Body Roundness Index Outperforms Body Mass Index in Predicting Obstructive Sleep Apnea Severity Among Chinese Adults
Abstract
1. Introduction
2. Methods
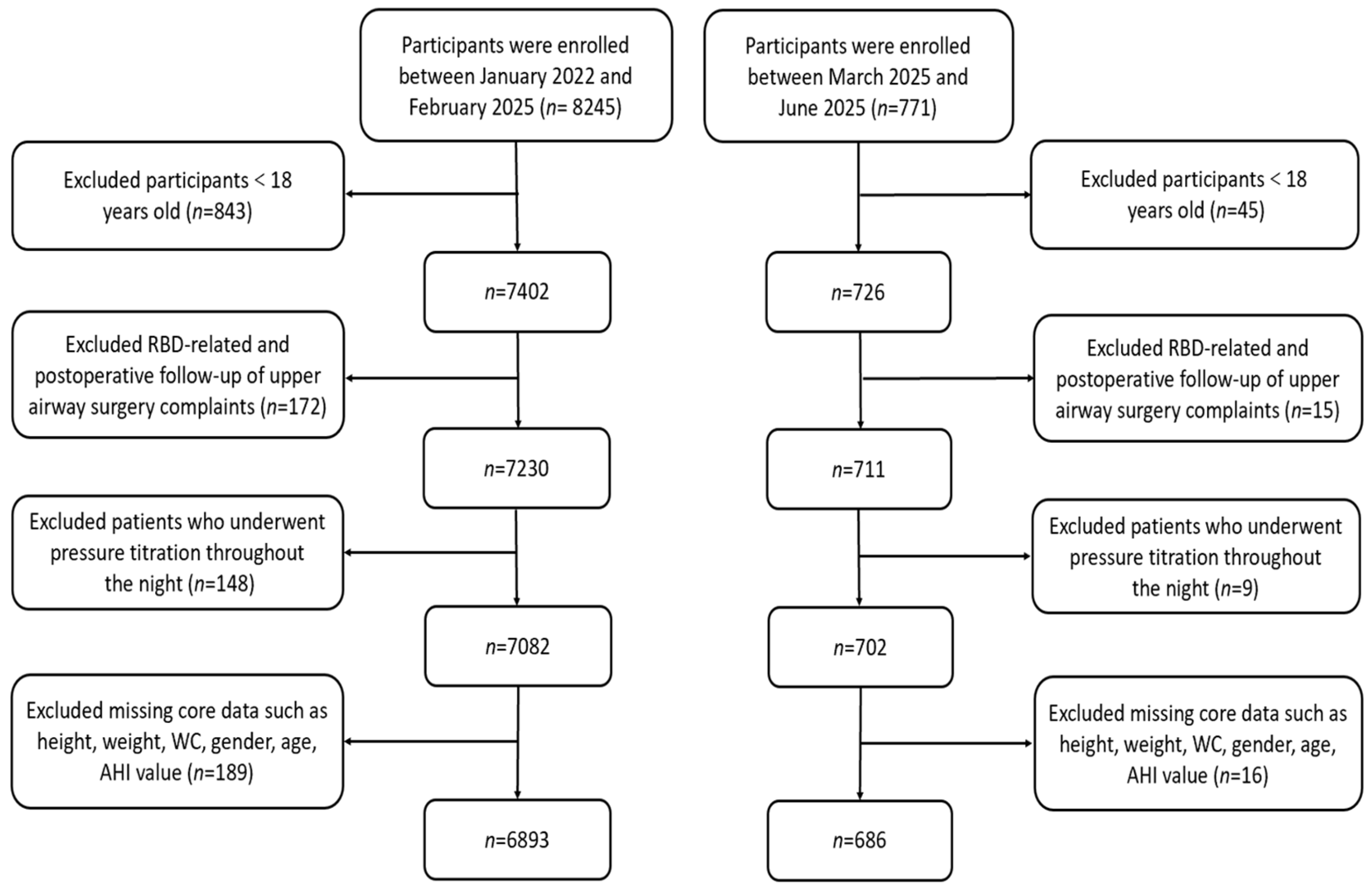
2.1. Study Population and Design
2.2. Anthropometric Measurements and Questionnaires
2.3. Polysomnography
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, G.T.; Caffo, B.; Newman, A.B.; Quan, S.F.; Rapoport, D.M.; Redline, S.; Resnick, H.E.; Samet, J.; Shahar, E. Prospective study of sleep-disordered breathing and hypertension: The Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 2009, 179, 1159–1164. [Google Scholar] [CrossRef]
- Abelleira, R.; Zamarrón, C.; Riveiro, V.; Casal, A.; Toubes, M.E.; Rábade, C.; Ricoy, J.; Lama, A.; Rodríguez-Núñez, N.; Ferreiro, L.; et al. Relationship between obstructive sleep apnea and type 2 diabetes mellitus. Relación entre la apnea obstructiva del sueño y la diabetes mellitus tipo 2. Med. Clin. 2024, 162, 363–369. [Google Scholar] [CrossRef]
- Pérez-Carbonell, L.; Bashir, S. Narrative review of sleep and stroke. J. Thorac. Dis. 2020, 12 (Suppl. S2), S176–S190. [Google Scholar] [CrossRef] [PubMed]
- Tobaldini, E.; Costantino, G.; Solbiati, M.; Cogliati, C.; Kara, T.; Nobili, L.; Montano, N. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci. Biobehav. Rev. 2017, 74 Pt B, 321–329. [Google Scholar] [CrossRef]
- Shah, F.; Stål, P. Myopathy of the upper airway in snoring and obstructive sleep apnea. Laryngoscope Investig. Otolaryngol. 2022, 7, 636–645. [Google Scholar] [CrossRef]
- Rubino, F.; Cummings, D.E.; Eckel, R.H.; Cohen, R.V.; Wilding, J.P.H.; Brown, W.A.; Stanford, F.C.; Batterham, R.L.; Farooqi, I.S.; Farpour-Lambert, N.J.; et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025, 13, 221–262. [Google Scholar] [CrossRef]
- Lee, R.W.; Vasudavan, S.; Hui, D.S.; Prvan, T.; Petocz, P.; Darendeliler, M.A.; Cistulli, P.A. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 2010, 33, 1075–1080. [Google Scholar] [CrossRef]
- Wang, L.; Zhao, W.; Liang, C.; Yan, X.; Zhang, H.; Dai, H.; Yu, H.; Zhang, H.; An, H.; Zhao, Y. Accuracy and modification of the STOP-bang questionnaire for screening patients with obstructive sleep apnea in China. J. Sleep Res. 2022, 32, e13781. [Google Scholar] [CrossRef]
- Sangkum, L.; Wathanavaha, C.; Tantrakul, V.; Pothong, M.; Karnjanarachata, C. Modified STOP-Bang for predicting perioperative adverse events in the Thai population. BMC Anesthesiol. 2021, 21, 132. [Google Scholar] [CrossRef]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2012, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Guo, Z.; Wang, M.; Xiang, C. Association between body roundness index and risk of osteoarthritis: A cross-sectional study. Lipids Health Dis. 2024, 23, 334. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Jin, L.; Li, D.; Zhang, Y.; Zhao, W.; Zhao, Y.; Gao, J.; Zhou, L.; Chen, P.; Dong, G. The association between the body roundness index and the risk of colorectal cancer: A cross-sectional study. Lipids Health Dis. 2023, 22, 53. [Google Scholar] [CrossRef]
- Pan, X.; Liu, F.; Fan, J.; Guo, Q.; Guo, M.; Chen, Y.; Sun, J.; Cao, X. Association of Body Roundness Index and A Body Shape Index with Obstructive Sleep Apnea: Insights from NHANES 2015-2018 data. Front. Nutr. 2024, 11, 1492673. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhai, Y.; Wang, J.; Han, X.; Si, W.; Zhou, Y. Association between body roundness index and obstructive sleep apnea among US adults: Data from the 2005–2008 and 2015–2018 National Health and Nutrition Examination Survey. Sleep Biol. Rhythm. 2025, 23, 171–179. [Google Scholar] [CrossRef]
- Chung, F.; Abdullah, H.R.; Liao, P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest 2016, 149, 631–638. [Google Scholar] [CrossRef]
- Zhao, X.; Xu, H.; Qian, Y.; Liu, Y.; Zou, J.; Yi, H.; Guan, J.; Yin, S. Abdominal Obesity Is More Strongly Correlated with Obstructive Sleep Apnea than General Obesity in China: Results from Two Separated Observational and Longitudinal Studies. Obes. Surg. 2019, 29, 2535–2547. [Google Scholar] [CrossRef]
- Chen, Y.; Yu, W.; Lv, J.; Sun, D.; Pei, P.; Du, H.; Yang, L.; Chen, Y.; Zhang, H.; Chen, J.; et al. Early adulthood BMI and cardiovascular disease: A prospective cohort study from the China Kadoorie Biobank. Lancet Public Health 2024, 9, e1005–e1013. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, C.; Feng, L.; Shen, Y.; Ma, J.; Wang, G. Modified STOP-bang questionnaire incorporating morning dry mouth and BMI adjustment in China: A retrospective study of 590 patients. Expert Rev. Respir. Med. 2023, 17, 1041–1048. [Google Scholar] [CrossRef]
- Gao, H.; Zhang, R.; Wang, P.; Liu, D.; Han, J.; Wang, B. Relationship between body roundness index and obstructive sleep apnea: A population-based study. Front. Nutr. 2025, 12, 1531006. [Google Scholar] [CrossRef] [PubMed]
- Qin, B.; Shu, M.; Cai, S.; Zhou, Y.; Song, J.; Peng, J. Association between body roundness index and obstructive sleep apnea: A cross-sectional study from the NHANES (2005–2008 to 2015–2020). BMC Oral Health 2025, 25, 666. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Papanicolaou, D.A.; Bixler, E.O.; Hopper, K.; Lotsikas, A.; Lin, H.-M.; Kales, A.; Chrousos, G.P. Sleep apnea and daytime sleepiness and fatigue: Relation to visceral obesity, insulin resistance, and hypercytokinemia. J. Clin. Endocrinol. Metab. 2000, 85, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Cho, T.; Yan, E.; Chung, F. The STOP-Bang questionnaire: A narrative review on its utilization in different populations and settings. Sleep Med. Rev. 2024, 78, 102007. [Google Scholar] [CrossRef]
- Cai, X.; Song, S.; Hu, J.; Zhu, Q.; Yang, W.; Hong, J.; Luo, Q.; Yao, X.; Li, N. Body roundness index improves the predictive value of cardiovascular disease risk in hypertensive patients with obstructive sleep apnea: A cohort study. Clin. Exp. Hypertens. 2023, 45, 2259132. [Google Scholar] [CrossRef]
- Mitra, A.K.; Bhuiyan, A.R.; Jones, E.A. Association and Risk Factors for Obstructive Sleep Apnea and Cardiovascular Diseases: A Systematic Review. Diseases 2021, 9, 88. [Google Scholar] [CrossRef]
- Zhan, Q.; An, Q.; Zhang, F.; Zhang, T.; Liu, T.; Wang, Y. Body roundness index and the risk of hypertension: A prospective cohort study in Southwest China. BMC Public Health 2024, 24, 2539. [Google Scholar] [CrossRef]
- Rico-Martín, S.; Calderón-García, J.F.; Sánchez-Rey, P.; Franco-Antonio, C.; Alvarez, M.M.; Muñoz-Torrero, J.F.S. Effectiveness of body roundness index in predicting metabolic syndrome: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13023. [Google Scholar] [CrossRef]
- Li, Y.; He, Y.; Yang, L.; Liu, Q.; Li, C.; Wang, Y.; Yang, P.; Wang, J.; Chen, Z.; Huang, X. Body Roundness Index and Waist-Hip Ratio Result in Better Cardiovascular Disease Risk Stratification: Results from a Large Chinese Cross-Sectional Study. Front. Nutr. 2022, 9, 801582. [Google Scholar] [CrossRef]
- Orbea, C.A.P.; Lloyd, R.M.; Faubion, S.S.; Miller, V.M.; Mara, K.C.; Kapoor, E. Predictive ability and reliability of the STOP-BANG questionnaire in screening for obstructive sleep apnea in midlife women. Maturitas 2020, 135, 1–5. [Google Scholar] [CrossRef]
- Mou, J.; Pflugeisen, B.M.; Crick, B.A.; Amoroso, P.J.; Harmon, K.T.; Tarnoczy, S.F.; Ho, S.S.; Mebust, K.A. The discriminative power of STOP-Bang as a screening tool for suspected obstructive sleep apnea in clinically referred patients: Considering gender differences. Sleep Breath. 2019, 23, 65–75. [Google Scholar] [CrossRef]
- Xia, M.; Liu, S.; Ji, N.; Xu, J.; Zhou, Z.; Tong, J.; Zhang, Y. BMI 35 kg/m2 does not fit everyone: A modified STOP-Bang questionnaire for sleep apnea screening in the Chinese population. Sleep Breath. 2018, 22, 1075–1082. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, R.; Jia, J.; Yuan, W.; Li, J. A modified STOP-Bang questionnaire for OSA screening in the young, middle-age women. J. Clin. Otorhinolaryngol. Head Neck Surg. 2020, 34, 811–814. [Google Scholar] [CrossRef]
- Perger, E.; Mattaliano, P.; Lombardi, C. Menopause and Sleep Apnea. Maturitas 2019, 124, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Popovic, R.M.; White, D.P. Upper airway muscle activity in normal women: Influence of hormonal status. J. Appl. Physiol. 1998, 84, 1055–1062. [Google Scholar] [CrossRef]
- Pillar, G.; Malhotra, A.; Fogel, R.; Beauregard, J.; Schnall, R.; White, D.P. Airway mechanics and ventilation in response to resistive loading during sleep: Influence of gender. Am. J. Respir. Crit. Care Med. 2000, 162, 1627–1632. [Google Scholar] [CrossRef]
- Chang, J.L.; Goldberg, A.N.; Alt, J.A.; Mohammed, A.; Ashbrook, L.; Auckley, D.; Ayappa, I.; Bakhtiar, H.; Barrera, J.E.; Bartley, B.L.; et al. International Consensus Statement on Obstructive Sleep Apnea. Int. Forum Allergy Rhinol. 2023, 13, 1061–1482. [Google Scholar] [CrossRef]
| All 1 | AHI < 30 n = 3715 1 | AHI ≥ 30 n = 3864 1 | p Value 2 | |
|---|---|---|---|---|
| Gender (%) | <0.001 | |||
| Female | 2176.0 (28.7%) | 1572.0 (42.3%) | 604.0 (15.6%) | |
| Male | 5403.0 (71.3%) | 2143.0 (57.7%) | 3260.0 (84.4%) | |
| Snore (%) | <0.001 | |||
| Yes | 6660.0 (87.9%) | 2861.0 (77.0%) | 3799.0 (98.3%) | |
| No | 919.0 (12.1%) | 854.0 (23.0%) | 65.0 (1.7%) | |
| Stop breathing (%) | <0.001 | |||
| Yes | 3380.0 (44.6%) | 1397.0 (37.6%) | 1983.0 (51.3%) | |
| No | 4199.0 (55.4%) | 2318.0 (62.4%) | 1881.0 (48.7%) | |
| Leg movement (%) | 0.026 | |||
| Yes | 1586.0 (20.9%) | 817.0 (22.0%) | 769.0 (19.9%) | |
| No | 5993.0 (79.1%) | 2898.0 (78.0%) | 3095.0 (80.1%) | |
| Daytime sleepiness (%) | <0.001 | |||
| Yes | 4019.0 (53.0%) | 1763.0 (47.5%) | 2256.0 (58.4%) | |
| No | 3560.0 (47.0%) | 1952.0 (52.5%) | 1608.0 (41.6%) | |
| Hypertension (%) | <0.001 | |||
| Yes | 1658.0 (21.9%) | 507.0 (13.6%) | 1151.0 (29.8%) | |
| No | 5921.0 (78.1%) | 3208.0 (86.4%) | 2713.0 (70.2%) | |
| Arrhythmia (%) | 0.158 | |||
| Yes | 518.0 (6.8%) | 238.0 (6.4%) | 280.0 (7.2%) | |
| No | 7061.0 (93.2%) | 3477.0 (93.6%) | 3584.0 (92.8%) | |
| Coronary heart disease (%) | 0.120 | |||
| Yes | 422.0 (5.6%) | 191.0 (5.1%) | 231.0 (6.0%) | |
| No | 7157.0 (94.4%) | 3524.0 (94.9%) | 3633.0 (94.0%) | |
| Diabetes (%) | <0.001 | |||
| Yes | 398.0 (5.3%) | 137.0 (3.7%) | 261.0 (6.8%) | |
| No | 7181.0 (94.7%) | 3578.0 (96.3%) | 3603.0 (93.2%) | |
| Cerebrovascular disease (%) | 0.025 | |||
| Yes | 316.0 (4.2%) | 135.0 (3.6%) | 181.0 (4.7%) | |
| No | 7263.0 (95.8%) | 3580.0 (96.4%) | 3683.0 (95.3%) | |
| Drinking (%) | <0.001 | |||
| Yes | 3280.0 (43.3%) | 1288.0 (34.7%) | 1992.0 (51.6%) | |
| No | 4299.0 (56.7%) | 2427.0 (65.3%) | 1872.0 (48.4%) | |
| Smoking (%) | <0.001 | |||
| Yes | 2440.0 (32.2%) | 944.0 (25.4%) | 1496.0 (38.7%) | |
| No | 5139.0 (67.8%) | 2771.0 (74.6%) | 2368.0 (61.3%) | |
| Age | <0.001 | |||
| Mean (SD) | 43.9 (13.1) | 41.9 (13.6) | 45.7 (12.4) | |
| Median (Q1, Q3) | 42.0 (34.0, 54.0) | 40.0 (32.0, 52.0) | 44.0 (36.0, 55.0) | |
| Height | <0.001 | |||
| Mean (SD) | 152.1 (48.1) | 147.5 (52.4) | 156.6 (43.2) | |
| Median (Q1, Q3) | 167.0 (159.0, 172.0) | 165.0 (157.0, 171.0) | 168.0 (162.0, 173.0) | |
| Weight | <0.001 | |||
| Mean (SD) | 71.6 (14.4) | 66.0 (12.8) | 77.0 (13.8) | |
| Median (Q1, Q3) | 70.0 (62.0, 80.0) | 65.0 (56.0, 74.0) | 75.0 (68.0, 85.0) | |
| NC | <0.001 | |||
| Mean (SD) | 38.1 (4.0) | 36.4 (3.8) | 39.7 (3.6) | |
| Median (Q1, Q3) | 38.0 (35.0, 41.0) | 36.0 (33.0, 39.0) | 40.0 (38.0, 42.0) | |
| BMI | <0.001 | |||
| Mean (SD) | 25.5 (4.1) | 23.9 (3.6) | 27.1 (3.9) | |
| Median (Q1, Q3) | 25.2 (22.9, 27.8) | 23.7 (21.5, 25.8) | 26.7 (24.6, 29.2) | |
| BRI | <0.001 | |||
| Mean (SD) | 4.4 (1.4) | 3.9 (1.2) | 4.9 (1.3) | |
| Median (Q1, Q3) | 4.3 (3.5, 5.2) | 3.8 (3.1, 4.5) | 4.8 (4.1, 5.6) | |
| WC | <0.001 | |||
| Mean (SD) | 91.8 (11.6) | 86.7 (10.8) | 96.6 (10.2) | |
| Median (Q1, Q3) | 92.0 (84.0, 99.0) | 87.0 (79.0, 93.0) | 96.0 (90.0, 102.0) | |
| ESS | <0.001 | |||
| Mean (SD) | 7.4 (5.6) | 6.9 (5.6) | 8.0 (5.6) | |
| Median (Q1, Q3) | 6.0 (3.0, 11.0) | 6.0 (2.0, 10.0) | 7.0 (4.0, 12.0) | |
| Stop-Bang | <0.001 | |||
| Mean (SD) | 3.5 (1.6) | 2.8 (1.5) | 4.2 (1.4) | |
| Median (Q1, Q3) | 3.0 (2.0, 5.0) | 3.0 (2.0, 4.0) | 4.0 (3.0, 5.0) | |
| BRI-optimized STOP-Bang | <0.001 | |||
| Mean (SD) | 4.0 (1.7) | 3.2 (1.6) | 4.8 (1.4) | |
| Median (Q1, Q3) | 4.0 (3.0, 5.0) | 3.0 (2.0, 4.0) | 5.0 (4.0, 6.0) |
| All 1 | BRI < Youden n = 3020 1 | BRI ≥ Youden n = 4559 1 | p Value 2 | |
|---|---|---|---|---|
| Gender (%) | <0.001 | |||
| Female | 2176.0 (28.7%) | 1212.0 (40.1%) | 964.0 (21.1%) | |
| Male | 5403.0 (71.3%) | 1808.0 (59.9%) | 3595.0 (78.9%) | |
| Snore (%) | <0.001 | |||
| Yes | 6660.0 (87.9%) | 2368.0 (78.4%) | 4292.0 (94.1%) | |
| No | 919.0 (12.1%) | 652.0 (21.6%) | 267.0 (5.9%) | |
| Stop breathing (%) | <0.001 | |||
| Yes | 3380.0 (44.6%) | 1136.0 (37.6%) | 2244.0 (49.2%) | |
| No | 4199.0 (55.4%) | 1884.0 (62.4%) | 2315.0 (50.8%) | |
| Leg movement (%) | 0.015 | |||
| Yes | 1586.0 (20.9%) | 590.0 (19.5%) | 996.0 (21.8%) | |
| No | 5993.0 (79.1%) | 2430.0 (80.5%) | 3563.0 (78.2%) | |
| Daytime sleepiness (%) | <0.001 | |||
| Yes | 4019.0 (53.0%) | 1437.0 (47.6%) | 2582.0 (56.6%) | |
| No | 3560.0 (47.0%) | 1583.0 (52.4%) | 1977.0 (43.4%) | |
| Hypertension (%) | <0.001 | |||
| Yes | 1658.0 (21.9%) | 304.0 (10.1%) | 1354.0 (29.7%) | |
| No | 5921.0 (78.1%) | 2716.0 (89.9%) | 3205.0 (70.3%) | |
| Arrhythmia (%) | <0.001 | |||
| Yes | 518.0 (6.8%) | 140.0 (4.6%) | 378.0 (8.3%) | |
| No | 7061.0 (93.2%) | 2880.0 (95.4%) | 4181.0 (91.7%) | |
| Coronary heart disease (%) | <0.001 | |||
| Yes | 422.0 (5.6%) | 83.0 (2.7%) | 339.0 (7.4%) | |
| No | 7157.0 (94.4%) | 2937.0 (97.3%) | 4220.0 (92.6%) | |
| Diabetes (%) | <0.001 | |||
| Yes | 398.0 (5.3%) | 82.0 (2.7%) | 316.0 (6.9%) | |
| No | 7181.0 (94.7%) | 2938.0 (97.3%) | 4243.0 (93.1%) | |
| Cerebrovascular disease (%) | <0.001 | |||
| Yes | 316.0 (4.2%) | 81.0 (2.7%) | 235.0 (5.2%) | |
| No | 7263.0 (95.8%) | 2939.0 (97.3%) | 4324.0 (94.8%) | |
| Drinking (%) | <0.001 | |||
| Yes | 3280.0 (43.3%) | 1096.0 (36.3%) | 2184.0 (47.9%) | |
| No | 4299.0 (56.7%) | 1924.0 (63.7%) | 2375.0 (52.1%) | |
| Smoking (%) | <0.001 | |||
| Yes | 2440.0 (32.2%) | 717.0 (23.7%) | 1723.0 (37.8%) | |
| No | 5139.0 (67.8%) | 2303.0 (76.3%) | 2836.0 (62.2%) | |
| Age | <0.001 | |||
| Mean (SD) | 43.9 (13.1) | 40.4 (12.6) | 46.1 (13.0) | |
| Median (Q1, Q3) | 42.0 (34.0, 54.0) | 39.0 (31.0, 50.0) | 45.0 (36.0, 56.0) | |
| AHI | <0.001 | |||
| Mean (SD) | 36.9 (28.5) | 22.9 (21.1) | 46.2 (28.9) | |
| Median (Q1, Q3) | 30.8 (11.9, 58.8) | 15.8 (5.8, 34.1) | 45.1 (20.8, 68.9) | |
| Height | 0.888 | |||
| Mean (SD) | 152.1 (48.1) | 150.6 (50.6) | 153.1 (46.4) | |
| Median (Q1, Q3) | 167.0 (159.0, 172.0) | 167.0 (158.0, 173.0) | 167.00 (160.0, 172.0) | |
| Weight | <0.001 | |||
| Mean (SD) | 71.6 (14.4) | 63.4 (10.8) | 77.0 (13.9) | |
| Median (Q1, Q3) | 70.0 (62.0, 80.0) | 63.0 (55.0, 70.0) | 75.0 (68.0, 85.0) | |
| NC | <0.001 | |||
| Mean (SD) | 38.1 (4.0) | 35.6 (3.4) | 39.7 (3.6) | |
| Median (Q1, Q3) | 38.0 (35.0, 41.0) | 36.0 (33.0, 38.0) | 40.0 (37.0, 42.0) | |
| BMI | <0.001 | |||
| Mean (SD) | 25.5 (4.1) | 22.5 (2.6) | 27.5 (3.7) | |
| Median (Q1, Q3) | 25.2 (22.9, 27.8) | 22.7 (20.9, 24.2) | 27.06 (25.2, 29.4) | |
| WC | <0.001 | |||
| Mean (SD) | 91.8 (11.6) | 81.7 (7.4) | 98.4 (8.8) | |
| Median (Q1, Q3) | 92.0 (84.0, 99.0) | 83.0 (77.0, 87.5) | 97.0 (93.0, 103.0) | |
| ESS | <0.001 | |||
| Mean (SD) | 7.4 (5.6) | 6.6 (5.1) | 8.0 (5.8) | |
| Median (Q1, Q3) | 6.0 (3.0, 11.0) | 6.0 (3.0, 10.0) | 7.0 (3.0, 12.0) | |
| Stop-Bang | <0.001 | |||
| Mean (SD) | 3.5 (1.6) | 2.6 (1.3) | 4.1 (1.5) | |
| Median (Q1, Q3) | 3.0 (2.0, 5.0) | 3.0 (2.0, 3.0) | 4.0 (3.0, 5.0) | |
| BRI-optimized STOP-Bang | <0.001 | |||
| Mean (SD) | 4.0 (1.7) | 2.6 (1.3) | 4.9 (1.4) | |
| Median (Q1, Q3) | 4.0 (3.0, 5.0) | 3.0 (2.0, 3.0) | 5.0 (4.0, 6.0) |
| AUC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | AUC (95% CI), p (Delong) | |
|---|---|---|---|---|---|---|
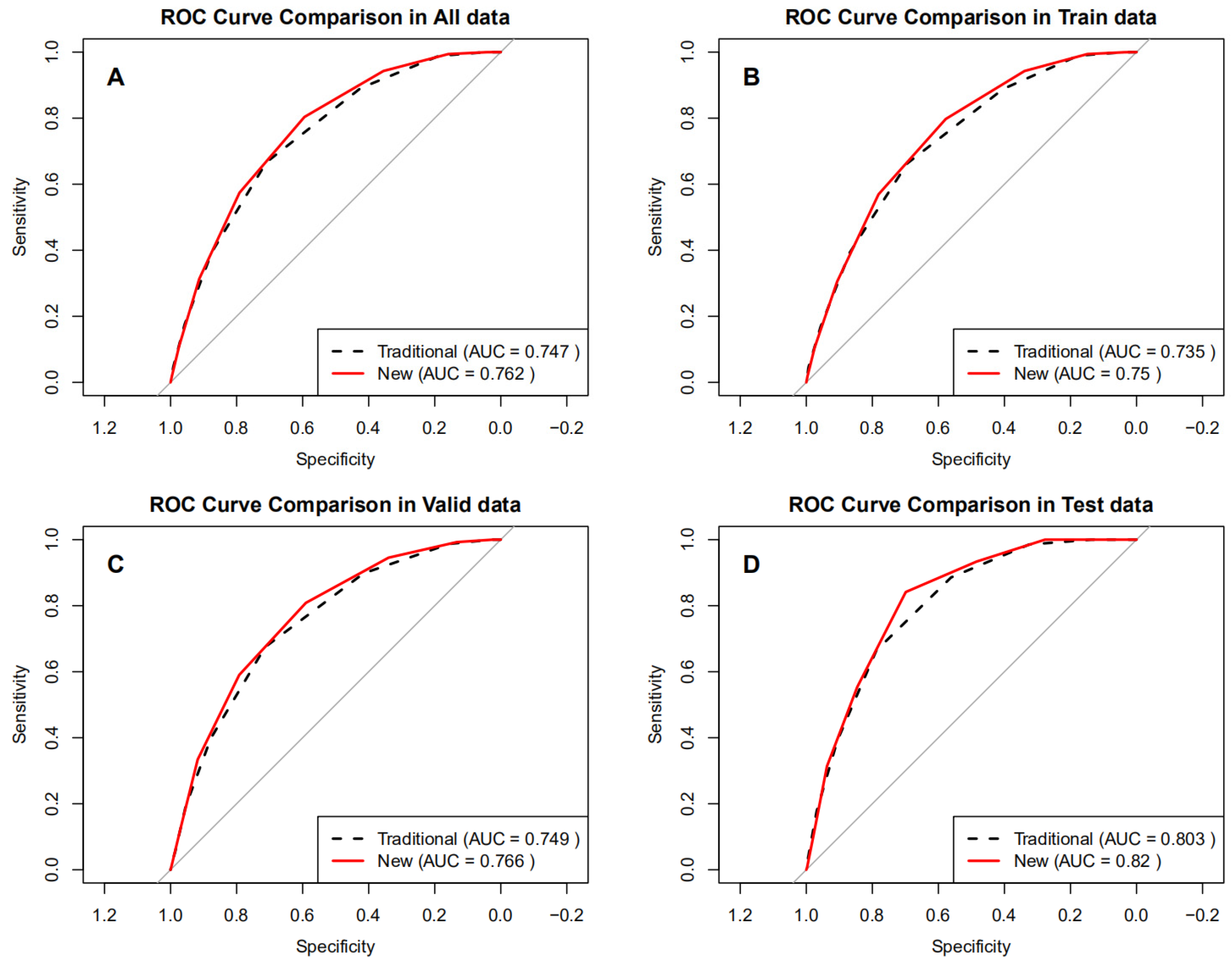
| All data | ||||||
| STOP-Bang | 0.747 (0.736–0.757) | 66.6 (65.1–68.1) | 71.0 (69.5–72.4) | 70.5 (69.0–72.0) | 67.2 (65.7–68.6) | - |
| BRI-optimized STOP-Bang | 0.762 (0.751–0.772) | 80.4 (79.1–81.6) | 59.5 (57.9–61.0) | 67.3 (66.0–68.7) | 74.4 (72.8–76.0) | 0.015 (0.011–0.019), p < 0.001 |
| Train data | ||||||
| STOP-Bang | 0.735 (0.722–0.749) | 66.3 (64.4–68.2) | 69.4 (67.5–71.3) | 70.2 (68.3–72.0) | 65.5 (63.6–67.4) | - |
| BRI-optimized STOP-Bang | 0.750 (0.737–0.763) | 79.7 (78.1–81.3) | 57.8 (55.7–59.8) | 67.2 (65.5–68.9) | 72.4 (70.3–74.5) | 0.015 (0.010–0.019), p < 0.001 |
| Valid data | ||||||
| STOP-Bang | 0.749 (0.729–0.770) | 67.4 (64.6–70.2) | 71.4 (68.5–74.2) | 72.1 (69.2–74.9) | 66.7 (63.7–69.5) | - |
| BRI-optimized STOP-Bang | 0.766 (0.746–0.786) | 80.9 (78.4–83.2) | 59.0 (55.9–62.1) | 68.4 (65.8–70.9) | 73.8 (70.5–76.8) | 0.017 (0.009–0.024), p < 0.001 |
| Test data | ||||||
| STOP-Bang | 0.803 (0.772–0.835) | 66.4 (60.5–72.0) | 78.8 (74.5–82.6) | 67.2 (61.2–72.8) | 78.2 (74.0–82.1) | - |
| BRI-optimized STOP-Bang | 0.820 (0.789–0.850) | 84.1 (79.2–88.3) | 69.9 (65.2–74.3) | 64.6 (59.4–69.6) | 87.1 (83.0–90.5) | 0.017 (0.006–0.027), p = 0.003 |
| AUC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | AUC (95% CI), p (Delong) | |
|---|---|---|---|---|---|---|
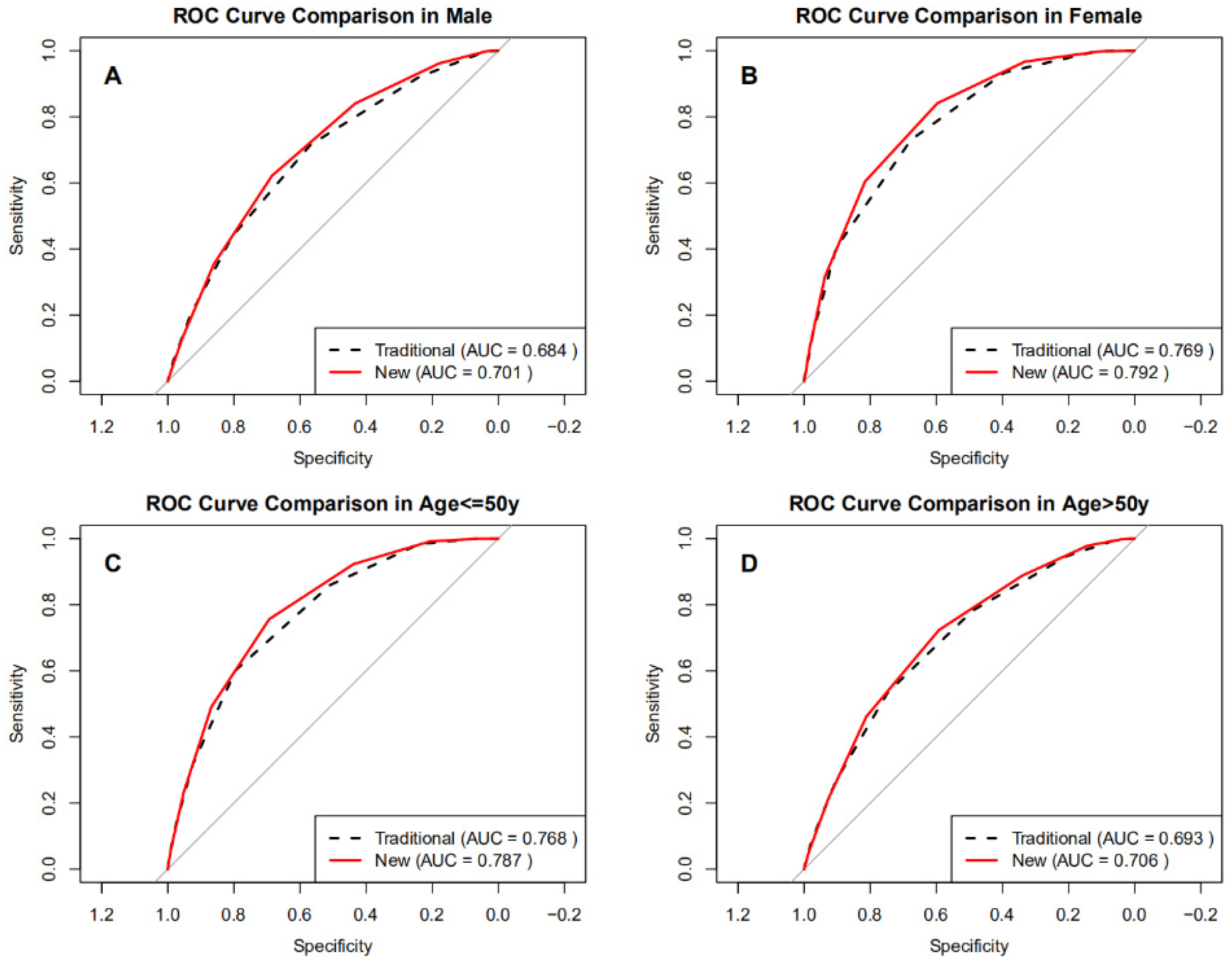
| Male | ||||||
| STOP-Bang | 0.684 (0.670–0.698) | 71.5 (69.9–73.0) | 56.8 (54.7–58.9) | 71.6 (70.0–73.1) | 56.7 (54.6–58.8) | - |
| BRI-optimized STOP-Bang | 0.701 (0.687–0.715) | 62.2 (60.5–63.8) | 68.5 (66.4–70.4) | 75.0 (73.3–76.6) | 54.3 (52.4–56.2) | 0.017 (0.011–0.022), p < 0.001 |
| Female | ||||||
| STOP-Bang | 0.769 (0.749–0.790) | 73.0 (69.3–76.5) | 67.7 (65.3–70.0) | 46.5 (43.3–49.7) | 86.7 (84.7–88.6) | - |
| BRI-optimized STOP-Bang | 0.792 (0.772–0.811) | 84.3 (81.1–87.1) | 59.6 (57.1–62.0) | 44.5 (41.6–47.4) | 90.8 (88.9–92.5) | 0.023 (0.014–0.031), p < 0.001 |
| Age ≤ 50 years | ||||||
| STOP-Bang | 0.768 (0.756–0.780) | 60.2 (58.2–62.1) | 79.5 (77.9–81.0) | 73.1 (71.1–75.0) | 68.3 (66.6–69.9) | - |
| BRI-optimized STOP-Bang | 0.787 (0.775–0.799) | 75.6 (73.9–77.3) | 69.3 (67.5–71.0) | 69.5 (67.7–71.2) | 75.5 (73.7–77.1) | 0.019 (0.014–0.024), p < 0.001 |
| Age > 50 years | ||||||
| STOP-Bang | 0.693 (0.673–0.714) | 53.5 (50.8–56.1) | 74.7 (71.9–77.3) | 73.9 (71.0–76.5) | 54.6 (51.9–57.2) | - |
| BRI-optimized STOP-Bang | 0.706 (0.685–0.726) | 72.3 (69.9–74.7) | 59.2 (56.2–62.2) | 70.3 (67.9–72.7) | 61.5 (58.4–64.6) | 0.013 (0.006–0.020), p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, N.; Ni, Y.; Luo, F. Body Roundness Index Outperforms Body Mass Index in Predicting Obstructive Sleep Apnea Severity Among Chinese Adults. J. Clin. Med. 2025, 14, 8764. https://doi.org/10.3390/jcm14248764
Tang N, Ni Y, Luo F. Body Roundness Index Outperforms Body Mass Index in Predicting Obstructive Sleep Apnea Severity Among Chinese Adults. Journal of Clinical Medicine. 2025; 14(24):8764. https://doi.org/10.3390/jcm14248764
Chicago/Turabian StyleTang, Ningchang, Yuenan Ni, and Fengming Luo. 2025. "Body Roundness Index Outperforms Body Mass Index in Predicting Obstructive Sleep Apnea Severity Among Chinese Adults" Journal of Clinical Medicine 14, no. 24: 8764. https://doi.org/10.3390/jcm14248764
APA StyleTang, N., Ni, Y., & Luo, F. (2025). Body Roundness Index Outperforms Body Mass Index in Predicting Obstructive Sleep Apnea Severity Among Chinese Adults. Journal of Clinical Medicine, 14(24), 8764. https://doi.org/10.3390/jcm14248764






