Effects of Task-Oriented Training on Gait Outcomes and Balance in Individuals with Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Data Resource
2.2. Eligibility and Exclusion Criteria
- Patients (P): Patients with a stroke (except where a person without disability acts as a person with disabilities);
- Intervention (I): TOT;
- Comparison (C): Conventional therapy or other rehabilitation interventions;
- Outcome (O): Gait and balance outcomes.
2.3. Screening, Selection, and Extraction Process
2.4. Data Extraction
2.5. Risk of Bias Assessment
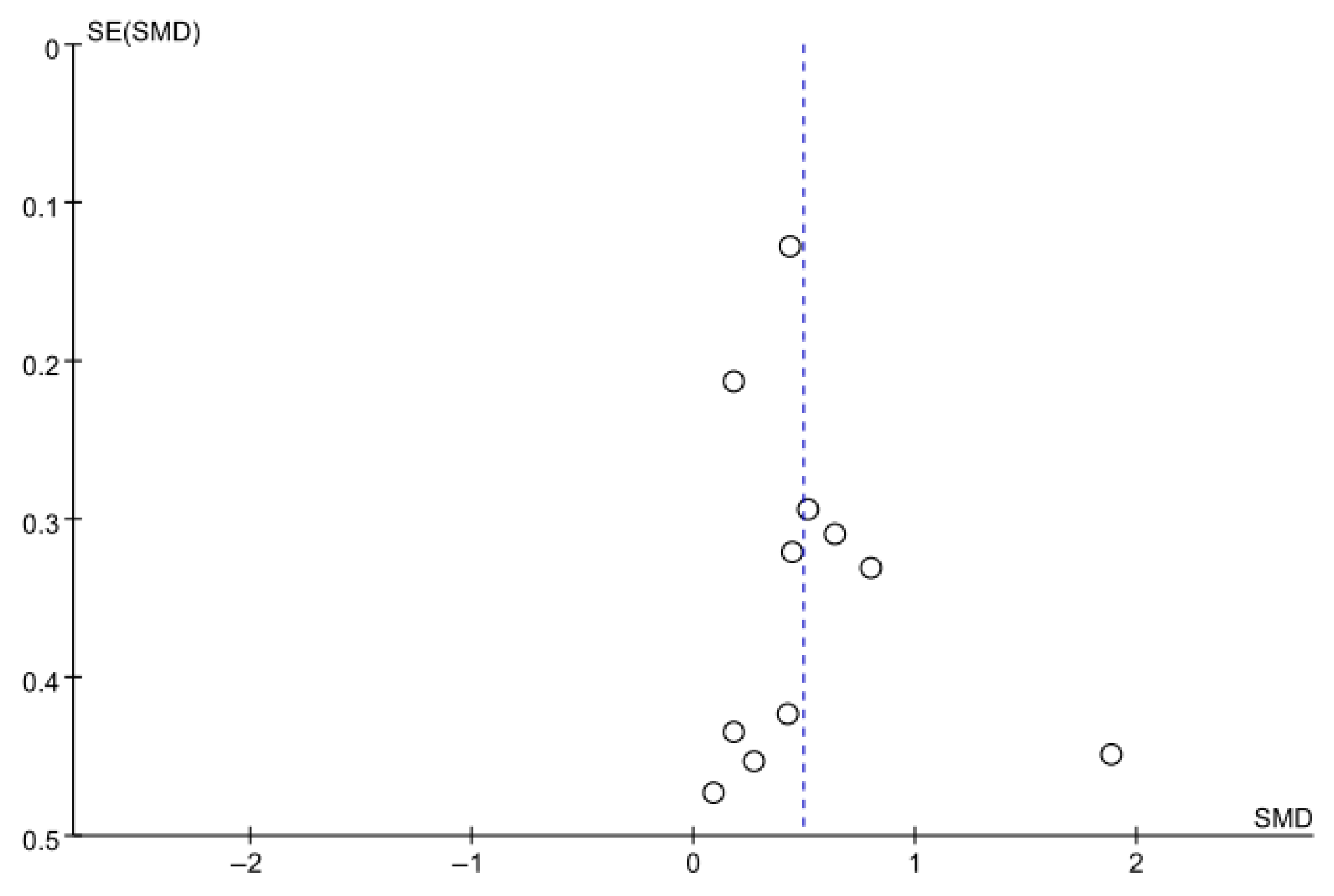
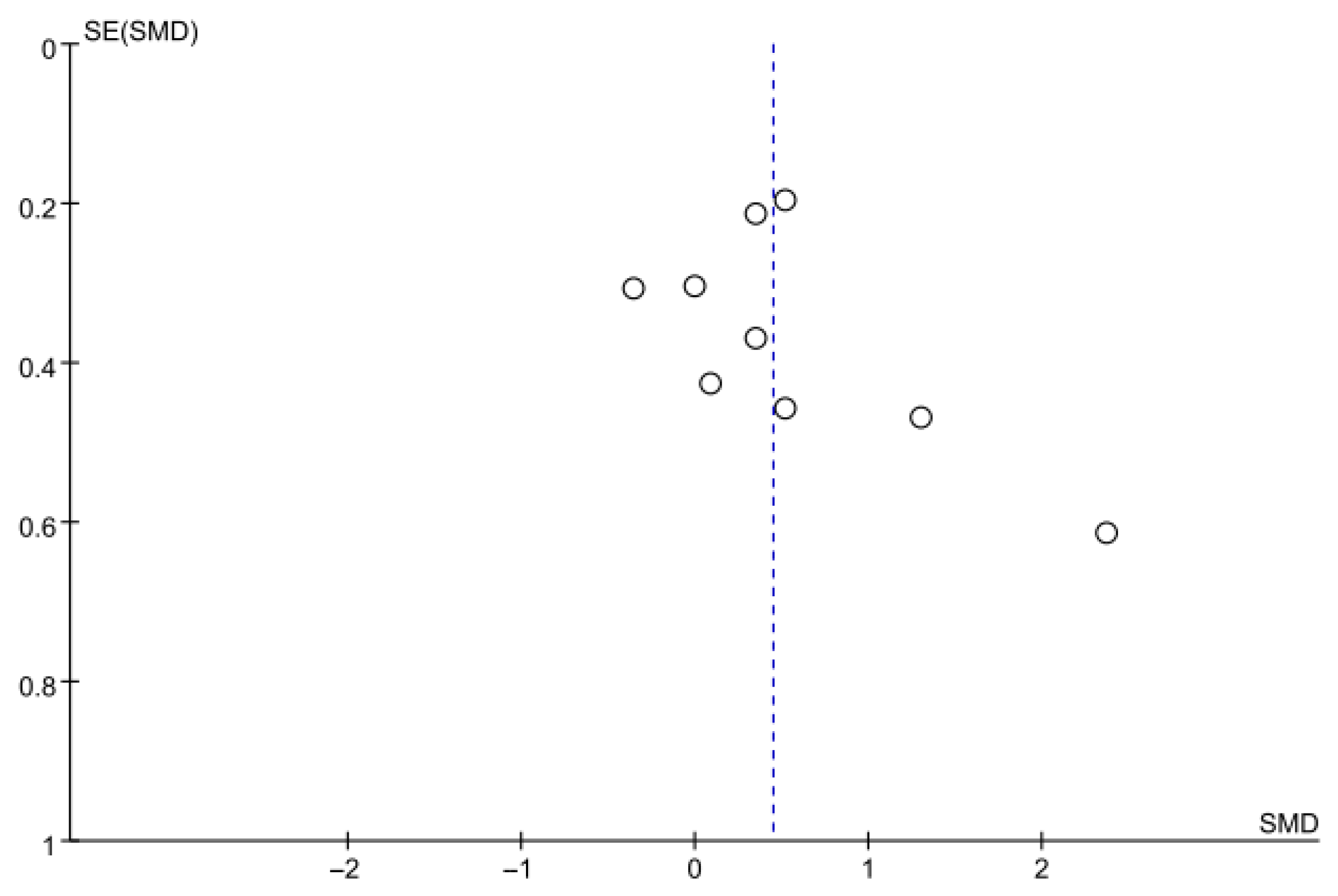
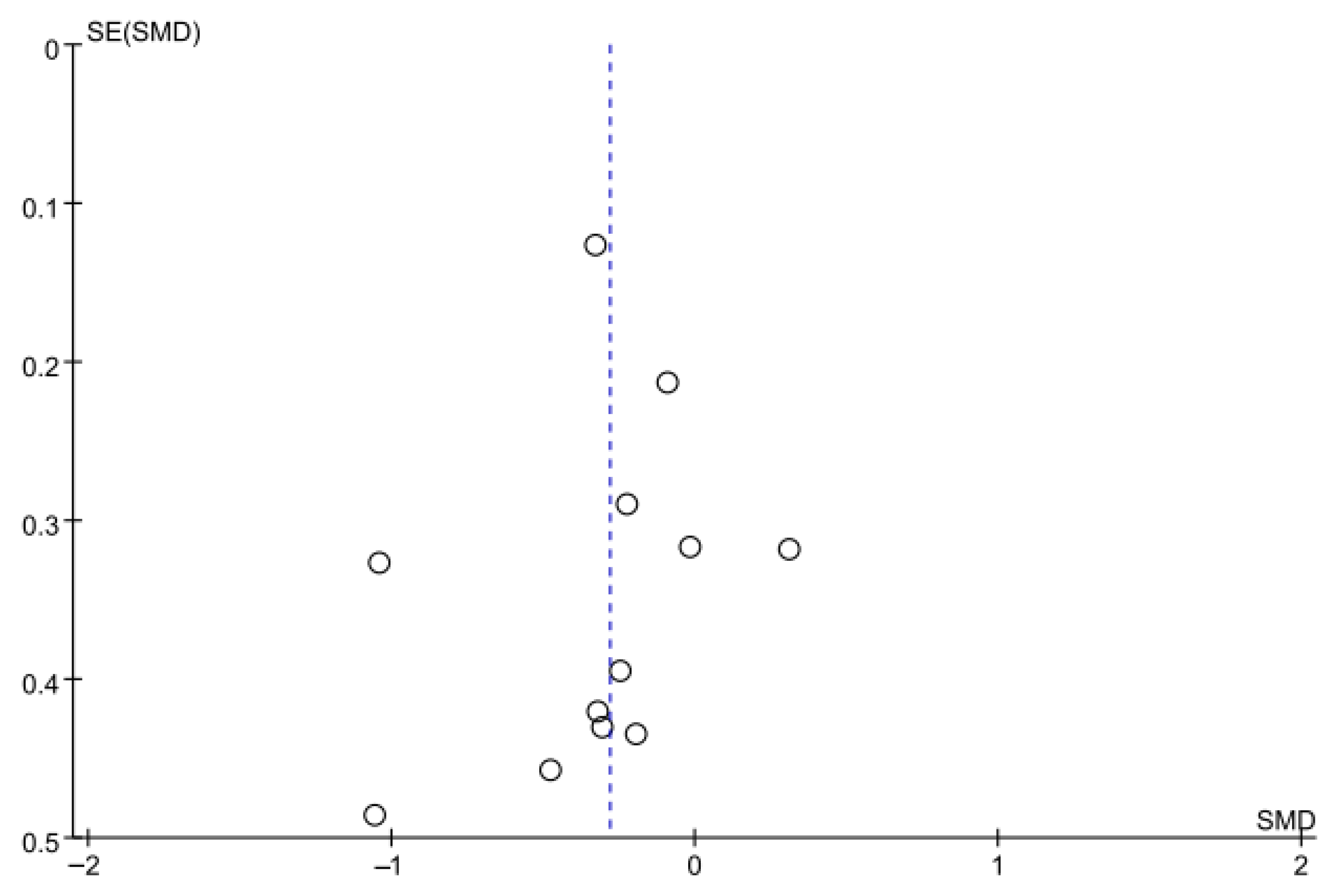
2.6. Reporting Bias Assessment
2.7. Statistical Analysis (Synthesis Methods)
3. Results
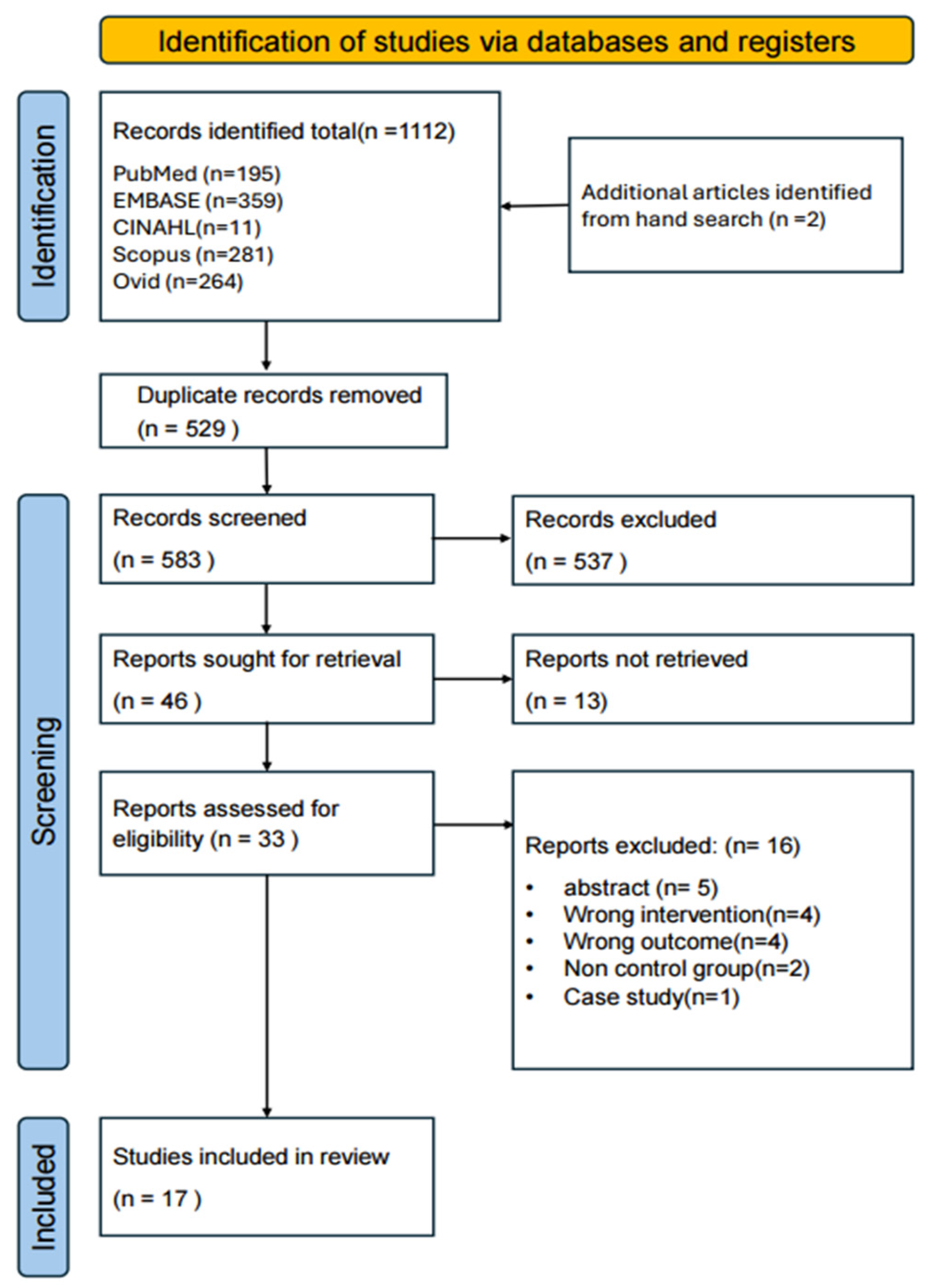
3.1. Study Selection
3.2. General Characteristics of the Studies
3.3. Outcomes Characteristics
3.4. Quality Assessment and Risk of Bias
3.5. Meta-Analysis Results
3.5.1. Gait Speed
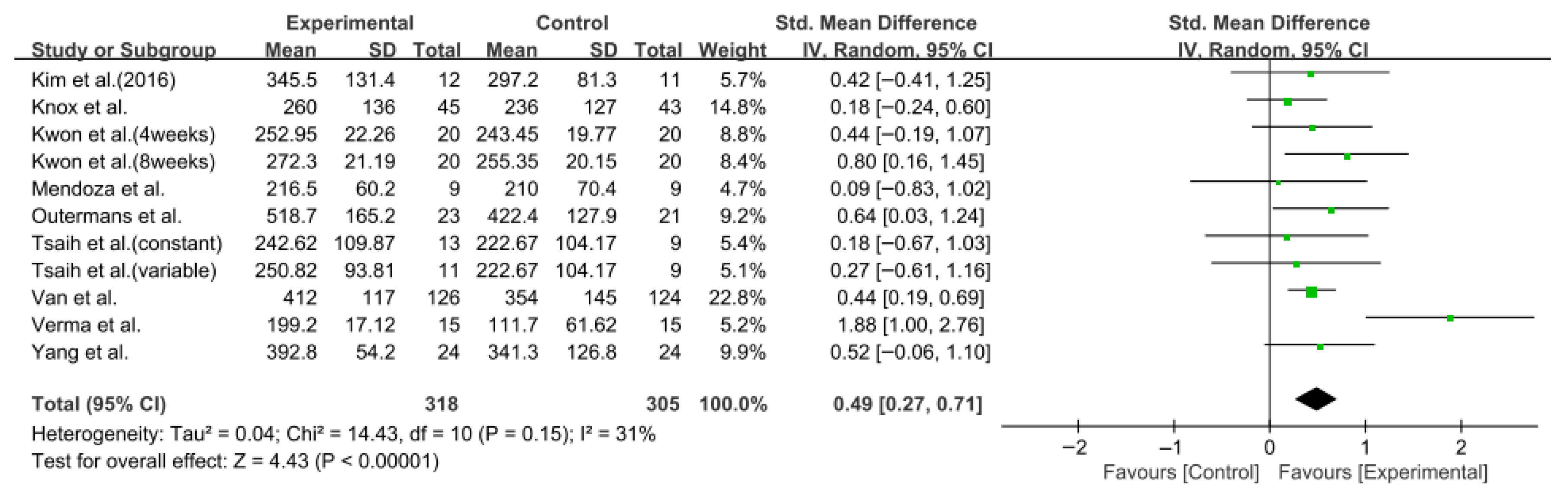
3.5.2. Six-Minute Walk Test
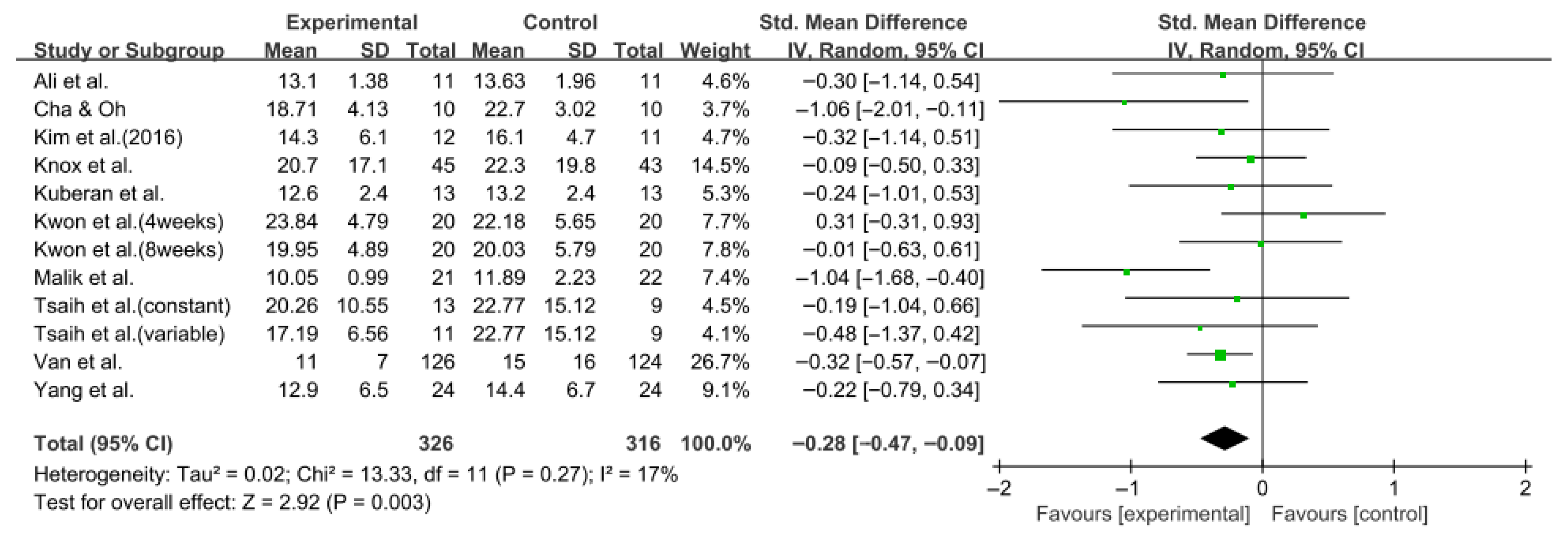
3.5.3. Berg Balance Scale
3.5.4. Timed up and Go Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Capirossi, C.; Laiso, A.; Renieri, L.; Capasso, F.; Limbucci, N. Epidemiology, organization, diagnosis and treatment of acute ischemic stroke. Eur. J. Radiol. Open 2023, 11, 100527. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Brainin, M.; Norrving, B.; Martins, S.O.; Pandian, J.; Lindsay, P.; Grupper, M.F.; Rautalin, I. World stroke organization: Global stroke fact sheet 2025. Int. J. Stroke 2025, 20, 132–144. [Google Scholar] [CrossRef] [PubMed]
- Van De Port, I.G.; Kwakkel, G.; Van Wijk, I.; Lindeman, E. Susceptibility to deterioration of mobility long-term after stroke: A prospective cohort study. Stroke 2006, 37, 167–171. [Google Scholar] [CrossRef]
- Gandolfi, M.; Valè, N.; Dimitrova, E.; Zanolin, M.E.; Mattiuz, N.; Battistuzzi, E.; Beccari, M.; Geroin, C.; Picelli, A.; Waldner, A. Robot-assisted stair climbing training on postural control and sensory integration processes in chronic post-stroke patients: A randomized controlled clinical trial. Front. Neurosci. 2019, 13, 1143. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research into Clinical Practice; Lippincott Williams & Wilkins: Ambler, PA, USA, 2007. [Google Scholar]
- Salem, Y.; Ciani, G.; Elokda, A.; Hegazy, F.; Aboelnasr, E.; Li, H. Immediate Effects of TaskOriented Training on Walking and Balance in Patients with Stroke: A Preliminary Study. Ageing Sci. Ment. Health Stud. 2022, 6, 1–5. [Google Scholar]
- Lyu, T.; Yan, K.; Lyu, J.; Zhao, X.; Wang, R.; Zhang, C.; Liu, M.; Xiong, C.; Liu, C.; Wei, Y. Comparative efficacy of gait training for balance outcomes in patients with stroke: A systematic review and network meta-analysis. Front. Neurol. 2023, 14, 1093779. [Google Scholar] [CrossRef]
- Alashram, A.R. Task-oriented training for gait rehabilitation in people with multiple sclerosis: A systematic review. J. Bodyw. Mov. Ther. 2024, 39, 87–96. [Google Scholar] [CrossRef]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Giovannini, S.; Iacovelli, C.; Brau, F.; Loreti, C.; Fusco, A.; Caliandro, P.; Biscotti, L.; Padua, L.; Bernabei, R.; Castelli, L. RObotic-Assisted Rehabilitation for balance and gait in Stroke patients (ROAR-S): Study protocol for a preliminary randomized controlled trial. Trials 2022, 23, 872. [Google Scholar] [CrossRef]
- Kawamoto, H.; Kamibayashi, K.; Nakata, Y.; Yamawaki, K.; Ariyasu, R.; Sankai, Y.; Sakane, M.; Eguchi, K.; Ochiai, N. Pilot study of locomotion improvement using hybrid assistive limb in chronic stroke patients. BMC Neurol. 2013, 13, 141. [Google Scholar] [CrossRef]
- Zhang, M.; Liang, Z.; Li, Y.; Meng, J.; Jiang, X.; Xu, B.; Li, H.; Liu, T. The effect of balance and gait training on specific balance abilities of survivors with stroke: A systematic review and network meta-analysis. Front. Neurol. 2023, 14, 1234017. [Google Scholar] [CrossRef]
- Potcovaru, C.-G.; Cinteză, D.; Săndulescu, M.I.; Poenaru, D.; Chiriac, O.; Lambru, C.; Moldoveanu, A.; Anghel, A.M.; Berteanu, M. The Impact of Virtual Reality as a Rehabilitation Method Using TRAVEE System on Functional Outcomes and Disability in Stroke Patients: A Pilot Study. Biomedicines 2024, 12, 2450. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, M.; Pan, X.; Geng, J. Effects of exercise on mobility, balance and gait in patients with the chronic stroke: A systematic review and meta-analysis. Sci. Rep. 2025, 15, 24158. [Google Scholar] [CrossRef] [PubMed]
- Gelaw, A.Y.; Janakiraman, B.; Teshome, A.; Ravichandran, H. Effectiveness of treadmill assisted gait training in stroke survivors: A systematic review and meta-analysis. Glob. Epidemiol. 2019, 1, 100012. [Google Scholar] [CrossRef]
- Liu, H.; Yin, H.; Yi, Y.; Liu, C.; Li, C. Effects of different rehabilitation training on balance function in stroke patients: A systematic review and network meta-analysis. Arch. Med. Sci. AMS 2023, 19, 1671. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Group, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Jpt, H. Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2008; Available online: http://www.cochrane.org/handbook (accessed on 15 July 2025).
- Higgins, J.; Li, T.; Deeks, J.J. Choosing effect measures and computing estimates of effect. In Cochrane Handbook of Systematic Reviews of Interventions; Cochrane: London, UK, 2019. [Google Scholar]
- Bhogal, S.K.; Teasell, R.W.; Foley, N.C.; Speechley, M.R. The PEDro scale provides a more comprehensive measure of methodological quality than the Jadad scale in stroke rehabilitation literature. J. Clin. Epidemiol. 2005, 58, 668–673. [Google Scholar] [CrossRef]
- Mavridis, D.; Salanti, G. How to assess publication bias: Funnel plot, trim-and-fill method and selection models. Èvid. Based Ment. Health 2014, 17, 30. [Google Scholar] [CrossRef]
- Harrer, M.; Cuijpers, P.; Furukawa, T.; Ebert, D. Doing Meta-Analysis with R: A Hands-on Guide; Chapman and Hall/CRC: Boca Raton, FL, USA, 2021. [Google Scholar]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Group, C.S.M. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; Cochrane: London, UK, 2019; pp. 241–284. [Google Scholar]
- Hedges, L.V.; Olkin, I. Statistical Methods for Meta-Analysis; Academic Press: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Durlak, J.A. How to select, calculate, and interpret effect sizes. J. Pediatr. Psychol. 2009, 34, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Feinn, R. Using effect size—Or why the P value is not enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Jin, Q.; Zhou, C.; Huang, Y.; Liu, J.; Chen, Y.; Hu, H.; Dai, Y.; Jin, R. Effect of Task-Oriented Biomechanical Perception-Balance Training on Motor Gait in Stroke Patients With Hemiplegia. J. Altern. Complement. Med. 2024, 30, 290–294. [Google Scholar]
- Ali, M.; Khan, S.U.; Asim, H.A.B. Effects of individual task specific training verses group circuit training on balance and ambulation in sub-acute stroke. Rawal Med. J. 2020, 45, 233–235. [Google Scholar]
- Kim, B.; Park, Y.; Seo, Y.; Park, S.; Cho, H.; Moon, H.; Lee, H.; Kim, M.; Yu, J. Effects of individualized versus group task-oriented circuit training on balance ability and gait endurance in chronic stroke inpatients. J. Phys. Ther. Sci. 2016, 28, 1872–1875. [Google Scholar] [CrossRef][Green Version]
- Cha, H.-G.; Oh, D.-W. Effects of mirror therapy integrated with task-oriented exercise on the balance function of patients with poststroke hemiparesis: A randomized-controlled pilot trial. Int. J. Rehabil. Res. 2016, 39, 70–76. [Google Scholar] [CrossRef]
- Kuberan, P.; Kumar, V.; Joshua, A.M.; Misri, Z.; Chakrapani, M. Effects of task oriented exercises with altered sensory input on balance and functional mobility in chronic stroke: A pilot randomized controlled trial. Bangladesh J. Med. Sci. 2017, 16, 307–313. [Google Scholar] [CrossRef]
- Kwon, O.-h.; Woo, Y.; Lee, J.-s.; Kim, K.-h. Effects of task-oriented treadmill-walking training on walking ability of stoke patients. Top. Stroke Rehabil. 2015, 22, 444–452. [Google Scholar] [CrossRef]
- Tsaih, P.-L.; Chiu, M.-J.; Luh, J.-J.; Yang, Y.-R.; Lin, J.-J.; Hu, M.-H. Practice variability combined with task-oriented electromyographic biofeedback enhances strength and balance in people with chronic stroke. Behav. Neurol. 2018, 2018, 7080218. [Google Scholar] [CrossRef]
- Knox, M.; Stewart, A.; Richards, C.L. Six hours of task-oriented training optimizes walking competency post stroke: A randomized controlled trial in the public health-care system of South Africa. Clin. Rehabil. 2018, 32, 1057–1068. [Google Scholar] [CrossRef]
- Verma, R.; Narayan Arya, K.; Garg, R.; Singh, T. Task-oriented circuit class training program with motor imagery for gait rehabilitation in poststroke patients: A randomized controlled trial. Top. Stroke Rehabil. 2011, 18, 620–632. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.-R.; Wang, R.-Y.; Lin, K.-H.; Chu, M.-Y.; Chan, R.-C. Task-oriented progressive resistance strength training improves muscle strength and functional performance in individuals with stroke. Clin. Rehabil. 2006, 20, 860–870. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.N.; Masood, T. Task-oriented training and exer-gaming for improving mobility after stroke: A randomized trial. J. Pak. Med. Assoc. 2021, 71, 186–190. [Google Scholar] [PubMed]
- Kim, C.-Y.; Lee, J.-S.; Kim, H.-D.; Kim, J.-S. The effect of progressive task-oriented training on a supplementary tilt table on lower extremity muscle strength and gait recovery in patients with hemiplegic stroke. Gait Posture 2015, 41, 425–430. [Google Scholar] [CrossRef]
- Atif, M.M.; Afzal, F. The effects of a task-oriented walking intervention on improving balance self-efficacy in post-stroke patients. Adv. Neurol. 2023, 2, 388. [Google Scholar] [CrossRef]
- Choi, J.-U.; Kang, S.-h. The effects of patient-centered task-oriented training on balance activities of daily living and self-efficacy following stroke. J. Phys. Ther. Sci. 2015, 27, 2985–2988. [Google Scholar] [CrossRef]
- Mendoza, K.G.; Aguila, M.E.R.; Alfonso, F.C.S.; Alfonso, M.G.T.; Elmi, K.D.; Gorgon, E.J.R. Comparison of two circuit class therapy programs on walking capacity, gait velocity and stair ambulation among patients with chronic stroke: A parallel pretest-posttest pilot study. Acta Medica Philipp. 2021, 55, 379–386. [Google Scholar] [CrossRef]
- Van de Port, I.G.; Wevers, L.E.; Lindeman, E.; Kwakkel, G. Effects of circuit training as alternative to usual physiotherapy after stroke: Randomised controlled trial. Br. Med. J. 2012, 344, e2672. [Google Scholar] [CrossRef]
- Outermans, J.C.; van Peppen, R.P.; Wittink, H.; Takken, T.; Kwakkel, G. Effects of a high-intensity task-oriented training on gait performance early after stroke: A pilot study. Clin. Rehabil. 2010, 24, 979–987. [Google Scholar] [CrossRef]
- Jeon, B.-J.; Kim, W.-H.; Park, E.-Y. Effect of task-oriented training for people with stroke: A meta-analysis focused on repetitive or circuit training. Top. Stroke Rehabil. 2015, 22, 34–43. [Google Scholar] [CrossRef]
- Schröder, J.; Truijen, S.; Van Criekinge, T.; Saeys, W. Feasibility and effectiveness of repetitive gait training early after stroke: A systematic review and meta-analysis. J. Rehabil. Med. 2019, 51, 78–88. [Google Scholar] [CrossRef]
- Bonini-Rocha, A.C.; de Andrade, A.L.S.; Moraes, A.M.; Matheus, L.B.G.; Diniz, L.R.; Martins, W.R. Effectiveness of circuit-based exercises on gait speed, balance, and functional mobility in people affected by stroke: A meta-analysis. Phys. Med. Rehabil. 2018, 10, 398–409. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.; Lewthwaite, R.; Blanton, S.R.; Wolf, L.B.; Wishart, L. Infusing motor learning research into neurorehabilitation practice: A historical perspective with case exemplar from the accelerated skill acquisition program. J. Neurol. Phys. Ther. 2014, 38, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Ren, H.; Hou, X.; Dong, X.; Zhang, S.; Lv, Y.; Li, C.; Yu, L. The effect of exercise on balance function in stroke patients: A systematic review and meta-analysis of randomized controlled trials. J. Neurol. 2024, 271, 4751–4768. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhong, D.; Ye, J.; He, M.; Liu, X.; Zheng, H.; Jin, R.; Zhang, S.-l. Rehabilitation for balance impairment in patients after stroke: A protocol of a systematic review and network meta-analysis. BMJ Open 2019, 9, e026844. [Google Scholar] [CrossRef]
- Li, X.; Wu, C.; Zhang, J.; Zeng, Q.; Wang, Y. Home-Based Exercise for Improving Balance Ability in Post-Stroke Patients: A Systematic Review and Meta-Analysis. Worldviews Evid.-Based Nurs. 2025, 22, e70057. [Google Scholar] [CrossRef]
- Awosika, O.O.; Garver, A.; Drury, C.; Sucharew, H.J.; Boyne, P.; Schwab, S.M.; Wasik, E.; Earnest, M.; Dunning, K.; Bhattacharya, A. Insufficiencies in sensory systems reweighting is associated with walking impairment severity in chronic stroke: An observational cohort study. Front. Neurol. 2023, 14, 1244657. [Google Scholar] [CrossRef]
- Meng, L.; Liang, Q.; Yuan, J.; Li, S.; Ge, Y.; Yang, J.; Tsang, R.C.; Wei, Q. Vestibular rehabilitation therapy on balance and gait in patients after stroke: A systematic review and meta-analysis. BMC Med. 2023, 21, 322. [Google Scholar] [CrossRef]
- Yamato, T.P.; Arora, M.; Stevens, M.L.; Elkins, M.R.; Moseley, A.M. Quality, language, subdiscipline and promotion were associated with article accesses on Physiotherapy Evidence Database (PEDro). Physiotherapy 2018, 104, 122–128. [Google Scholar] [CrossRef]



| Study (Year) | Age (Years, Mean ± SD) | Sample Size (Sex (M/F)) | Phase of Stroke | Intervention | Outcomes |
|---|---|---|---|---|---|
| Gao et al. (2024) [29] | E: 67.9 ± 7.0 C: 65.5 ± 6.4 | E: 53 (26/27) C: 53 (31/22) | Subacute | E: essential rehabilitation treatment and Task-Oriented Biomechanical Perception-Balance training C: essential rehabilitation training treatment | BBS, FMA |
| Ali et al. (2020) [30] | Total: 60.81 | E: 11 (7/4) C: 11 (6/5) | Subacute | E: group task-specific training C: individual task-specific training | BBS, TUG, 10MWT |
| Kim et al. (2016) [31] | E: 50 ± 9.3 C: 54 ± 7.1 | E: 15 (8/7) C: 15 (10/5) | Chronic | E: group task-oriented circuit training C: individual task-oriented circuit training | BBS, TUG, 6MWT |
| Cha and Oh (2016) [32] | E: 60 ± 3.19 C: 58.6 ± 4.08 | E: 10 (4/6) C: 10 (5/5) | Chronic | E: task-oriented exercise program with a mirror C: task-oriented exercise program | BBS, TUG |
| Kuberan et al. (2017) [33] | E: 58.82 ± 9.12 C: 60.07 ± 7.56 | E: 13 (9/4) C: 13 (9/4) | Chronic | E: task-oriented training with sensory input manipulations and provision of sensory conflict for the trunk and lower limb C: conventional physiotherapy program | TUG |
| Kwon et al. (2015) [34] | E: 50.7 ± 15.16 C: 47.15 ± 18.65 | E: 20 (14/6) C: 20 (12/8) | Chronic | E: task-oriented treadmill walking training C: conventional treadmill walking training | TUG, 6MWT |
| Tsaih et al. (2018) [35] | E1: 48.6 ± 12.6 E2: 55.5 ± 12.4 C: 56.1 ± 9.0 | E1: 11 (10/1) E2: 13 (9/4) C: 9 (7/2) | Chronic | E1: variable-practice EMGBFB and general PT E2: constant-practice EMGBFB and general PT C: upper extremity exercise and general PT | Gait speed, TUG, 6MWT |
| Knox et al. (2018) [36] | E: 51 ± 15 C: 48 ± 14 | E: 51 (25/26) C: 48 (22/26) | Subacute | E: task intervention C: stroke management | Gait speed (CV, FV), BBS, TUG, 6MWT |
| Verma et al. (2011) [37] | E: 53.27 ± 8.53 C: 55.07 ± 6.8 | E: 15 (10/5) C: 15 (12/3) | Acute | E: motor imagery and task-oriented circuit class training C: lower extremity rehabilitation program | Gait speed (CV, FV), 6MWT |
| Yang et al. (2006) [38] | E: 56.8 ± 10.2 C: 60.0 ± 10.4 | E: 24 (16/8) C: 24 (16/8) | Chronic | E: task-oriented progressive resistance strength training C: did not receive any rehabilitation training | Gait speed, 6MWT, TUG |
| Malik et al. (2021) [39] | Total: 40–70 | E: 26 C: 26 Total: 52 (36/16) | Subacute | E: task-oriented training and exercise gaming C: task-oriented training | TUG, BBS |
| Kim et al. (2015) [40] | E: 58.53 ± 11.83 C: 61.24 ± 8.73 | E: 10 (4/6) C: 10 (6/4) | Subacute | E: routine therapy and tilted table with task-oriented training C: routine therapy and tilted table | Gait speed |
| Atif and Afzal (2023) [41] | - | E: 15 C: 15 Total: 30 (18/12) | Subacute | E: task-oriented walking C: conventional therapy | BBS |
| Choi and Kang (2015) [42] | E: 61.5 ± 7.2 C: 66.4 ± 9.3 | E: 10 (4/6) C: 10 (4/6) | Chronic | E: task-oriented training C: general physical therapy | BBS |
| Mendoza et al. (2021) [43] | E: 47.2 ± 8.8 C: 49 ± 11.2 | E: 9 (9/0) C: 9 (7/2) | Chronic | E: task-oriented circuit class training C: circuit class training focused on specific impairments | Gait speed (CV, FV), 6MWT |
| Van et al. (2012) [44] | E: 56 ± 10 C: 58 ± 10 | E: 126 (82/44) C: 124 (80/44) | Subacute | E: task-oriented circuit training C: outpatient physiotherapy | Gait speed (CV), 6MWT, TUG |
| Outermans et al. (2010) [45] | E: 56.8 ± 8.6 C: 56.3 ± 8.6 | E: 23 (19/4) C: 21 (17/4) | Subacute | E: high-intensity task-oriented training C: low-intensity physiotherapy | 6MWT, 10MWT, BBS |
| Study (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gao et al. (2024) [29] | Y | Y | N | Y | N | N | N | Y (0%) | Y | Y | Y | 6 |
| Ali et al. (2020) [30] | Y | Y | N | N | N | N | N | Y (0%) | Y | Y | Y | 5 |
| Kim et al. (2016) [31] | Y | Y | N | N | N | N | N | N (23%) | N | Y | Y | 3 |
| Cha and Oh (2016) [32] | Y | Y | N | Y | N | N | Y | N (20%) | N | Y | Y | 5 |
| Kuberan et al. (2017) [33] | Y | Y | N | Y | N | N | Y | Y (0%) | Y | Y | Y | 7 |
| kwon et al. (2015) [34] | Y | Y | N | Y | N | N | N | Y (9%) | N | Y | Y | 5 |
| Tsaih et al. (2018) [35] | Y | Y | N | Y | N | N | Y | Y (0%) | Y | Y | Y | 7 |
| Knox et al. (2018) [36] | Y | Y | Y | Y | N | Y | Y | Y (11%) | N | Y | Y | 8 |
| Verma et al. (2011) [37] | Y | Y | Y | Y | Y | N | Y | Y (3%) | Y | Y | Y | 9 |
| Yang et al. (2006) [38] | Y | Y | Y | Y | N | N | Y | Y (0%) | Y | Y | Y | 8 |
| Malik et al. (2021) [39] | Y | Y | Y | Y | N | N | Y | N (17%) | N | Y | Y | 6 |
| Kim et al. (2015) [40] | Y | Y | N | Y | N | N | Y | N (18%) | N | Y | Y | 5 |
| Atif and Afzal (2023) [41] | Y | Y | N | N | N | N | N | Y (0%) | Y | Y | Y | 5 |
| Choi and Kang (2015) [42] | Y | Y | N | Y | N | N | N | Y (0%) | Y | Y | Y | 6 |
| Mendoza et al. (2021) [43] | Y | Y | Y | Y | N | N | Y | Y (0%) | Y | Y | Y | 8 |
| Van et al. (2012) [44] | Y | Y | Y | N | N | N | Y | Y (3%) | N | Y | Y | 6 |
| Outermans et al. (2010) [45] | Y | Y | Y | Y | N | N | N | N (27%) | Y | Y | Y | 6 |
| Category | Subgroup | No. of Trials | Sample Size | SMD (d) [95% CI] | Heterogeneity p-Value of Chi-Square Test (I2) | Overall Effect Z Value (p-Value) | Subgroup Diff. p-Value |
|---|---|---|---|---|---|---|---|
| Phase of stroke | Acute | 0 | 0 | ||||
| Subacute | 6 | 332 | 0.22 [−0.04, 0.48] | 6.82 (27%) | 1.63 (0.10) | 0.03 * | |
| Chronic | 3 | 63 | 1.33 [0.34. 2.32] | 5.92 (66%) | 2.64 (0.008 *) | ||
| During session | ≤60 min | 5 | 198 | 0.64 [0.10, 1.18] | 10.29 (61%) | 2.33 (0.02 *) | 0.32 |
| >60 min | 4 | 197 | 0.25 [−0.29, 0.80] | 9.70 (69%) | 0.91 (0.36) | ||
| Weekly frequency | ≤3 times/week | 6 | 249 | 0.23 [−0.14, 0.61] | 9.92 (50%) | 1.21 (0.22) | 0.14 |
| >3 times/week | 3 | 146 | 1.00 [0.06, 1.95] | 8.36 (76%) | 2.08 (0.04 *) | ||
| Duration of trial | ≤6 weeks | 5 | 128 | 0.77 [0.00, 1.53] | 15.86 (75%) | 1.96 (0.05) | 0.24 |
| >6 weeks | 4 | 267 | 0.26 [−0.10, 0.61] | 5.83 (49%) | 1.43 (0.15) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-H.; Lee, D.-Y. Effects of Task-Oriented Training on Gait Outcomes and Balance in Individuals with Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2025, 14, 8766. https://doi.org/10.3390/jcm14248766
Lee M-H, Lee D-Y. Effects of Task-Oriented Training on Gait Outcomes and Balance in Individuals with Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2025; 14(24):8766. https://doi.org/10.3390/jcm14248766
Chicago/Turabian StyleLee, Myoung-Ho, and Do-Youn Lee. 2025. "Effects of Task-Oriented Training on Gait Outcomes and Balance in Individuals with Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 14, no. 24: 8766. https://doi.org/10.3390/jcm14248766
APA StyleLee, M.-H., & Lee, D.-Y. (2025). Effects of Task-Oriented Training on Gait Outcomes and Balance in Individuals with Stroke: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 14(24), 8766. https://doi.org/10.3390/jcm14248766






