The Effectiveness of Orofacial Myofunctional Therapy in Adults with Myogenous Temporomandibular Disorders: Insights from a Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Therapeutic Intervention
- Awareness and mindfulness training: Participants were educated on physiological versus dysfunctional orofacial patterns and introduced to breathing awareness and orofacial mindfulness, both during in-office sessions and at home.
- Logopedic Myofascial Massage: Manual myofascial release techniques targeted soft-tissue restrictions in the shoulder girdle, neck, suprahyoid region, and masticatory and facial muscles. The logopedic myofascial massage used in this study represents an adaptation of classical myofascial release techniques for the orofacial region, designed and applied by a speech-language pathologist trained in manual therapy.
- Oromotor training: passive, active, and resistance exercises were applied to enhance range, precision, and strength of movements of the lips, tongue, and mandible. Exercises were adapted to individual functional capacities.
- Functional Re-education: Training focused on restoring physiological orofacial functions, including nasal–diaphragmatic breathing (Buteyko method), mandibular stabilization and dissociation, bilateral mastication, physiological swallowing and physiological resting posture of the tongue, lips, and mandible with freeway space [30,31]. These components were introduced in a progressive sequence, prioritizing breathing normalization before masticatory and swallowing re-education to support coherent neuromuscular integration.
- Habituation and self-therapy: Participants received an individualized home program to reinforce newly acquired motor patterns through daily self-massage and consolidation exercises. The habituation phase lasted approximately two weeks after completion of the in-office sessions. Participants were contacted once by phone to verify stability and continued adherence. Adherence was monitored through daily exercise logs and self-reports collected at each session. Participants were instructed to record frequency and duration of home practice to ensure consistency in exercise performance. The applied OMT protocol extended the established approach proposed by de Felício et al. which provide structured frameworks for orofacial myofunctional retraining [23].
2.4. Measurement Protocol
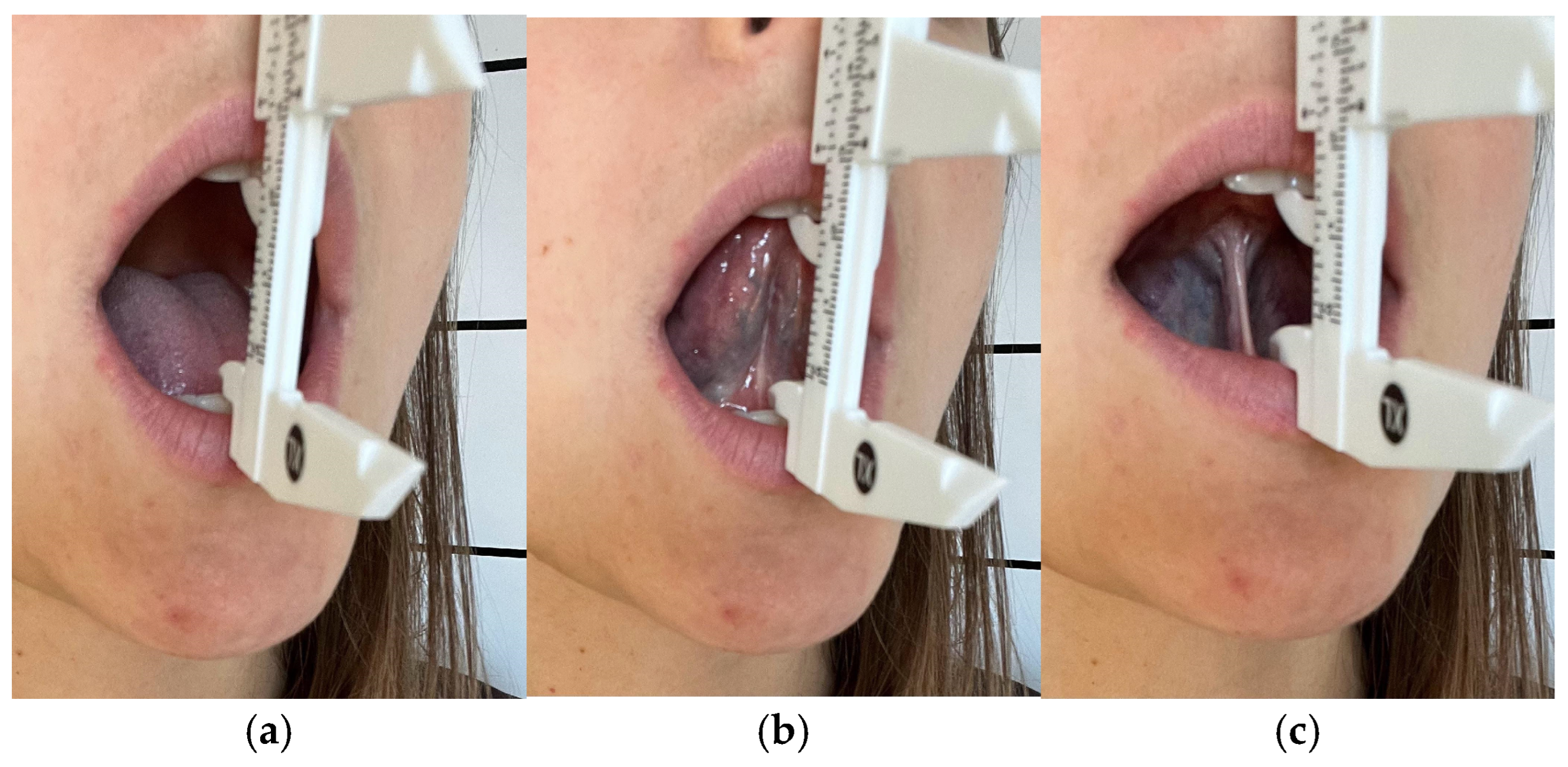
- Maximum mouth opening (MAX): The interincisal distance (mm) was measured with a caliper before and after each therapy session. (Figure 4a). Maximum mouth opening was measured actively. Participants were instructed to stop before pain occurred to ensure measurement safety.
- Tongue Range of Motion Ratio (TRMR): Two indices were recorded—TRMR-TIP (tongue tip to incisive papilla: Figure 4b) and TRMR-LPS (lingual-palatal suction: Figure 4c)—following the methods of Zaghi et al. [32]. Values were expressed in millimeters and represented the ratio between maximum mouth opening and tongue elevation tasks. Each measurement was repeated three times with participants seated upright; the mean value was used for analysis. Intraclass correlation coefficients (ICC) were calculated, indicating excellent reliability (ICC > 0.90).
- Visual Analogue Scale (VAS): Participants rated intensity on a 10-point scale at base and after the third session.
- SF-36 Questionnaire [33]: Self-reported quality of life was evaluated before the first and after the third therapy session. Lower scores indicated a better perceived quality of life. In this pilot context, the global SF-36 score was used to provide an overall proxy of health-related quality of life while minimizing respondent burden and enabling preliminary feasibility assessment.
2.5. Statistical Analysis
3. Results
3.1. Changes in Mandibular Mobility
3.2. Changes in Tongue Mobility
3.3. Pain Intensity and Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TMD | Temporomandibular Disorders |
| OMD | Orofacial Myofunctional Disorders |
| OMT | Orofacial Myofunctional Therapy |
| TRMR | Tongue Range of Motion Ratio |
| TIP | Tongue to Incisive Papilla |
| LPS | Lingual Palatal Suction |
| MAX | Maximum mouth opening |
| VAS | Visual Analogue Scale |
References
- Yost, O.; Liverman, C.T.; English, R.; Mackey, S.; Bond, E.C. (Eds.) Temporomandibular Disorders: Priorities for Research and Care. National Academies of Sciences, Engineering, and Medicine. In Definition and Scope: What are TMDs? National Academies Press: Washington, DC, USA, 2020; pp. 31–79. [Google Scholar]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef]
- Ivkovic, N.; Racic, M. Structural and Functional Disorders of the Temporomandibular Joint (Internal Disorders). In Maxillofacial Surgery and Craniofacial Deformity—Practices and Updates; IntechOpen: London, UK, 2020; pp. 1–26. [Google Scholar] [CrossRef]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion; Elsevier: St. Louis, MO, USA, 2020; Volume 8, ISBN 9780323676748. [Google Scholar]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Palla, S.; Erni, S.; Sieber, M.; Gallo, L.M. Nonfunctional tooth contact in healthy controls and patients with myogenous facial pain. J. Orofac. Pain 2007, 21, 185–193. [Google Scholar]
- Zieliński, G. Quo Vadis Temporomandibular Disorders? By 2050, the Global Prevalence of TMD May Approach 44%. J. Clin. Med. 2025, 14, 4414. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 8, 129–136. [Google Scholar] [CrossRef]
- D’Onofrio, L. Oral dysfunction as a cause of malocclusion. Orthod. Craniofacial Res. 2019, 22 (Suppl. S1), 43–48. [Google Scholar] [CrossRef]
- Maspero, C.; Prevedello, C.; Giannini, L.; Galbiati, G.; Farronato, G. Atypical swallowing: A review. Minerva Stomatol. 2014, 63, 217–227. [Google Scholar]
- Marchesi, A.; D’Apote, D.; D’Apote, A.; Ciancaglini, R.; Strohmenger, L. The correlation between temporomandibular disorders, atypical swallowing and dyslalia. Int. J. Oral Craniofacial Sci. 2019, 5, 10–14. [Google Scholar] [CrossRef]
- Ferro, K.J.; Morgano, S.M.; Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; McGarryl, T.J.; Editorial Staff Glossary of Prosthodontic Terms Committee of the Academy of Prosthodontics. The Glossary of Prosthodontic Terms Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar] [CrossRef]
- Zaghi, S.; Valcu-Pinkerton, S.; Jabara, M.; Norouz-Knutsen, L.; Govardhan, C.; Moeller, J.; Sinkus, V.; Thorsen, R.S.; Downing, V.; Camacho, M.; et al. Lingual frenuloplasty with myofunctional therapy: Exploring safety and efficacy in 348 cases. Laryngoscope Investig. Otolaryngol. 2019, 4, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Moeller, M.; Silke, A.; Weber, T.; Paskay, L.; Amat, P.; Gonçalves, E.; Bianchini, E.; Botzer, E.; Boyd, K.; Bruni, O.; et al. Consensus statement on the orofacial myofunctional assessment and therapy in patients with OSA: Proposal of an international Delphi Method process. Rev. Orthop. Dento. Faciale 2021, 55, 513–520. [Google Scholar] [CrossRef]
- Yoon, A.; Zaghi, S.; Weitzman, R.; Ha, S.; Law, C.S.; Guilleminault, C.; Liu, S.Y. Toward a functional definition of ankyloglossia: Validating current grading scales for lingual frenulum length and tongue mobility in 1052 subjects. Sleep Breath. 2017, 21, 767–775. [Google Scholar] [CrossRef]
- Hosoya, H.; Kitaura, H.; Hashimoto, T.; Ito, M.; Kinbara, M.; Deguchi, T.; Irokawa, T.; Ohisa, N.; Ogawa, H.; Takano-Yamamoto, T. Relationship between sleep bruxism and sleep respiratory events in patients with obstructive sleep apnea syndrome. Sleep Breath. 2014, 18, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Martynowicz, H.; Gac, P.; Brzecka, A.; Poreba, R.; Wojakowska, A.; Mazur, G.; Smardz, J.; Wieckiewicz, M. The Relationship between Sleep Bruxism and Obstructive Sleep Apnea Based on Polysomnographic Findings. J. Clin. Med. 2019, 8, 1653. [Google Scholar] [CrossRef]
- da Costa Lopes, A.J.; Cunha, T.C.A.; Monteiro, M.C.M.; Serra-Negra, J.M.; Cabral, L.C.; Júnior, P.C.S. Is there an association between sleep bruxism and obstructive sleep apnea syndrome? A systematic review. Sleep Breath. 2020, 24, 913–921. [Google Scholar] [CrossRef]
- Saccomanno, S.; Paskay, L.C. New Trends in Myofunctional Therapy: Occlusion, Muscles and Posture; Edi-Ermes s.r.l.: Milano, Italy, 2020; ISBN 978-88-7051-629-6. [Google Scholar]
- Debucean, D.; Mihaiu, J.; Maghiar, A.M.; Marcu, F.; Marcu, O.A. A Multidisciplinary Approach to Swallowing Rehabilitation in Patients with Forward Head Posture. Medicina 2023, 59, 1580. [Google Scholar] [CrossRef]
- Lv, R.; Liu, X.; Zhang, Y.; Dong, N.; Wang, X.; He, Y.; Yue, H.; Yin, Q. Pathophysiological mechanisms and therapeutic approaches in obstructive sleep apnea syndrome. Signal Transduct. Target. Ther. 2023, 8, 218. [Google Scholar] [CrossRef]
- Suzuki, H.; Watanabe, A.; Akihiro, Y.; Takao, M.; Ikematsu, T.; Kimoto, S.; Asano, T.; Kawara, M. Pilot study to assess the potential of oral myofunctional therapy for improving respiration during sleep. J. Prosthodont. Res. 2013, 57, 195–199. [Google Scholar] [CrossRef]
- Maria de Felício, C.; de Oliveira Melchior, M.; Rodrigues Da Silva, M.A.M. Effects of orofacial myofunctional therapy on temporomandibular disorders. Cranio—J. Craniomandib. Sleep Pract. 2010, 28, 249–259. [Google Scholar] [CrossRef] [PubMed]
- Maria de Felício, C.; de Oliveira Melchior, M.; Lúcia Pimenta Ferreira, C.; Rodrigues Da Silva, M.A.M. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. Cranio—J. Craniomandib. Sleep Pract. 2008, 26, 118–125. [Google Scholar] [CrossRef]
- Melis, M.; di Giosia, M.; Zawawi, K.H. Oral myofunctional therapy for the treatment of temporomandibular disorders: A systematic review. Cranio—J. Craniomandib. Pract. 2022, 40, 41–47. [Google Scholar] [CrossRef]
- Mulet, M.; Decker, K.L.; O Look, J.; A Lenton, P.; Schiffman, E.L. A randomized clinical trial assessing the efficacy of adding 6 × 6 exercises to self-care for the treatment of masticatory myofascial pain. J. Orofac. Pain 2007, 21, 318–328. [Google Scholar]
- Machado, B.C.Z.; Mazzetto, M.O.; Da Silva, M.A.M.R.; de Felício, C.M. Effects of oral motor exercises and laser therapy on chronic temporomandibular disorders: A randomized study with follow-up. Lasers Med. Sci. 2016, 31, 945–954. [Google Scholar] [CrossRef] [PubMed]
- Gallerano, G.; Ruoppolo, G.; Silvestri, A. Myofunctional and speech rehabilitation after orthodontic-surgical treatment of dento-maxillofacial dysgnathia. Prog. Orthod. 2012, 13, 57–68. [Google Scholar] [CrossRef]
- Migliorucci, R.R.; Abramides, D.V.M.; Rosa, R.R.; Bresaola, M.D.; Filho, H.N.; Berretin-Felix, G. Effect of Myofunctional Therapy on Orofacial Functions and Quality of Life in Individuals Undergoing Orthognathic Surgery. Int. J. Orofac. Myol. Myofunct. Ther. 2017, 43, 60–76. [Google Scholar] [CrossRef]
- Mason, R.M.; Franklin, H.; Grant, P.; Role, E.B. The Importance of the Freeway Space in Orofacial Myofunctional Therapy. Int. J. Orofac. Myol. Myofunct. Ther. 2020, 46, 37–47. [Google Scholar] [CrossRef]
- Lorenc, A.; Borowiec, A. Normative tongue resting position. A preliminary study with the use of EMA and CBCT technology. Pr. Językoznawcze 2024, 26, 69–92. [Google Scholar] [CrossRef]
- Zaghi, S.; Shamtoob, S.; Peterson, C.; Christianson, L.; Valcu-Pinkerton, S.; Peeran, Z.; Fung, B.; Kwok-Keung Ng, D.; Jagomagi, T.; Archambault, N.; et al. Assessment of posterior tongue mobility using lingual-palatal suction: Progress towards a functional definition of ankyloglossia. J. Oral. Rehabil. 2021, 48, 692–700. [Google Scholar] [CrossRef]
- Tylka, J.; Piotrowicz, R. Quality of life SF-36 questionnaire—The Polish version. Kardiol. Pol. 2009, 67, 1166–1169. [Google Scholar]
- Zieliński, G.; Więckiewicz, M. New effect size and sample size guidelines in dentistry. Dent. Med. Probl. 2025, 62, 907–917. [Google Scholar] [CrossRef]
- Avivi-Arber, L.; Martin, R.; Lee, J.C.; Sessle, B.J. Face sensorimotor cortex and its neuroplasticity related to orofacial sensorimotor functions. Arch. Oral Biol. 2011, 56, 1440–1465. [Google Scholar] [CrossRef] [PubMed]






| Measurement | Median | Minimum | Maximum | SD |
|---|---|---|---|---|
| VAS before OMT | 7 | 5 | 9 | 1.15 |
| VAS after OMT | 4 | 1 | 7 | 1.38 |
| Measurement | Median | Minimum | Maximum | SD |
|---|---|---|---|---|
| SF-36 before OMT | 28 | 21 | 47 | 6.83 |
| SF-36 after OMT | 19 | 13 | 38 | 6.83 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czarnecka, P.; Bujan, B.; Pekacka-Egli, A.M. The Effectiveness of Orofacial Myofunctional Therapy in Adults with Myogenous Temporomandibular Disorders: Insights from a Pilot Study. J. Clin. Med. 2025, 14, 8718. https://doi.org/10.3390/jcm14248718
Czarnecka P, Bujan B, Pekacka-Egli AM. The Effectiveness of Orofacial Myofunctional Therapy in Adults with Myogenous Temporomandibular Disorders: Insights from a Pilot Study. Journal of Clinical Medicine. 2025; 14(24):8718. https://doi.org/10.3390/jcm14248718
Chicago/Turabian StyleCzarnecka, Paulina, Bartosz Bujan, and Anna Maria Pekacka-Egli. 2025. "The Effectiveness of Orofacial Myofunctional Therapy in Adults with Myogenous Temporomandibular Disorders: Insights from a Pilot Study" Journal of Clinical Medicine 14, no. 24: 8718. https://doi.org/10.3390/jcm14248718
APA StyleCzarnecka, P., Bujan, B., & Pekacka-Egli, A. M. (2025). The Effectiveness of Orofacial Myofunctional Therapy in Adults with Myogenous Temporomandibular Disorders: Insights from a Pilot Study. Journal of Clinical Medicine, 14(24), 8718. https://doi.org/10.3390/jcm14248718







