Ten-Year Outcomes of Patients with Left Main Coronary Artery Disease and Diabetes Mellitus Treated with Percutaneous Coronary Intervention
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Study Definitions
2.3. Study Endpoints and Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Baseline Data
3.2. Clinical Outcome
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ielasi, A.; Chieffo, A. Tools & techniques: Left main coronary artery percutaneous coronary intervention. EuroIntervention 2011, 6, 1020–1021. [Google Scholar] [CrossRef] [PubMed]
- Carson, J.L.; Scholz, P.M.; Chen, A.Y.; Peterson, E.D.; Gold, J.; Schneider, S.H. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J. Am. Coll. Cardiol. 2002, 40, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Angiolillo, D.J.; Kappetein, A.P. Current concepts on coronary revascularization in diabetic patients. Eur. Heart J. 2011, 32, 2748–2757. [Google Scholar] [CrossRef] [PubMed]
- Wit, M.A.; de Mulder, M.; Jansen, E.K.; Umans, V.A. Diabetes mellitus and its impact on long-term outcomes after coronary artery bypass graft surgery. Acta Diabetol. 2013, 50, 123–128. [Google Scholar] [CrossRef]
- Gaba, P.; Sabik, J.F.; Murphy, S.A.; Bellavia, A.; O’Gara, P.T.; Smith, P.K.; Serruys, P.W.; Kappetein, A.P.; Park, S.J.; Park, D.W.; et al. Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting in Patients With Left Main Disease With and Without Diabetes: Findings From a Pooled Analysis of 4 Randomized Clinical Trials. Circulation 2024, 149, 1328–1338. [Google Scholar] [CrossRef]
- Davidson, L.J.; Cleveland, J.C.; Welt, F.G.; Anwaruddin, S.; Bonow, R.O.; Firstenberg, M.S.; Gaudino, M.F.; Gersh, B.J.; Grubb, K.J.; Kirtane, A.J.; et al. A Practical Approach to Left Main Coronary Artery Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2022, 80, 2119–2134. [Google Scholar] [CrossRef]
- Mohammad, M.A.; Persson, J.; Buccheri, S.; Odenstedt, J.; Sarno, G.; Angeras, O.; Volz, S.; Todt, T.; Gotberg, M.; Isma, N.; et al. Trends in Clinical Practice and Outcomes After Percutaneous Coronary Intervention of Unprotected Left Main Coronary Artery. J. Am. Heart Assoc. 2022, 11, e024040. [Google Scholar] [CrossRef]
- Sabatine, M.S.; Bergmark, B.A.; Murphy, S.A.; O’Gara, P.T.; Smith, P.K.; Serruys, P.W.; Kappetein, A.P.; Park, S.J.; Park, D.W.; Christiansen, E.H.; et al. Percutaneous coronary intervention with drug-eluting stents versus coronary artery bypass grafting in left main coronary artery disease: An individual patient data meta-analysis. Lancet 2021, 398, 2247–2257. [Google Scholar] [CrossRef]
- Wang, H.; Wang, H.; Wei, Y.; Li, X.; Jhummun, V.; Ahmed, M.A. Ten-Year Outcomes of Percutaneous Coronary Intervention Versus Coronary Artery Bypass Grafting for Patients with Type 2 Diabetes Mellitus Suffering from Left Main Coronary Disease: A Meta-Analysis. Diabetes Ther. 2021, 12, 1041–1054. [Google Scholar] [CrossRef]
- Lee, K.; Ahn, J.M.; Yoon, Y.H.; Kang, D.Y.; Park, S.Y.; Ko, E.; Park, H.; Cho, S.C.; Park, S.; Kim, T.O.; et al. Long-Term (10-Year) Outcomes of Stenting or Bypass Surgery for Left Main Coronary Artery Disease in Patients With and Without Diabetes Mellitus. J. Am. Heart Assoc. 2020, 9, e015372. [Google Scholar] [CrossRef]
- Disney, L.; Ramaiah, C.; Ramaiah, M.; Keshavamurthy, S. Left Main Coronary Artery Disease in Diabetics: Percutaneous Coronary Intervention or Coronary Artery Bypass Grafting? Int. J. Angiol. 2021, 30, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Kralisz, P.; Dabrowski, E.J.; Dobrzycki, S.; Kozlowska, W.U.; Lipska, P.O.; Nowak, K.; Gugala, K.; Prokopczuk, P.; Mezynski, G.; Swieczkowski, M.; et al. Long-term impact of diabetes on mortality in patients undergoing unprotected left main PCI: A propensity score-matched analysis from the BIA-LM registry. Cardiovasc. Diabetol. 2025, 24, 175. [Google Scholar] [CrossRef] [PubMed]
- Mehilli, J.; Kastrati, A.; Byrne, R.A.; Bruskina, O.; Iijima, R.; Schulz, S.; Pache, J.; Seyfarth, M.; Massberg, S.; Laugwitz, K.L.; et al. Paclitaxel- versus sirolimus-eluting stents for unprotected left main coronary artery disease. J. Am. Coll. Cardiol. 2009, 53, 1760–1768. [Google Scholar] [CrossRef] [PubMed]
- Mehilli, J.; Richardt, G.; Valgimigli, M.; Schulz, S.; Singh, A.; Abdel-Wahab, M.; Tiroch, K.; Pache, J.; Hausleiter, J.; Byrne, R.A.; et al. Zotarolimus- versus everolimus-eluting stents for unprotected left main coronary artery disease. J. Am. Coll. Cardiol. 2013, 62, 2075–2082. [Google Scholar] [CrossRef]
- Sianos, G.; Morel, M.A.; Kappetein, A.P.; Morice, M.C.; Colombo, A.; Dawkins, K.; van den Brand, M.; Van Dyck, N.; Russell, M.E.; Mohr, F.W.; et al. The SYNTAX Score: An angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005, 1, 219–227. [Google Scholar]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Grambsch, P.M.; Therneau, T.M. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994, 81, 515–526. [Google Scholar] [CrossRef]
- Bataille, V.; Ferrieres, J.; Danchin, N.; Puymirat, E.; Zeller, M.; Simon, T.; Carrie, D. Increased mortality risk in diabetic patients discharged from hospital with insulin therapy after an acute myocardial infarction: Data from the FAST-MI 2005 registry. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 218–230. [Google Scholar] [CrossRef]
- Roumeliotis, A.; Siasos, G.; Dangas, G.; Power, D.; Sartori, S.; Vavouranakis, M.; Tsioufis, K.; Leone, P.P.; Vogel, B.; Cao, D.; et al. Significance of diabetes mellitus status in patients undergoing percutaneous left main coronary artery intervention. Catheter. Cardiovasc. Interv. 2024, 104, 723–732. [Google Scholar] [CrossRef]
- Wang, R.; Serruys, P.W.; Gao, C.; Hara, H.; Takahashi, K.; Ono, M.; Kawashima, H.; O’Leary, N.; Holmes, D.R.; Witkowski, A.; et al. Ten-year all-cause death after percutaneous or surgical revascularization in diabetic patients with complex coronary artery disease. Eur. Heart J. 2021, 43, 56–67. [Google Scholar] [CrossRef]
- Herman, M.E.; O’Keefe, J.H.; Bell, D.S.H.; Schwartz, S.S. Insulin Therapy Increases Cardiovascular Risk in Type 2 Diabetes. Prog. Cardiovasc. Dis. 2017, 60, 422–434. [Google Scholar] [CrossRef]
- Nolan, C.J.; Ruderman, N.B.; Prentki, M. Intensive insulin for type 2 diabetes: The risk of causing harm. Lancet Diabetes Endocrinol. 2013, 1, 9–10. [Google Scholar] [CrossRef]
- Chico, A.; Vidal-Rios, P.; Subira, M.; Novials, A. The continuous glucose monitoring system is useful for detecting unrecognized hypoglycemias in patients with type 1 and type 2 diabetes but is not better than frequent capillary glucose measurements for improving metabolic control. Diabetes Care 2003, 26, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Paty, B.W. The Role of Hypoglycemia in Cardiovascular Outcomes in Diabetes. Can. J. Diabetes 2015, 39 (Suppl. 5), S155–S159. [Google Scholar] [CrossRef] [PubMed]
- Dandona, P.; Chaudhuri, A.; Dhindsa, S. Proinflammatory and prothrombotic effects of hypoglycemia. Diabetes Care 2010, 33, 1686–1687. [Google Scholar] [CrossRef] [PubMed]
- Joy, N.G.; Hedrington, M.S.; Briscoe, V.J.; Tate, D.B.; Ertl, A.C.; Davis, S.N. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes Care 2010, 33, 1529–1535. [Google Scholar] [CrossRef]
- Aberer, F.; Pferschy, P.N.; Tripolt, N.J.; Sourij, C.; Obermayer, A.M.; Pruller, F.; Novak, E.; Reitbauer, P.; Kojzar, H.; Prietl, B.; et al. Hypoglycaemia leads to a delayed increase in platelet and coagulation activation markers in people with type 2 diabetes treated with metformin only: Results from a stepwise hypoglycaemic clamp study. Diabetes Obes. Metab. 2020, 22, 212–221. [Google Scholar] [CrossRef]
- Joy, N.G.; Tate, D.B.; Younk, L.M.; Davis, S.N. Effects of Acute and Antecedent Hypoglycemia on Endothelial Function and Markers of Atherothrombotic Balance in Healthy Humans. Diabetes 2015, 64, 2571–2580. [Google Scholar] [CrossRef]
- Wright, R.J.; Frier, B.M. Vascular disease and diabetes: Is hypoglycaemia an aggravating factor? Diabetes Metab. Res. Rev. 2008, 24, 353–363. [Google Scholar] [CrossRef]
- Zoungas, S.; Patel, A.; Chalmers, J.; de Galan, B.E.; Li, Q.; Billot, L.; Woodward, M.; Ninomiya, T.; Neal, B.; MacMahon, S.; et al. Severe hypoglycemia and risks of vascular events and death. N. Engl. J. Med. 2010, 363, 1410–1418. [Google Scholar] [CrossRef]
- Spadafora, L.; Pastena, P.; Cacciatore, S.; Betti, M.; Biondi-Zoccai, G.; D’Ascenzo, F.; De Ferrari, G.M.; De Filippo, O.; Versaci, F.; Sciarretta, S.; et al. One-Year Prognostic Differences and Management Strategies between ST-Elevation and Non-ST-Elevation Myocardial Infarction: Insights from the PRAISE Registry. Am. J. Cardiovasc. Drugs 2025, 25, 681–691. [Google Scholar] [CrossRef]

| Characteristic | Without Diabetes (n = 896) | With Diabetes (n = 361) | p Value | |
|---|---|---|---|---|
| On Oral Antidiabetic Drugs (n = 246) | On Insulin Therapy (n = 115) | |||
| Age (years) | 69.4 [62.1; 76.2] | 70.8 [65.5; 76.9] | 70.4 [65.5; 77.1] | 0.433 |
| Women | 206 (23.0%) | 66 (26.8%) | 29 (25.2%) | 0.433 |
| Body mass index (kg/m2) | 26.2 [24.2; 28.7] | 27.8 [25.2; 30.7] | 28.0 [25.4; 31.6] | <0.001 |
| Arterial hypertension | 592 (66.1%) | 193 (78.5%) | 83 (72.2%) | 0.001 |
| Hypercholesterolemia | 662 (73.9%) | 183 (74.4%) | 91 (79.1%) | 0.478 |
| Current smoking | 113 (12.6%) | 28 (11.4%) | 11 (9.57%) | 0.596 |
| Extent of coronary artery disease | <0.001 | |||
| 2-vessel | 287 (32.0%) | 58 (23.6%) | 14 (12.2%) | |
| 3-vessel | 609 (68.0%) | 188 (76.4%) | 101 (87.8%) | |
| Clinical presentation | 0.051 | |||
| Stable coronary artery disease | 572 (63.8%) | 146 (59.3%) | 61 (53.0%) | |
| Acute coronary syndrome | 324 (36.2%) | 100 (40.7%) | 54 (47.0%) | |
| History of myocardial infarction | 257 (28.7%) | 70 (28.5%) | 31 (27.0%) | 0.928 |
| History of percutaneous coronary intervention | 448 (50.0%) | 125 (50.8%) | 62 (53.9%) | 0.728 |
| Serum creatinine (mg/dl) | 0.95 [0.80; 1.10] | 1.00 [0.81; 1.20] | 1.10 [0.90; 1.46] | <0.001 |
| Glucated hemoglobin A1c (%) | - | 6.67 [5.05; 13.1] | 7.28 [5.32; 14.6] | <0.001 |
| Left ventricular ejection fraction (%) | 58.0 [47.8; 62.0] | 55.5 [41.0; 60.0] | 48.0 [35.0; 60.0] | <0.001 |
| Comorbidities | ||||
| Peripheral artery disease | 70 (7.8%) | 38 (15.4%) | 18 (15.7%) | <0.001 |
| Chronic obstructive pulmonary disease | 20 (2.2%) | 14 (5.7%) | 6 (5.2%) | 0.012 |
| Malignancies | 151 (16.9%) | 43 (17.5%) | 15 (13.0%) | 0.541 |
| Vessel (left main) size (mm) | 3.73 (0.51) | 3.71 (0.52) | 3.69 (0.50) | 0.588 |
| SYNTAX score | 29.0 [21.0; 36.0] | 30.0 [22.0; 38.0] | 32.0 [24.5; 39.5] | 0.014 |
| Second generation drug-eluting stents | 465 (51.9%) | 124 (50.4%) | 61 (53.0%) | 0.877 |
| Characteristic | Without Diabetes (n = 896) | With Diabetes (n = 361) | p Value | |
|---|---|---|---|---|
| On Oral Antidiabetic Drugs (n = 246) | On Insulin Therapy (n = 115) | |||
| Lesion location in the left main coronary artery | 0.240 | |||
| Ostial | 94 (10.5%) | 31 (12.6%) | 20 (17.4%) | |
| Distal | 655 (73.1%) | 172 (69.9%) | 76 (66.1%) | |
| Mid-shaft | 147 (16.4%) | 43 (17.5%) | 19 (16.5%) | |
| Occluded right coronary artery | 103 (11.5%) | 31 (12.6%) | 19 (16.5%) | 0.292 |
| Trifurcation morphology | 108 (12.1%) | 31 (12.6%) | 20 (17.4%) | 0.269 |
| Coronary artery dominance | 0.074 | |||
| Left | 92 (10.3%) | 32 (13.0%) | 8 (7.0%) | |
| Right | 745 (83.1%) | 192 (78.0%) | 93 (80.9%) | |
| Balanced | 59 (6.6%) | 22 (8.9%) | 14 (12.2%) | |
| Stenting technique | 0.293 | |||
| Single | 512 (57.1%) | 137 (55.7%) | 70 (60.9%) | |
| T-stenting | 43 (4.80%) | 6 (2.44%) | 1 (0.87%) | |
| Culotte stenting | 5 (0.56%) | 1 (0.41%) | 1 (0.87%) | |
| Kissing balloon | 336 (37.5%) | 102 (41.5%) | 43 (37.4%) | |
| Final kissing balloon | 389 (43.4%) | 112 (45.5%) | 37 (32.2%) | 0.045 |
| Outcome | Without Diabetes (n = 896) | With Diabetes (n = 361) | Hazard Ratio with 95% Confidence Interval | |||
|---|---|---|---|---|---|---|
| On Oral Antidiabetic Drugs (n = 246) | On Insulin (n = 115) | On Oral Antidiabetic Drugs vs. No Diabetes | On Insulin vs. No Diabetes | On Insulin vs. Oral Antidiabetic Drugs | ||
| All-cause death | 291 (35.7) | 111 (49.5) | 75 (70.0) | 1.57 [1.26–1.96] | 2.80 [2.17–3.61] | 1.78 [1.33–2.39] |
| Cardiac death | 181 (22.6) | 62 (27.9) | 42 (40.1) | 1.44 [1.07–1.92] | 2.65 [1.90–3.70] | 1.85 [1.24–2.74] |
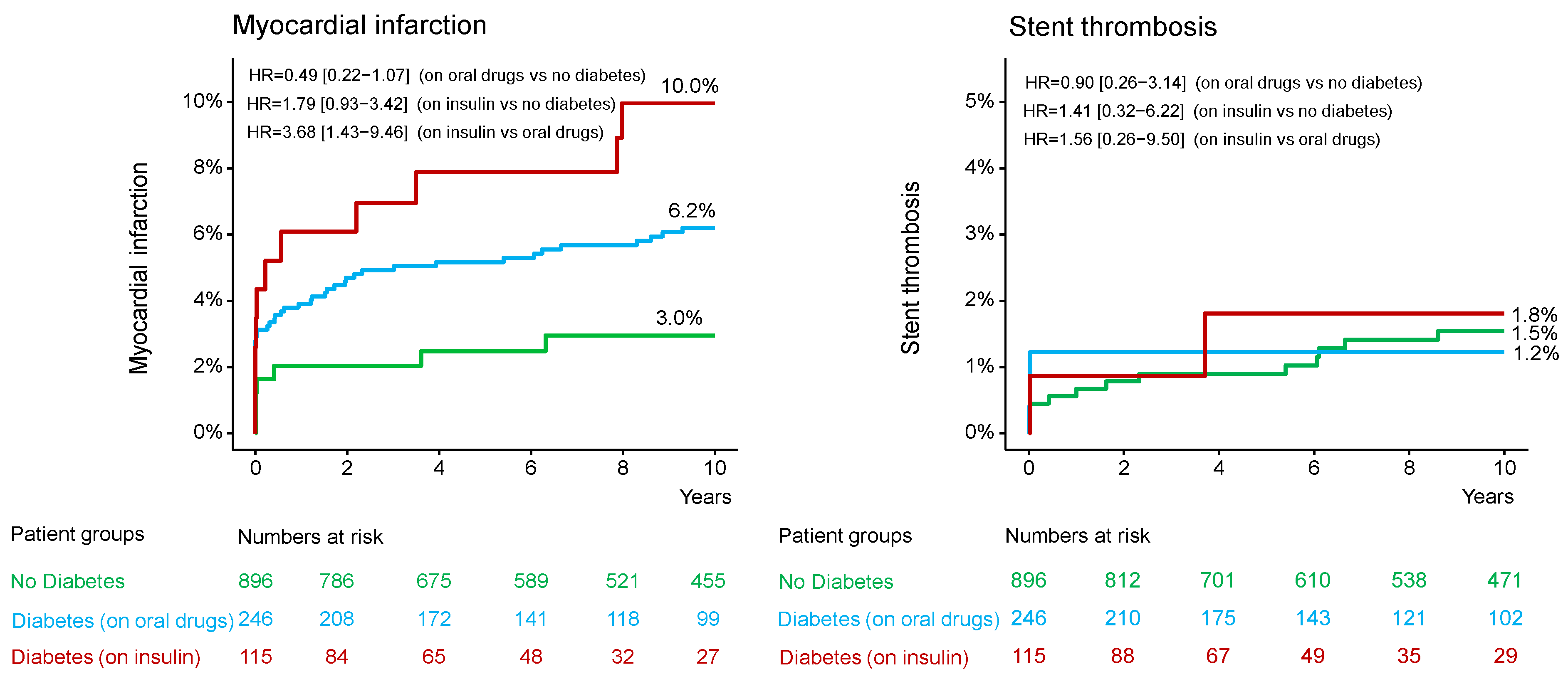
| Myocardial infarction | 54 (6.2) | 7 (3.0) | 11 (10.0) | 0.49 [0.22–1.07] | 1.79 [0.93–3.42] | 3.68 [1.43–9.46] |
| Definite stent thrombosis | 13 (1.5) | 3 (1.2) | 2 (1.8) | 0.90 [0.26–3.14] | 1.41 [0.32–6.22] | 1.56 [0.26–9.50] |
| Coronary artery bypass graft surgery | 23 (2.7) | 5 (2.2) | 2 (1.7) | 0.85 [0.32–2.23] | 0.81 [0.19–3.44] | 0.96 [0.19–4.92] |
| Repeat PCI | 175 (20.6) | 51 (21.8) | 25 (22.1) | 1.15 [0.84–1.57] | 1.36 [0.89–2.08] | 1.18 [0.73–1.91] |
| Target lesion revascularization | 190 (22.3) | 56 (24.0) | 27 (23.8) | 1.16 [0.86–1.56] | 1.34 [0.89–2.01] | 1.15 [0.73–1.83] |
| Stroke | 20 (2.3) | 7 (2.9) | 2 (1.7) | 1.36 [0.58–3.19] | 0.90 [0.21–3.81] | 0.66 [0.14–3.19] |
| Nontarget lesion revascularization | 360 (41.3) | 103 (43.4) | 54 (47.7) | 1.12 [0.90–1.39] | 1.39 [1.05–1.84] | 1.24 [0.90–1.71] |
| Outcome | Adjusted Hazard Ratio with 95% Confidence Interval | ||
|---|---|---|---|
| On Oral Antidiabetic Drugs vs. No Diabetes | On Insulin Therapy vs. No Diabetes | On Insulin Therapy vs. Oral Antidiabetic Drugs | |
| All-cause death | 1.23 [0.98–1.55] * | 2.10 [1.58–2.78] | 1.71 [1.25–2.32] |
| Cardiac death | 1.08 [0.79–1.47] | 1.76 [1.18–2.62] | 1.64 [1.05–2.56] |
| Myocardial infarction | 0.47 [0.21–1.05] | 1.43 [0.67–3.05] | 3.03 [1.09–8.43] |
| Definite stent thrombosis | 0.91 [0.23–3.53] | 1.23 [0.18–8.26] | 1.35 [0.18–10.46] |
| Coronary artery bypass graft surgery | 0.91 [0.33–2.50] | 0.57 [0.12–2.75] | 0.62 [0.12–3.21] |
| Repeat PCI | 1.07 [0.76–1.50] | 1.08 [0.65–1.79] | 1.01 [0.59–1.73] |
| Target lesion revascularization | 1.08 [0.78–1.48] | 1.05 [0.64–1.71] | 0.97 [0.58–1.63] |
| Stroke | 1.35 [0.61–2.97] | 0.91 [0.21–4.00] | 0.67 [0.14–3.18] |
| Nontarget lesion revascularization | 1.14 [0.90–1.43] | 1.34 [0.99–1.82] ** | 1.18 [0.84–1.65] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bresha, J.; Ndrepepa, G.; Kuna, C.; Kessler, T.; Hintz, I.; Justenhoven, P.; Ibrahim, T.; Kufner, S.; Schunkert, H.; Valgimigli, M.; et al. Ten-Year Outcomes of Patients with Left Main Coronary Artery Disease and Diabetes Mellitus Treated with Percutaneous Coronary Intervention. J. Clin. Med. 2025, 14, 8851. https://doi.org/10.3390/jcm14248851
Bresha J, Ndrepepa G, Kuna C, Kessler T, Hintz I, Justenhoven P, Ibrahim T, Kufner S, Schunkert H, Valgimigli M, et al. Ten-Year Outcomes of Patients with Left Main Coronary Artery Disease and Diabetes Mellitus Treated with Percutaneous Coronary Intervention. Journal of Clinical Medicine. 2025; 14(24):8851. https://doi.org/10.3390/jcm14248851
Chicago/Turabian StyleBresha, Jola, Gjin Ndrepepa, Constantin Kuna, Thorsten Kessler, Isabella Hintz, Paul Justenhoven, Tareq Ibrahim, Sebastian Kufner, Heribert Schunkert, Marco Valgimigli, and et al. 2025. "Ten-Year Outcomes of Patients with Left Main Coronary Artery Disease and Diabetes Mellitus Treated with Percutaneous Coronary Intervention" Journal of Clinical Medicine 14, no. 24: 8851. https://doi.org/10.3390/jcm14248851
APA StyleBresha, J., Ndrepepa, G., Kuna, C., Kessler, T., Hintz, I., Justenhoven, P., Ibrahim, T., Kufner, S., Schunkert, H., Valgimigli, M., Richardt, G., Laugwitz, K.-L., Cassese, S., Kastrati, A., & Wiebe, J. (2025). Ten-Year Outcomes of Patients with Left Main Coronary Artery Disease and Diabetes Mellitus Treated with Percutaneous Coronary Intervention. Journal of Clinical Medicine, 14(24), 8851. https://doi.org/10.3390/jcm14248851








