Early Postoperative Mortality Risk Factors and Five- and Ten-Year Mortality Rates After Hip Arthroplasty for Femoral Neck Fracture
Abstract
1. Introduction
2. Materials and Methods
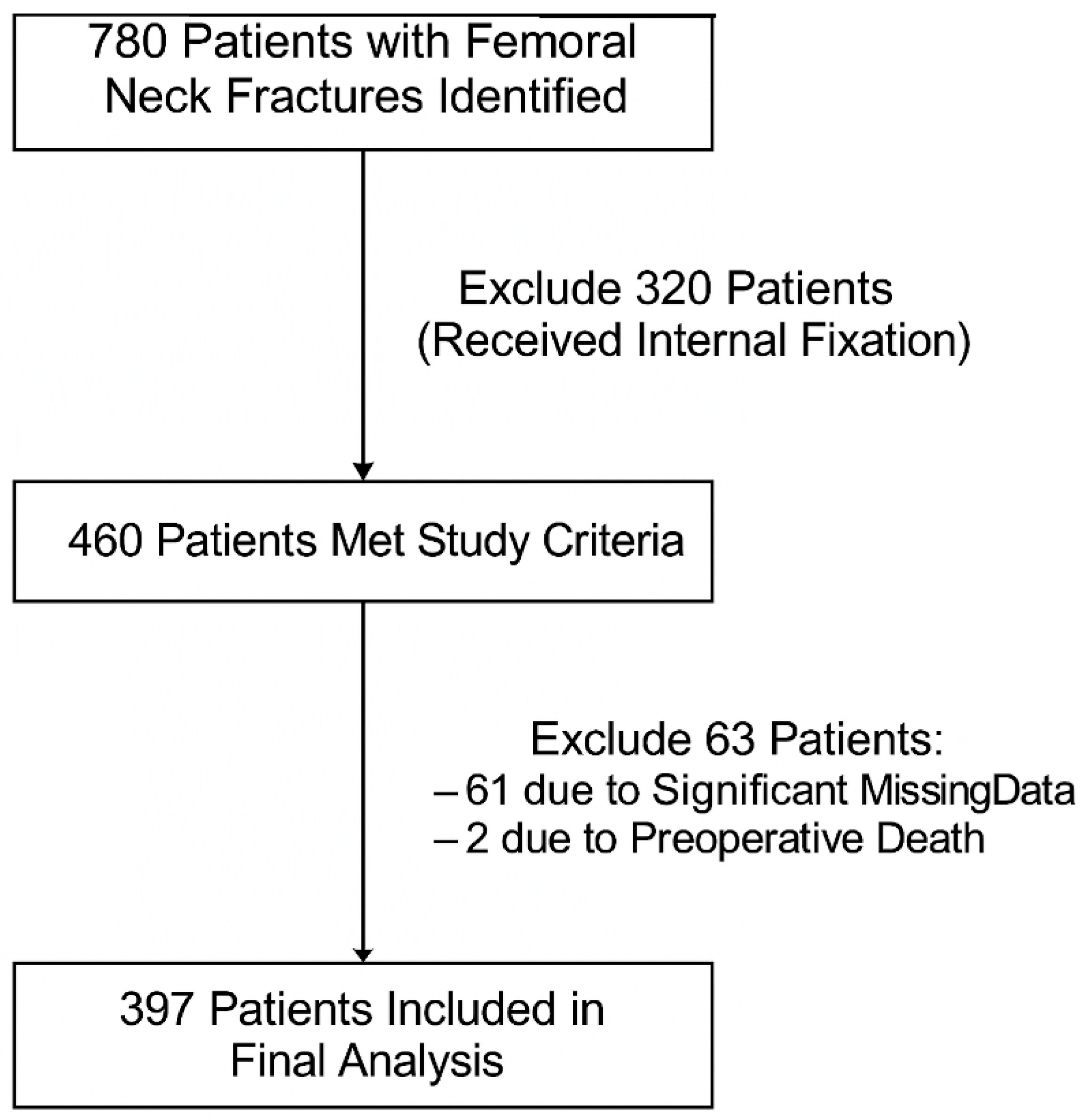
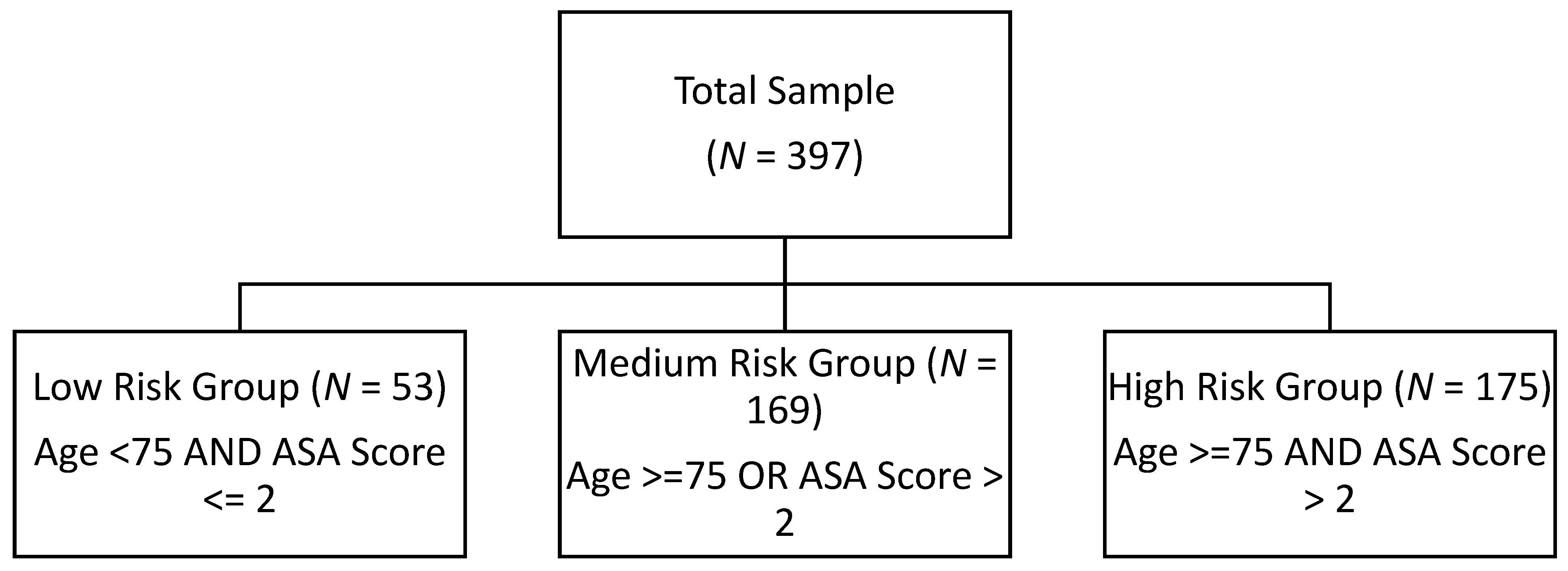
2.1. Study Design and Population
2.2. Statistical Methods
3. Results
3.1. Sample and Surgical Characteristics
3.2. Post-Op Medical and Surgical Complications
3.3. Mortality Rate
- 30-Day Mortality:
- 90-Day Mortality:
- 1-Year Mortality:
4. Discussion
4.1. Demographic and Lifestyle Factors
4.2. Preoperative Functional Status
4.3. Perioperative Characteristics
4.4. Survival Rates at 5 and 10 Years
4.5. Practical Implementation of Risk Stratification Tools
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sing, C.W.; Lin, T.C.; Bartholomew, S.; Bell, J.S.; Bennett, C.; Beyene, K.; Bosco-Levy, P.; Bradbury, B.D.; Chan, A.H.Y.; Chandran, M.; et al. Global Epidemiology of Hip Fractures: Secular Trends in Incidence Rate, Post-Fracture Treatment, and All-Cause Mortality. J. Bone Miner. Res. 2023, 38, 1064–1075. [Google Scholar] [CrossRef]
- Feng, J.N.; Zhang, C.G.; Li, B.H.; Zhan, S.Y.; Wang, S.F.; Song, C.L. Global burden of hip fracture: The Global Burden of Disease Study. Osteoporos. Int. 2024, 35, 41–52. [Google Scholar] [CrossRef]
- Papadimitriou, N.; Tsilidis, K.K.; Orfanos, P.; Benetou, V.; Ntzani, E.E.; Soerjomataram, I.; Künn-Nelen, A.; Pettersson-Kymmer, U.; Eriksson, S.; Brenner, H.; et al. Burden of hip fracture using disability-adjusted life-years: A pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health 2017, 2, e239–e246. [Google Scholar] [CrossRef]
- Tate, J.P.; Reinhart, N.M.; Desai, N.; Collins, L.K.; Sherman, W.F. Who Is on Call? Trends in Hemiarthroplasty Versus Total Hip Arthroplasty for Femoral Neck Fractures Based on Subspecialty Training. J. Arthroplast. 2025, in press. [CrossRef] [PubMed]
- Moldovan, F.; Moldovan, L. A Modeling Study for Hip Fracture Rates in Romania. J. Clin. Med. 2025, 14, 3162. [Google Scholar] [CrossRef]
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Catherine Sherrington for the Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. [Google Scholar] [CrossRef]
- Prestmo, A.; Hagen, G.; Sletvold, O.; Helbostad, J.L.; Thingstad, P.; Taraldsen, K.; Lydersen, S.; Halsteinli, V.; Saltnes, T.; Lamb, S.E.; et al. Comprehensive geriatric care for patients with hip fractures: A prospective, randomised, controlled trial. Lancet 2015, 385, 1623–1633. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Foss, N.B.; Ekdahl, C.; Kehlet, H. Prefracture functional level evaluated by the New Mobility Score predicts in-hospital outcome after hip fracture surgery. Acta Orthop. 2010, 81, 296–302. [Google Scholar] [CrossRef]
- Gao, F.; Liu, G.; Ge, Y.; Tan, Z.; Chen, Y.; Peng, W.; Zhang, J.; Zhang, X.; He, J.; Wen, L.; et al. Orthogeriatric co-managements lower early mortality in long-lived elderly hip fracture: A post-hoc analysis of a prospective study. BMC Geriatr. 2023, 23, 571. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Carrozzino, D.; Guidi, J.; Patierno, C. Charlson Comorbidity Index: A Critical Review of Clinimetric Properties. Psychother. Psychosom. 2022, 91, 8–35. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.J.; Palmer, C.R. A new mobility score for predicting mortality after hip fracture. J. Bone Jt. Surg. Br. 1993, 75, 797–798. [Google Scholar] [CrossRef]
- Major, L.J.; North, J.B. Predictors of mortality in patients with femoral neck fracture. J. Orthop. Surg. 2016, 24, 150–152. [Google Scholar] [CrossRef]
- Meessen, J.M.T.A.; Pisani, S.; Gambino, M.L.; Bonarrigo, D.; Van Schoor, N.M.; Fozzato, S.; Cherubino, P.; Surace, M.F. Assessment of mortality risk in elderly patients after proximal femoral fracture. Orthopedics 2014, 37, e194–e200. [Google Scholar] [CrossRef] [PubMed]
- Petersen, M.B.; Jørgensen, H.L.; Hansen, K.; Duus, B.R. Factors affecting postoperative mortality of patients with displaced femoral neck fracture. Injury 2006, 37, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Turan, O.; Pan, X.; Kunze, K.N.; Rullan, P.J.; Emara, A.K.; Molloy, R.M.; Piuzzi, N.S. 30-day to 10-year mortality rates following total hip arthroplasty: A meta-analysis of the last decade (2011–2021). Hip Int. 2024, 34, 4–14. [Google Scholar] [CrossRef]
- Voeten, S.C.; Nijmeijer, W.S.; Vermeer, M.; Schipper, I.B.; Hegeman, J.H. Validation of the Fracture Mobility Score against the Parker Mobility Score in hip fracture patients. Injury 2020, 51, 395–399. [Google Scholar] [CrossRef]
- Norring-Agerskov, D.; Laulund, A.S.; Lauritzen, J.B.; Duus, B.R.; van der Mark, S.; Mosfeldt, M.; Jørgensen, H.L. Metaanalysis of risk factors for mortality in patients with hip fracture. Dan. Med. J. 2013, 60, A4675. [Google Scholar] [PubMed]
- Hendrix, J.M.; Garmon, E.H. American Society of Anesthesiologists Physical Status Classification System; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Kim, C.H.; Lim, E.J.; Lee, J. Clinical Outcomes following Primary Hip Replacement Arthroplasties in Patients with Solid Organ Transplantation: A Systematic Review and Meta-Analysis. Hip Pelvis. 2022, 34, 127–139. [Google Scholar] [CrossRef]
- Daugaard, C.L.; Jorgensen, H.L.; Riis, T.; Lauritzen, J.B.; Duus, B.R.; Van Der Mark, S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop. 2012, 83, 609–613. [Google Scholar] [CrossRef]
- Shiga, T.; Wajima, Z.; Ohe, Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can. J. Anaesth. 2008, 55, 146–154. [Google Scholar] [CrossRef]
- Castellanos, S.C.; Marco, F.L.; Domínguez, E.B.; Gálvez, E.M.V.; Pérez, B.M. Does delaying surgery for “healthy” hip fracture patients have increased complications and mortality? Injury 2022, 53, 3209–3213. [Google Scholar] [CrossRef]
- Yoo, J.; Lee, J.S.; Kim, S.; Kim, B.S.; Choi, H.; Song, D.Y.; Kim, W.B.; Won, C.W. Length of hospital stay after hip fracture surgery and 1-year mortality. Osteoporos. Int. 2019, 30, 145–153. [Google Scholar] [CrossRef]
- Ek, S.; Meyer, A.C.; Hedström, M.; Modig, K. Hospital Length of Stay After Hip Fracture and It’s Association With 4-Month Mortality-Exploring the Role of Patient Characteristics. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 1472–1477. [Google Scholar] [CrossRef]
- Jeon, C.Y.; Neidell, M.; Jia, H.; Sinisi, M.; Larson, E. On the role of length of stay in healthcare-associated bloodstream infection. Infect Control Hosp. Epidemiol. 2012, 33, 1213–1218. [Google Scholar] [CrossRef]
- Jolles, B.M.; Bogoch, E.R. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst. Rev. 2004, CD003828. [Google Scholar] [CrossRef] [PubMed]
- Voskuijl, T.; Neuhaus, V.; Kinaci, A.; Vrahas, M.; Ring, D. In-Hospital Outcomes after Hemiarthroplasty versus Total Hip Arthroplasty for Isolated Femoral Neck Fractures. Arch. Bone Jt. Surg. 2014, 2, 151. [Google Scholar] [PubMed]
- Total Hip Arthroplasty or Hemiarthroplasty for Hip Fracture. N. Engl. J. Med. 2019, 381, 2199–2208. [CrossRef]
- Lewis, D.P.; Wæver, D.; Thorninger, R.; Donnelly, W.J. Hemiarthroplasty vs Total Hip Arthroplasty for the Management of Displaced Neck of Femur Fractures: A Systematic Review and Meta-Analysis. J. Arthroplast. 2019, 34, 1837–1843.e2. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Bi, N.; Zheng, J.; Xi, N. Does total hip arthroplasty provide better outcomes than hemiarthroplasty for the femoral neck fracture? A systematic review and meta-analysis. Chin. J. Traumatol. 2020, 23, 356. [Google Scholar] [CrossRef]
- Vail, E.A.; Feng, R.; Sieber, F.; Carson, J.L.; Ellenberg, S.S.; Magaziner, J.; Dillane, D.; Marcantonio, E.R.; Sessler, D.I.; Ayad, S.; et al. Long-term Outcomes with Spinal versus General Anesthesia for Hip Fracture Surgery: A Randomized Trial. Anesthesiology 2024, 140, 375–386. [Google Scholar] [CrossRef]
- Neuman, M.D.; Rosenbaum, P.R.; Ludwig, J.M.; Zubizarreta, J.R.; Silber, J.H. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA 2014, 311, 2508–2517. [Google Scholar] [CrossRef]
- Lin, D.Y.; Woodman, R.; Oberai, T.; Brown, B.; Morrison, C.; Kroon, H.; Jaarsma, R. Association of anesthesia and analgesia with long-term mortality after hip fracture surgery: An analysis of the Australian and New Zealand hip fracture registry. Reg. Anesth. Pain Med. 2023, 48, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Koole, C.; Bleeser, T.; Hoogma, D.F.; Coppens, S.; Teunkens, A.; Rex, S. Haemodynamic effects of continuous spinal anaesthesia versus single-shot spinal anaesthesia or general anaesthesia for hip fracture surgery: A systematic review and meta-analysis. Br. J. Anaesth. 2024, 132, 1160–1162. [Google Scholar] [CrossRef]
- D’Amico, F.; Fominskiy, E.V.; Turi, S.; Pruna, A.; Fresilli, S.; Triulzi, M.; Zangrillo, A.; Landoni, G. Intraoperative hypotension and postoperative outcomes: A meta-analysis of randomised trials. Br. J. Anaesth. 2023, 131, 823–831. [Google Scholar] [CrossRef]
- Culver, D.H.; Horan, T.C.; Gaynes, R.P.; Martone, W.J.; Jarvis, W.R.; Emori, T.G.; Banerjee, S.N.; Edwards, J.R.; Henderson, T.S.; Hughes, J.M.; et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. Am. J. Med. 1991, 91, S152–S157. [Google Scholar] [CrossRef]
- Morales, C. Surgical site infection in abdominal trauma patients: Risk prediction and performance of the NNIS and SENIC indexes. Can. J. Surg. 2011, 54, 17–24. [Google Scholar] [CrossRef]
- Greenhalgh, M.S.; Gowers, B.T.V.; Iyengar, K.P.; Adam, R.F. Blood transfusions and hip fracture mortality—A retrospective cohort study. J. Clin. Orthop. Trauma 2021, 21, 101506. [Google Scholar] [CrossRef] [PubMed]
- Loh, B.; Jiang, L.; Timing, L.; Kong, N.; Ganesan, G.; Tan, K.B.; Bee, S.; Koh, J.S.B.; Howe, T.S.; Huei, N.Y. Predictors of 10-year Mortality After Hip Fracture Surgery in a Pre-Pandemic Cohort. Geriatr. Orthop. Surg. Rehabil. 2023, 14, 21514593231216560. [Google Scholar] [CrossRef] [PubMed]
- Tiihonen, R.; Alaranta, R.; Helkamaa, T.; Nurmi-Lüthje, I.; Kaukonen, J.P.; Lüthje, P. A 10-Year Retrospective Study of 490 Hip Fracture Patients: Reoperations, Direct Medical Costs, and Survival. Scand J. Surg. 2019, 108, 178–184. [Google Scholar] [CrossRef]
- Paksima, N.; Koval, K.J.; Aharanoff, G.; Walsh, M.; Kubiak, E.N.; Zuckerman, J.D.; Egol, K.A. Predictors of mortality after hip fracture: A 10-year prospective study. Bull. NYU Hosp. Jt. Dis. 2008, 66, 111. [Google Scholar]
| Characteristics | Mean ± Std or N (%) | |
|---|---|---|
| Age | 83.26 ± 10.4 | |
| BMI | 23.09 ± 3.84 | |
| Gender | Male | 118 (29.7%) |
| Female | 279 (70.3%) | |
| Smoker (N = 384) | Yes | 42 (10.9%) |
| No | 342 (89.1%) | |
| Surgical Side | Right | 186 (46.9%) |
| Left | 211 (53.1%) | |
| Garden Classification | I | 3 (0.8%) |
| II | 5 (1.3%) | |
| III | 38 (9.6%) | |
| IV | 351 (88.4%) | |
| Surgical Approach | Postero-lateral | 335 (84.4%) |
| Antero-lateral | 53 (13.4%) | |
| Hardinge | 6 (1.5%) | |
| Hueter | 3 (0.8%) | |
| Hip Replacement | Total | 140 (35.3%) |
| Hemiarthroplasty | 257 (64.7%) | |
| Cemented Prosthesis | Yes | 59 (14.9%) |
| No | 338 (85.1%) | |
| Total Charlson Score | N (%) | ASA Score | N (%) | Parker Mobility Score (N = 352) | N (%) |
|---|---|---|---|---|---|
| 0 | 2 (0.5%) | 1 | 40 (10.1%) | 0 | 2 (0.6%) |
| 1 | 6 (1.5%) | 2 | 168 (42.3%) | 1 | 6 (1.7%) |
| 2 | 13 (3.3%) | 3 | 170 (42.8%) | 2 | 22 (6.3%) |
| 3 | 27 (6.8%) | 4 | 19 (4.8%) | 3 | 48 (13.6%) |
| 4 | 71 (17.9%) | 4 | 57 (16.2%) | ||
| 5 | 94 (23.7%) | 5 | 36 (10.2%) | ||
| 6 | 75 (18.9%) | 6 | 37 (10.5%) | ||
| 7 | 55 (13.9%) | 7 | 26 (7.4%) | ||
| 8 | 29 (7.3%) | 8 | 8 (2.3%) | ||
| 9 | 20 (5.0%) | 9 | 110 (31.3%) | ||
| 10 | 4 (1.0%) | ||||
| 13 | 1 (0.3%) |
| Complications | N (%) |
|---|---|
| Heart Failure | 1 (0.3%) |
| Anaphylactic Shock | 1 (0.3%) |
| Acute Pulmonary Edema | 1 (0.3%) |
| Complications | N (%) | Complications | N (%) |
|---|---|---|---|
| Acute Coronary Syndrome | 1 (0.3%) | Hypoglycemia | 1 (0.3%) |
| Acute Urinary Retention | 2 (0.5%) | Melena | 1 (0.3%) |
| Acute Kidney Injury | 2 (0.5%) | Oral Mycosis | 1 (0.3%) |
| Anemia | 3 (0.8%) | Phlebitis | 1 (0.3%) |
| Atrial Fibrillation | 1 (0.3%) | Pneumonia | 7 (1.8%) |
| Cardiopulmonary Arrest | 1 (0.3%) | Prostatitis | 1 (0.3%) |
| Delirium | 5 (1.3%) | Pulmonary Embolism | 2 (0.5%) |
| Deep Venous Thrombosis | 4 (1%) | Respiratory Failure | 1 (0.3%) |
| Esophagitis | 1 (0.3%) | Uncontrolled Diabetes | 1 (0.3%) |
| Heart Failure | 4 (1%) | Upper Respiratory Infection | 1 (0.3%) |
| Hematoma | 1 (0.3%) | Urinary Tract Infection | 13 (3.3%) |
| Complications | N (%) | Complications | N (%) |
|---|---|---|---|
| Acetabular Implant Loosening | 1 (0.3%) | No osteointegration | 1 (0.3%) |
| Bowel Obstruction | 1 (0.3%) | Painful Scar | 1 (0.3%) |
| Delayed Wound Healing | 1 (0.3%) | Periprosthetic Fracture | 8 (2%) |
| Dislocation | 15 (3.8%) | Prosthesis Subsidence | 3 (0.8%) |
| Gluteus Medius Tendinopathy | 2 (0.5%) | Quadriceps Muscular Atrophy | 1 (0.3%) |
| Hematoma | 6 (1.5%) | Sciatic Nerve Injury | 2 (0.5%) |
| Leg Length Discrepancy | 1 (0.3%) | Wound Dehiscence | 1 (0.3%) |
| Risk Groups | p-Value | |||
|---|---|---|---|---|
| Low (N = 53) | Medium (N = 169) | High (N = 175) | ||
| 30 Days Mortality (N = 14) | 0 (0%) | 1 (0.6%) | 13 (7.4%) | <0.001 |
| 90 Days Mortality (N = 28) | 0 (0%) | 5 (3%) | 23 (13.1%) | <0.001 |
| 1 Year Mortality (N = 56) | 0 (0%) | 18 (10.7%) | 38 (21.7%) | <0.001 |
| 30 Days Mortality | p-Value | 90 Days Mortality | p-Value | 1 Year Mortality | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | |||||
| Age (years) | 83.08 ± 10.48 | 88.14 ± 5.53 | 0.064 | 83 ± 10.56 | 86.68 ± 7.25 | 0.099 | 82.67 ± 10.74 | 86.86 ± 7.09 | 0.006 | |
| BMI | 23.09 ± 3.83 | 22.90 ± 4.15 | 0.992 | 23.14 ± 3.74 | 22.32 ± 5.05 | 0.167 | 23.20 ± 3.785 | 22.38 ± 4.136 | 0.125 | |
| Gender | Male | 109 (92.4%) | 9 (7.6%) | 0.007 | 105 (89%) | 13 (11%) | 0.045 | 92 (78%) | 26 (22%) | 0.003 |
| Female | 274 (98.2%) | 5 (1.8%) | 264 (94.6%) | 15 (5.4%) | 249 (89.2%) | 30 (10.8%) | ||||
| Smoker | No | 329 (96.2%) | 13 (3.8%) | 1 | 317 (92.7%) | 25 (7.3%) | 1 | 296 (86.5%) | 46 (13.5%) | 0.164 |
| Yes | 41 (97.6%) | 1 (2.4%) | 39 (92.9%) | 3 (7.1%) | 33 (78.6%) | 9 (21.4%) | ||||
| Hospitalization period (Days) | 9.51 ± 6.32 | 10.3 ± 4.72 | 0.696 | 9.36 ± 5.86 | 12.20 ± 10.68 | 0.208 | 9.275 ± 5.91 | 11.21 ± 8.11 | 0.038 | |
| OR Delay (hours) | 42.89 ± 69.89 | 72.39 ± 54.03 | 0.119 | 43.26 ± 71.02 | 52.77 ± 45.98 | 0.486 | 43.36 ± 73.21 | 47.40 ± 41.07 | 0.687 | |
| Nutritional Status (Proteins) | 69.23 ± 6.52 | 65.92 ± 6.84 | 0.055 | 69.16 ± 6.49 | 68.5 ± 7.37 | 0.57 | 69.13 ± 6.36 | 69 ± 7.61 | 0.925 | |
| Aspirin | No | 290 (97%) | 9 (3%) | 1 | 280 (93.6%) | 19 (6.4%) | 0.617 | 262 (87.6%) | 37 (12.4%) | 0.177 |
| Yes | 86 (96.6%) | 3 (3.4%) | 82 (92.1%) | 7 (7.9%) | 73 (82%) | 16 (18%) | ||||
| Clopidogrel | No | 360 (97.3%) | 10 (2.7%) | 0.021 | 347 (93.8%) | 23 (6.2%) | 0.035 | 322 (87%) | 48 (13%) | 0.035 |
| Yes | 16 (84.2%) | 3 (15.8%) | 15 (78.9%) | 4 (21.1%) | 13 (68.4%) | 6 (31.6%) | ||||
| Antivitamin K | No | 279 (97.2%) | 8 (2.8%) | 0.214 | 271 (94.4%) | 16 (5.6%) | 0.043 | 252 (87.8%) | 35 (12.2%) | 0.046 |
| Yes | 98 (94.2%) | 6 (5.8%) | 92 (88.5%) | 12 (11.5%) | 83 (79.8%) | 21 (20.2%) | ||||
| NOACs | No | 371 (96.4%) | 14 (3.6%) | 1 | 357 (92.7%) | 28 (7.3%) | 1 | 330 (85.7%) | 55 (14.3%) | 1 |
| Yes | 6 (100%) | 0 (0%) | 6 (100%) | 0 (0%) | 5 (83.3%) | 1 (16.7%) | ||||
| Immunosuppressant | No | 358 (97%) | 11 (3%) | 0.057 | 346 (93.8%) | 23 (6.2%) | 0.029 | 322 (87.3%) | 47 (12.7%) | 0.006 |
| Yes | 23 (88.5%) | 3 (11.5%) | 21 (80.8%) | 5 (19.2%) | 17 (65.4%) | 9 (34.6%) | ||||
| Parker Mobility Score | 5.897 ± 2.575 | 4.583 ± 1.928 | 0.04 | 5.929 ± 2.594 | 4.791 ± 1.864 | 0.009 | 6.053 ± 2.598 | 4.666 ± 2.006 | <0.001 | |
| Total Charlson Score | 5.41 ± 1.875 | 6.86 ± 1.46 | 0.004 | 5.398 ± 1.889 | 6.25 ± 1.554 | 0.021 | 5.263 ± 1.816 | 6.642 ± 1.833 | <0.001 | |
| NNIS Score | 0 | 202 (99.5%) | 1 (0.5%) | 0.002 | 200 (98.5%) | 3 (1.5%) | <0.001 | 189 (93.1%) | 14 (6.9%) | <0.001 |
| 1 | 175 (93.1%) | 13 (6.9%) | 163 (86.7%) | 25 (13.3%) | 146 (77.7%) | 42 (22.3%) | ||||
| 2 | 6 (100.0%) | 0 (0%) | 6 (100.0%) | 0 (0.0%) | 6 (100.0%) | 0 (0.0%) | ||||
| ASA Score | 1 | 40 (100%) | 0 (0%) | <0.001 | 40 (100%) | 0 (0%) | <0.001 | 40 (100%) | 0 (0%) | <0.001 |
| 2 | 167 (99.4%) | 1 (0.6%) | 165 (98.2%) | 3 (1.8%) | 154 (91.7%) | 14 (8.3%) | ||||
| 3 | 160 (94.1%) | 10 (5.9%) | 149 (87.6%) | 21 (12.4%) | 135 (79.4%) | 35 (20.6%) | ||||
| 4 | 16 (84.2%) | 3 (15.8%) | 15 (78.9%) | 4 (21.1%) | 12 (63.2%) | 7 (36.8%) | ||||
| pRBCs Transfusion | No | 276 (97.2%) | 8 (2.8%) | 0.236 | 268 (94.4%) | 16 (5.6%) | 0.08 | 255 (89.8%) | 29 (10.2%) | <0.001 |
| Yes | 107 (94.7%) | 6 (5.3%) | 101 (89.4%) | 12 (10.6%) | 86 (76.1%) | 27 (23.9%) | ||||
| Surgical Side | Right | 179 (96.2%) | 7 (3.8%) | 0.81 | 174 (93.5%) | 12 (6.5%) | 0.66 | 165 (88.7%) | 21 (11.3%) | 0.13 |
| Left | 204 (96.7%) | 7 (3.3%) | 195 (92.4%) | 16 (7.6%) | 176 (83.4%) | 35 (16.6%) | ||||
| Garden Classification | I | 3 (100%) | 0 (0%) | 0.513 | 3 (100%) | 0 (0%) | 0.676 | 3 (100%) | 0 (0%) | 0.783 |
| II | 4 (80%) | 1 (20%) | 4 (80%) | 1 (20%) | 4 (80%) | 1 (20%) | ||||
| III | 37 (97.4%) | 1 (2.6%) | 36 (94.7%) | 2 (5.3%) | 33 (86.8%) | 5 (13.2%) | ||||
| IV | 339 (96.6%) | 12 (3.4%) | 326 (92.9%) | 25 (7.1%) | 301 (85.8%) | 50 (14.2%) | ||||
| Type of hip arthroplasty | HA | 244 (94.9%) | 13 (5.1%) | 0.024 | 232 (90.3%) | 25 (9.7%) | 0.005 | 209 (81.3%) | 48 (18.7%) | <0.001 |
| THA | 139 (99.3%) | 1 (0.7%) | 137 (97.9%) | 3 (2.1%) | 132 (94.3%) | 8 (5.7%) | ||||
| Approach | PL | 323 (96.4%) | 12 (3.6%) | 0.883 | 311 (92.8%) | 24 (7.2%) | 0.743 | 292 (87.2%) | 43 (12.8%) | 0.243 |
| AL | 51 (96.2%) | 2 (3.8%) | 50 (94.3%) | 3 (5.7%) | 41 (77.4%) | 12 (22.6%) | ||||
| Hardinge | 6 (100%) | 0 (0%) | 5 (83.3%) | 1 (16.7%) | 5 (83.3%) | 1 (16.7%) | ||||
| Hueter | 3 (100%) | 0 (0%) | 3 (100%) | 0 (0%) | 3 (100%) | 0 (0%) | ||||
| Cemented | No | 325 (96.2%) | 13 (3.8%) | 0.703 | 313 (92.6%) | 25 (7.4%) | 0.782 | 287 (84.9%) | 51 (15.1%) | 0.178 |
| Yes | 58 (98.3%) | 1 (1.7%) | 56 (94.9%) | 3 (5.1%) | 54 (91.5%) | 5 (8.5%) | ||||
| Anesthesia | GA | 200 (97.6%) | 5 (2.4%) | 0.207 | 194 (94.6%) | 11 (5.4%) | 0.028 | 183 (89.3%) | 22 (10.7%) | 0.011 |
| SSS | 162 (96.4%) | 6 (3.6%) | 157 (93.5%) | 11 (6.5%) | 143 (85.1%) | 25 (14.9%) | ||||
| CS | 20 (87%) | 3 (13%) | 17 (73.9%) | 6 (26.1%) | 14 (60.9%) | 9 (39.1%) | ||||
| Regional | 1 (100%) | 0 (0%) | 1 (100%) | 0 (0%) | 1 (100%) | 0 (0%) | ||||
| Complications pre-op | No | 380 (96.4%) | 14 (3.6%) | 1 | 367 (93.1%) | 27 (6.9%) | 0.197 | 339 (86%) | 55 (14%) | 0.367 |
| Yes | 3 (100%) | 0 (0%) | 2 (66.7%) | 1 (33.3%) | 2 (66.7%) | 1 (33.3%) | ||||
| Medical Complications post-op | No | 326 (98.2%) | 6 (1.8%) | <0.001 | 314 (94.6%) | 18 (5.4%) | 0.013 | 293 (88.3%) | 39 (11.7%) | 0.002 |
| Yes | 57 (87.7%) | 8 (12.3%) | 55 (84.6%) | 10 (15.4%) | 48 (73.8%) | 17 (26.2%) | ||||
| Surgical Complications post-op | No | 337 (96.3%) | 13 (3.7%) | 1 | 327 (93.4%) | 23 (6.6%) | 0.356 | 302 (86.3%) | 48 (13.7%) | 0.541 |
| Yes | 46 (97.9%) | 1 (2.1%) | 42 (89.4%) | 5 (10.6%) | 39 (83%) | 8 (17%) | ||||
| Age | BMI | OR Delay (hours) | Hospitalization Period (Days) | Nutritional Status (Proteins) | Parker Mobility Score | Total Charlson Score | ASA score | |
|---|---|---|---|---|---|---|---|---|
| 30 Days Mortality | 0.090 | −0.009 | 0.078 | 0.020 | −0.095 | −0.093 | 0.142 ** | 0.187 *** |
| 90 Days Mortality | 0.091 | −0.053 | 0.035 | 0.109 * | −0.026 | −0.112 * | 0.116 * | 0.229 *** |
| 1 Year Mortality | 0.140 ** | −0.075 | 0.020 | 0.105 * | −0.007 | −0.190 *** | 0.256 *** | 0.249 *** |
| Variables | Hazard Ratio | 95% CI for HR | p-Value |
|---|---|---|---|
| Age (years) | 1.01 | 0.97–1.05 | 0.573 |
| Gender (Ref: Female) | 1.64 | 0.92–2.90 | 0.093 |
| ASA score (Ref: ASA IV) | |||
| ASA I | 0.00 | 0.00–3.04 × 103 | 0.970 |
| ASA II | 0.30 | 0.11–0.81 | 0.017 |
| ASA III | 0.40 | 0.17–0.95 | 0.038 |
| Charlson Comorbidity Index | 1.23 | 1.04–1.47 | 0.018 |
| Parker Mobility Score | 0.86 | 0.76–0.97 | 0.014 |
| Post-op Medical Complication (Ref: No Complication) | 2.88 | 1.56–5.34 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khalil, K.; Jamaleddine, Y.; Haj Hussein, A.; Daccache, E.; Mouawad, J.; Fricault, G.; Khoury, A.; Reina, N. Early Postoperative Mortality Risk Factors and Five- and Ten-Year Mortality Rates After Hip Arthroplasty for Femoral Neck Fracture. J. Clin. Med. 2025, 14, 8263. https://doi.org/10.3390/jcm14238263
Khalil K, Jamaleddine Y, Haj Hussein A, Daccache E, Mouawad J, Fricault G, Khoury A, Reina N. Early Postoperative Mortality Risk Factors and Five- and Ten-Year Mortality Rates After Hip Arthroplasty for Femoral Neck Fracture. Journal of Clinical Medicine. 2025; 14(23):8263. https://doi.org/10.3390/jcm14238263
Chicago/Turabian StyleKhalil, Khalil, Youssef Jamaleddine, Ahmad Haj Hussein, Elio Daccache, Joseph Mouawad, Guillaume Fricault, Alfred Khoury, and Nicolas Reina. 2025. "Early Postoperative Mortality Risk Factors and Five- and Ten-Year Mortality Rates After Hip Arthroplasty for Femoral Neck Fracture" Journal of Clinical Medicine 14, no. 23: 8263. https://doi.org/10.3390/jcm14238263
APA StyleKhalil, K., Jamaleddine, Y., Haj Hussein, A., Daccache, E., Mouawad, J., Fricault, G., Khoury, A., & Reina, N. (2025). Early Postoperative Mortality Risk Factors and Five- and Ten-Year Mortality Rates After Hip Arthroplasty for Femoral Neck Fracture. Journal of Clinical Medicine, 14(23), 8263. https://doi.org/10.3390/jcm14238263





