Male Gender and Normal Trochlear Anatomy Are Associated with a Higher Risk of Osteochondral Fracture Following Patellar Dislocation: A Retrospective Review of 261 Skeletally Mature Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Imaging Protocol and Analysis
2.3. Inter-Observer Reliability
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Patient Demographics and Baseline Characteristics
3.2. Osteochondral Fracture Prevalence and Distribution
3.3. Univariate Comparisons
3.4. Logistic Regression Analysis
4. Discussion
- Clinical Implications
- Limitations
- Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sanders, T.L.; Pareek, A.; Hewett, T.E.; Stuart, M.J.; Dahm, D.L.; Krych, A.J. Incidence of first-time lateral patellar dislocation: A 21-year population-based study. Sports Health 2018, 10, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Fithian, D.C.; Paxton, E.W.; Stone, M.L.; Silva, P.; Davis, D.K.; Elias, D.A.; White, L.M. Epidemiology and natural history of acute patellar dislocation. Am. J. Sports Med. 2004, 32, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Nietosvaara, Y.; Aalto, K.; Kallio, P.E. Acute patellar dislocation in children: Incidence and associated osteochondral fractures. J. Pediatr. Orthop. 1994, 14, 513–515. [Google Scholar] [CrossRef] [PubMed]
- Kirsch, M.D.; Fitzgerald, S.W.; Friedman, H.; Rogers, L.F. Transient lateral patellar dislocation: Diagnosis with MR imaging. AJR Am. J. Roentgenol. 1993, 161, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Sallay, P.I.; Poggi, J.; Speer, K.P.; Garrett, W.E. Acute dislocation of the patella: A correlative pathoanatomic study. Am. J. Sports Med. 1996, 24, 52–60. [Google Scholar] [CrossRef] [PubMed]
- Stefancin, J.J.; Parker, R.D. First-time traumatic patellar dislocation: A systematic review. Clin. Orthop. Relat. Res. 2007, 455, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Gesslein, M.; Merkl, C.; Bail, H.J.; Krutsch, V.; Biber, R.; Schuster, P. Refixation of Large Osteochondral Fractures After Patella Dislocation Shows Better Mid- to Long-Term Outcome Compared with Debridement. Cartilage 2021, 13, 966S–973S. [Google Scholar] [CrossRef] [PubMed]
- Vavken, P.; Wimmer, M.D.; Camathias, C.; Quidde, J.; Valderrabano, V.; Pagenstert, G. Treating patella instability in skeletally immature patients. Arthroscopy 2013, 29, 1410–1422. [Google Scholar] [CrossRef] [PubMed]
- Nomura, E.; Inoue, M.; Kobayashi, S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am. J. Sports Med. 2007, 35, 1851–1858. [Google Scholar] [CrossRef] [PubMed]
- Schüttler, K.F.; Struewer, J.; Roessler, P.P.; Gesslein, M.; Rominger, M.B.; Ziring, E.; Efe, T. Patellofemoral osteoarthritis after Insall’s proximal realignment for recurrent patellar dislocation. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2623–2628. [Google Scholar] [CrossRef] [PubMed]
- Dejour, H.; Walch, G.; Nove-Josserand, L.; Guier, C. Factors of patellar instability: An anatomic radiographic study. Knee Surg. Sports Traumatol. Arthrosc. 1994, 2, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Insall, J.; Salvati, E. Patella position in the normal knee joint. Radiology 1971, 101, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Gravesen, K.S.; Kallemose, T.; Blønd, L.; Troelsen, A.; Barfod, K.W. High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24,154 primary dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1204–1209. [Google Scholar] [CrossRef] [PubMed]
- Palmu, S.; Kallio, P.E.; Donell, S.T.; Helenius, I.; Nietosvaara, Y. Acute patellar dislocation in children and adolescents: A randomized clinical trial. J. Bone Jt. Surg. Am. 2008, 90, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Blønd, L.; Askenberger, M.; Stephen, J.; Akmeşe, R.; Balcarek, P.; El Attal, R.; Chouliaras, V.; Ferrua, P.; Monart, J.M.; Pagenstert, G.; et al. Management of first-time patellar dislocation: The ESSKA 2024 formal consensus—Part 1. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1925–1932. [Google Scholar] [CrossRef] [PubMed]
- Balcarek, P.; Blønd, L.; Beaufils, P.; Askenberger, M.; Stephen, J.M.; Akmeşe, R.; El Attal, R.; Chouliaras, V.; Ferrua, P.; Minguell Monart, J.; et al. Management of first-time patellar dislocation: The ESSKA 2024 formal consensus—Part 2. Knee Surg. Sports Traumatol. Arthrosc. 2025. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Hua, Q.; Wen, C.; Qian, W.; Su, J.; Yang, M.; Lei, M. Effect of Patellar Morphology on the Risk of Osteochondral Fracture after Patellar Dislocation: A Cross-sectional Study. Orthop. Surg. 2024, 16, 1089–1100. [Google Scholar] [CrossRef] [PubMed]
- Bram, J.T.; Lijesen, E.; Green, D.W.; Heyworth, B.E.; Veerkamp, M.W.; Chipman, D.E.; Propp, B.E.; Brady, J.M.; Parikh, S.N.; Shubin Stein, B.E.; et al. The Number of Patellar Dislocation Events Is Associated with Increased Chondral Damage of the Trochlea. Am. J. Sports Med. 2024, 52, 2541–2546. [Google Scholar] [CrossRef] [PubMed]
- Parikh, S.N.; Schlechter, J.A.; Veerkamp, M.W.; Stacey, J.D.; Gupta, R.; Pendleton, A.M.; Shea, K.G.; Friel, N.A.; Molony, J.T., Jr.; Yaniv, M.; et al. Consensus-Based Guidelines for Management of First-Time Patellar Dislocation in Adolescents. J. Pediatr. Orthop. 2024, 44, e369–e374. [Google Scholar] [CrossRef] [PubMed]
- Hinckel, B.B.; Liebensteiner, M.; Smith, J.T.; Gobbi, R.G.; Arendt, E.A. Patellofemoral instability part 2 (Bony procedure for patellar surgical stabilization): State of the art. J. ISAKOS 2024, 10, 100347. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Category | No Fracture (n = 128) | Fracture (n = 133) | Overall (n = 261) | p-Value | Statistical Test |
|---|---|---|---|---|---|---|
| DEMOGRAPHIC CHARACTERISTICS | ||||||
| Age (years, ±SD [range]) | 24 ± 10 [17–30] | 23 ± 10 [16–27] | 24 ± 10 [16–30] | 0.542 | t-test | |
| Gender (n, %) | Female: Male: | 70 (55%) 58 (45%) | 38 (29%) 95 (71%) | 108 (41%) 153 (59%) | <0.001 | X2 = 18.34 |
| Side (n, %) | Left: Right: | 96 (75%) 32 (25%) | 76 (57%) 57 (43%) | 172(66%) 89 (34%) | <0.01 | X2 = 9.26 |
| FRACTURE CHARACTERISTICS | ||||||
| Defect Size (cm, ±SD [range]) | - | 3.2 ± 3.2 [1.0–4.0] | - | - | - | |
| TROCHLEAR MORPHOLOGY (MRI) | ||||||
| Déjour Classification (n, %) | No dysplasia: | 39 (30%) | 63 (47%) | 102 (39%) | 0.003 | X2 = 16.52 |
| Grade A: | 18 (14%) | 27 (20%) | 45 (17%) | |||
| Grade B: | 37 (29%) | 30 (23%) | 67 (26%) | |||
| Grade C: | 27 (21%) | 12 (9.0%) | 39 (15%) | |||
| Grade D | 7 (5.5%) | 1 (0.8%) | 8 (3.1%) | |||
| Sulcus angle (°, ±SD) | 150 ± 12 | 147 ± 10 | 148 ± 11 | 0.081 | t-test | |
| Congruence Angle (°, ± SD) | −1 ± 37 | 5 ± 22 | 2 ± 30 | 0.125 | t-test | |
| Trochlear Facet Asymmetry (±SD) | 0.6 ± 0.2 | 0.6 ± 0.2 | 0.6 ± 0.2 | 0.689 | t-test | |
| Medial Trochlear Facet Length (mm, ±SD) | 12.7 ± 2.9 | 13.3 ± 2.9 | 13.0 ± 2.9 | 0.162 | t-test | |
| Lateral Trochlear Facet Length (mm, ±SD) | 21.3 ± 3.7 | 22.4 ± 3.4 | 21.9 ± 3.6 | 0.021 | t-test | |
| Trochlear Groove Depth (mm, ±SD) | 5.1 ± 1.6 | 10.5 ± 60.8 | 7.9 ± 43.9 | 0.823 | Mann–Whitney U | |
| Trochlear Condyle Asymmetry (±SD) | 1.0 ± 0.03 | 1.0 ± 0.03 | 1.0 ± 0.03 | <0.05 | t-test | |
| Lateral Trochlear Angle Inclination (°, ±SD) | 16.4 ± 4.5 | 15.5 ± 4.4 | 15.9 ± 4.5 | 0.378 | t-test | |
| PATELLOFEMORAL ALIGNMENT | ||||||
| Q-angle (°, ±SD) | 4 ± 10.4 | 7 ± 16.1 | 6 ± 14.2 | 0.543 | t-test | |
| TT-TG Distance (mm, ±SD) | 13.1 ± 5.6 | 13.3 ± 4.9 | 13.2 ± 5.3 | 0.743 | t-test | |
| TT-PCL Distance (mm, ±SD) | 24.2 ± 9.3 | 25.4 ± 10.1 | 24.9 ± 9.6 | 0.345 | t-test |
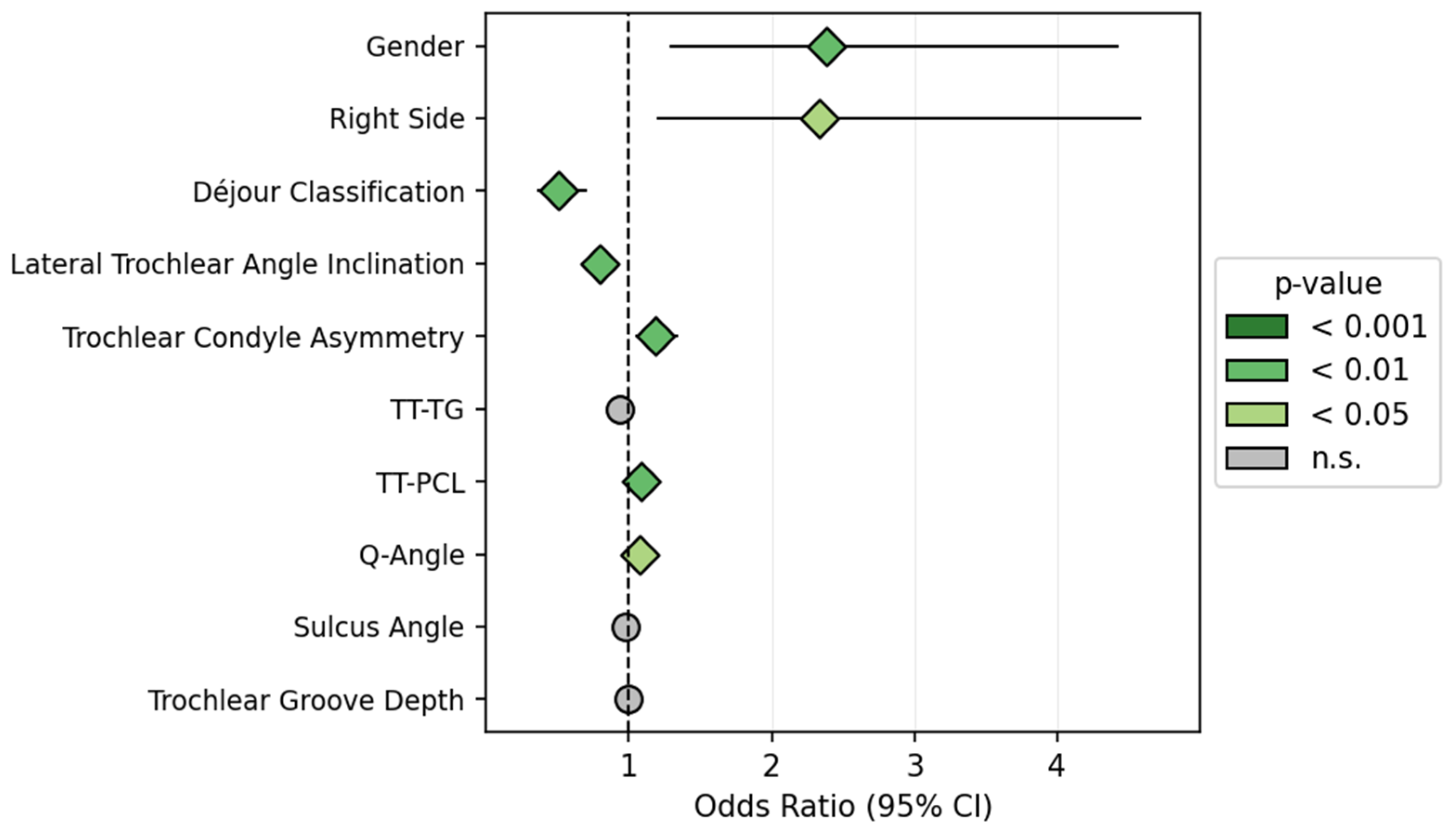
| Predictor | OR (95% CI) | p-Value |
|---|---|---|
| Gender | 2.38 (1.3–4.42) | 0.005 |
| Right Side | 2.33 (1.21–4.58) | 0.013 |
| Déjour Classification | 0.51 (0.37–0.70) | <0.001 |
| Lateral Trochlear Angle Inclination | 0.80 (0.71–0.90) | <0.001 |
| Trochlear Condyle Asymmetry | 1.19 (1.06–1.34) | 0.004 |
| TT-TG | 0.94 (0.88–1.01) | 0.077 |
| TT-PCL | 1.09 (1.03–1.15) | 0.001 |
| Q-Angle | 1.08 (1.03–1.13) | 0.028 |
| Sulcus Angle | 0.98 (0.94–1.01) | 0.157 |
| Trochlear Groove Depth | 1.00 (1.00–1.00) | 0.094 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rüther, J.; Geßlein, M.; Millrose, M.; Willauschus, M.; Beck, J.; Engel, N.; Kopf, A.; Bail, H.J.; Hielscher, L. Male Gender and Normal Trochlear Anatomy Are Associated with a Higher Risk of Osteochondral Fracture Following Patellar Dislocation: A Retrospective Review of 261 Skeletally Mature Patients. J. Clin. Med. 2025, 14, 8235. https://doi.org/10.3390/jcm14228235
Rüther J, Geßlein M, Millrose M, Willauschus M, Beck J, Engel N, Kopf A, Bail HJ, Hielscher L. Male Gender and Normal Trochlear Anatomy Are Associated with a Higher Risk of Osteochondral Fracture Following Patellar Dislocation: A Retrospective Review of 261 Skeletally Mature Patients. Journal of Clinical Medicine. 2025; 14(22):8235. https://doi.org/10.3390/jcm14228235
Chicago/Turabian StyleRüther, Johannes, Markus Geßlein, Michael Millrose, Maximilian Willauschus, Jonas Beck, Niklas Engel, Andreas Kopf, Hermann Josef Bail, and Lotta Hielscher. 2025. "Male Gender and Normal Trochlear Anatomy Are Associated with a Higher Risk of Osteochondral Fracture Following Patellar Dislocation: A Retrospective Review of 261 Skeletally Mature Patients" Journal of Clinical Medicine 14, no. 22: 8235. https://doi.org/10.3390/jcm14228235
APA StyleRüther, J., Geßlein, M., Millrose, M., Willauschus, M., Beck, J., Engel, N., Kopf, A., Bail, H. J., & Hielscher, L. (2025). Male Gender and Normal Trochlear Anatomy Are Associated with a Higher Risk of Osteochondral Fracture Following Patellar Dislocation: A Retrospective Review of 261 Skeletally Mature Patients. Journal of Clinical Medicine, 14(22), 8235. https://doi.org/10.3390/jcm14228235









