From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Mediastinum Surgery: How Far Are We?
Abstract
1. Background
- To analyze available data about different mediastinum surgeries performed under SV, with emphasis on published reports in the last 10 years.
- To describe some key anesthesiologic and surgical technical aspects.
- To describe the main reported outcomes, including comparisons with equivalent procedures under intubation with single-lung MV.
- To critically analyze the advantages and limitations of SV in mediastinum surgery.
- To highlight future perspectives and potential areas of investigation in this evolving field.
2. Thymectomy, Thymomectomy, and Other Mediastinum Tumor Excision
Controversial Issues
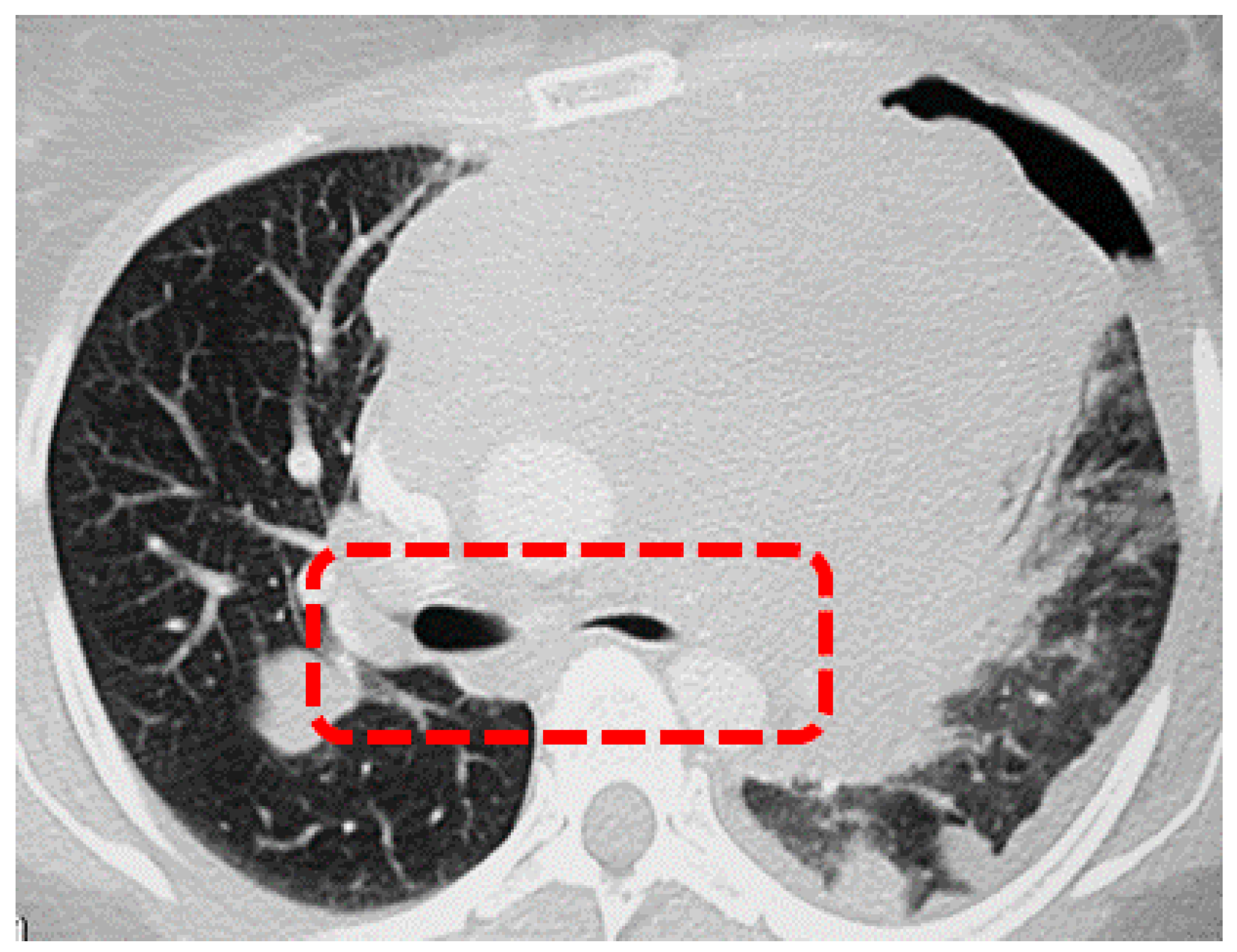
3. Biopsy of Mediastinal Masses
Controversial Issues
4. Thoracic Sympathectomy
Controversial Issues
5. Tracheal Resection
Controversial Issues
6. Pericardial Window
Controversial Issues
7. Esophagectomy
Controversial Issues
8. Limitations
9. Future Perspectives
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Pompeo, E.; Mineo, T.C. Awake Thoracic Surgery; Bentham Science Publishers: Sharjah, United Arab Emirates, 2012; pp. 3–8. [Google Scholar]
- Vischnevski, A.A. Local anesthesia in thoracic surgery: Lungs, heart, and esophagus. Minerva Anestesiol. 1954, 20, 432–435. [Google Scholar]
- Bjork, V.O.; Carlens, E. The prevention of spread during pulmonary resection by the use of a double-lumen catheter. J. Thorac. Surg. 1950, 20, 151–157. [Google Scholar] [CrossRef]
- Slutsky, A.S.; Ranieri, V.M. Ventilator-induced lung injury. N. Engl. J. Med. 2013, 369, 2126–2136. [Google Scholar] [CrossRef] [PubMed]
- Pompeo, E. From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Lung Surgery: An Ongoing Journey. J. Clin. Med. 2025, 14, 2475. [Google Scholar] [CrossRef] [PubMed]
- Pompeo, E.; Tacconi, F.; Mineo, T.C. Awake video-assisted thoracoscopic biopsy in complex anterior mediastinal masses. Thorac. Surg. Clin. 2010, 20, 225–233. [Google Scholar] [CrossRef]
- Al-Abdullatief, M.; Wahood, A.; Al-Shirawi, N.; Arabi, Y.; Wahba, M.; Al-Jumah, M.; Al-Sheha, S.; Yamani, N. Awake anaesthesia for major thoracic surgical procedures: An observational study. Eur. J. Cardiothorac. Surg. 2007, 32, 346–350. [Google Scholar] [CrossRef]
- Elia, S.; Guggino, G.; Mineo, D.; Vanni, G.; Gatti, A.; Mineo, T.C. Awake one stage bilateral thoracoscopic sympathectomy for palmar hyperhidrosis: A safe outpatient procedure. Eur. J. Cardiothorac. Surg. 2005, 28, 312–317; discussion 317. [Google Scholar] [CrossRef]
- Wolfe, G.I.; Kaminski, H.J.; Aban, I.B.; Minisman, G.; Kuo, H.C.; Marx, A.; Ströbel, P.; Mazia, C.; Oger, J.; Cea, J.G.; et al. Randomized Trial of Thymectomy in Myasthenia Gravis. N. Engl. J. Med. 2016, 375, 511–522, Erratum in N. Engl. J. Med. 2017, 376, 2097. https://doi.org/10.1056/NEJMx170003. [Google Scholar] [CrossRef]
- Rabiou, S.; Lakranbi, M.; Ghizlane, T.; Elfatemi, H.; Serraj, M.; Ouadnouni, Y.; Smahi, M. Quelle chirurgie pour quelle tumeur du médiastin: Expérience du service de chirurgie thoracique de CHU Hassan II de Fès [Which surgery for mediastinum tumor: Experience of the Department of thoracic surgery of CHU Hassan II of Fès]. Rev. Pneumol. Clin. 2017, 73, 246–252. [Google Scholar] [CrossRef]
- Mao, Z.F.; Mo, X.A.; Qin, C.; Lai, Y.R.; Hackett, M.L. Incidence of thymoma in myasthenia gravis: A systematic review. J. Clin. Neurol. 2012, 8, 161–169. [Google Scholar] [CrossRef]
- Rahman, M.M.; Islam, M.R.; Dhar, P.S. Myasthenia gravis in current status: Epidemiology, types, etiology, pathophysiology, symptoms, diagnostic tests, prevention, treatment, and complications—correspondence. Int. J. Surg. 2023, 109, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Yim, A.P.; Kay, R.L.; Ho, J.K. Video-assisted thoracoscopic thymectomy for myasthenia gravis. Chest 1995, 108, 1440–1443. [Google Scholar] [CrossRef] [PubMed]
- Ashton, R.C., Jr.; McGinnis, K.M.; Connery, C.P.; Swistel, D.G.; Ewing, D.R.; DeRose, J.J., Jr. Totally endoscopic robotic thymectomy for myasthenia gravis. Ann. Thorac. Surg. 2003, 75, 569–571. [Google Scholar] [CrossRef]
- Maniscalco, P.; Tamburini, N.; Quarantotto, F.; Grossi, W.; Garelli, E.; Cavallesco, G. Long-term outcome for early stage thymoma: Comparison between thoracoscopic and open approaches. Thorac. Cardiovasc. Surg. 2015, 63, 201–205. [Google Scholar] [CrossRef]
- Pompeo, E.; Elkhouly, A.G. Spontaneous ventilation thoracoscopic thymectomy: Attractive or exceptionable? J. Thorac. Dis. 2018, 10 (Suppl. 33), S3981–S3983. [Google Scholar] [CrossRef]
- Tsunezuka, Y.; Oda, M.; Matsumoto, I.; Tamura, M.; Watanabe, G. Extended thymectomy in patients with myasthenia gravis with high thoracic epidural anesthesia alone. World J. Surg. 2004, 28, 962–965; discussion 965–966. [Google Scholar] [CrossRef]
- Hartert, M.; Tripsky, J.; Brandt, A.; Huertgen, M. Non-intubated Uniportal Subxiphoid Video-Assisted Thoracoscopic Surgery for Extended Thymectomy in Myasthenia Gravis Patients: A Case Series. J. Chest Surg. 2022, 55, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, L.; Tang, W.; Yang, R. Non-intubated uniportal subxiphoid thoracoscopic extended thymectomy for thymoma associated with myasthenia gravis. World J. Surg. Oncol. 2021, 19, 342. [Google Scholar] [CrossRef]
- Huang, W.; Deng, H.; Lan, Y.; Wang, R.; Ge, F.; Huo, Z.; Lu, Y.; Lin, W.; Lin, G.; Liang, W.; et al. Spontaneous ventilation video-assisted thoracic surgery for mediastinal tumor resection in patients with pulmonary function deficiency. Ann. Transl. Med. 2020, 8, 1444. [Google Scholar] [CrossRef]
- Mao, Y.; Liang, H.; Deng, S.; Qiu, Y.; Zhou, Y.; Chen, H.; Jiang, L.; He, J. Non-intubated video-assisted thoracic surgery for subxiphoid anterior mediastinal tumor resection. Ann. Transl. Med. 2021, 9, 403. [Google Scholar] [CrossRef]
- Liang, H.; Liu, J.; Wu, S.; Zhang, Y.; Liu, H.; Yang, H.; Zhao, Y.; Hao, Z.; Liang, W.; He, J. Nonintubated Spontaneous Ventilation Offers Better Short-term Outcome for Mediastinal Tumor Surgery. Ann. Thorac. Surg. 2019, 108, 1045–1051. [Google Scholar] [CrossRef]
- Liu, Z.; Yang, R.; Sun, Y. Nonintubated Uniportal Thoracoscopic Thymectomy with Laryngeal Mask. Thorac. Cardiovasc. Surg. 2020, 68, 450–456. [Google Scholar] [CrossRef]
- Jiang, L.; Depypere, L.; Rocco, G.; Chen, J.S.; Liu, J.; Shao, W.; Yang, H.; He, J.; AME Thoracic Surgery Collaborative Group. Spontaneous ventilation thoracoscopic thymectomy without muscle relaxant for myasthenia gravis: Comparison with “standard” thoracoscopic thymectomy. J. Thorac. Cardiovasc. Surg. 2018, 155, 1882–1889.e3. [Google Scholar] [CrossRef]
- Pompeo, E.; Dauri, M.; Massa, R.; Peer, M. Minimalist thoracoscopic resection of thymoma associated with myasthenia gravis. J. Thorac. Cardiovasc. Surg. 2017, 154, 1463–1465. [Google Scholar] [CrossRef]
- Gelzinis, T. The Anesthetic Management of Patients Undergoing Nonintubated Video-Assisted Thoracic Surgery. Curr. Anesthesiol. Rep. 2021, 11, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Patirelis, A.; Elia, S.; Cristino, B.; Puxeddu, E.; Cavalli, F.; Rogliani, P.; Pompeo, E. Spontaneous Ventilation Thoracoscopic Lung Biopsy in Undetermined Interstitial Lung Disease: Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 374. [Google Scholar] [CrossRef]
- Pompeo, E.; Elkhouly, A.; Rogliani, P.; Dauri, M.; Peer, M.; Sergiacomi, G.; Sorge, R. Quasilobar minimalist lung volume reduction surgery. Eur. J. Cardiothorac. Surg. 2021, 60, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, J.; Strange, C.D.; Agrawal, R.; Erasmus, L.T.; Truong, M.T. Approach to Imaging of Mediastinal Masses. Diagnostics 2023, 13, 3171. [Google Scholar] [CrossRef]
- Goh, M.H.; Liu, X.Y.; Goh, Y.S. Anterior mediastinal masses: An anaesthetic challenge. Anaesthesia 1999, 54, 670–674. [Google Scholar] [CrossRef]
- Feng, J.; Zhao, J.; Zhang, Y.; Hu, Y. Incidence, outcome and risk factors of perioperative pulmonary complications in pediatric patients with mediastinal mass. BMC Pediatr. 2025, 25, 108. [Google Scholar] [CrossRef]
- Béchard, P.; Létourneau, L.; Lacasse, Y.; Côté, D.; Bussières, J.S. Perioperative cardiorespiratory complications in adults with mediastinal mass: Incidence and risk factors. Anesthesiology 2004, 100, 826–834; discussion 5A. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.N.; Yun, S.J.; Kim, J.I.; Ryu, C.W. Diagnostic outcome and safety of CT-guided core needle biopsy for mediastinal masses: A systematic review and meta-analysis. Eur. Radiol. 2020, 30, 588–599. [Google Scholar] [CrossRef] [PubMed]
- Petranovic, M.; Gilman, M.D.; Muniappan, A.; Hasserjian, R.P.; Digumarthy, S.R.; Muse, V.V.; Sharma, A.; Shepard, J.A.; Wu, C.C. Diagnostic Yield of CT-Guided Percutaneous Transthoracic Needle Biopsy for Diagnosis of Anterior Mediastinal Masses. AJR Am. J. Roentgenol. 2015, 205, 774–779. [Google Scholar] [CrossRef]
- Frederiksen, J.K.; Sharma, M.; Casulo, C.; Burack, W.R. Systematic review of the effectiveness of fine-needle aspiration and/or core needle biopsy for subclassifying lymphoma. Arch. Pathol. Lab. Med. 2015, 139, 245–251. [Google Scholar] [CrossRef]
- Eichenauer, D.A.; Aleman, B.M.P.; André, M.; Federico, M.; Hutchings, M.; Illidge, T.; Engert, A.; Ladetto, M.; ESMO Guidelines Committee. Hodgkin lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018, 29 (Suppl. 4), iv19–iv29. [Google Scholar] [CrossRef] [PubMed]
- Vitolo, U.; Seymour, J.F.; Martelli, M.; Illerhaus, G.; Illidge, T.; Zucca, E.; Campo, E.; Ladetto, M.; ESMO Guidelines Committee. Extranodal diffuse large B-cell lymphoma (DLBCL) and primary mediastinal B-cell lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016, 27 (Suppl. 5), v91–v102. [Google Scholar] [CrossRef]
- Blank, R.S.; de Souza, D.G. Anesthetic management of patients with an anterior mediastinal mass: Continuing professional development. Can. J. Anaesth. 2011, 58, 853–859, 860–867, (In English, in French.). [Google Scholar] [CrossRef]
- Hartigan, P.M.; Karamnov, S.; Gill, R.R.; Ng, J.M.; Yacoubian, S.; Tsukada, H.; Swanson, J.; Barlow, J.; McMurry, T.L.; Blank, R.S. Mediastinal Masses, Anesthetic Interventions, and Airway Compression in Adults: A Prospective Observational Study. Anesthesiology 2022, 136, 104–114. [Google Scholar] [CrossRef]
- Tacconi, F.; Rogliani, P.; Cristino, B.; Gilardi, F.; Palombi, L.; Pompeo, E.; Awake Thoracic Surgery Research Group. Minimalist video-assisted thoracic surgery biopsy of mediastinal tumors. J. Thorac. Dis. 2016, 8, 3704–3710. [Google Scholar] [CrossRef]
- Han, D.; Chen, Y.; Guo, H.; Wu, Y.; Pan, S.; Yan, F. Feasibility and Safety of Nonintubated Anesthesia in Pediatric Video-assisted Thoracoscopic Surgery: A Preliminary Report. J. Cardiothorac. Vasc. Anesth. 2025, 39, 3082–3089. [Google Scholar] [CrossRef]
- Atkins, J.L.; Butler, P.E. Hyperhidrosis: A review of current management. Plast. Reconstr. Surg. 2002, 110, 222–228. [Google Scholar] [CrossRef]
- Henning, M.A.S.; Bouazzi, D.; Jemec, G.B.E. Treatment of Hyperhidrosis: An Update. Am. J. Clin. Dermatol. 2022, 23, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Cerfolio, R.J.; De Campos, J.R.; Bryant, A.S.; Connery, C.P.; Miller, D.L.; DeCamp, M.M.; McKenna, R.J.; Krasna, M.J. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann. Thorac. Surg. 2011, 91, 1642–1648. [Google Scholar] [CrossRef]
- Chen, J.; Du, Q.; Lin, M.; Lin, J.; Li, X.; Lai, F.; Tu, Y. Transareolar Single-Port Needlescopic Thoracic Sympathectomy Under Intravenous Anesthesia Without Intubation: A Randomized Controlled Trial. J. Laparoendosc. Adv. Surg. Tech. A 2016, 26, 958–964. [Google Scholar] [CrossRef]
- Cui, F.; Liu, J.; Li, S.; Yin, W.; Xin, X.; Shao, W.; He, J. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J. Thorac. Dis. 2016, 8, 2226–2232. [Google Scholar] [CrossRef]
- Caviezel, C.; Schuepbach, R.; Grande, B.; Opitz, I.; Zalunardo, M.; Weder, W.; Hillinger, S. Establishing a non-intubated thoracoscopic surgery programme for bilateral uniportal sympathectomy. Swiss Med. Wkly. 2019, 149, w20064. [Google Scholar] [CrossRef] [PubMed]
- Shao, G.Q.; Pang, D.Z.; Zhang, J.T.; Wang, H.X.; Liuru, T.Y.; Liu, Z.H.; Liang, Y.N.; Liu, J.S. Spontaneous ventilation anesthesia combined with uniportal and tubeless thoracoscopic sympathectomy in selected patients with primary palmar hyperhidrosis. J. Cardiothorac. Surg. 2022, 17, 177. [Google Scholar] [CrossRef] [PubMed]
- Taje, R.; Fabbi, E.; Sorge, R.; Elia, S.; Dauri, M.; Pompeo, E. Adjuvant Transthoracic Negative-Pressure Ventilation in Nonintubated Thoracoscopic Surgery. J. Clin. Med. 2023, 12, 4234. [Google Scholar] [CrossRef]
- Wang, R.; Chen, J.; He, J.; Li, S. Non-intubated Airway Surgery. Thorac. Surg. Clin. 2025, 35, 17–23. [Google Scholar] [CrossRef]
- Hobai, I.A.; Chhangani, S.V.; Alfille, P.H. Anesthesia for tracheal resection and reconstruction. Anesthesiol. Clin. 2012, 30, 709–730. [Google Scholar] [CrossRef]
- Chitilian, H.V.; Bao, X.; Mathisen, D.J.; Alfille, P.H. Anesthesia for Airway Surgery. Thorac. Surg. Clin. 2018, 28, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Wiedemann, K.; Männle, C. Anesthesia and gas exchange in tracheal surgery. Thorac. Surg. Clin. 2014, 24, 13–25. [Google Scholar] [CrossRef]
- MacIntyre, N.R. High-frequency jet ventilation. Respir. Care Clin. N. Am. 2001, 7, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Lorente, D.; Iglesias, M.; Rodríguez, A.; Jungebluth, P.; Macchiarini, P. The pumpless extracorporeal lung membrane provides complete respiratory support during complex airway reconstructions without inducing cellular trauma or a coagulatory and inflammatory response. J. Thorac. Cardiovasc. Surg. 2012, 144, 425–430. [Google Scholar] [CrossRef]
- Liang, H.; Gonzalez-Rivas, D.; Zhou, Y.; Liu, J.; Wu, X.; He, J.; Li, S. Nonintubated Anesthesia for Tracheal/Carinal Resection and Reconstruction. Thorac. Surg. Clin. 2020, 30, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Macchiarini, P.; Rovira, I.; Ferrarello, S. Awake upper airway surgery. Ann. Thorac. Surg. 2010, 89, 387–390; discussion 390–3911. [Google Scholar] [CrossRef]
- Peng, G.; Cui, F.; Ang, K.L.; Zhang, X.; Yin, W.; Shao, W.; Dong, Q.; Liang, L.; He, J. Non-intubated combined with video-assisted thoracoscopic in carinal reconstruction. J. Thorac. Dis. 2016, 8, 586–593. [Google Scholar] [CrossRef]
- Caronia, F.P.; Loizzi, D.; Nicolosi, T.; Castorina, S.; Fiorelli, A. Tubeless tracheal resection and reconstruction for management of benign stenosis. Head. Neck. 2017, 39, E114–E117. [Google Scholar] [CrossRef]
- Zhang, Y.; Mo, Z.; Yang, C.; He, J.; Li, S.; Lan, L. Non-intubated tracheal resection and reconstruction for a tracheal tumor in an 8-year-old child. J. Cardiothorac. Surg. 2024, 19, 468. [Google Scholar] [CrossRef]
- Guo, M.; Peng, G.; Wei, B.; He, J. Uniportal video-assisted thoracoscopic surgery in tracheal tumour under spontaneous ventilation anaesthesia. Eur. J. Cardiothorac. Surg. 2017, 52, 392–394. [Google Scholar] [CrossRef]
- Guido Guerra, R.E.; Bolaños Morales, F.V.; Silva Gómez, O.F.; Olvera Prado, H.; Ibáñez Barzalobre, S.; Bosinceanu, M.; Gonzalez-Rivas, D. Uniportal Robotic-Assisted Tracheal Resection and Reconstruction Under Spontaneous Ventilation. Case Rep. Anesthesiol. 2025, 2025, 4991280. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Liang, H.; Xu, K.; Yang, C.; Liang, L.; Dong, Q.; Yang, H.; Liu, H.; Li, Y.; Patolia, S.; et al. The strategy of non-intubated spontaneous ventilation anesthesia for upper tracheal surgery: A retrospective case series study. Transl. Lung Cancer Res. 2022, 11, 880–889. [Google Scholar] [CrossRef]
- Liu, Y.; Liang, L.; Yang, H. Airway management in “tubeless” spontaneous-ventilation video-assisted thoracoscopic tracheal surgery: A retrospective observational case series study. J. Cardiothorac. Surg. 2023, 18, 59. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Liu, J.; Gonzalez-Rivas, D.; Shargall, Y.; Kolb, M.; Shao, W.; Dong, Q.; Liang, L.; He, J. Thoracoscopic surgery for tracheal and carinal resection and reconstruction under spontaneous ventilation. J. Thorac. Cardiovasc. Surg. 2018, 155, 2746–2754. [Google Scholar] [CrossRef]
- Adler, Y.; Charron, P.; Imazio, M.; Badano, L.; Barón-Esquivias, G.; Bogaert, J.; Brucato, A.; Gueret, P.; Klingel, K.; Lionis, C.; et al. ESCGuidelines for the diagnosis management of pericardial diseases: The Task Force for the Diagnosis Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2015, 36, 2921–2964. [Google Scholar] [CrossRef]
- Cho, Y.H.; Schaff, H.V.; Dearani, J.A.; Daly, R.C.; Park, S.J.; Li, Z.; Oh, J.K. Completion pericardiectomy for recurrent constrictive pericarditis: Importance of timing of recurrence on late clinical outcome of operation. Ann. Thorac. Surg. 2012, 93, 1236–1240. [Google Scholar] [CrossRef]
- Park, C.Y.; McGonigle, N.C. Single-Port Thoracoscopic Pericardial Window Under Local Anesthesia. Innovations 2018, 13, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Madhivathanan, P.R.; Corredor, C.; Smith, A. Perioperative implications of pericardial effusions and cardiac tamponade. BJA Educ. 2020, 20, 226–234. [Google Scholar] [CrossRef]
- Lee, D.; Flores, R. Awake thoracoscopic pericardial window is safe and feasible. J. Vis. Surg. 2024, 10, 1–6. [Google Scholar] [CrossRef]
- Çardak, M.E.; Külahçioglu, S.; Erdem, E. Awake uniportal video-assisted thoracoscopic surgery for the management of pericardial effusion. J. Minim. Access Surg. 2023, 19, 482–488. [Google Scholar] [CrossRef]
- Bhayani, N.H.; Gupta, A.; Dunst, C.M.; Kurian, A.A.; Reavis, K.M.; Swanström, L.L. Esophagectomies with thoracic incisions carry increased pulmonary morbidity. JAMA Surg. 2013, 148, 733–738. [Google Scholar] [CrossRef]
- Linden, P.A.; Towe, C.W.; Watson, T.J.; Low, D.E.; Cassivi, S.D.; Grau-Sepulveda, M.; Worrell, S.G.; Perry, Y. Mortality After Esophagectomy: Analysis of Individual Complications and Their Association with Mortality. J. Gastrointest. Surg. 2020, 24, 1948–1954. [Google Scholar] [CrossRef]
- Liu, J.; Cui, F.; Li, S.; Chen, H.; Shao, W.; Liang, L.; Yin, W.; Lin, Y.; He, J. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: A randomized control study. Surg. Innov. 2015, 22, 123–130. [Google Scholar] [CrossRef]
- Xu, Q.; Mo, X.; Xiong, J.; Zhang, Y. Case Report: Discontinuous Spontaneous Ventilating Anesthesia for McKeown Esophagectomy by Laryngeal Mask: A Case Series-A Novel Approach of Discontinuous Spontaneous Ventilating Anesthesia for Esophagectomy. Front. Surg. 2021, 8, 783859. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Chen, J.; Zhou, Y.; He, H.; Li, Z.; Yang, H.; Liang, L.; He, J.; Liu, J. McKeown minimally invasive esophagectomy under discontinuous spontaneous ventilating anesthesia by laryngeal mask: A retrospective non-inferiority cohort study. J. Thorac. Dis. 2025, 17, 5014–5023. [Google Scholar] [CrossRef] [PubMed]
- Batchelor, T.J.P.; Rasburn, N.J.; Abdelnour-Berchtold, E.; Brunelli, A.; Cerfolio, R.J.; Gonzalez, M.; Ljungqvist, O.; Petersen, R.H.; Popescu, W.M.; Slinger, P.D.; et al. Guidelines for enhanced recovery after lung surgery: Recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardiothorac. Surg. 2019, 55, 91–115. [Google Scholar] [CrossRef] [PubMed]
- Tacconi, F.; Pompeo, E. Non-intubated video-assisted thoracic surgery: Where does evidence stand? J. Thorac. Dis. 2016, 8 (Suppl. 4), S364–S375. [Google Scholar] [CrossRef]
| First Author | Year | Country | Study Design | Number of Patients | Surgical Access | Comparison with MV-VATS (SV vs. MV) | MG Patients |
|---|---|---|---|---|---|---|---|
| Hartert [18] | 2022 | Germany | Case series | 3 | Subxiphoid | No | Yes |
| Liu [19] | 2021 | China | Case series | 10 | Subxiphoid | No | Yes |
| Huang [20] | 2020 | China | Retrospective | 32 | Triportal | Yes (15 vs. 17) | No |
| Mao [21] | 2020 | China | Retrospective | 40 | Subxiphoid | Yes (21 vs. 19) | Yes |
| Liang [22] | 2019 | China | Retrospective with PSM | 198 | Biportal | Yes (55 vs. 55) | Yes |
| Liu [23] | 2019 | China | Retrospective | 225 | Uniportal | Yes (96 vs. 129) | No |
| Jiang [24] | 2018 | China | Retrospective | 104 | Triportal | Yes (36 vs. 68) | Yes |
| Pompeo [25] | 2017 | Italy | Case series | 3 | Uniportal | No | Yes |
| Mediastinum Tumor Excision | Mediastinum Mass Biopsy | Thoracic Sympathectomy | Tracheal Resection | Pericardial Window | Esophagectomy | |
|---|---|---|---|---|---|---|
| Risk of hypoxemia | + | +/− | +/− | ++ | +/− | ++ |
| Risk of hypercapnia | + | +/− | +/− | ++ | +/− | ++ |
| Lack of safe airway control | − | + | − | +/− | − | + |
| More difficult surgical maneuvering due to mediastinum movement | + | +/− | +/− | +/− | − | + |
| Risks of bilateral pneumothorax | ++ | − | − | + | − | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patirelis, A.; Ambrogi, V.; Pompeo, E. From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Mediastinum Surgery: How Far Are We? J. Clin. Med. 2025, 14, 8396. https://doi.org/10.3390/jcm14238396
Patirelis A, Ambrogi V, Pompeo E. From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Mediastinum Surgery: How Far Are We? Journal of Clinical Medicine. 2025; 14(23):8396. https://doi.org/10.3390/jcm14238396
Chicago/Turabian StylePatirelis, Alexandro, Vincenzo Ambrogi, and Eugenio Pompeo. 2025. "From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Mediastinum Surgery: How Far Are We?" Journal of Clinical Medicine 14, no. 23: 8396. https://doi.org/10.3390/jcm14238396
APA StylePatirelis, A., Ambrogi, V., & Pompeo, E. (2025). From Awake to Minimalist Spontaneous Ventilation Thoracoscopic Mediastinum Surgery: How Far Are We? Journal of Clinical Medicine, 14(23), 8396. https://doi.org/10.3390/jcm14238396







