Anemia and Iron Deficiency in Cardiac Surgery Patients: Prevalence, Implications, and Therapeutic Considerations
Abstract
1. Introduction
2. Search Strategies
3. Preoperative Anemia in Cardiac Surgery Patients
3.1. Definition of Anemia
3.2. Definition of Iron Deficiency
3.3. Common Types of Anemia
3.4. Iron Deficiency Anemia
3.5. Anemia of Chronic Disease
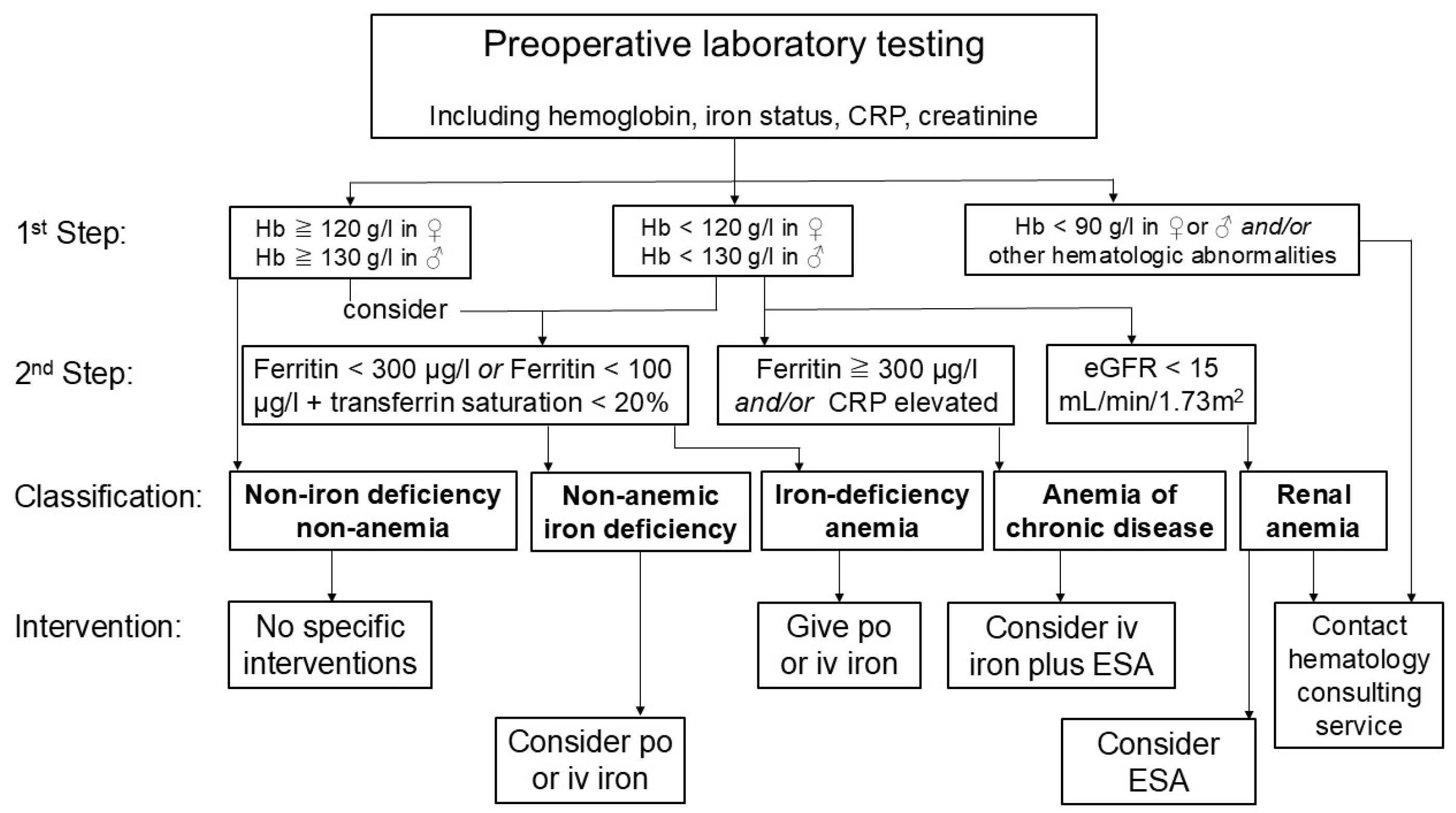
3.6. Laboratory Testing in Anemia
3.7. Specific Consideration Before Cardiac Surgery
4. Impact of Anemia on Outcome After Cardiac Surgery
4.1. Association of Preoperative Anemia and Adverse Outcomes
4.2. Non-Anemic Iron Deficiency and Outcome
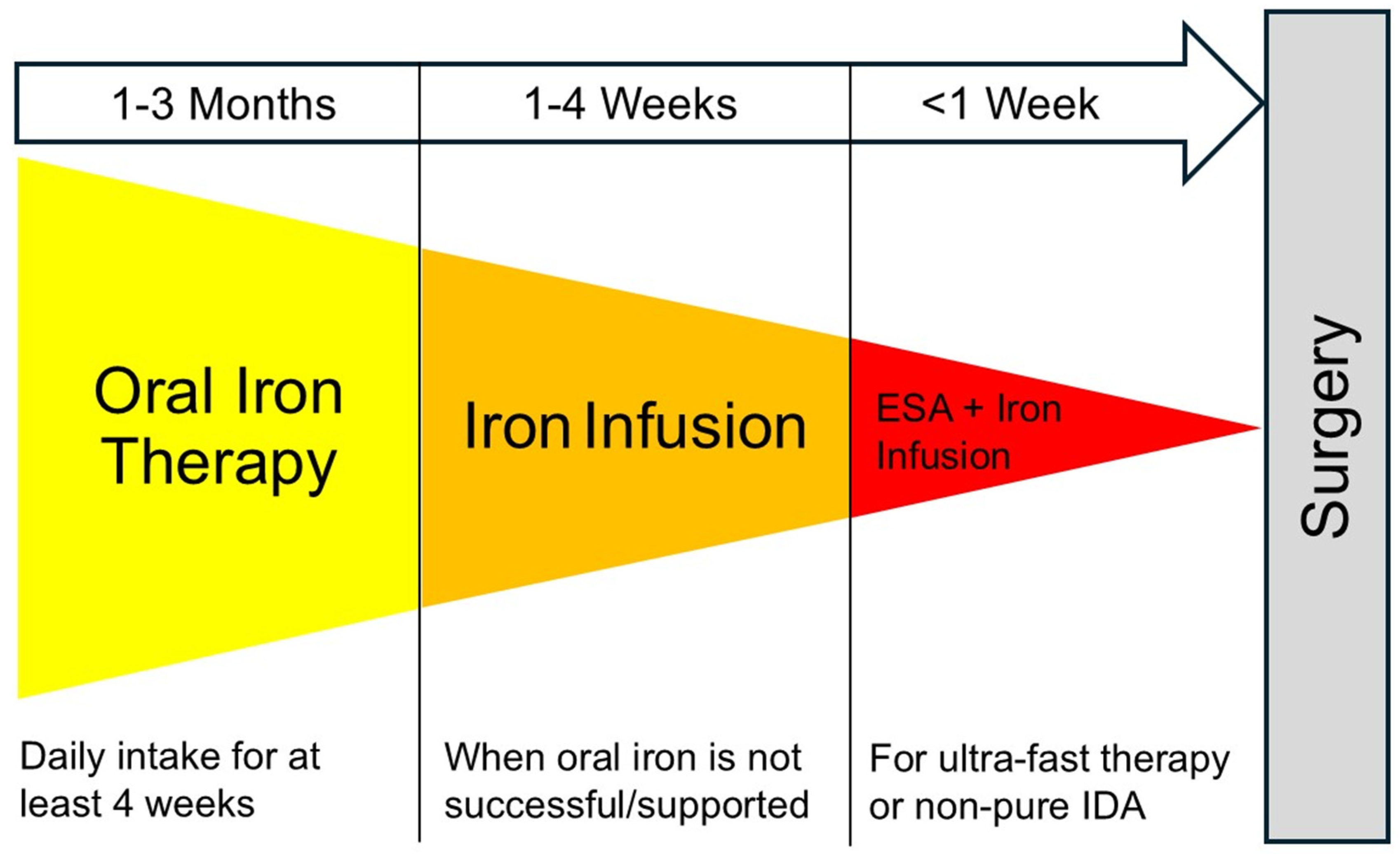
5. Intervention in Anemic and Iron-Deficient Patients Before Cardiac Surgery
5.1. Evidence for Oral Iron Substitution
5.2. Evidence for Administration of Intravenous Iron
5.3. Evidence of Combined Therapy with ESA
5.4. Evidence for Iron Supplementation in Non-Anemic Iron Deficiency
5.5. Evidence for Postoperative Iron Supplementation
5.6. Strategies for Non-Elective Cardiac Surgery
6. Cost-Effectiveness of Preoperative Interventions to Treat Anemia
7. Conclusions and Future Direction
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kassebaum, N.J.; Jasrasaria, R.; Naghavi, M.; Wulf, S.K.; Johns, N.; Lozano, R.; Regan, M.; Weatherall, D.; Chou, D.P.; Eisele, T.P.; et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 2014, 123, 615–624. [Google Scholar] [CrossRef]
- Gaskell, H.; Derry, S.; Andrew Moore, R.; McQuay, H.J. Prevalence of anaemia in older persons: Systematic review. BMC Geriatr. 2008, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Karkouti, K.; Wijeysundera, D.N.; Beattie, W.S.; Reducing Bleeding in Cardiac Surgery. Risk associated with preoperative anemia in cardiac surgery: A multicenter cohort study. Circulation 2008, 117, 478–484. [Google Scholar] [CrossRef]
- Klein, A.A.; Collier, T.J.; Brar, M.S.; Evans, C.; Hallward, G.; Fletcher, S.N.; Richards, T.; Association of Cardiothoracic Anaesthetists (ACTA). The incidence and importance of anaemia in patients undergoing cardiac surgery in the UK—The first Association of Cardiothoracic Anaesthetists national audit. Anaesthesia 2016, 71, 627–635. [Google Scholar] [CrossRef]
- Bolliger, D.; Mauermann, E.; Buser, A. Preoperative anaemia in cardiac surgery: Preoperative assessment, treatment and outcome. Br. J. Anaesth. 2022, 128, 599–602. [Google Scholar] [CrossRef]
- Capdevila, X.; Lasocki, S.; Duchalais, A.; Rigal, J.C.; Mertl, P.; Ghewy, P.; Farizon, F.; Lanz, T.; Buckert, A.; Belarbia, S.; et al. Perioperative Iron Deficiency in Patients Scheduled for Major Elective Surgeries: A French Prospective Multicenter Cross-Sectional Study. Anesth. Analg. 2023, 137, 322–331. [Google Scholar] [CrossRef]
- Peri, V.; Devlin, P.; Perry, L.; Richards, T.; Miles, L.F. Associations Between Nonanemic Iron Deficiency and Postoperative Outcomes in Cardiac Surgery: A Systematic Review and Meta-Analysis. Anesth. Analg. 2024, 139, 47–57. [Google Scholar] [CrossRef]
- Horwood, C.G.A.; Patel, N.D.; Walker, J.D.; Evans, C.R. Nonanemic Iron Deficiency in Cardiac Surgery: A Retrospective Observational Study. J. Cardiothorac. Vasc. Anesth. 2024, 38, 1899–1906. [Google Scholar] [CrossRef] [PubMed]
- Bolliger, D.; Frei, I.; Tanaka, K. Transfusion, Bleeding, or Coagulopathy: What Matters Most in Patients After Cardiac Surgery? J. Cardiothorac. Vasc. Anesth. 2025, 39, 1615–1618. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.; Hart, D.; Ruggiero, A.; Dowling, O.; Ausubel, G.; Preminger, J.; Vitiello, C.; Shore-Lesserson, L. The Relationship Between Transfusion in Cardiac Surgery Patients and Adverse Outcomes. J. Cardiothorac. Vasc. Anesth. 2024, 38, 1492–1498. [Google Scholar] [CrossRef]
- Bolliger, D.; Buser, A.; Tanaka, K.A. Outcomes, cost-effectiveness, and ethics in patient blood management. Curr. Opin. Anaesthesiol. 2025, 38, 151–156. [Google Scholar] [CrossRef]
- Bolliger, D.; Erb, J.M.; Buser, A. Controversies in the Clinical Practice of Patient Blood Management. J. Cardiothorac. Vasc. Anesth. 2021, 35, 1933–1941. [Google Scholar] [CrossRef] [PubMed]
- Casselman, F.P.A.; Lance, M.D.; Ahmed, A.; Ascari, A.; Blanco-Morillo, J.; Bolliger, D.; Eid, M.; Erdoes, G.; Haumann, R.G.; Jeppsson, A.; et al. 2024 EACTS/EACTAIC Guidelines on Patient Blood Management in Adult Cardiac Surgery in Collaboration With EBCP. J. Cardiothorac. Vasc. Anesth. 2025, 39, 1964–2018. [Google Scholar] [CrossRef]
- Charbonneau, H.; Savy, S.; Savy, N.; Pasquie, M.; Mayeur, N.; Group, C.-P.S.; Angles, O.; Balech, V.; Berthelot, A.L.; Croute-Bayle, M.; et al. Comprehensive perioperative blood management in patients undergoing elective bypass cardiac surgery: Benefit effect of health care education and systematic correction of iron deficiency and anemia on red blood cell transfusion. J. Clin. Anesth. 2024, 98, 111560. [Google Scholar] [CrossRef]
- Kloeser, R.; Buser, A.; Bolliger, D. Treatment Strategies in Anemic Patients Before Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2023, 37, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.M.; Van Remoortel, H.; Meybohm, P.; Aranko, K.; Aubron, C.; Burger, R.; Carson, J.L.; Cichutek, K.; De Buck, E.; Devine, D.; et al. Patient Blood Management: Recommendations From the 2018 Frankfurt Consensus Conference. JAMA 2019, 321, 983–997. [Google Scholar] [CrossRef] [PubMed]
- Pasricha, S.R.; Rogers, L.; Branca, F.; Garcia-Casal, M.N. Measuring haemoglobin concentration to define anaemia: WHO guidelines. Lancet 2024, 403, 1963–1966. [Google Scholar] [CrossRef]
- Bolliger, D.; Gebhard, C.E. Unravelling the Impact of Gender Disparities in Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2024, 38, 1084–1087. [Google Scholar] [CrossRef]
- Cappellini, M.D.; Motta, I. Anemia in Clinical Practice-Definition and Classification: Does Hemoglobin Change with Aging? Semin. Hematol. 2015, 52, 261–269. [Google Scholar] [CrossRef]
- Braat, S.; Fielding, K.; Han, J.; Jackson, V.E.; Zaloumis, S.; Xu, J.X.H.; Moir-Meyer, G.; Blaauwendraad, S.M.; Jaddoe, V.W.V.; Gaillard, R.; et al. Statistical haemoglobin thresholds to define anaemia across the lifecycle. medRxiv 2023. [Google Scholar] [CrossRef]
- Munoz, M.; Acheson, A.G.; Auerbach, M.; Besser, M.; Habler, O.; Kehlet, H.; Liumbruno, G.M.; Lasocki, S.; Meybohm, P.; Rao Baikady, R.; et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2017, 72, 233–247. [Google Scholar] [CrossRef]
- Tanaka, K.A.; Alejo, D.; Ghoreishi, M.; Salenger, R.; Fonner, C.; Ad, N.; Whitman, G.; Taylor, B.S.; Mazzeffi, M.A. Impact of Preoperative Hematocrit, Body Mass Index, and Red Cell Mass on Allogeneic Blood Product Usage in Adult Cardiac Surgical Patients: Report from a Statewide Quality Initiative. J. Cardiothorac. Vasc. Anesth. 2023, 37, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Li, M.M.; Miles, S.; Callum, J.; Lin, Y.; Karkouti, K.; Bartoszko, J. Postoperative anemia in cardiac surgery patients: A narrative review. Can. J. Anaesth. 2024, 71, 408–421. [Google Scholar] [CrossRef]
- Anker, S.D.; Comin Colet, J.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Luscher, T.F.; Bart, B.; Banasiak, W.; Niegowska, J.; et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N. Engl. J. Med. 2009, 361, 2436–2448. [Google Scholar] [CrossRef]
- Miles, L.F.; Pac Soo, V.; Braat, S.; Bade-Boon, J.; Heritier, S.; Klein, A.A.; Myles, P.S.; Richards, T.; Symons, J.; Burbury, K.L.; et al. Associations between non-anaemic iron deficiency and outcomes following elective cardiac surgery (IDOCS): A prospective cohort study. Lancet Haematol. 2022, 9, e514–e522. [Google Scholar] [CrossRef] [PubMed]
- Hands, K.; Daru, J.; Evans, C.; Kotze, A.; Lewis, C.; Narayan, S.; Richards, T.; Taylor, C.; Timmins, S.; Wilson, A.; et al. Identification and management of preoperative anaemia in adults: A British Society for Haematology Guideline update. Br. J. Haematol. 2024, 205, 88–99. [Google Scholar] [CrossRef]
- Munoz, M.; Gomez-Ramirez, S.; Kozek-Langeneker, S. Pre-operative haematological assessment in patients scheduled for major surgery. Anaesthesia 2016, 71, 19–28. [Google Scholar] [CrossRef]
- Liu, H.M.; Tang, X.S.; Yu, H.; Yu, H. The efficacy of intravenous iron for treatment of anemia before cardiac surgery: An updated systematic review and meta-analysis with trial sequential analysis. J. Cardiothorac. Surg. 2023, 18, 16. [Google Scholar] [CrossRef]
- Ng, O.; Keeler, B.D.; Mishra, A.; Simpson, J.A.; Neal, K.; Al-Hassi, H.O.; Brookes, M.J.; Acheson, A.G. Iron therapy for preoperative anaemia. Cochrane Database Syst. Rev. 2019, 12, CD011588. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, G. Role of hepcidin in the pathophysiology and diagnosis of anemia. Blood Res. 2013, 48, 10–15. [Google Scholar] [CrossRef]
- Weiss, G.; Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef]
- Dai, L.; Mick, S.L.; McCrae, K.R.; Houghtaling, P.L.; Sabik, J.F., III; Blackstone, E.H.; Koch, C.G. Preoperative Anemia in Cardiac Operation: Does Hemoglobin Tell the Whole Story? Ann. Thorac. Surg. 2018, 105, 100–107. [Google Scholar] [CrossRef]
- Mentz, R.J.; Garg, J.; Rockhold, F.W.; Butler, J.; De Pasquale, C.G.; Ezekowitz, J.A.; Lewis, G.D.; O’Meara, E.; Ponikowski, P.; Troughton, R.W.; et al. Ferric Carboxymaltose in Heart Failure with Iron Deficiency. N. Engl. J. Med. 2023, 389, 975–986. [Google Scholar] [CrossRef] [PubMed]
- Panjeta, M.; Tahirovic, I.; Karamehic, J.; Sofic, E.; Ridic, O.; Coric, J. The Relation of Erythropoietin Towards Hemoglobin and Hematocrit in Varying Degrees of Renal Insufficiency. Mater. Sociomed. 2015, 27, 144–148. [Google Scholar] [CrossRef]
- Goodnough, L.T.; Maniatis, A.; Earnshaw, P.; Benoni, G.; Beris, P.; Bisbe, E.; Fergusson, D.A.; Gombotz, H.; Habler, O.; Monk, T.G.; et al. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br. J. Anaesth. 2011, 106, 13–22. [Google Scholar] [CrossRef]
- Liu, C.; Han, J.; Fu, R.; Li, T.; Margonis, G.A.; Wang, J.J.; Ma, K.; Wang, W.; Lin, C. Timing of intravenous iron for treatment of anaemia in surgical patients: A systematic review and network meta-analysis. EClinicalMedicine 2025, 86, 103361. [Google Scholar] [CrossRef]
- Hazen, Y.; Noordzij, P.G.; Gerritse, B.M.; Scohy, T.V.; Houterman, S.; Bramer, S.; Berendsen, R.R.; Bouwman, R.A.; Eberl, S.; Haenen, J.S.E.; et al. Preoperative anaemia and outcome after elective cardiac surgery: A Dutch national registry analysis. Br. J. Anaesth. 2022, 128, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Kulier, A.; Levin, J.; Moser, R.; Rumpold-Seitlinger, G.; Tudor, I.C.; Snyder-Ramos, S.A.; Moehnle, P.; Mangano, D.T.; Investigators of the Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation. Impact of preoperative anemia on outcome in patients undergoing coronary artery bypass graft surgery. Circulation 2007, 116, 471–479. [Google Scholar] [CrossRef]
- Lau, M.; Low, C.J.W.; Ling, R.R.; Liu, N.S.H.; Tan, C.S.; Ti, L.K.; Kofidis, T.; MacLaren, G.; Ramanathan, K. Preoperative anemia and anemia treatment in cardiac surgery: A systematic review and meta-analysis. Can. J. Anaesth. 2024, 71, 127–142. [Google Scholar] [CrossRef] [PubMed]
- Kattou, F.; Montandrau, O.; Rekik, M.; Delentdecker, P.; Brini, K.; Zannis, K.; Beaussier, M. Critical Preoperative Hemoglobin Value to Predict Anemia-Related Complications After Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2022, 36, 1901–1907. [Google Scholar] [CrossRef]
- Ripoll, J.G.; Smith, M.M.; Hanson, A.C.; Schulte, P.J.; Portner, E.R.; Kor, D.J.; Warner, M.A. Sex-Specific Associations Between Preoperative Anemia and Postoperative Clinical Outcomes in Patients Undergoing Cardiac Surgery. Anesth. Analg. 2021, 132, 1101–1111. [Google Scholar] [CrossRef] [PubMed]
- Blaudszun, G.; Munting, K.E.; Butchart, A.; Gerrard, C.; Klein, A.A. The association between borderline pre-operative anaemia in women and outcomes after cardiac surgery: A cohort study. Anaesthesia 2018, 73, 572–578. [Google Scholar] [CrossRef] [PubMed]
- LaPar, D.J.; Hawkins, R.B.; McMurry, T.L.; Isbell, J.M.; Rich, J.B.; Speir, A.M.; Quader, M.A.; Kron, I.L.; Kern, J.A.; Ailawadi, G.; et al. Preoperative anemia versus blood transfusion: Which is the culprit for worse outcomes in cardiac surgery? J. Thorac. Cardiovasc. Surg. 2018, 156, 66–74.e2. [Google Scholar] [CrossRef] [PubMed]
- Oprea, A.D.; Del Rio, J.M.; Cooter, M.; Green, C.L.; Karhausen, J.A.; Nailer, P.; Guinn, N.R.; Podgoreanu, M.V.; Stafford-Smith, M.; Schroder, J.N.; et al. Pre- and postoperative anemia, acute kidney injury, and mortality after coronary artery bypass grafting surgery: A retrospective observational study. Can. J. Anaesth. 2018, 65, 46–59. [Google Scholar] [CrossRef] [PubMed]
- Tauriainen, T.; Koski-Vahala, J.; Kinnunen, E.M.; Biancari, F. The Effect of Preoperative Anemia on the Outcome After Coronary Surgery. World J. Surg. 2017, 41, 1910–1918. [Google Scholar] [CrossRef]
- Padmanabhan, H.; Aktuerk, D.; Brookes, M.J.; Nevill, A.M.; Ng, A.; Cotton, J.; Luckraz, H. Anemia in cardiac surgery: Next target for mortality and morbidity improvement? Asian Cardiovasc. Thorac. Ann. 2016, 24, 12–17. [Google Scholar] [CrossRef]
- von Heymann, C.; Kaufner, L.; Sander, M.; Spies, C.; Schmidt, K.; Gombotz, H.; Wernecke, K.D.; Balzer, F. Does the severity of preoperative anemia or blood transfusion have a stronger impact on long-term survival after cardiac surgery? J. Thorac. Cardiovasc. Surg. 2016, 152, 1412–1420. [Google Scholar] [CrossRef]
- Greenhouse, D.G.; Schwann, T.A.; Engelman, D.T. Preoperative Anemic Patients Have Poor Outcomes; How Can We Optimize These Patients Prior to Surgery? Semin. Thorac. Cardiovasc. Surg. 2019, 31, 164–165. [Google Scholar] [CrossRef]
- Padmanabhan, H.; Siau, K.; Curtis, J.; Ng, A.; Menon, S.; Luckraz, H.; Brookes, M.J. Preoperative Anemia and Outcomes in Cardiovascular Surgery: Systematic Review and Meta-Analysis. Ann. Thorac. Surg. 2019, 108, 1840–1848. [Google Scholar] [CrossRef]
- Mazer, C.D.; Whitlock, R.P.; Fergusson, D.A.; Hall, J.; Belley-Cote, E.; Connolly, K.; Khanykin, B.; Gregory, A.J.; de Medicis, E.; McGuinness, S.; et al. Restrictive or Liberal Red-Cell Transfusion for Cardiac Surgery. N. Engl. J. Med. 2017, 377, 2133–2144. [Google Scholar] [CrossRef]
- Murphy, G.J.; Pike, K.; Rogers, C.A.; Wordsworth, S.; Stokes, E.A.; Angelini, G.D.; Reeves, B.C.; Investigators, T.I. Liberal or restrictive transfusion after cardiac surgery. N. Engl. J. Med. 2015, 372, 997–1008. [Google Scholar] [CrossRef]
- Carson, J.L.; Brooks, M.M.; Hebert, P.C.; Goodman, S.G.; Bertolet, M.; Glynn, S.A.; Chaitman, B.R.; Simon, T.; Lopes, R.D.; Goldsweig, A.M.; et al. Restrictive or Liberal Transfusion Strategy in Myocardial Infarction and Anemia. N. Engl. J. Med. 2023, 389, 2446–2456. [Google Scholar] [CrossRef]
- Ranucci, M.; Baryshnikova, E.; Castelvecchio, S.; Pelissero, G.; Surgical and Clinical Outcome Research Group. Major bleeding, transfusions, and anemia: The deadly triad of cardiac surgery. Ann. Thorac. Surg. 2013, 96, 478–485. [Google Scholar] [CrossRef]
- Nashef, S.A.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardiothorac. Surg. 2012, 41, 734–744; discussion 44–45. [Google Scholar] [CrossRef] [PubMed]
- Corwin, H.L.; Shander, A.; Speiss, B.; Munoz, M.; Faraoni, D.; Calcaterra, D.; Welsby, I.; Ozawa, S.; Arnofsky, A.; Goldweit, R.S.; et al. Management of Perioperative Iron Deficiency in Cardiac Surgery: A Modified RAND Delphi Study. Ann. Thorac. Surg. 2022, 113, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Miles, L.F.; Kunz, S.A.; Na, L.H.; Braat, S.; Burbury, K.; Story, D.A. Postoperative outcomes following cardiac surgery in non-anaemic iron-replete and iron-deficient patients—An exploratory study. Anaesthesia 2018, 73, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Hazen, Y.; Noordzij, P.G.; Geuzebroek, G.S.C.; Koets, J.; Somers, T.; Gerritse, B.M.; Scohy, T.V.; Vernooij, L.M.; van Gammeren, A.; Thelen, M.H.M.; et al. Abnormal Iron Status and Adverse Outcome After Elective Cardiac Surgery: A Prospective, Observational Multicenter Study. J. Cardiothorac. Vasc. Anesth. 2024, 38, 667–674. [Google Scholar] [CrossRef]
- Gomez-Ramirez, S.; Brilli, E.; Tarantino, G.; Girelli, D.; Munoz, M. Sucrosomial((R)) Iron: An Updated Review of Its Clinical Efficacy for the Treatment of Iron Deficiency. Pharmaceuticals 2023, 16, 847. [Google Scholar] [CrossRef]
- Dignass, A.U.; Gasche, C.; Bettenworth, D.; Birgegard, G.; Danese, S.; Gisbert, J.P.; Gomollon, F.; Iqbal, T.; Katsanos, K.; Koutroubakis, I.; et al. European consensus on the diagnosis and management of iron deficiency and anaemia in inflammatory bowel diseases. J. Crohns Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Schmidt, C.; Allen, S.; Kopyt, N.; Pergola, P. Iron Replacement Therapy with Oral Ferric Maltol: Review of the Evidence and Expert Opinion. J. Clin. Med. 2021, 10, 4448. [Google Scholar] [CrossRef]
- Iolascon, A.; Andolfo, I.; Russo, R.; Sanchez, M.; Busti, F.; Swinkels, D.; Aguilar Martinez, P.; Bou-Fakhredin, R.; Muckenthaler, M.U.; Unal, S.; et al. Recommendations for diagnosis, treatment, and prevention of iron deficiency and iron deficiency anemia. Hemasphere 2024, 8, e108. [Google Scholar] [CrossRef]
- Kaundal, R.; Bhatia, P.; Jain, A.; Jain, A.; Nampoothiri, R.V.; Mishra, K.; Jandial, A.; Goni, D.; Sandal, R.; Jindal, N.; et al. Randomized controlled trial of twice-daily versus alternate-day oral iron therapy in the treatment of iron-deficiency anemia. Ann. Hematol. 2020, 99, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Pierelli, L.; De Rosa, A.; Falco, M.; Papi, E.; Rondinelli, M.B.; Turani, F.; Weltert, L. Preoperative Sucrosomial Iron Supplementation Increases Haemoglobin and Reduces Transfusion Requirements in Elective Heart Surgery Patients: A Prospective Randomized Study. Surg. Technol. Int. 2021, 39, 321–328. [Google Scholar] [CrossRef]
- Weltert, L.P.; De Rosa, A.; Rondinelli, M.B.; Falco, M.; Turani, F.; Pierelli, L. Benefits of pre-operative oral Sucrosomial(R) iron supplementation in cardiac surgery: Influence of patient’s baseline hemoglobin and gender. Blood Transfus. 2023, 21, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Hung, K.C.; Chang, L.C.; Ho, C.N.; Hsu, C.W.; Yu, C.H.; Wu, J.Y.; Lin, C.M.; Chen, I.W. Efficacy of intravenous iron supplementation in reducing transfusion risk following cardiac surgery: An updated meta-analysis of randomised controlled trials. Br. J. Anaesth. 2024, 133, 1137–1149. [Google Scholar] [CrossRef]
- Spahn, D.R.; Schoenrath, F.; Spahn, G.H.; Seifert, B.; Stein, P.; Theusinger, O.M.; Kaserer, A.; Hegemann, I.; Hofmann, A.; Maisano, F.; et al. Effect of ultra-short-term treatment of patients with iron deficiency or anaemia undergoing cardiac surgery: A prospective randomised trial. Lancet 2019, 393, 2201–2212. [Google Scholar] [CrossRef]
- Kong, R.; Hutchinson, N.; Hill, A.; Ingoldby, F.; Skipper, N.; Jones, C.; Bremner, S.; Bruce, C.; Wright, J.; Lewis, M.; et al. Randomised open-label trial comparing intravenous iron and an erythropoiesis-stimulating agent versus oral iron to treat preoperative anaemia in cardiac surgery (INITIATE trial). Br. J. Anaesth. 2022, 128, 796–805. [Google Scholar] [CrossRef]
- Peel, J.K.; Trudeau, J.; Tano, R.; Jadunandan, S.; Callum, J.; Moussa, F.; Lin, Y. Determining Optimal Treatment to Correct Preoperative Anemia and Reduce Perioperative Allogeneic Blood Transfusions in Cardiac Surgery: A Retrospective Cohort Study. J. Cardiothorac. Vasc. Anesth. 2021, 35, 2631–2639. [Google Scholar] [CrossRef]
- Shin, H.J.; Ko, E.; Jun, I.; Kim, H.J.; Lim, C.H. Effects of perioperative erythropoietin administration on acute kidney injury and red blood cell transfusion in patients undergoing cardiac surgery: A systematic review and meta-analysis. Medicine 2022, 101, e28920. [Google Scholar] [CrossRef]
- Hakim, S.M.; Ahmad, A.H.M.; Amer, A.M. Effect of Preoperative Recombinant Human Erythropoietin on the Need for Blood Transfusion and Surgical Outcomes in Adult Patients Undergoing Cardiac Surgery: A Systematic Review and Meta-Analysis with Trial Sequential Analysis. J. Cardiothorac. Vasc. Anesth. 2024, 38, 2402–2411. [Google Scholar] [CrossRef] [PubMed]
- Friedman, T.; Dann, E.J.; Bitton-Worms, K.; Makhoul, M.; Glam, R.; Weis, A.; Tam, D.Y.; Bolotin, G. Intravenous iron administration before cardiac surgery reduces red blood cell transfusion in patients without anaemia. Br. J. Anaesth. 2023, 131, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Toledo, F.V.; De Carli, D.; Meletti, J.F.A.; Togo, H.Y.A.; Gomes, I.P.; Sakashita, R.M.; Montes, L.F.; Tiburcio, R.S.; Miranda, C.A. Preoperative iron supplementation in non-anemic patients undergoing major surgery: A systematic review and meta-analysis. Braz. J. Anesthesiol. 2025, 75, 844618. [Google Scholar] [CrossRef]
- Lim, J.; Joo, J.; MacLean, B.; Richards, T. The use of iron after surgery: A systematic review and meta-analysis. Anaesthesia 2025, 80, 988–996. [Google Scholar] [CrossRef]
- Venturini, E.; Iannuzzo, G.; Di Lorenzo, A.; Cuomo, G.; D’Angelo, A.; Merone, P.; Cudemo, G.; Pacileo, M.; D’Andrea, A.; Vigorito, C.; et al. Short-term treatment of iron deficiency anemia after cardiac surgery. Int. J. Cardiol. Heart Vasc. 2022, 40, 101038. [Google Scholar] [CrossRef]
- Blum, L.V.; Hipp, N.; Neef, V.; Prinzing, A.; Zacharowski, K.; Meybohm, P.; Choorapoikayil, S. Effect of (short-term) intravenous iron supplementation in iron-deficient non-anaemic cardiac surgical patients on perioperative outcome. Perioper. Med. 2025, 14, 107. [Google Scholar] [CrossRef]
- Irving, A.; McQuilten, Z.K. Does patient blood management represent good value for money? Best. Pract. Res. Clin. Anaesthesiol. 2023, 37, 511–518. [Google Scholar] [CrossRef]
- Roman, M.A.; Abbasciano, R.G.; Pathak, S.; Oo, S.; Yusoff, S.; Wozniak, M.; Qureshi, S.; Lai, F.Y.; Kumar, T.; Richards, T.; et al. Patient blood management interventions do not lead to important clinical benefits or cost-effectiveness for major surgery: A network meta-analysis. Br. J. Anaesth. 2021, 126, 149–156. [Google Scholar] [CrossRef]
- Lasocki, S.; Delahaye, D.; Fuks, D.; Savoie, P.H.; Dussart, C.; Hofmann, A.; Paubel, P. Management of perioperative iron deficiency anemia as part of patient blood management in France: A budget impact model-based analysis based on real world data. Transfusion 2023, 63, 1692–1700. [Google Scholar] [CrossRef]
- Meybohm, P.; Straub, N.; Fullenbach, C.; Judd, L.; Kleineruschkamp, A.; Taeuber, I.; Zacharowski, K.; Choorapoikayil, S. Health economics of Patient Blood Management: A cost-benefit analysis based on a meta-analysis. Vox Sang. 2020, 115, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Payan-Pernia, S.; Mendez Arias, E.; Perez Blanco, J.L.; Navarro-Garcia, M.A.; Martinez-Leon, J.B.; Colomina, M.J.; Garcia-Erce, J.A. Sucrosomial iron? Not so fast. Eur. J. Cardiothorac. Surg. 2025, 67, ezaf067. [Google Scholar] [CrossRef] [PubMed]
- Farabi, H.; Tomini, F.; Evans, H.; Murphy, M.F.; Green, L.; Dhiman, P.; Fabiano, G.; Palmer, A.J.R.; von Neree, L.; Stanworth, S.J. Evaluating Economic and Clinical Impacts of Anaemia Management Strategies: A Systematic Review of the Evidence From the UK Perspective. EJHaem 2025, 6, e70124. [Google Scholar] [CrossRef] [PubMed]
- Quarterman, C.; Shaw, M.; Hughes, S.; Wallace, V.; Agarwal, S. Anaemia in cardiac surgery—A retrospective review of a centre’s experience with a pre-operative intravenous iron clinic. Anaesthesia 2021, 76, 629–638. [Google Scholar] [CrossRef] [PubMed]

| Type | Etiology |
|---|---|
| Iron deficiency anemia |
|
| |
| Anemia of chronic disease |
|
| Megaloblastic anemia |
|
| Inherited blood disorders |
|
| Laboratory Test | Iron-Deficiency Anemia | Non-Anemic Iron Deficiency | Anemia of Chronic Disease |
|---|---|---|---|
| Hemoglobin | ↓ | normal | ↓ |
| Mean corpuscular volume | ↓ | normal/↓ | ↓/normal |
| Reticulocyte count | ↓ | normal | ↓ |
| Ferritin | ↓ | ↓ | normal/↑ |
| Transferrin | ↑ | ↑ | ↓/normal |
| Transferrin saturation | ↓ | ↓/normal | ↓ |
| Soluble transferrin receptor | ↑ | ↑/normal | normal |
| Reticulocyte hemoglobin content | ↓ | ↓ | ↓/normal |
| Erythropoietin levels | ↑ | ↑/normal | normal/slightly ↑ |
| C-reactive protein | normal | normal | ↑/normal |
| Study | Study Design | Sample Size Total/Anemic (%) | Reported Outcome | Anemic vs. Non-Anemic (% or aHR) | p |
|---|---|---|---|---|---|
| Hazen (2022) [37] | Prospective nation-wide registry; 16 centers; CABG and valves | 35,484/6802 (19) | 30-day mortality Any RBC transfusion Renal failure Cardiac complications Neurological complications Infections | 2.4% vs. 1.0% 49.1% vs. 17.1% 3.5% vs. 1.5% 34.2% vs. 30.4% 1.3% vs. 1.0% 4.5% vs. 3.0% | <0.001 <0.001 <0.001 <0.001 <0.05 <0.001 |
| Kattou (2022) [40] | Retrospective cohort study; 1 center; CABG and valves | 1004/251 (25) | 30-day mortality Any RBC transfusion AKI MI Stroke/TIA Respiratory failure | 5.2% vs. 1.6% 72.5% vs. 30.1% 15.1% vs. 2.6% 16.3% vs. 4.9% 13.1% vs. 6.1% 10.0% vs. 2.9% | 0.005 <0.01 <0.001 <0.001 0.001 <0.001 |
| Ripoll (2021) [41] | Retrospective cohort study; 1 center; CABG and valves | 4117/1234 (30) | In-hospital mortality Any RBC Transfusion AKI MI or stroke or PE | 0.13% vs. 0.03% 80.0% vs. 41.1% 17.7% vs. 7.8% 5.4% vs. 3.4% | 0.300 <0.001 <0.001 0.012 |
| Blaudszun (2018) [42] | Retrospective cohort study; 1 center, only women; CABG and valves | 1388/333 (24) | In-hospital mortality Any RBC transfusions | 2.1% vs. 1.4% 89% vs. 54% | 0.552 <0.001 |
| Dai (2018) [32] | Retrospective cohort study; 1 center; CABG and valves | 10,589/2715 (26) | In-hospital mortality Any RBC transfusion Renal failure Prolonged ventilation | 1.5% vs. 0.4% 66% vs. 26% 5.3% vs. 1.7% 13.3% vs. 6.1% | <0.001 <0.001 <0.001 <0.001 |
| LaPar (2018) [43] | Retrospective quality data analysis; 19 centers; only CABG | 33,411/NA | In-hospital mortality Any RBC transfusion Renal failure | 1.5% vs. 1.1% (predicted probability) 22.8% vs. 62.1% (predicted probability) 2.3% vs. 1.3% (predicted probability) | NA NA NA |
| Oprea (2018) [44] | Retrospective cohort study; 1 center; only CABG | 6130/1197 (20) | Long-term mortality (median 6.8 years) AKI | aHR 1.29 (95% CI: 1.15–1.44) aHR 1.23 (95% CI: 1.13–1.33) | <0.001 <0.001 |
| Tauriainen (2017) [45] | Retrospective cohort study; 1 center; only CABG | 2099/662 (32) | 30-day mortality Any RBC transfusion AKI Stroke ICU LOS (mean ± SD) | 6.2% vs. 2.3% 89.6% vs. 55.3% 30.6% vs. 12.1% 3.8% vs. 1.6% 2.9 ± 3.5 vs. 1.9 ± 2.0 days | <0.001 <0.001 <0.001 0.001 <0.001 |
| Klein (2016) [4] | National audit; 12 centers; CABG and valves | 19,033/5895 (31) | In-hospital mortality Any RBC transfusion ICU LOS (median (IQR)) | 5.6% vs. 2.3% 63.9% vs. 36.6% 2 (1–4) vs. 2 (0–4) | <0.001 <0.001 <0.001 |
| Padmanabhan (2016) [46] | Retrospective matched case–control study; 1 center; CABG and valves | 2340/1170 (50) | In-hospital mortality Any RBC transfusion Renal replacement Surgical site Infections Prolonged airway support | 5.6% vs. 3.5% 58% vs. 38% 13% vs. 8% 9% vs. 7% 15% vs. 12% | 0.02 <0.01 <0.01 0.05 0.05 |
| von Heymann (2016) [47] | Retrospective cohort study; single center; CABG and valves | 4494/1620 (36); of them 1274 with mild and 346 with severe anemia | 3-year mortality In-hospital mortality ICU LOS (median (IQR) | 51.2% (severe) vs. 30.8% (mild) vs. 15.0% 15.0% (severe) vs. 8.6% (mild) vs. 3.7% 4 (3–7) vs. 6 (4–11) vs. 10.5 (4–11) days | <0.001 <0.001 <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frei, I.; Gogniat, A.L.; Buser, A.; Bolliger, D. Anemia and Iron Deficiency in Cardiac Surgery Patients: Prevalence, Implications, and Therapeutic Considerations. J. Clin. Med. 2025, 14, 8261. https://doi.org/10.3390/jcm14228261
Frei I, Gogniat AL, Buser A, Bolliger D. Anemia and Iron Deficiency in Cardiac Surgery Patients: Prevalence, Implications, and Therapeutic Considerations. Journal of Clinical Medicine. 2025; 14(22):8261. https://doi.org/10.3390/jcm14228261
Chicago/Turabian StyleFrei, Isabelle, Annika Léonie Gogniat, Andreas Buser, and Daniel Bolliger. 2025. "Anemia and Iron Deficiency in Cardiac Surgery Patients: Prevalence, Implications, and Therapeutic Considerations" Journal of Clinical Medicine 14, no. 22: 8261. https://doi.org/10.3390/jcm14228261
APA StyleFrei, I., Gogniat, A. L., Buser, A., & Bolliger, D. (2025). Anemia and Iron Deficiency in Cardiac Surgery Patients: Prevalence, Implications, and Therapeutic Considerations. Journal of Clinical Medicine, 14(22), 8261. https://doi.org/10.3390/jcm14228261





