Analgesia for Upper Abdominal Surgery, a Scoping Review of the Current Fascial Plane Block Techniques
Abstract
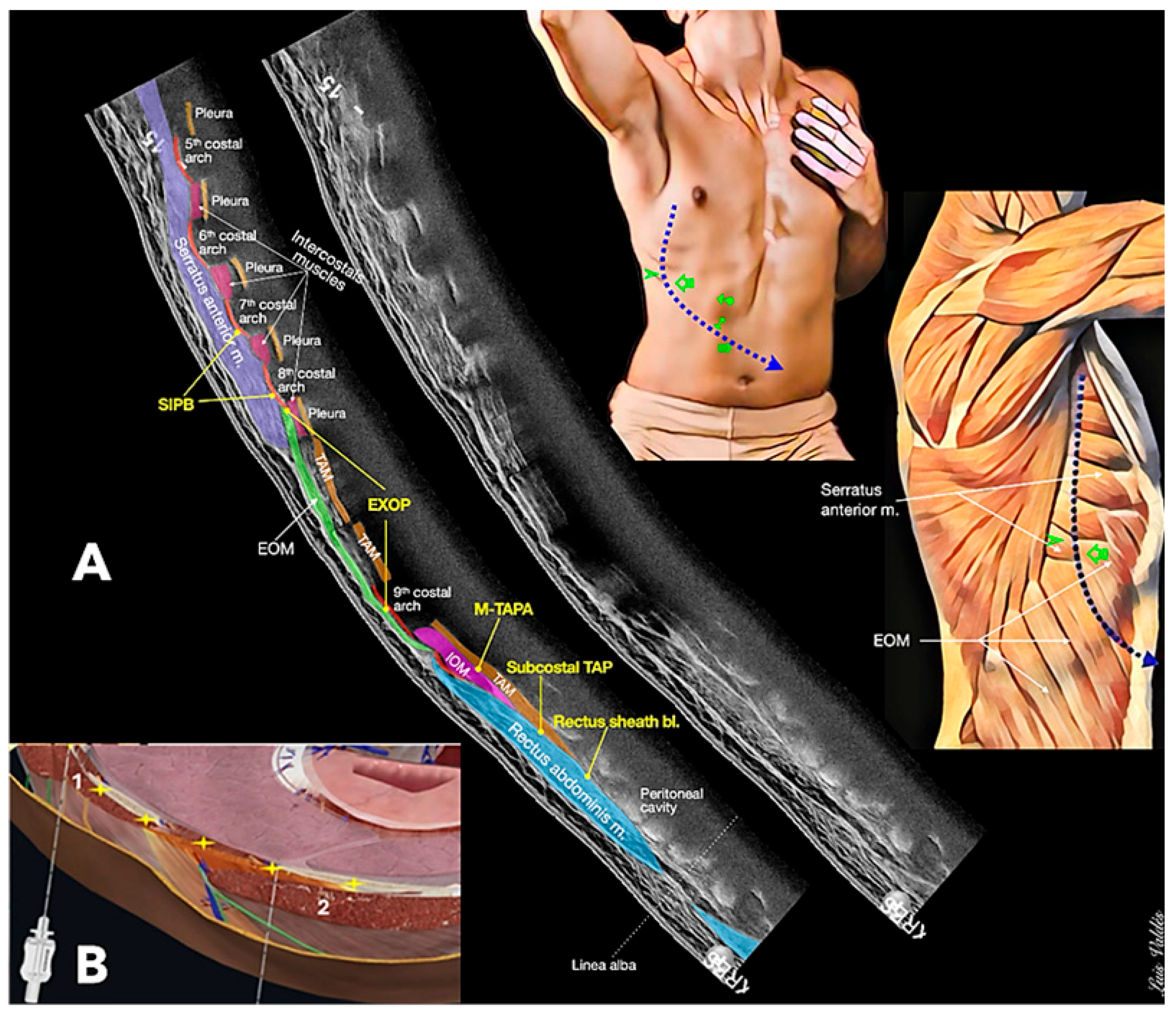
1. Introduction
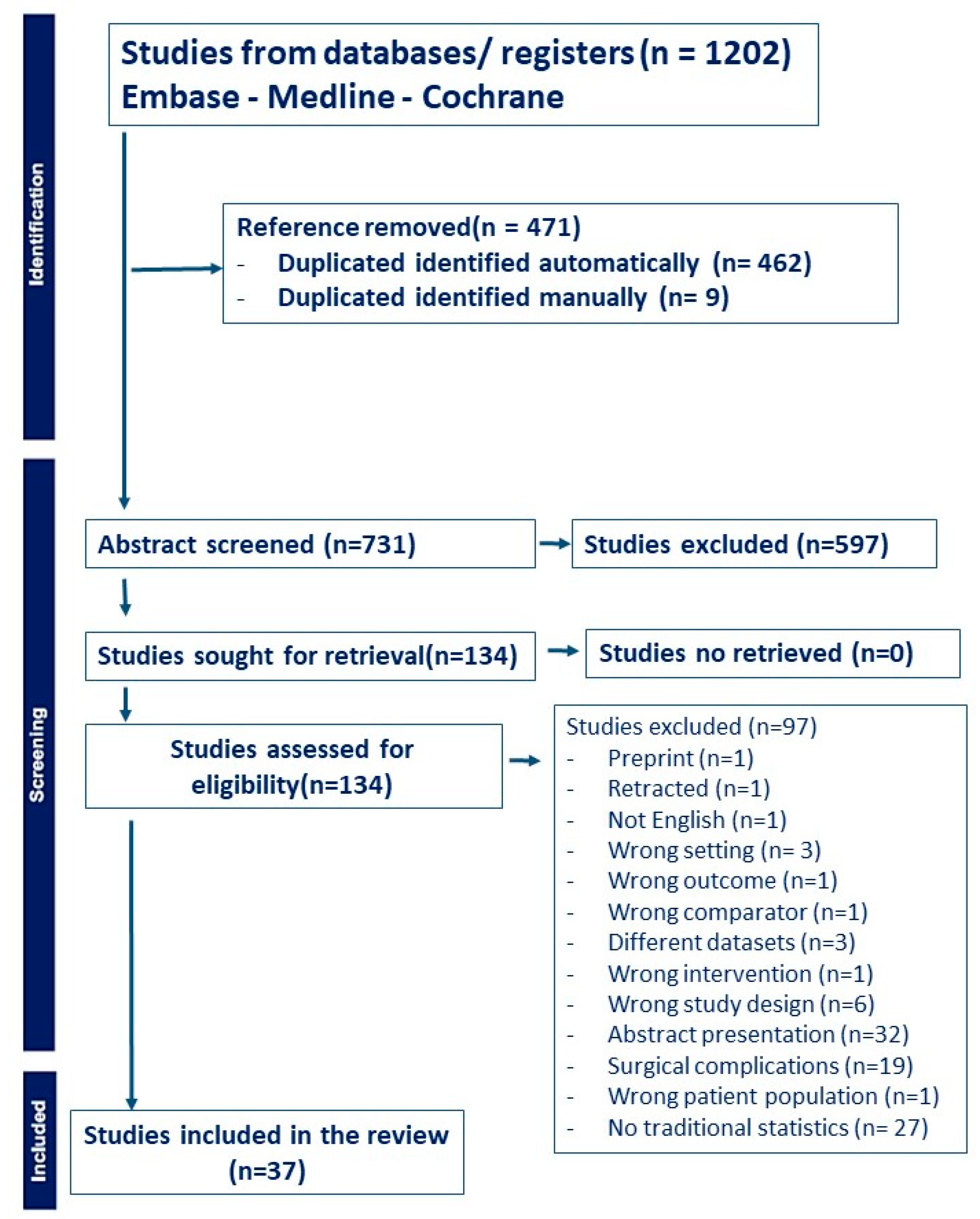
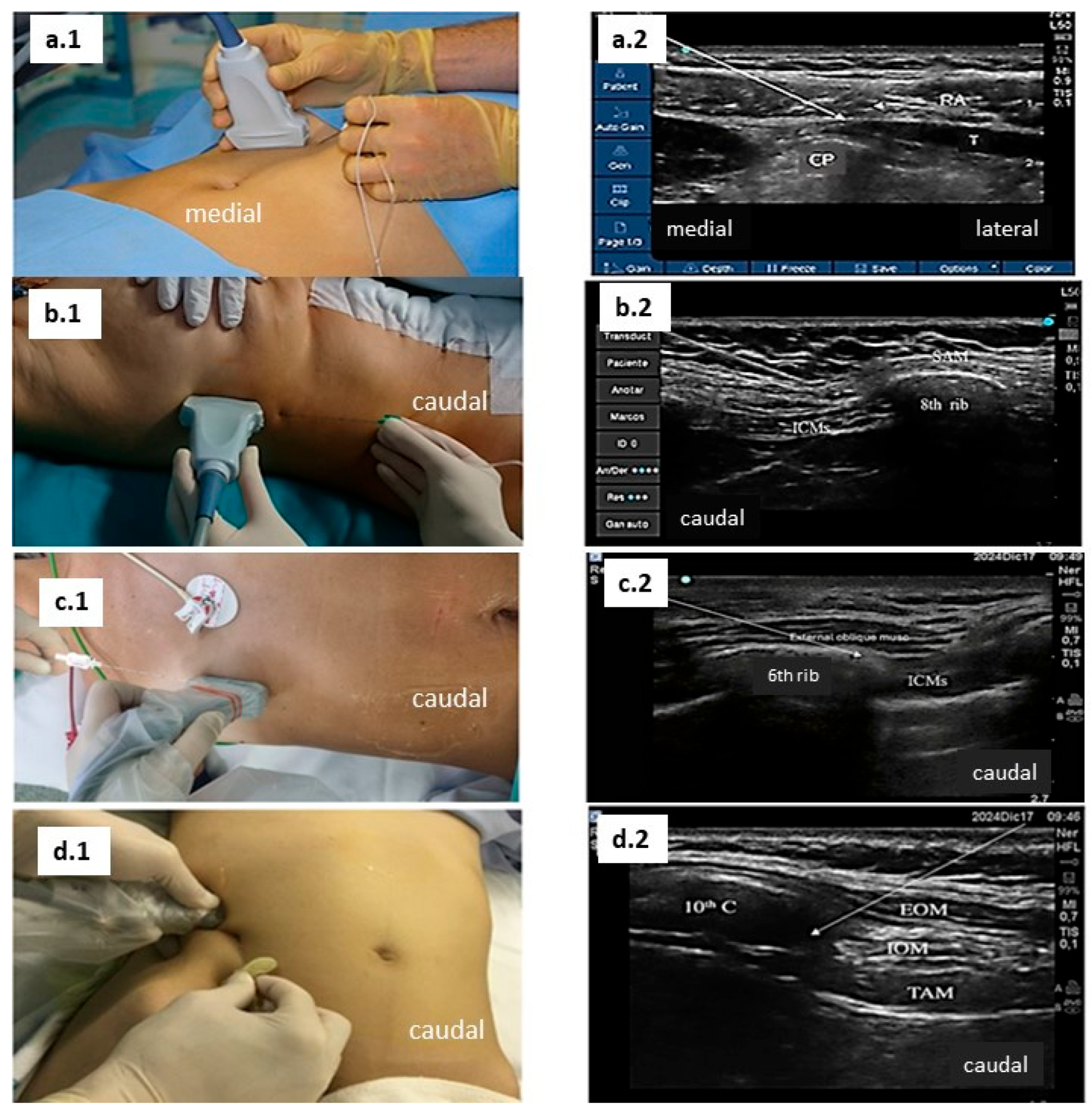
2. Materials and Methods
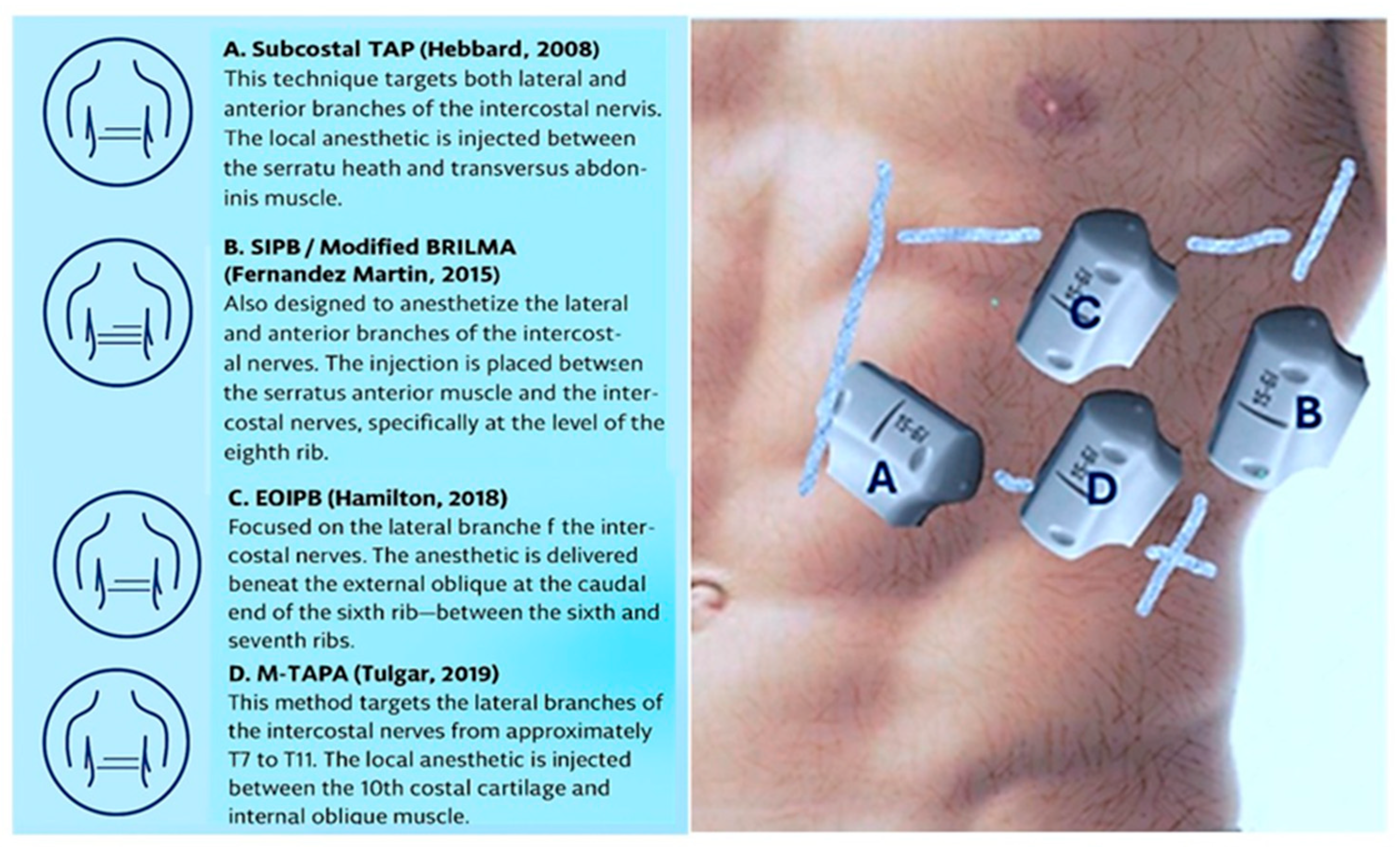
3. Results
4. Discussion
5. Considerations for Future Research and Practice
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| T | thoracic |
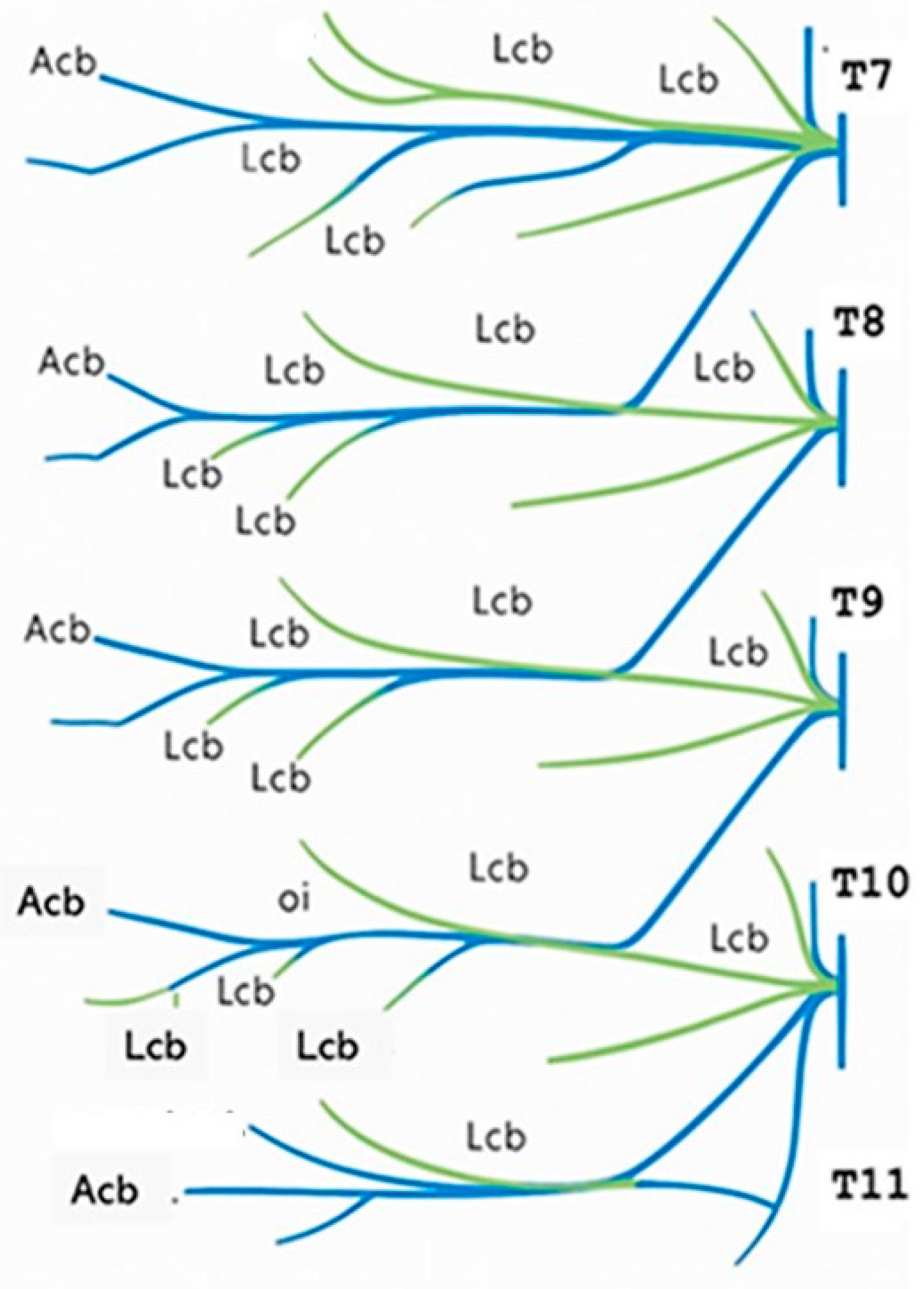
| Lcb | lateral cutaneous branches |
| acb | anterior cutaneous branches |
| ASRA-ESRA | American society regional anaesthesia–European society regional anaesthesia |
| STAP | subcostal abdominis plane block |
| OSTAP | oblique subcostal transversus abdominis plane |
| IFPB | intercostal fascial plane block |
| ‘modified BRILMA’ | block of the rami of the intercostal nerves in the middle axillary line |
| SIPB | low serratus–intercostal interfascial plane block |
| TAPA | the thoraco-abdominal perichondrial approach/MTAPA modified the thoraco-abdominal perichondrial approach |
| LA | local anaesthestic |
| EOIB | external oblique intercostal block |
| QLB | quadratus lumborum block |
| p | patients |
| PCA | patient control activation |
| IV | intravenous |
References
- Mariano, E.R.; Dickerson, D.M.; Szokol, J.W.; Harned, M.; Mueller, J.T.; Philip, B.K.; Baratta, J.L.; Gulur, P.; Robles, J.; Schroeder, K.M.; et al. A multisociety organizational consensus process to define guiding principles for acute perioperative pain management. Reg. Anesth. Pain Med. 2022, 47, 118–127. [Google Scholar] [CrossRef]
- Lee, B.H.; Kumar, K.K.; Wu, E.C.; Wu, C.L. Role of regional anesthesia and analgesia in the opioid epidemic. Reg. Anesth. Pain Med. 2019, 44, 492–493. [Google Scholar] [CrossRef]
- Seeras, K.; Qasawa, R.N.; Ju, R.; Prakash, S. Anatomy, Abdomen and Pelvis: Anterolateral Abdominal Wall. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar] [PubMed]
- Boezaart, A.P.; Smith, C.R.; Chembrovich, S.; Zasimovich, Y.; Server, A.; Morgan, G.; Theron, A.; Booysen, K.; Reina, M.A. Visceral versus somatic pain: An educational review of anatomy and clinical implications. Reg. Anesth. Pain Med. 2021, 46, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Lohmöller, K.; Carstensen, V.; Pogatzki-Zahn, E.M.; Freys, S.M.; Weibel, S.; Schnabel, A. Regional anaesthesia for postoperative pain management following laparoscopic, visceral, non-oncological surgery a systematic review and meta-analysis. Surg. Endosc. 2024, 38, 1844–1866. [Google Scholar] [CrossRef] [PubMed]
- El-Boghdadly, K.; Wolmarans, M.; Stengel, A.D.; Albrecht, E.; Chin, K.J.; Elsharkawy, H.; Kopp, S.; Mariano, E.R.; Xu, J.L.; Adhikary, S.; et al. Standardizing nomenclature in regional anesthesia: An ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg. Anesth. Pain Med. 2021, 46, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.W.; Kim, C.S.; Choi, K.T.; Jeong, S.M.; Kim, D.H.; Lee, J.H. Preoperative versus Postoperative Rectus Sheath Block for Acute Postoperative Pain Relief after Laparoscopic Cholecystectomy: A Randomized Controlled Study. J. Clin. Med. 2019, 8, 1018. [Google Scholar] [CrossRef]
- Chen, C.K.; Tan, P.C.; Phui, V.E.; Teo, S.C. A comparison of analgesic efficacy between oblique subcostal transversus abdominis plane block and intravenous morphine for laparascopic cholecystectomy. A prospective randomized controlled trial. Korean J. Anesthesiol. 2013, 64, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Oksar, M.; Koyuncu, O.; Turhanoglu, S.; Temiz, M.; Oran, M.C. Transversus abdominis plane block as a component of multimodal analgesia for laparoscopic cholecystectomy. J. Clin. Anesth. 2016, 34, 72–78. [Google Scholar] [CrossRef]
- Fernández, M.T.; López, S.; Aguirre, J.A.; Andrés, J.; Ortigosa, E. Serratus intercostal interfascial plane block in supraumbilical surgery: A prospective randomized comparison. Minerva Anestesiol. 2020, 87, 165–173. [Google Scholar] [CrossRef]
- Saravanan, R.; Venkatraman, R.; Karthika, U. Comparison of Ultrasound-Guided Modified BRILMA Block with Subcostal Transversus Abdominis Plane Block for Postoperative Analgesia in Laparoscopic Cholecystectomy—A Randomized Controlled Trial. Local Reg. Anesth. 2021, 14, 109–116. [Google Scholar] [CrossRef]
- Kara, Y.B.; Ital, I.; Ertekin, S.C.; Yol, S.; Yardimci, S. Ultrasonography Guided Modified BRILMA (Blocking the Cutaneous Branches of Intercostal Nerves in the Middle Axillary Line) Block in Bariatric Surgery. J. Laparoendosc. Adv. Surg. Tech. A 2023, 33, 1141–1145. [Google Scholar] [CrossRef]
- Amin, S.R.; Khedr, A.N.; Elhadad, M.A. External oblique intercostal plane block versus subcostal transversus abdominis plane block for pain control in supraumbilical surgeries: A randomised controlled clinical trial. S. Afr. J. Anaesth. Analg. 2024, 30, 112–117. [Google Scholar] [CrossRef]
- Rajitha, A.; Kandukuru, K.C.; Williams, A.I.; Deepthi, G.S.; Devaram, V.; Aarumulla, S.P. Efficacy of External Oblique Intercostal Plane Block versus Transversus Abdominis Plane Block for Postoperative Analgesia in Laparoscopic Upper Abdominal Surgeries: A Randomised Clinical Study. J. Clin. Diagn. Res. 2024, 18, UC17–UC22. [Google Scholar] [CrossRef]
- Doymus, O.; Ahiskalioglu, A.; Kaciroglu, A.; Bedir, Z.; Tayar, S.; Yeni, M.; Karadeniz, E. External Oblique Intercostal Plane Block Versus Port-Site Infiltration for Laparoscopic Sleeve Gastrectomy: A Randomized Controlled Study. Obes. Surg. 2024, 34, 1826–1833. [Google Scholar] [CrossRef]
- Gangadhar, V.; Gupta, A.; Saini, S. Comparison of analgesic efficacy of combined external oblique intercostal and rectus sheath block with local infiltration analgesia at port site in patients undergoing laparoscopic cholecystectomy: A randomized controlled trial. Anesth. Pain Med. 2024, 19, 247–255. [Google Scholar] [CrossRef]
- Mehmet Selim, Ç.; Halide, S.; Erkan Cem, Ç.; Onur, K.; Sedat, H.; Senem, U. Efficacy of Unilateral External Oblique Intercostal Fascial Plane Block Versus Subcostal TAP Block in Laparoscopic Cholecystectomy: Randomized, Prospective Study. Surg. Innov. 2024, 31, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Ozel, E.S.; Kaya, C.; Turunc, E.; Ustun, Y.B.; Cebeci, H.; Dost, B. Analgesic efficacy of the external oblique intercostal fascial plane block on postoperative acute pain in laparoscopic sleeve gastrectomy: A randomized controlled trial. Korean J. Anesthesiol. 2025, 78, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Ciftci, B.; Alver, S.; Gölboyu, B.E.; Haksal, M.C.; Tulgar, S.; De Cassai, A.; Alici, H.A. A Comparison of Two Fascial Plane Blocks for Abdominal Analgesia in Laparoscopic Cholecystectomy Surgery (M-TAPA vs. External Oblique Intercostal Plane Block): A Prospective Randomized Study. J. Clin. Med. 2025, 14, 3050. [Google Scholar] [CrossRef]
- Hebbard, P. Subcostal Transversus Abdominis Plane Block Under Ultrasound Guidance. Anesth. Analg. 2008, 106, 674–675. [Google Scholar] [CrossRef]
- Fernández Martín, M.T.; López Álvarez, S.; Mozo Herrera, G.; Platero Burgos, J.J. Bloqueo fascial ecoguiado de las ramas cutáneas de los nervios intercostales: Una buena alternativa analgésica para la cirugía abierta de vesícula biliar [Ultrasound-guided cutaneous intercostal branches nerves block: A good analgesic alternative for gallbladder open surgery]. Rev. Esp. Anestesiol. Reanim. 2015, 62, 580–584. (In Spanish) [Google Scholar]
- Hamilton, D.L.; Manickam, B.P.; Wilson, M.A.J.; Abdel Meguid, E. External oblique fascial plane block. Reg. Anesth. Pain Med. 2019, 44, 528–529. [Google Scholar] [CrossRef] [PubMed]
- Tulgar, S.; Selvi, O.; Thomas, D.T.; Deveci, U.; Özer, Z. Modified thoracoabdominal nerves block through perichondrial approach (M-TAPA) provides effective analgesia in abdominal surgery and is a choice for opioid sparing anesthesia. J. Clin. Anesth. 2019, 55, 109. [Google Scholar] [CrossRef] [PubMed]
- Elsharkawy, H.; Kolli, S.; Soliman, L.M.; Seif, J.; Drake, R.L.; Mariano, E.R.; El-Boghdadly, K. The External Oblique Intercostal Block: Anatomic Evaluation and Case Series. Pain Med. 2021, 22, 2436–2442. [Google Scholar] [CrossRef] [PubMed]
- Hollmén, A.; Saukkonen, J. Postoperative elimination of pain following upper abdominal surgery. Anesthetics, intercostal block and epidural anesthesia and their effect on respiration. Der Anaesthesist 1969, 18, 298–303. [Google Scholar]
- Soliz, J.M.; Lipski, I.; Hancher-Hodges, S.; Speer, B.B.; Popat, K. Subcostal Transverse Abdominis Plane Block for Acute Pain Management: A Review. Anesth. Pain Med. 2017, 7, e12923. [Google Scholar] [CrossRef]
- Shin, H.J.; Oh, A.Y.; Baik, J.S.; Kim, J.H.; Han, S.H.; Hwang, J.W. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: A randomized, controlled, observer-blinded study. Minerva Anestesiol. 2014, 80, 185–193. [Google Scholar]
- Basaran, B.; Basaran, A.; Kozanhan, B.; Kasdogan, E.; Eryilmaz, M.A.; Ozmen, S. Analgesia and respiratory function after laparoscopic cholecystectomy in patients receiving ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: A randomized double-blind study. Med. Sci. Monit. 2015, 21, 1304–1312. [Google Scholar]
- Emile, S.H.; Elfeki, H.; Elbahrawy, K.; Sakr, A.; Shalaby, M. Ultrasound-guided versus laparoscopic-guided subcostal transversus abdominis plane (TAP) block versus No TAP block in laparoscopic cholecystectomy; a randomized double-blind controlled trial. Int. J. Surg. 2022, 101, 106639. [Google Scholar] [CrossRef]
- Jung, J.; Jung, W.; Ko, E.Y.; Chung, Y.H.; Koo, B.S.; Chung, J.C.; Kim, S.H. Impact of Bilateral Subcostal Plus Lateral Transversus Abdominis Plane Block on Quality of Recovery After Laparoscopic Cholecystectomy: A Randomized Placebo-Controlled Trial. Anesth. Analg. 2021, 133, 1624–1632. [Google Scholar] [CrossRef]
- Di Mauro, D.; Reece-Smith, A.; Njere, I.; Hubble, S.; Manzelli, A. The Effect of Postoperative Analgesia on the Day-Case Rate of Laparoscopic Cholecystectomy: A Randomised Pilot Study of the Laparoscopic-Assisted Right Subcostal Transversus Abdominis Plane Block plus Local Anaesthetic Wound Infiltration versus Local Anaesthetic Wound Infiltration only. Med. Princ. Pract. 2024, 33, 545–554. [Google Scholar]
- Houben, A.M.; Moreau, A.J.; Detry, O.M.; Kaba, A.; Joris, J.L. Bilateral subcostal transversus abdominis plane block does not improve the postoperative analgesia provided by multimodal analgesia after laparoscopic cholecystectomy: A randomised placebo-controlled trial. Eur. J. Anaesthesiol. 2019, 36, 772–777. [Google Scholar] [CrossRef]
- Altıparmak, B.; Korkmaz Toker, M.; Uysal, A.I.; Kuşçu, Y.; Gümüş Demirbilek, S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: Randomized, controlled trial. J. Clin. Anesth. 2019, 57, 31–36. [Google Scholar] [CrossRef]
- Ozdemir, H.; Araz, C.; Karaca, O.; Turk, E. Comparison of Ultrasound-Guided Erector Spinae Plane Block and Subcostal Transversus Abdominis Plane Block for Postoperative Analgesia after Laparoscopic Cholecystectomy: A Randomized, Controlled Trial. J. Investig. Surg. 2022, 35, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Song, D.; Wu, Z.; Lin, C.; Fu, W.; Wang, F. Comparison of postoperative analgesic effects of ultrasound-guided intercostal nerve block and transversus abdominis plane block in patients undergoing laparoscopic cholecystectomy: Randomized clinical trial. BJS Open 2025, 9, zraf022. [Google Scholar] [CrossRef] [PubMed]
- Baytar, Ç.; Yılmaz, C.; Karasu, D.; Topal, S. Comparison of Ultrasound-Guided Subcostal Transversus Abdominis Plane Block and Quadratus Lumborum Block in Laparoscopic Cholecystectomy: A Prospective, Randomized, Controlled Clinical Study. Pain Res. Manag. 2019, 2019, 2815301. [Google Scholar] [CrossRef]
- Güngör, H.; Ciftci, B.; Alver, S.; Gölboyu, B.E.; Ozdenkaya, Y.; Tulgar, S. Modified thoracoabdominal nerve block through perichondrial approach (M-TAPA) vs local infiltration for pain management after laparoscopic cholecystectomy surgery: A randomized study. J. Anesth. 2023, 37, 254–260. [Google Scholar] [CrossRef]
- Korkusuz, M.; Basaran, B.; Et, T.; Bilge, A.; Yarimoglu, R.; Yildirim, H. Bilateral external oblique intercostal plane block (EOIPB) in patients undergoing laparoscopic cholecystectomy: A randomized controlled trial. Saudi Med. J. 2023, 44, 1037–1046. [Google Scholar] [CrossRef] [PubMed]
- Arı, D.E.; Ar, A.Y.; Karip, C.S.; Köksal, C.; Aydın, M.T.; Gazi, M.; Akgün, F. Ultrasound-guided subcostal-posterior transversus abdominis plane block for pain control following laparoscopic sleeve gastrectomy. Saudi Med. J. 2017, 38, 1224–1229. [Google Scholar] [CrossRef]
- Albrecht, E.; Kirkham, K.R.; Endersby, R.V.; Chan, V.W.; Jackson, T.; Okrainec, A.; Penner, T.; Jin, R.; Brull, R. Ultrasound-guided transversus abdominis plane (TAP) block for laparoscopic gastric-bypass surgery: A prospective randomized controlled double-blinded trial. Obes. Surg. 2013, 23, 1309–1314. [Google Scholar] [CrossRef]
- Coşkun, M.; Yardimci, S.; Arslantaş, M.K.; Altun, G.T.; Uprak, T.K.; Kara, Y.B.; Cingi, A. Subcostal Transversus Abdominis Plane Block for Laparoscopic Sleeve Gastrectomy, Is It Worth the Time? Obes. Surg. 2019, 29, 3188–3194. [Google Scholar] [CrossRef]
- Nie, B.Q.; Niu, L.X.; Yang, E.; Yao, S.L.; Yang, L. Effect of Subcostal Anterior Quadratus Lumborum Block vs. Oblique Subcostal Transversus Abdominis Plane Block after Laparoscopic Radical Gastrectomy. Curr. Med. Sci. 2021, 41, 974–980. [Google Scholar] [CrossRef]
- Abdelhamid, B.M.; Khaled, D.; Mansour, M.A.; Hassan, M.M. Comparison between the ultrasound-guided erector spinae block and the subcostal approach to the transversus abdominis plane block in obese patients undergoing sleeve gastrectomy: A randomized controlled trial. Minerva Anestesiol. 2020, 86, 816–826. [Google Scholar] [CrossRef]
- Mu, T.; Chen, K.; Xu, Y.; Hao, Y.; Liu, D.; Wei, K. Comparison Between Erector Spinae Plane Block at T9 Level and Transversus Abdominis Plane Block for Postoperative Analgesia and Recovery in Patients with Obesity Undergoing Laparoscopic Sleeve Gastrectomy: A Randomized Controlled Trial. Obes. Surg. 2025, 35, 2249–2263. [Google Scholar] [CrossRef]
- Fernandez Martin, M.T.; Matesanz, M.G.; Andres, J.; Muñoz, H.; Muñoz, M.F.; Fadrique, A.; Castillo, P.; Casas, P.; Lopez, S. Intercostal serratus plane block versus posterior quadratus lumbar block in laparoscopic nephrectomy: A randomized, controlled, double-blind study. Rev. Esp. Anestesiol. Reanim. 2025, 72, 501728. [Google Scholar] [CrossRef]
- Wu, Y.; Liu, F.; Tang, H.; Wang, Q.; Chen, L.; Wu, H.; Zhang, X.; Miao, J.; Zhu, M.; Hu, C.; et al. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth. Analg. 2013, 117, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Erdogan, M.A.; Ozgul, U.; Uçar, M.; Yalin, M.R.; Colak, Y.Z.; Çolak, C.; Toprak, H.I. Effect of transversus abdominis plane block in combination with general anesthesia on perioperative opioid consumption, hemodynamics, and recovery in living liver donors: The prospective, double-blinded, randomized study. Clin. Transplant. 2017, 31, e12931. [Google Scholar] [CrossRef] [PubMed]
- Kıtlık, A.; Erdogan, M.A.; Ozgul, U.; Aydogan, M.S.; Ucar, M.; Toprak, H.I.; Colak, C.; Durmus, M. Ultrasound-guided transversus abdominis plane block for postoperative analgesia in living liver donors: A prospective, randomized, double-blinded clinical trial. J. Clin. Anesth. 2017, 37, 103–107. [Google Scholar] [CrossRef]
- Maeda, A.; Shibata, S.C.; Wada, H.; Marubashi, S.; Kamibayashi, T.; Eguchi, H.; Fujino, Y. The efficacy of continuous subcostal transversus abdominis plane block for analgesia after living liver donation: A retrospective study. J. Anesth. 2016, 30, 39–46, Erratum in J. Anesth. 2016, 30, 546. [Google Scholar] [CrossRef]
- Assefi, M.; Trillaud, E.; Vezinet, C.; Duceau, B.; Baron, E.; Pons, S.; Clavieras, N.; Quemeneur, C.; Selves, A.; Scatton, O.; et al. Subcostal transversus abdominis plane block for postoperative analgesia in liver transplant recipients: A before-and-after study. Reg. Anesth. Pain Med. 2023, 48, 352–358. [Google Scholar] [CrossRef]
- Mostafa, M.; Mousa, M.S.; Hasanin, A.; Arafa, A.S.; Raafat, H.; Ragab, A.S. Erector spinae plane block versus subcostal transversus abdominis plane block in patients undergoing open liver resection surgery: A randomized controlled trial. Anaesth. Crit. Care Pain Med. 2023, 42, 101161. [Google Scholar] [CrossRef]
- Jiang, F.; Wu, A.; Liang, Y.; Huang, H.; Tian, W.; Chen, B.; Liu, D. Assessment of Ultrasound-Guided Continuous Low Serratus Anterior Plane Block for Pain Management After Hepatectomy: A Randomized Controlled Trial. J. Pain Res. 2023, 16, 2383–2392. [Google Scholar] [CrossRef]
- Yi, S.; Zhang, X.; Song, Y.; Wang, X.; Gao, H.; Yuan, Z.; Kong, M. The impact of external oblique intercostal block on early postoperative pain and recovery in patients undergoing J-shaped incisions for upper abdominal surgery: A single-center prospective randomized controlled study. BMC Anesthesiol. 2025, 25, 158. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.H.; Abdallah, M.W.; Mahrous, A.M.; Ali, N.A. Quadratus lumborum block (transmuscular approach) versus transversus abdominis plane block (unilateral subcostal approach) for perioperative analgesia in patients undergoing open nephrectomy: A randomized, double-blinded, controlled trial. Braz. J. Anesthesiol. 2021, 71, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Niraj, G.; Kelkar, A.; Jeyapalan, I.; Graff-Baker, P.; Williams, O.; Darbar, A.; Maheshwaran, A.; Powell, R. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia 2011, 66, 465–471. [Google Scholar] [CrossRef]
- Shrey, S.; Sinha, C.; Kumar, A.; Kumar, A.; Kumar, A.; Nambiar, S. Comparison of analgesic efficacy of ultrasound-guided external oblique intercostal plane block and subcostal transversus abdominis plane block in patients undergoing upper abdominal surgery: A randomised clinical study. Indian J. Anaesth. 2024, 68, 965–970. [Google Scholar]
- Srinivasaraghavan, N.; Seshadri, R.A.; Ramasamy, Y.; Raj, P.; Chockalingam, P.; Sankar, P.R.P.; Modh, V.; Ramakrishnan, B. Bilateral External Oblique Intercostal Plane Block Versus Intravenous Morphine for Rescue Pain Relief in Patients with Epidurals Following Upper Abdominal Surgeries: A Randomized Controlled Trial. AA Pract. 2025, 19, e02019. [Google Scholar] [CrossRef]
- Mamoun, M.A.; Alrefaey, A.K.; Abo-Zeid, M.A. Continuous Serratus—Intercostal Plane Block for Perioperative Analgesia in Upper Abdominal Surgeries: A Prospective Randomized Controlled Study. Turk. J. Anaesthesiol. Reanim. 2023, 51, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, D.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
| Author Year | Study (N° Patients) | Fascial Block | Surgery | Results |
|---|---|---|---|---|
| Hye-Won Jeong [7] (2019) | RCT (200) | Rectus Sheath pre/post | Laparoscopic Cholecystectomy | Pre-RSB less fentanyl at 24 h (210/267 µg) (0.02) |
| Chen CK [8] (2013) | RCT (40) | OSTAP/Control | Laparoscopic Cholecystectomy | OSTAP: Shorter extubation time (0.021)
|
| Oksar M [9] (2016) | RCT (60) | OSTAP/TAP/Control | Cholecystectomy | OSTAP < TAP < Control VAS (0.01) |
| Fernandez MT [10] (2021) | RCT (102) | SIPB/Control | Upper Abdomial Surgery (Open) | SIPB: Efficient analgesia:
|
| Saravanan [11] (2021) | RCT (60) | Modified BRILMA/STAP | Laparoscopic Cholecystectomy | Modified BRILMA (SIPB) = subcostal TAP
|
| Kara Y [12] (2023) | COHORT (30) | Modified BRILMA/Port | Bariatric Surgery | Modified BRILMA alternative to port LA
|
| Amin [13] (2024) | RCT (63) | EOIB/STAP/Control | Supra-Umbilical Surgeries |
|
| Rajitha A [14] (2024) | RCT (100) | EOIB/STAP | Laparoscopic Upper Abdominal Surgeries | EOIB is superior to STAP
|
| Doymus [15] (2024) | RCT (70) | EOIB/Port | Laparoscopic Sleeve Gastrectomy | EOIB/port: 12 h VAS 3.9/4.7 (>0.08)
|
| Gangadhar V [16] (2024) | RCT (70) | EOIB + RS/LIA | Laparoscopic Cholecystectomy | EOIB + RSB superior to LIA: pain scores and rescue analgesia (<0.001) |
| Mehmet C [17] (2024) | RCT (73) | EOIB/OSTAP | Laparoscopic Cholecystectomy | EOIB = OSTAP block: VAS scores and first analgesia (>0.05) |
| Ozel ES [18] (2024) | RCT (60) | EIOB/Control | Laparoscopic Sleeve Gastrectomy | EOIB/control
|
| Ciftci [19] (2025) | RCT (60) | MTAPA/EOIB | Laparoscopic Cholecystectomy | M-TAPA = EOIB NRS 24 h (0/0)
|
| Surgery | Block | Author | Sample Size | Results |
|---|---|---|---|---|
| Cholecystectomy | -STAP | Shin et al. [27] | 53 p | STAP block better analgesia than the TAP block |
| -STAP | Basaran et al. [28] | 76 p | Significant improvement in respiratory function and better pain relief | |
| -STAP | Oksar et al. [9] | 60 p | STAP effective analgesic technique | |
| -STAP | Emile et al. [29] | 110 p | Improves recovery (pain relief, PONV…) | |
| -STAP | Jung et al. [30] | 38 p | Does not improve the quality and analgesia | |
| -STAP | Di Mauro et al. [31] | 60 p | No additional benefit | |
| -STAP | Houben et al. [32] | 60 p | Does not improve the analgesia provided | |
| -STAP/ESPB | Altıparmak [33] | 76 p | ESPB more effective than STAP | |
| -STAP/ESPB | Ozdemir et al. [34] | 64 p | ESPB provides superior analgesia | |
| -USicns/STAP | Xu et al. [35] | 64 p | US icns T6-11 better results | |
| -SIPB/STAP | Saravanan et al. [11] | 60 p | SIPB is equally efficacious than STAP | |
| -STAP/QLB | Baytar et al. [36] | 107 p | Similar results. STAP easier to perform | |
| -EOIB/STAP | Mehmet et al. [17] | 70 p | Similar analgesic activity | |
| -MTAPA | Güngör et al. [37] | 60 p | Superior analgesia compared to infiltration | |
| -EOIB | Korkusuz [38] | 80 p | Minimal clinically important differences | |
| Laparoscopic | -STAP | Ari et al. [39] | 40 p | STAP effective analgesic technique |
| Gastric surgery | -STAP | Albrecht el al [40] | 70 p | Bilateral STAP blocks no analgesic benefit |
| -STAP | Coşkun et al. [41] | 45 p | STAP not better than infiltration | |
| -QLB/STAP | Nie et al. [42] | 60 p | QLB provided greater opioid-sparing effect | |
| -ESPB/STAP | Abdelhamid et al. [43] | 66 p | ESPB lowers postoperative pain scores | |
| -ESPB/STAP | Mu et al. [44] | 168 p | ESP’s ability to reduce opioid use and promote faster recovery | |
| -SIPB | Kara et al. [12] | 30 p | SIPB is an alternative technique | |
| -EOIB | Doymus et al. [15] | 60 p | EOIB can be used as part of multimodal analgesia | |
| Laparoscopic nephrectomy | -SIPB/QLB | Fernandez et al. [45] | 120 p | SIPB and QLB showed adequate postoperative pain control |
| Radical gastrectomy | -STAP/epidural | Wu et al. [46] | 90 p | Epidural better analgesia than STAP, however STAP better analgesia than opioids iv. |
| Liver surgery | -STAP | Erdogan et al. [47] | 49 p | STAP reduces opioids consumption |
| -STAP | Kitlik et al. [48] | 50 p | STAP reduces postoperative morphine consumption | |
| -STAP | Maeda et al. [49] | 32 p | Less intraop fentanyl consumption | |
| -STAP | Assefi [50] | 132 p | A small opioid reducing effect after orthotopic liver transplantation surgery. | |
| -ESPB/STAP | Mostafa et al. [51] | 60 p | ESPB provided superior analgesia | |
| -SIPB | Jiang et al. [52] | 136 p | SIPB effective analgesia, saving opioids | |
| -EOIB | Yi et al. [53] | 48 p | EOIB significantly enhances postoperative analgesia | |
| -SIPB | Fernandez et al. [10] | 58 p | Effective analgesia, saving opioids | |
| Open nephrectomy | -STAP/QL | Saleh et al. [54] | 48 p | QLB better results than STAP |
| -SIPB | Fernandez et al. [10] | 15 p | Effective analgesic technique | |
| Ventral hernia repair | -SIPB | Fernandez et al. [10] | 26 p | SIPB provide effective analgesia and better postoperative recovery |
| Supraumbilical incision | -STAP | Niraj et al. [55] | 62 p | Superior analgesia STAP to epidural |
| -EOIB/STAP | Shrey [56] | 50 p | EOIB effective analgesia | |
| -EOIB/epidural | Srinivasaraghavan [57] | 66 p | EOIB alternative to epidural | |
| -SIPB | Mamoun et al. [58] | 60 p | SIPB provides a good analgesia |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandez Martin, M.T.; Mariano, E.R.; Valdes-Vilches, L.F.; Lopez Alvarez, S.; Elkassabany, N. Analgesia for Upper Abdominal Surgery, a Scoping Review of the Current Fascial Plane Block Techniques. J. Clin. Med. 2025, 14, 8632. https://doi.org/10.3390/jcm14248632
Fernandez Martin MT, Mariano ER, Valdes-Vilches LF, Lopez Alvarez S, Elkassabany N. Analgesia for Upper Abdominal Surgery, a Scoping Review of the Current Fascial Plane Block Techniques. Journal of Clinical Medicine. 2025; 14(24):8632. https://doi.org/10.3390/jcm14248632
Chicago/Turabian StyleFernandez Martin, Maria T., Edward R. Mariano, Luis F. Valdes-Vilches, Servando Lopez Alvarez, and Nabil Elkassabany. 2025. "Analgesia for Upper Abdominal Surgery, a Scoping Review of the Current Fascial Plane Block Techniques" Journal of Clinical Medicine 14, no. 24: 8632. https://doi.org/10.3390/jcm14248632
APA StyleFernandez Martin, M. T., Mariano, E. R., Valdes-Vilches, L. F., Lopez Alvarez, S., & Elkassabany, N. (2025). Analgesia for Upper Abdominal Surgery, a Scoping Review of the Current Fascial Plane Block Techniques. Journal of Clinical Medicine, 14(24), 8632. https://doi.org/10.3390/jcm14248632






