Impact of Antihypertensive Treatment Adherence on Premature Mortality over Seven Years: A Follow-Up Investigation
Abstract
1. Introduction
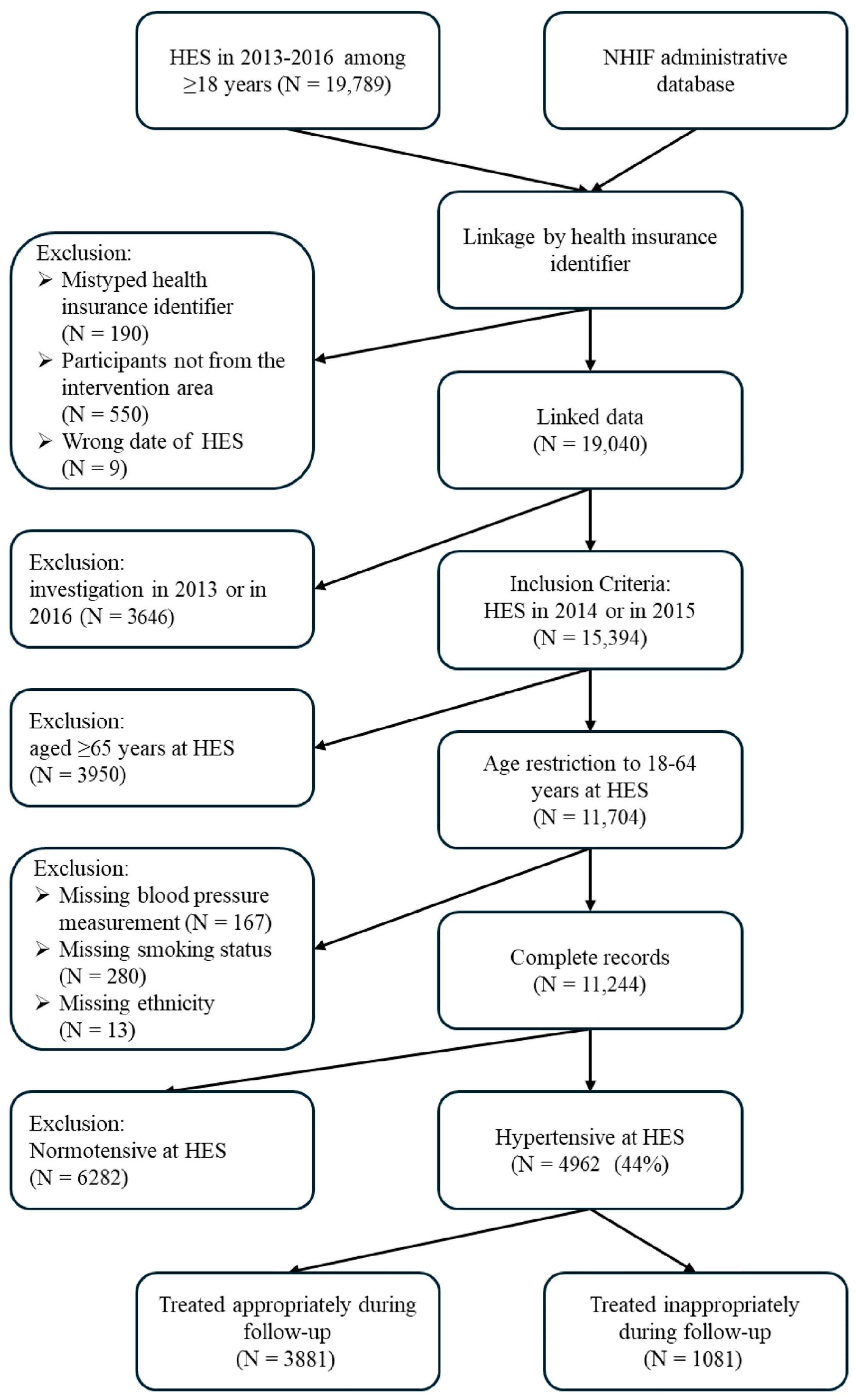
2. Materials and Methods
2.1. Study Design and Setting
2.2. Variables
2.3. Data Analysis
2.4. Ethical Aspects
3. Results
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHM | Antihypertensive medication |
| AOR | Adjusted odds ratio |
| ATAP | Antihypertensive treatment adherence appropriateness |
| BP | Blood pressure |
| CA | Cancer |
| COPD | Chronic obstructive pulmonary disease |
| CVDs | Cardiovascular diseases |
| DBP | Diastolic blood pressure |
| DM | Diabetes mellitus |
| DWR | Dispensed to written prescription ratio |
| HES | Health examination survey |
| HTN | Hypertension |
| IHD | Ischemic heart disease |
| NIHIF | National Health Insurance Fund |
| OR | Odds ratio |
| SBP | Systolic blood pressure |
| USPSTF | United States Preventive Services Task Force |
References
- World Health, Organization (WHO). Global Report on Hypertension: The Race Against a Silent Killer. 2023. Available online: https://www.who.int/publications/i/item/9789240081062 (accessed on 15 January 2025).
- Centers for Disease Control and Prevention (CDC). Heart Disease. Heart Disease Risk Factors. 2024. Available online: https://www.cdc.gov/heart-disease/risk-factors/index.html (accessed on 31 October 2025).
- UN News, Highblood Pressure Now More Common in Low and Middle-Income Countries, New Reportfinds. 2021. Available online: https://news.un.org/en/story/2021/08/1098342 (accessed on 31 October 2025).
- World Health Organization (WHO). Hypertension. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 15 January 2025).
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- World Heart Federation. World Hypertension Day: Taking Action Against the Silent Epidemic of High Blood Pressure [Internet]. World Heart Federation. 2022. Available online: https://world-heart-federation.org/news/world-hypertension-day-taking-action-against-the-silent-epidemic-of-high-blood-pressure/ (accessed on 15 January 2025).
- Pristianty, L.; Hingis, E.S.; Priyandani, Y.; Rahem, A. Relationship between knowledge and adherence to hypertension treatment. J. Public Health Afr. 2023, 14, 2502. [Google Scholar] [CrossRef]
- Sharma, S.; Sharma, C.R.; Aryal, S.; Bhandari, B. Adherence to antihypertensive medication and its associated factors among patients with hypertension attending a tertiary hospital in Kathmandu, Nepal. PLoS ONE 2024, 19, e0305941. [Google Scholar] [CrossRef]
- Peeters, L.; van Gelder, T.; van Dijk, L.; Koch, B.; Versmissen, J. Lessons learned from conducting a randomized controlled trial to improve non-adherence to antihypertensive drug treatment. Blood Press. 2023, 32, 2281316. [Google Scholar] [CrossRef]
- Zuin, M.; Tognola, C.; Maloberti, A.; Parati, G.; Di Fusco, S.A.; Gil Ad, V.; Armata, D.; Valle, C.D.; Colivicchi, F.; Bilato, C.; et al. Advances in Hypertension Management: Insights from the Latest European Guidelines. J. Cardiovasc. Dev. Dis. 2025, 12, 155. [Google Scholar] [CrossRef] [PubMed]
- Nemcsik, J.; Páll, D.; Nemes-Nagy, Z.; Bacskai, M.; Kovács, T.; Benczúr, B.; Kiss, A.; Ábrahám, G.; Barna, I.; Beaney, T.; et al. May Measurement Month 2019: An analysis of blood pressure screening results from Hungary. Eur. Hear. J. Suppl. 2021, 23, B70–B72. [Google Scholar] [CrossRef] [PubMed]
- EUROSTAT: Standardised Preventable and Treatable Mortality, 2011–2022. Available online: https://ec.europa.eu/eurostat/databrowser/product/page/SDG_03_42 (accessed on 23 September 2025). [CrossRef]
- Organisation for Economic Co-operation and Development. European Commission Eurostat: Avoidable Mortality: OECD/Eurostat Lists of Preventable and Treatable Causes of Death (Jan 2022 version). Available online: https://www.oecd.org/content/dam/oecd/en/data/datasets/oecd-health-statistics/avoidable-mortality-2019-joint-oecd-eurostat-list-preventable-treatable-causes-of-death.pdf (accessed on 23 September 2025).
- Vamvakis, A.; Lazaridis, A.; Grammatikopoulou, M.G.; Malliora, A.; Tsiroukidou, K.; Tzimos, C.; Di Blasio, A.; Izzicupo, P.; Gkaliagkousi, E. Impact of Dietary Patterns on the Lipidemic Profile and the Cardiovascular Risk in Stage 1 Hypertension: A Post Hoc Analysis of the HINTreat Trial. Nutrients 2025, 17, 2632. [Google Scholar] [CrossRef] [PubMed]
- Hossain, A.; Ahsan, G.U.; Hossain, M.Z.; Hossain, M.A.; Sutradhar, P.; Alam, S.-E.; Sultana, Z.Z.; Hijazi, H.; Rahman, S.A.; Alameddine, M. Medication adherence and blood pressure control in treated hypertensive patients: First follow-up findings from the PREDIcT-HTN study in Northern Bangladesh. BMC Public Health 2025, 25, 1–12. [Google Scholar] [CrossRef]
- Tomasino, C.; Tomasino, M. Medication adherence and non-adherence in arterial hypertension: A narrative review. Explor. Med. 2025, 6, 1001276. [Google Scholar] [CrossRef]
- Schedlbauer, A.; Davies, P.; Fahey, T. Interventions to improve adherence to lipid lowering medication. Cochrane Database Syst. Rev. 2010, CD004371. [Google Scholar] [CrossRef]
- Claxton, A.J.; Cramer, J.; Pierce, C. A systematic review of the associations between dose regimens and medication compliance. Clin. Ther. 2001, 23, 1296–1310. [Google Scholar] [CrossRef] [PubMed]
- Torres-Robles, A.; Wiecek, E.; Tonin, F.S.; Benrimoj, S.I.; Fernandez-Llimos, F.; Garcia-Cardenas, V. Comparison of Interventions to Improve Long-Term Medication Adherence Across Different Clinical Conditions: A Systematic Review with Network Meta-Analysis. Front. Pharmacol. 2018, 9, 1454. [Google Scholar] [CrossRef]
- Banning, M. A review of interventions used to improve adherence to medication in older people. Int. J. Nurs. Stud. 2009, 46, 1505–1515. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Nguyen, P.-A.A.; Clinciu, D.L.; Hsu, C.-K.; Lu, J.-C.R.; Yang, H.; Wu, C.-C.; Tsai, W.-C.; Chou, Y.-C.; Kuo, T.B.; et al. A personalized medication management platform (PMMP) to improve medication adherence: A randomized control trial. Comput. Methods Programs Biomed. 2017, 140, 275–281. [Google Scholar] [CrossRef]
- Ferdinand, K.C.; Senatore, F.F.; Clayton-Jeter, H.; Cryer, D.R.; Lewin, J.C.; Nasser, S.A.; Fiuzat, M.; Califf, R.M. Improving Medication Adherence in Cardiometabolic Disease. JACC 2017, 69, 437–451. [Google Scholar] [CrossRef]
- Farris, K.B.; Salgado, T.M.; Batra, P.; Piette, J.D.; Singh, S.; Guhad, A.; Newman, S.; Marshall, V.D.; An, L. Confirming the theoretical structure of expert-developed text messages to improve adherence to anti-hypertensive medications. Res. Soc. Adm. Pharm. 2016, 12, 578–591. [Google Scholar] [CrossRef]
- McNally, R.J.; Teo, V.; Imran, H.; Wright, A.; Waters, B.; Faconti, L.; Patel, J.; Stevenson, J.; Chowienczyk, P.J.; Weinman, J. Pharmacist interventions in the control of hypertension and adherence to anti-hypertensive treatment: A systematic review and meta-analysis of randomised controlled trials. Int. J. Pharm. Pract. 2024, 32, ii6–ii7. [Google Scholar] [CrossRef]
- Rashid, A.; Ejara, D.; Deybasso, H.A. Adherence to antihypertensive medications and associated factors in patients with hypertension, Oromia, Ethiopia: A multicenter study. Sci. Rep. 2024, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Alruwaili, B.F. Evaluation of Hypertension-Related Knowledge, Medication Adherence, and Associated Factors Among Hypertensive Patients in the Aljouf Region, Saudi Arabia: A Cross-Sectional Study. Medicina 2024, 60, 1822. [Google Scholar] [CrossRef]
- Suleiman, S.Z.; Htay, M.N.N.; Soe, H.H.K.; Low, C.L.Y.; Alias, S.H.; Yussof, S.; Keng, W.X.; Chong, K.; Sahiran, M.F.; Harun, M.H.; et al. Association between medication adherence and blood pressure control and factors associated with antihypertensive medication adherence in the Melaka Tengah District: A cross-sectional survey. Malays. Fam. Physician 2024, 19, 56. [Google Scholar] [CrossRef] [PubMed]
- Radic, J.; Dogas, H.; Vuckovic, M.; Kolak, E.; Gelemanovic, A.; Nenadic, D.B.; Radic, M. MEDICATION ADHERENCE AND GENDER DIFFERENCE IN HYPERTENSIVE PATIENTS. J. Hypertens. 2023, 41, e314. [Google Scholar] [CrossRef]
- Harsha, N.; Papp, M.; Kőrösi, L.; Czifra, Á.; Ádány, R.; Sándor, J. Enhancing Primary Adherence to Prescribed Medications through an Organized Health Status Assessment-Based Extension of Primary Healthcare Services. Int. J. Environ. Res. Public Health 2019, 16, 3797. [Google Scholar] [CrossRef]
- Farsang, C.; Burnier, M.; Narkiewicz, K.; Rokszin, G.; Abonyi-Tóth, Z.; Kovács, G.; Potukuchi, P.K.; Abdel-Moneim, M.; Simonyi, G. IMPACT OF RAMIPRIL/AMLODIPINE DOSE COMBINATIONS OF SINGLE-PILL VERSUS FREE EQUIVALENT COMBINATIONS ON PERSISTENCE AND MAJOR ADVERSE CARDIOVASCULAR EVENTS: A REAL-WORLD ANALYSIS. J. Hypertens. 2023, 41, e81. [Google Scholar] [CrossRef]
- Simonyi, G.; Burnier, M.; Narkiewicz, K.; Rokszin, G.; Abonyi-Tóth, Z.; Kovács, G.; Potukuchi, P.K.; Abdel-Moneim, M.; Farsang, C. Effect of single-pill versus free equivalent combinations on persistence and major adverse cardiovascular events in hypertension: A real-world analysis. J. Hypertens. 2024, 43, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Sándor, J.; Nagy, A.; Jenei, T.; Földvári, A.; Szabó, E.; Csenteri, O.; Vincze, F.; Sipos, V.; Kovács, N.; Pálinkás, A.; et al. Influence of patient characteristics on preventive service delivery and general practitioners’ preventive performance indicators: A study in patients with hypertension or diabetes mellitus from Hungary. Eur. J. Gen. Pract. 2018, 24, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Pálinkás, A.; Sándor, J.; Papp, M.; Kőrösi, L.; Falusi, Z.; Pál, L.; Bélteczki, Z.; Rihmer, Z.; Döme, P. Associations between untreated depression and secondary health care utilization in patients with hypertension and/or diabetes. Chest 2018, 54, 255–276. [Google Scholar] [CrossRef]
- Sándor, J.; Kósa, K.; Papp, M.; Fürjes, G.; Kőrösi, L.; Jakovljevic, M.; Ádány, R. Capitation-Based Financing Hampers the Provision of Preventive Services in Primary Health Care. Front. Public Health 2016, 4, 200. [Google Scholar] [CrossRef]
- Sándor, J.; Nagy, A.; Földvári, A.; Szabó, E.; Csenteri, O.; Vincze, F.; Sipos, V.; Kovács, N.; Pálinkás, A.; Papp, M.; et al. Delivery of cardio-metabolic preventive services to Hungarian Roma of different socio-economic strata. Fam. Pract. 2016, 34, 83–89. [Google Scholar] [CrossRef]
- Vidal-Petiot, E. Thresholds for Hypertension Definition, Treatment Initiation, and Treatment Targets: Recent Guidelines at a Glance. Circulation 2022, 146, 805–807. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Wan, L.; Yu, B.; Zhang, J. The link between adherence to antihypertensive medications and mortality rates in patients with hypertension: A systematic review and meta-analysis of cohort studies. BMC Cardiovasc. Disord. 2025, 25, 145. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kim, B.S.; Kim, H.; Lee, J.; Shin, J.-H.; Sung, K.-C. Impact of blood pressure and medication adherence on clinical outcomes in patients with hypertension. Front. Med. 2025, 12, 1564791. [Google Scholar] [CrossRef] [PubMed]
- Hamrahian, S.M.; Maarouf, O.H.; Fülöp, T. A Critical Review of Medication Adherence in Hypertension: Barriers and Facilitators Clinicians Should Consider. Patient Prefer. Adherence 2022, ume 16, 2749–2757. [Google Scholar] [CrossRef]
- Salazar, M.R. Early adherence to antihypertensive drugs and long—Erm cardiovascular mortality in the “real world”. J. Clin. Hypertens. 2021, 23, 1703–1705. [Google Scholar] [CrossRef]
- Lee, J.S.; Escano, R.S.; Therrien, N.L.; Kumar, A.; Bhatt, A.; Pollack, L.M.; Jackson, S.L.; Luo, F. Antihypertensive Medication Adherence and Medical Costs, Health Care Use, and Labor Productivity Among People with Hypertension. J. Am. Hear. Assoc. 2024, 13, e037357. [Google Scholar] [CrossRef]
- Dalli, L.L.; Olaiya, M.T.; Kim, J.; Andrew, N.E.; Cadilhac, D.A.; Ung, D.; Lindley, R.I.; Sanfilippo, F.M.; Thrift, A.G.; Nelson, M.R.; et al. Antihypertensive Medication Adherence and the Risk of Vascular Events and Falls After Stroke: A Real-World Effectiveness Study Using Linked Registry Data. Hypertension 2023, 80, 182–191. [Google Scholar] [CrossRef]
- Aune, D.; Huang, W.; Nie, J.; Wang, Y. Hypertension and the Risk of All-Cause and Cause-Specific Mortality: An Outcome-Wide Association Study of 67 Causes of Death in the National Health Interview Survey. BioMed Res. Int. 2021, 2021, 9376134. [Google Scholar] [CrossRef]
- Wang, M.; Wu, T.; Yu, C.; Gao, W.; Lv, J.; Wu, Y.; Qin, X.; Tang, X.; Gao, P.; Zhan, S.; et al. Association between blood pressure levels and cardiovascular deaths: A 20-year follow-up study in rural China. BMJ Open 2020, 10, e035190. [Google Scholar] [CrossRef]
- Chambergo-Michilot, D.; Rebatta-Acuña, A.; Delgado-Flores, C.J.; Toro-Huamanchumo, C.J. Socioeconomic determinants of hypertension and prehypertension in Peru: Evidence from the Peruvian Demographic and Health Survey. PLoS ONE 2021, 16, e0245730. [Google Scholar] [CrossRef]
- Lombardi, M.; Severi, P.; Mazza, A.; Bendini, M.G.; Caldarone, E.; Armeni, M.; D’Emidio, S.; Leggio, M. Sex Differences in Hypertension: A Question worth Asking? Ann. Clin. Hypertens. 2017, 1, 001–005. [Google Scholar] [CrossRef]
- SenthilKumar, G.; Katunaric, B.; Bordas-Murphy, H.; Sarvaideo, J.; Freed, J.K. Estrogen and the Vascular Endothelium: The Unanswered Questions. Endocrinology 2023, 164, bqad079. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Tobe, S.W.; Kaczorowski, J.; Bacon, S.L.; Vafaei, A.; Hasan, O.S.M.; Krishnan, R.J.; Raifu, A.O.; Rehm, J. Sex-Specific Associations Between Alcohol Consumption and Incidence of Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. J. Am. Hear. Assoc. 2018, 7, e008202. [Google Scholar] [CrossRef]
- Yu, S.; Guo, X.; Li, G.; Yang, H.; Zheng, L.; Sun, Y. Low educational status correlates with a high incidence of mortality among hypertensive subjects from Northeast Rural China. Front. Public Health 2022, 10, 951930. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Huo, Y.; Liu, Q.; Ahn, A.C.; Zhou, J.; Yu, R.; Chen, Z.; Wang, Y.; Liu, H. Attributable risk of all-cause mortality in hypertensive adults based on disease risk prediction model: A Chinese cohort study. J. Infect. Public Health 2020, 13, 1290–1296. [Google Scholar] [CrossRef]
- Lim, K.H.; Cheong, Y.L.; Lim, H.L.; Kee, C.C.; Ghazali, S.M.; Singh, B.S.G.P.; Omar, M.A.; Hashim, M.H.M.; Cheah, Y.K.; Lim, J.H. Assessment of association between smoking and all-cause mortality among Malaysian adult population: Findings from a retrospective cohort study. Tob. Induc. Dis. 2022, 20, 1–10. [Google Scholar] [CrossRef]
- Ouyang, F.; Cheng, X.; Zhou, W.; He, J.; Xiao, S. Increased Mortality Trends in Patients with Chronic Non-communicable Diseases and Comorbid Hypertension in the United States, 2000–2019. Front. Public Health 2022, 10, 753861. [Google Scholar] [CrossRef] [PubMed]
- Weiss, E.; Badila, E.; Japie, C.; Balahura, A.M.; Bartos, D. Target Organ Damage and Cardiovascular Risk in a Hypertensive Roma Sample Population in Romania. Maedica 2018, 13, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Casillas-Clot, J.; Pereyra-Zamora, P.; Nolasco, A. Health conditions contribution to disability burden in Spain and the role of ethnicity and migrant status: A nation-wide study. PLoS ONE 2024, 19, e0306526. [Google Scholar] [CrossRef]
- Angelov, A.; Atanassov, A.; Atanasov, V.; Gyoshev, S.; Saraivanova, J.; Volodina, V. Circulatory diseases and the wide sex and ethnic life expectancy gaps in Bulgaria since 2010. Public Health 2024, 236, 144–152. [Google Scholar] [CrossRef]
- Vallée, A.; Grave, C.; Gabet, A.; Blacher, J.; Olié, V. Treatment and adherence to antihypertensive therapy in France: The roles of socioeconomic factors and primary care medicine in the ESTEBAN survey. Hypertens. Res. 2021, 44, 550–560. [Google Scholar] [CrossRef]
- Sekkarie, A.; Fang, J.; Hayes, D.; Loustalot, F. Prevalence of Self-Reported Hypertension and Antihypertensive Medication Use Among Adults—United States, 2017–2021. Mmwr-Morbidity Mortal. Wkly. Rep. 2024, 73, 191–198. [Google Scholar] [CrossRef]
- Jin, Q.; Mei, J.; Wong, Y.C.; Lam, C.L.K.; Wan, E.Y.F. Associations and attributable burden between risk factors and all-cause and cause-specific mortality at different ages in patients with hypertension. Hypertens. Res. 2024, 47, 2053–2063. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Lo, S.H.S.; Miu, E.Y.N.; Choi, K.C. Educational programmes for improving medication adherence among older adults with coronary artery disease: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2025, 161, 104924. [Google Scholar] [CrossRef] [PubMed]
- Bekele, B.B.; Harsha, N.; Kőrösi, L.; Vincze, F.; Czifra, Á.; Ádány, R.; Sándor, J. Is Prescription Nonredemption a Source of Poor Health Among the Roma? Cross-Sectional Analysis of Drug Consumption Data From the National Health Insurance Fund of Hungary. Front. Pharmacol. 2021, 12, 616092. [Google Scholar] [CrossRef] [PubMed]
- Harsha, N.; Kőrösi, L.; Pálinkás, A.; Bíró, K.; Boruzs, K.; Ádány, R.; Sándor, J.; Czifra, Á. Determinants of Primary Nonadherence to Medications Prescribed by General Practitioners Among Adults in Hungary: Cross-Sectional Evaluation of Health Insurance Data. Front. Pharmacol. 2019, 10, 1280. [Google Scholar] [CrossRef]
- World Health Organization (WHO). How to Investigate Drug Use in Health Facilities. Selected Drug Use Indicators [Internet]. 1993. Available online: https://www.who.int/publications/i/item/who-dap-93.1 (accessed on 15 January 2025).
| Variables | Categories | Appropriate Treatment Adherence N (%) | Inappropriate Treatment Adherence N (%) | Total N | p-Value * |
|---|---|---|---|---|---|
| Age | 18–45 years 46–64 years | 1019 (61%) 2862 (87%) | 642 (39%) 439 (13%) | 1661 3301 | <0.001 |
| Sex | Male Female | 1762 (71%) 2119 (85%) | 715 (29%) 366 (15%) | 2477 2485 | <0.001 |
| Educational level | Eight years of school Vocational school Graduation Advanced | 1259 (78%) 1267 (80%) 1017 (77%) 338 (78%) | 363 (22%) 313 (20%) 312 (23%) 93 (22%) | 1622 1580 1329 431 | 0.100 |
| Roma ethnicity | Non-Roma Roma | 3653 (79%) 228 (69%) | 979 (21%) 102 (31%) | 4632 330 | <0.001 |
| Smoking | Non-smokers Current smokers Former smokers | 1654 (80%) 1456 (74%) 771 (82%) | 407 (20%) 506 (26%) 168 (18%) | 2061 1962 939 | <0.001 |
| Diabetes mellitus | No Yes | 3568 (78%) 313 (82%) | 1014 (22%) 67 (18%) | 4582 380 | 0.040 |
| Ischemic heart disease | No Yes | 3808 (78%) 73 (77%) | 1059 (22%) 22 (23%) | 4867 95 | 0.740 |
| COPD | No Yes | 3784 (79%) 97 (66%) | 1032 (21%) 49 (34%) | 4816 146 | <0.001 |
| Cancer | No Yes | 3771 (78%) 110 (73%) | 1040 (22%) 41 (27%) | 4811 151 | 0.100 |
| Lethal outcome | Survived Died | 3750 (84%) 131 (27%) | 719 (16%) 362 (73%) | 4469 493 | <0.001 |
| Total | 3881 | 1081 | 4962 |
| Variables | Categories | Lethal Outcome N (%) | Survived N (%) | Crude Mortality Rate /1000 | OR [95%CI] * | aOR [95%CI] * |
|---|---|---|---|---|---|---|
| Antihypertensive treatment adherence appropriateness | Appropriate Inappropriate | 131 (27%) 362 (73%) | 3750 (84%) 719 (16%) | 33.7 334.8 | Ref ** 14.4 [11.6–17.8] | Ref 56.2 [41.9–75.4] |
| Age | 18–45 years 46–64 years | 49 (10%) 444 (90%) | 1612 (36%) 2857 (64%) | 29.5 134.5 | Ref 5.11 [3.78–6.91] | Ref 29.8 [20.4–43.5] |
| Sex | Male Female | 320 (65%) 173 (35%) | 2157 (48%) 2312 (52%) | 129.1 69.6 | Ref 0.50 [0.41–0.61] | Ref 0.56 [0.43–0.75] |
| Educational level | Eight years of school Vocational school Graduation Advanced | 224 (45%) 155 (32%) 90 (18%) 24 (5.0%) | 1398 (31%) 1425 (32%) 1239 (28%) 407 (9.0%) | 138.1 98.1 67.7 55.6 | Ref 0.67 [0.54–0.84] 0.45 [0.35–0.58] 0.36 [0.23–0.56] | Ref 0.59 [0.43–0.82] 0.44 [0.31–0.64] 0.31 [0.17–0.56] |
| Roma ethnicity | Non-Roma Roma | 454 (92%) 39 (8.0%) | 4178 (93%) 291 (7.0%) | 98.0 118.1 | Ref 1.23 [0.87–1.74] | Ref 0.93 [0.57–1.51] |
| Smoking | Non-smokers Current smokers Former smokers | 120 (24%) 264 (54%) 109 (22%) | 1941 (43%) 1698 (38%) 830 (19%) | 58.2 134.5 116.0 | Ref 2.51 [2.00–3.15] 2.12 [1.61–2.78] | Ref 2.46 [1.81–3.34] 1.58 [1.08–2.30] |
| Diabetes mellitus | No Yes | 411 (83%) 82 (17%) | 4171 (93%) 298 (7.0%) | 89.6 215.7 | Ref 2.79 [2.14–3.63] | Ref 2.61 [1.76–3.86] |
| Ischemic heart disease | No Yes | 464 (94%) 29 (6.0%) | 4403 (98%) 66 (2.0%) | 95.3 305.2 | Ref 4.17 [2.66–6.52] | Ref 2.76 [1.47–5.18] |
| COPD | No Yes | 445 (90%) 48 (10%) | 4371 (98%) 98 (2.0%) | 92.4 328.7 | Ref 4.81 [3.36–6.88] | Ref 2.37 [1.36–4.12] |
| Cancer | No Yes | 450 (91%) 43 (9.0%) | 4361 (98%) 108 (2.0%) | 93.5 284.7 | Ref 3.85 [2.67–5.56] | Ref 3.28 [1.88–5.70] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elehamer, N.M.K.; Merzah, M.; Saeed, S.N.; Sándor, J.; Czifra, Á. Impact of Antihypertensive Treatment Adherence on Premature Mortality over Seven Years: A Follow-Up Investigation. J. Clin. Med. 2025, 14, 8321. https://doi.org/10.3390/jcm14238321
Elehamer NMK, Merzah M, Saeed SN, Sándor J, Czifra Á. Impact of Antihypertensive Treatment Adherence on Premature Mortality over Seven Years: A Follow-Up Investigation. Journal of Clinical Medicine. 2025; 14(23):8321. https://doi.org/10.3390/jcm14238321
Chicago/Turabian StyleElehamer, Nafisa Mhna Kmbo, Mohammed Merzah, Sami Najmaddin Saeed, János Sándor, and Árpád Czifra. 2025. "Impact of Antihypertensive Treatment Adherence on Premature Mortality over Seven Years: A Follow-Up Investigation" Journal of Clinical Medicine 14, no. 23: 8321. https://doi.org/10.3390/jcm14238321
APA StyleElehamer, N. M. K., Merzah, M., Saeed, S. N., Sándor, J., & Czifra, Á. (2025). Impact of Antihypertensive Treatment Adherence on Premature Mortality over Seven Years: A Follow-Up Investigation. Journal of Clinical Medicine, 14(23), 8321. https://doi.org/10.3390/jcm14238321







