Supportive Text Messaging and Peer Support for Patients in the 6 Months Following Discharge from a Psychiatric Admission: Mental Health Outcomes from a Cluster-Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Design
2.2. Data Collection and Inclusion Criteria
2.3. Ethics Statement
2.4. Sample Size Calculation
2.5. Outcome Measures
2.5.1. Generalized Anxiety Disorder Scale (GAD-7)
2.5.2. Patient Health Questionnaire (PHQ-9)
2.5.3. World Health Organization-Five Well-Being Index (WHO-5)
2.6. Statistical Analysis
3. Results
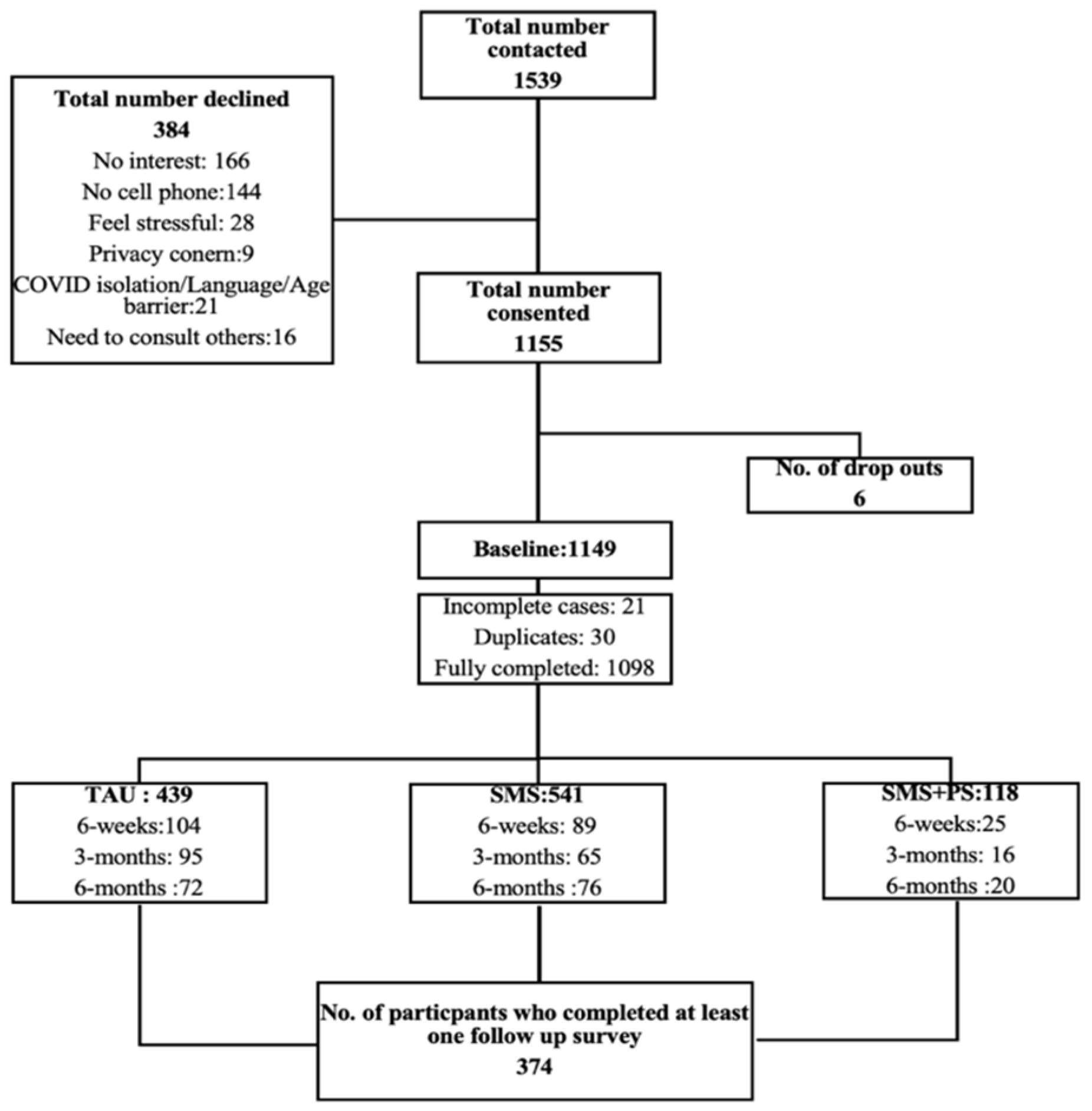
3.1. Summary of Study Recruitment and Enrollment
3.2. Baseline Data Analysis
3.3. ANOVA Analysis
| Variable | TAU (M ± SD) | SMS (M ± SD) | SMS+PS (M ± SD) | Chi Square | df | p-Value |
|---|---|---|---|---|---|---|
| GAD-7 | 8.78 ± 5.76 | 8.32 ± 5.71 | 7.77 ± 4.67 | 8.94 | 2 | 0.01 * |
| PHQ-9 | 11.01 ± 6.56 | 11.39 ± 6.80 | 11.26 ± 5.27 | 1.86 | 2 | 0.40 |
| WHO-5 | 51.68 ± 23.38 | 52.02 ± 23.43 | 47.80 ± 21.33 | 3.62 | 2 | 0.16 |
| Suicidal Ideation | 0.76 ± 0.96 | 0.79 ± 0.99 | 0.75 ± 0.81 | 7.51 | 6 | 0.75 |
| Sleep Issues | 1.44 ± 1.06 | 1.48 ± 1.04 | 1.49 ± 0.86 | 3.47 | 6 | 0.28 |
3.4. ANCOVA Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ED | Emergency Department |
| CIHI | Canadian Institute for Health Information |
| TAU | Treatment as Usual |
| SMS | Supportive Text Messaging |
| SMS+PS | Supportive Text Messaging Plus Peer Support |
| ORs | Odds Ratios |
| CIs | Confidence Intervals |
| GAD-7 | Generalized Anxiety Disorder Scale |
| PHQ-9 | Patient Health Questionnaire |
| WHO-5 | World Health Organization-Five Well-Being Index |
| ANCOVA | Analysis of Covariance |
References
- Mao, W.; Shalaby, R.; Owusu, E.; Elgendy, H.; Shalaby, N.; Agyapong, B.; Nichols, A.; Eboreime, E.; Nkire, N.; Agyapong, V.I.O. Status after Hospital Discharge: An Observational Study of the Progression of Patients’ Mental Health Symptoms Six Weeks after Hospital Discharge. J. Clin. Med. 2023, 12, 7559. [Google Scholar] [CrossRef]
- Smith, T.E.; Haselden, M.; Corbeil, T.; Wall, M.M.; Tang, F.; Essock, S.M.; Frimpong, E.; Goldman, M.L.; Mascayano, F.; Radigan, M.; et al. Effect of scheduling a post-discharge outpatient mental health appointment on the likelihood of successful transition from hospital to community-based care. J. Clin. Psychiatry 2020, 81, 18891. [Google Scholar] [CrossRef]
- Gillard, S.; White, R.; Miller, S.; Turner, K. Open access support groups for people experiencing personality disorders: Do group members’ experiences reflect the theoretical foundations of the SUN project? Psychol. Psychother. Theory Res. Pract. 2015, 88, 87–104. [Google Scholar] [CrossRef]
- Vigod, S.N.; Kurdyak, P.A.; Dennis, C.-L.; Leszcz, T.; Taylor, V.H.; Blumberger, D.M.; Seitz, D.P. Transitional interventions to reduce early psychiatric readmissions in adults: Systematic review. Br. J. Psychiatry 2013, 202, 187–194. [Google Scholar] [CrossRef]
- Canadian Institute for Health Information. Health Indicators. 2008. Available online: https://secure.cihi.ca/free_products/HealthIndicators2008_FRweb.pdf (accessed on 25 March 2025).
- Eboreime, E.; Shalaby, R.; Mao, W.; Owusu, E.; Vuong, W.; Surood, S.; Bales, K.; MacMaster, F.P.; McNeil, D.; Rittenbach, K.; et al. Reducing readmission rates for individuals discharged from acute psychiatric care in Alberta using peer and text message support: Protocol for an innovative supportive program. BMC Health Serv. Res. 2022, 22, 332. [Google Scholar] [CrossRef]
- Herman, D.; Conover, S.; Gorroochurn, P.; Hinterland, K.; Hoepner, L.; Susser, E. A randomized trial of critical time intervention in persons with severe mental illness following institutional discharge. Psychiatr. Serv. 2011, 62, 713–719. [Google Scholar] [CrossRef]
- Forchuk, C.; Martin, M.L.; Jensen, E.; Ouseley, S.; Sealy, P.; Beal, G.; Reynolds, W.; Sharkey, S. Integrating an evidence-based intervention into clinical practice: ‘Transitional relationship model’. J. Psychiatr. Ment. Health Nurs. 2013, 20, 584–594. [Google Scholar] [CrossRef]
- Wakeman, S.E.; Rigotti, N.A.; Chang, Y.; Herman, G.E.; Erwin, A.; Regan, S.; Metlay, J.P. Effect of integrating substance use disorder treatment into primary care on inpatient and emergency department utilization. J. Gen. Intern. Med. 2019, 34, 871–877. [Google Scholar] [CrossRef]
- Abraham, O.; Myers, M.N.; Brothers, A.L.; Montgomery, J.; Norman, B.A.; Fabian, T. Assessing need for pharmacist involvement to improve care coordination for patients on LAI antipsychotics transitioning from hospital to home: A work system approach. Res. Soc. Adm. Pharm. 2017, 13, 1004–1013. [Google Scholar] [CrossRef]
- Shaw, H.; Mackie, C.A.; Sharkie, I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int. J. Pharm. Pract. 2000, 8, 144–153. [Google Scholar] [CrossRef]
- Attfield, J.; Brown, S.; Carter, T.; Callaghan, P. A retrospective case comparison study of the relationship between an Integrated Care Pathway for people diagnosed with schizophrenia in acute mental health care and service users’ length of stay, readmission rates and follow-up within 7 days of discharge. J. Psychiatr. Ment. Health Nurs. 2017, 24, 348–357. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- calculator.net. Sample Size Calculator. 2024. Available online: https://www.calculator.net/sample-size-calculator.html?type=1&cl=95&ci=3&pp=50&ps=4756408&x=Calculate (accessed on 25 March 2025).
- Williams, N. The GAD-7 questionnaire. Occup. Med. 2014, 64, 224. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Mao, W.; Adu, M.; Eboreime, E.; Shalaby, R.; Nkire, N.; Agyapong, B.; Pazderka, H.; Obuobi-Donkor, G.; Owusu, E.; Oluwasina, F.; et al. Post-traumatic stress disorder, major depressive disorder, and wildfires: A fifth-year postdisaster evaluation among residents of Fort McMurray. Int. J. Environ. Res. Public Health 2022, 19, 9759. [Google Scholar] [CrossRef]
- Beard, C.; Hsu, K.; Rifkin, L.; Busch, A.; Björgvinsson, T. Validation of the PHQ-9 in a psychiatric sample. J. Affect. Disord. 2016, 193, 267–273. [Google Scholar] [CrossRef]
- Lequerica, A.H.; Watson, E.; Dijkers, M.P.; Goldin, Y.; Hoffman, J.M.; Niemeier, J.P.; Silva, M.A.; Rabinowitz, A.; Chiaravalloti, N.D. The utility of the Patient Health Questionnaire (PHQ-9) sleep disturbance item as a screener for insomnia in individuals with moderate to severe traumatic brain injury. J. Head Trauma Rehabil. 2022, 37, E383–E389. [Google Scholar] [CrossRef]
- Morin, C.M. Insomnia: Psychological Assessment and Management; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Simon, G.E.; Rutter, C.M.; Peterson, D.; Oliver, M.; Whiteside, U.; Operskalski, B.; Ludman, E.J. Do PHQ depression questionnaires completed during outpatient visits predict subsequent suicide attempt or suicide death? Psychiatr. Serv. 2013, 64, 1195. [Google Scholar] [CrossRef]
- MacGregor, K.L.; Funderburk, J.S.; Pigeon, W.; Maisto, S.A. Evaluation of the PHQ-9 Item 3 as a screen for sleep disturbance in primary care. J. Gen. Intern. Med. 2012, 27, 339–344. [Google Scholar] [CrossRef]
- Louzon, S.A.; Bossarte, R.; McCarthy, J.F.; Katz, I.R. Does suicidal ideation as measured by the PHQ-9 predict suicide among VA patients? Psychiatr. Serv. 2016, 67, 517–522. [Google Scholar] [CrossRef]
- Bauer, A.M.; Chan, Y.-F.; Huang, H.; Vannoy, S.; Unützer, J. Characteristics, management, and depression outcomes of primary care patients who endorse thoughts of death or suicide on the PHQ-9. J. Gen. Intern. Med. 2013, 28, 363–369. [Google Scholar] [CrossRef]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef]
- De Wit, M.; Pouwer, F.; Gemke, R.J.; Delemarre-Van De Waal, H.A.; Snoek, F.J. Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diabetes Care 2007, 30, 2003–2006. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Mac; Version 25.0.; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Chung, D.T.; Ryan, C.J.; Hadzi-Pavlovic, D.; Singh, S.P.; Stanton, C.; Large, M.M. Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry 2017, 74, 694–702. [Google Scholar] [CrossRef]
- Walter, F.; Carr, M.J.; Mok, P.L.; Antonsen, S.; Pedersen, C.B.; Appleby, L.; Fazel, S.; Shaw, J.; Webb, R.T. Multiple adverse outcomes following first discharge from inpatient psychiatric care: A national cohort study. Lancet Psychiatry 2019, 6, 582–589. [Google Scholar] [CrossRef]
- Olfson, M.; Marcus, S.C.; Doshi, J.A. Continuity of care after inpatient discharge of patients with schizophrenia in the Medicaid program: A retrospective longitudinal cohort analysis. J. Clin. Psychiatry 2010, 71, 3717. [Google Scholar] [CrossRef]
- Agyapong, V.I.; Mrklas, K.; Juhás, M.; Omeje, J.; Ohinmaa, A.; Dursun, S.M.; Greenshaw, A.J. Cross-sectional survey evaluating Text4Mood: Mobile health program to reduce psychological treatment gap in mental healthcare in Alberta through daily supportive text messages. BMC Psychiatry 2016, 16, 378. [Google Scholar] [CrossRef]
- Tyler, N.; Wright, N.; Waring, J. Interventions to improve discharge from acute adult mental health inpatient care to the community: Systematic review and narrative synthesis. BMC Health Serv. Res. 2019, 19, 883. [Google Scholar] [CrossRef]
- Meng, N.; Liu, R.; Wong, M.; Liao, J.; Feng, C.; Li, X. The association between patient-reported readiness for hospital discharge and outcomes in patients diagnosed with anxiety disorders: A prospective and observational study. J. Psychiatr. Ment. Health Nurs. 2020, 27, 380–392. [Google Scholar] [CrossRef]
- Newnham, E.A.; Hooke, G.R.; Page, A.C. Progress monitoring and feedback in psychiatric care reduces depressive symptoms. J. Affect. Disord. 2010, 127, 139–146. [Google Scholar] [CrossRef]
- Puschner, B.; Steffen, S.; Völker, K.; Spitzer, C.; Gaebel, W.; Janssen, B.; Klein, H.E.; Spiessl, H.; Steinert, T.; Grempler, J.; et al. Needs-oriented discharge planning for high utilisers of psychiatric services: Multicentre randomised controlled trial. Epidemiol. Psychiatr. Sci. 2011, 20, 181–192. [Google Scholar] [CrossRef]
- Balaban, R.B.; Weissman, J.S.; Samuel, P.A.; Woolhandler, S. Redefining and redesigning hospital discharge to enhance patient care: A randomized controlled study. J. Gen. Intern. Med. 2008, 23, 1228–1233. [Google Scholar] [CrossRef]
- Marissa, L. Evidence-Based Best Practice for Discharge Planning: A Policy Review. 2022. Available online: https://soar.usa.edu/scholprojects/79/ (accessed on 25 March 2025).
- Kuwabara, A.; Su, S.; Krauss, J. Utilizing digital health technologies for patient education in lifestyle medicine. Am. J. Lifestyle Med. 2020, 14, 137–142. [Google Scholar] [CrossRef]
- Albarqi, M.N. Exploring the effectiveness of technology-assisted interventions for promoting independence in elderly patients: A systematic review. Healthcare 2024, 12, 2105. [Google Scholar] [CrossRef]
- Moggia, D.; Lutz, W.; Brakemeier, E.L.; Bickman, L. Treatment Personalization and Precision Mental Health Care: Where are we and where do we want to go? Adm. Policy Ment. Health Ment. Health Serv. Res. 2024, 51, 611–616. [Google Scholar] [CrossRef]
- Isaacs, A.N.; Mitchell, E.K.L. Mental health integrated care models in primary care and factors that contribute to their effective implementation: A scoping review. Int. J. Ment. Health Syst. 2024, 18, 5. [Google Scholar] [CrossRef]
- Ojo, S.; Okoye, T.O.; Olaniyi, S.A.; Ofochukwu, V.C.; Obi, M.O.; Nwokolo, A.S.; Okeke-Moffatt Chinwe Iyun Oluwatosin, B.; Idemudia Etinosa, A.; Obodo Okiemute, R. Ensuring continuity of care: Effective strategies for the post-hospitalization transition of psychiatric patients in a family medicine outpatient clinic. Cureus 2024, 16, e52263. [Google Scholar] [CrossRef]
| Variables | Treatment Groups | |||
|---|---|---|---|---|
| TAU (n = 439) n (%) = 40.0% | SMS (n = 541) n (%) = 49.3% | SMS+PS (n = 118) n (%) = 10.7% | Total (n = 1098) | |
| Age 18–25 y 26–40 y >40 y | 116 (26.4) 168 (38.3) 155 (35.3) | 226 (41.8) 180 (33.3) 135 (25.0) | 59 (50.0) 28 (23.7) 31 (26.3) | 401 (36.5) 376 (34.2) 321 (29.2) |
| Gender Male Female Other Gender | 201 (45.8) 225 (51.3) 13 (3.0) | 227 (42.0) 301 (55.6) 13 (2.4) | 40 (33.9) 72 (61.0) 6 (5.1) | 468 (42.6) 598 (54.5) 32 (2.9) |
| Ethnicity Caucasian Indigenous Black people Asian Mixed/Other | 281 (64.0) 44 (10.0) 44 (10.0) 45 (10.3) 25 (5.7) | 323 (59.7) 48 (8.9) 63 (11.6) 66 (12.2) 41 (7.6) | 71(60.2) 10 (8.5) 13 (11.0) 14 (11.9) 10 (8.5) | 675 (61.5) 102 (9.3) 120 (10.9) 125 (11.4) 76 (6.9) |
| Education Level Less than High School High School Diploma Post-secondary Education Prefer not to say | 22 (5.0) 211 (48.1) 197 (44.9) 9 (2.1) | 15 (2.8) 286 (52.9) 221 (40.9) 19 (3.5) | 4 (3.4) 68 (57.6) 40 (33.9) 6 (5.1) | 41 (3.7) 565 (51.5) 458 (41.7) 34 (3.1) |
| Relationship Status Married/Partnered/Common-Law Single Separated or Divorced Widowed Prefer not to say | 103 (29.6) 256 (58.3) 39 (8.9) 6 (1.4) 8 (1.8) | 160 (29.6) 323 (59.7) 39 (7.2) 3 (0.6) 16 (3.0) | 31 (26.3) 68 (57.6) 8 (6.8) 3 (2.5) 8 (6.8) | 321 (29.2) 647 (58.9) 86 (7.8) 12 (1.1) 32 (2.9) |
| Employment status Employed Unemployed Student Retired Other | 139 (31.7) 236 (53.8) 21 (4.8) 34 (7.7) 9 (2.1) | 156 (28.8) 283 (52.3) 56 (10.4) 26 (4.8) 20 (3.7) | 31 (26.3) 62 (52.5) 12 (10.2) 6 (5.1) 7 (5.9) | 326 (29.7) 585 (52.9) 89 (8.1) 68 (6.0) 36 (3.3) |
| Housing Status Own Home Rented Accommodation Live with Family or Friend Couchsurfing/Shelter/Street/Other | 105 (23.9) 148 (33.7) 159 (36.2) 27 (6.2) | 98 (18.1) 169 (31.3) 238 (44.1) 35 (6.5) | 15 (12.7) 36 (30.5) 61 (51.7) 6 (5.1) | 218 (19.9) 355 (32.2) 458 (41.8) 68 (6.2) |
| Primary Mental Health Diagnosis Depression Bipolar Disorder Anxiety Schizophrenia Personality Disorder Substance Use Disorder Other | 129 (29.4) 74 (16.9) 55 (12.5) 71 (16.2) 28 (6.4) 10 (2.3) 72 (16.4) | 140 (25.9) 126 (23.3) 65 (12.0) 88 (16.3) 53 (9.8) 5 (0.9) 63(11.7) | 21 (17.8) 23 (19.5) 21 (17.8) 19 (16.1) 24 (20.3) 0 (0.0) 10 (8.5) | 290 (26.4) 223 (20.3) 141 (12.9) 178 (16.2) 105 (9.6) 15 (1.4) 145 (13.2) |
| Measures | Descriptives | ANCOVA Parameters | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) | 6-Weeks Mean (SE) | 3-Months Mean (SE) | 6-Months Mean (SE) | ||||||||||||||||||
| TAU | SMS | SMS+PS | TAU | SMS | SMS+PS | F Value (df) | p-Value | Partial eta | TAU | SMS | SMS+PS | F Value (df) | p-Value | Partial eta | TAU | SMS | SMS+PS | F Value (df) | p-Value | Partial eta | |
| GAD-7 | 8.78 (5.76) | 8.32 (5.71) | 7.77 (4.67) | 9.05 (0.68) | 8.65 (0.66) | 8.54 (1.16) | 0.12 | 0.89 | 0.00 | 10.09 (0.76) | 9.17 (1.19) | 9.58 (1.53) | 0.23 | 0.80 | 0.00 | 8.24 (0.88) | 7.58 (0.74) | 9.83 (1.58) | 2.78 | 0.01 * | 0.10 |
| PHQ-9 | 11.01 (6.56) | 11.39 (6.80) | 11.26 (5.27) | 12.51 (0.77) | 11.07 (0.75) | 11.61 (1.24) | 0.91 | 0.40 | 0.01 | 12.84 (0.96) | 11.75 (1.22) | 11.97 (1.94) | 0.28 | 0.76 | 0.00 | 11.42 (1.11) | 11.08 (0.95) | 11.64 (1.73) | 2.50 | 0.03 * | 0.09 |
| WHO-5 | 51.68 (23.38) | 52.02 (23.43) | 47.80 (21.33) | 46.88 (2.50) | 49.48 (2.40) | 44.78 (4.02) | 4.24 | 0.00 | 0.10 | 48.24 (3.00) | 47.24 (3.82) | 42.07 (6.12) | 1.89 | 0.09 | 0.06 | 47.95 (3.46) | 50.31 (2.95) | 48.78 (5.39) | 0.14 | 0.87 | 0.00 |
| Suicidal Ideation | 0.76 (0.96) | 0.79 (0.99) | 0.75 (0.81) | 0.93 (0.11) | 0.74 (0.11) | 0.65 (0.18) | 1.15 | 0.32 | 0.01 | 1.11 (0.31) | 1.00 (0.40) | 0.75 (0.63) | 0.14 | 0.87 | 0.00 | 0.79 (0.14) | 0.82 (0.12) | 1.25 (0.22) | 2.00 | 0.07 | 0.07 |
| Sleep Issues | 1.44 (1.06) | 1.48 (1.04) | 1.49 (0.86) | 1.55 (0.13) | 1.47 (0.13) | 1.61 (0.21) | 0.18 | 0.84 | 0.00 | 1.80 (0.76) | 2.09 (0.96) | 1.52 (1.53) | 0.06 | 0.094 | 0.00 | 1.66 (0.21) | 1.61 (0.18) | 1.66 (0.33) | 0.72 | 0.63 | 0.03 |
| Measures | Study Groups | Paired Groups | Mean Difference | S.E | p-Value | 95% Confidence Interval for Difference | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| GAD-7 | TAU | SMS | 0.67 | 1.51 | 0.56 | −1.61 | 2.94 |
| PS | −1.59 | 1.81 | 0.38 | −5.18 | 2.00 | ||
| SMS | TAU | −0.67 | 1.51 | 0.56 | −2.94 | 1.61 | |
| PS | −2.26 | 1.75 | 0.20 | −5.71 | 1.20 | ||
| PS | TAU | 1.59 | 1.81 | 0.38 | −2.00 | 5.18 | |
| SMS | 2.26 | 1.75 | 0.20 | −1.20 | 5.71 | ||
| PHQ-9 | TAU | SMS | 0.35 | 1.46 | 0.81 | −4.27 | 3.84 |
| PS | −0.21 | 2.05 | 0.92 | −4.27 | 3.84 | ||
| SMS | TAU | −0.35 | 2.46 | 0.81 | −3.23 | 2.53 | |
| PS | −0.56 | 1.97 | 0.78 | −4.44 | 3.33 | ||
| PS | TAU | 0.21 | 2.05 | 0.92 | −3.84 | 4.27 | |
| SMS | 0.56 | 1.97 | 0.78 | −3.33 | 4.44 | ||
| WHO-5 | TAU | SMS | −2.33 | 4.55 | 0.61 | −11.31 | 6.65 |
| PS | −0.80 | 6.41 | 0.90 | −13.46 | 11.86 | ||
| SMS | TAU | 2.33 | 4.55 | 0.61 | −6.65 | 11.31 | |
| PS | 1.53 | 6.14 | 0.80 | −10.60 | 13.65 | ||
| PS | TAU | 0.80 | 6.41 | 0.90 | −11.86 | 13.46 | |
| SMS | −1.53 | 6.14 | 0.80 | −13.65 | 10.60 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mao, W.; Shalaby, R.; Owusu, E.; Elgendy, H.E.; Agyapong, B.; Silverstone, P.H.; Li, X.-M.; Greenshaw, A.J.; Eboreime, E.; Vuong, W.; et al. Supportive Text Messaging and Peer Support for Patients in the 6 Months Following Discharge from a Psychiatric Admission: Mental Health Outcomes from a Cluster-Randomized Controlled Trial. J. Clin. Med. 2025, 14, 8262. https://doi.org/10.3390/jcm14238262
Mao W, Shalaby R, Owusu E, Elgendy HE, Agyapong B, Silverstone PH, Li X-M, Greenshaw AJ, Eboreime E, Vuong W, et al. Supportive Text Messaging and Peer Support for Patients in the 6 Months Following Discharge from a Psychiatric Admission: Mental Health Outcomes from a Cluster-Randomized Controlled Trial. Journal of Clinical Medicine. 2025; 14(23):8262. https://doi.org/10.3390/jcm14238262
Chicago/Turabian StyleMao, Wanying, Reham Shalaby, Ernest Owusu, Hossam Eldin Elgendy, Belinda Agyapong, Peter H. Silverstone, Xin-Min Li, Andrew J. Greenshaw, Ejemai Eboreime, Wesley Vuong, and et al. 2025. "Supportive Text Messaging and Peer Support for Patients in the 6 Months Following Discharge from a Psychiatric Admission: Mental Health Outcomes from a Cluster-Randomized Controlled Trial" Journal of Clinical Medicine 14, no. 23: 8262. https://doi.org/10.3390/jcm14238262
APA StyleMao, W., Shalaby, R., Owusu, E., Elgendy, H. E., Agyapong, B., Silverstone, P. H., Li, X.-M., Greenshaw, A. J., Eboreime, E., Vuong, W., Ohinmaa, A., & Agyapong, V. I. O. (2025). Supportive Text Messaging and Peer Support for Patients in the 6 Months Following Discharge from a Psychiatric Admission: Mental Health Outcomes from a Cluster-Randomized Controlled Trial. Journal of Clinical Medicine, 14(23), 8262. https://doi.org/10.3390/jcm14238262











