 | 0.015 * | 0.791 | 0.005 | <0.001 *** |
| Total Score | <0.001 | 0.288 | 0.699 | 0.006 ** | 0.024 * | 0.404 | 0.004 ** | <0.001 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrera-Valencia, M.; Calderon-Delgado, L.; Adan, A. Sleep Quality and Cognitive Impairments in Children and Adolescents with Post Traumatic Stress Disorder and/or Depressive Symptoms. J. Clin. Med. 2025, 14, 1010. https://doi.org/10.3390/jcm14031010
Barrera-Valencia M, Calderon-Delgado L, Adan A. Sleep Quality and Cognitive Impairments in Children and Adolescents with Post Traumatic Stress Disorder and/or Depressive Symptoms. Journal of Clinical Medicine. 2025; 14(3):1010. https://doi.org/10.3390/jcm14031010
Chicago/Turabian StyleBarrera-Valencia, Mauricio, Liliana Calderon-Delgado, and Ana Adan. 2025. "Sleep Quality and Cognitive Impairments in Children and Adolescents with Post Traumatic Stress Disorder and/or Depressive Symptoms" Journal of Clinical Medicine 14, no. 3: 1010. https://doi.org/10.3390/jcm14031010
APA StyleBarrera-Valencia, M., Calderon-Delgado, L., & Adan, A. (2025). Sleep Quality and Cognitive Impairments in Children and Adolescents with Post Traumatic Stress Disorder and/or Depressive Symptoms. Journal of Clinical Medicine, 14(3), 1010. https://doi.org/10.3390/jcm14031010







