Plasma Neurofilament Light Chain and Phosphorylated Tau Are Elevated in Myotonic Dystrophy Type 1
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Measurement of Blood Biomarkers
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Comparison of Biomarker Levels Between DM1 Patients and Controls
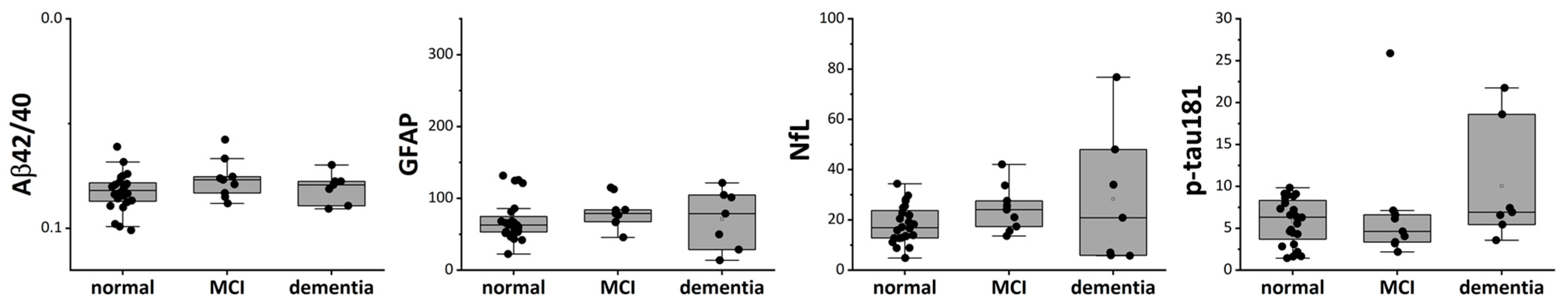
3.3. Sex-Related Difference in Biomarkers
3.4. Correlation Analyses Among Biomarkers and Clinical Parameters in DM1
4. Discussion
4.1. NfL
4.2. p-Tau181
4.3. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Aβ | amyloid beta |
| AD | Alzheimer’s disease |
| ALS | amyotrophic lateral sclerosis |
| ANCOVA | analysis of covariance |
| CK | creatine kinase |
| CNS | central nervous system |
| CSF | cerebrospinal fluid |
| DM | Myotonic dystrophy |
| GFAP | glial fibrillary acidic protein |
| MCI | mild cognitive impairment |
| MMSE | Mini-Mental State Examination |
| mRS | modified Rankin Scale |
| NfL | neurofilament light chain |
| pTau | phosphorylated tau |
| PSP | progressive supranuclear palsy |
| Simoa | single-molecule array |
| 3R | three-repeat |
| 4PL | four-parameter logistic |
| 4R | four-repeat |
References
- Ashizawa, T.; Sarkar, P.S. Myotonic Dystrophy Types 1 and 2. Handb. Clin. Neurol. 2011, 101, 193–237. [Google Scholar] [CrossRef] [PubMed]
- Rahm, L.; Hale, M.A.; Raaijmakers, R.H.L.; Marrero Quiñones, A.; Patki, T.; Johnson, N.E.; van Bokhoven, H.; Mul, K. Myotonic Dystrophy Type 1: Clinical Diversity, Molecular Insights and Therapeutic Perspectives. Nat. Rev. Neurol. 2025, 21, 623–641. [Google Scholar] [CrossRef] [PubMed]
- López-Martínez, A.; Soblechero-Martín, P.; De-La-puente-ovejero, L.; Nogales-Gadea, G.; Arechavala-Gomeza, V. An Overview of Alternative Splicing Defects Implicated in Myotonic Dystrophy Type I. Genes 2020, 11, 1109. [Google Scholar] [CrossRef] [PubMed]
- Udd, B.; Krahe, R. The Myotonic Dystrophies: Molecular, Clinical, and Therapeutic Challenges. Lancet Neurol. 2012, 11, 891–905. [Google Scholar] [CrossRef]
- Kuntawala, D.H.; Vitorino, R.; Cruz, A.C.; Martins, F.; Rebelo, S. Multisystem Symptoms in Myotonic Dystrophy Type 1: A Management and Therapeutic Perspective. Int. J. Mol. Sci. 2025, 26, 5350. [Google Scholar] [CrossRef]
- Gourdon, G.; Meola, G. Myotonic Dystrophies: State of the Art of New Therapeutic Developments for the CNS. Front. Cell. Neurosci. 2017, 11, 101. [Google Scholar] [CrossRef]
- Takahashi, M.P. Update on the Clinical and Therapeutic Aspects of Myotonic Dystrophy Type 1. Curr. Opin. Neurol. 2025, 38, 531–537. [Google Scholar] [CrossRef]
- Miller, J.N.; Kruger, A.; Moser, D.J.; Gutmann, L.; van der Plas, E.; Koscik, T.R.; Cumming, S.A.; Monckton, D.G.; Nopoulos, P.C. Cognitive Deficits, Apathy, and Hypersomnolence Represent the Core Brain Symptoms of Adult-Onset Myotonic Dystrophy Type 1. Front. Neurol. 2021, 12, 700796. [Google Scholar] [CrossRef]
- Okkersen, K.; Buskes, M.; Groenewoud, J.; Kessels, R.P.C.; Knoop, H.; van Engelen, B.; Raaphorst, J. The Cognitive Profile of Myotonic Dystrophy Type 1: A Systematic Review and Meta-Analysis. Cortex 2017, 95, 143–155. [Google Scholar] [CrossRef]
- Fujino, H.; Shingaki, H.; Suwazono, S.; Ueda, Y.; Wada, C.; Nakayama, T.; Takahashi, M.P.; Imura, O.; Matsumura, T. Cognitive Impairment and Quality of Life in Patients with Myotonic Dystrophy Type 1. Muscle Nerve 2018, 57, 742–748. [Google Scholar] [CrossRef]
- Minnerop, M.; Weber, B.; Schoene-Bake, J.C.; Roeske, S.; Mirbach, S.; Anspach, C.; Schneider-Gold, C.; Betz, R.C.; Helmstaedter, C.; Tittgemeyer, M.; et al. The Brain in Myotonic Dystrophy 1 and 2: Evidence for a Predominant White Matter Disease. Brain 2011, 134, 3527–3543. [Google Scholar] [CrossRef]
- Minnerop, M.; Gliem, C.; Kornblum, C. Current Progress in CNS Imaging of Myotonic Dystrophy. Front. Neurol. 2018, 9, 646. [Google Scholar] [CrossRef] [PubMed]
- Okkersen, K.; Monckton, D.G.; Le, N.; Tuladhar, A.M.; Raaphorst, J.; Van Engelen, B.G.M. Brain Imaging in Myotonic Dystrophy Type 1: A Systematic Review. Neurology 2017, 89, 960–969. [Google Scholar] [CrossRef] [PubMed]
- Weijs, R.; Okkersen, K.; van Engelen, B.; Küsters, B.; Lammens, M.; Aronica, E.; Raaphorst, J.; van Cappellen van Walsum, A.M. Human Brain Pathology in Myotonic Dystrophy Type 1: A Systematic Review. Neuropathology 2021, 41, 3–20. [Google Scholar] [CrossRef] [PubMed]
- Jiang, H.; Mankodi, A.; Swanson, M.S.; Moxley, R.T.; Thornton, C.A. Myotonic Dystrophy Type 1 Is Associated with Nuclear Foci of Mutant RNA, Sequestration of Muscleblind Proteins and Deregulated Alternative Splicing in Neurons. Hum. Mol. Genet. 2004, 13, 3079–3088. [Google Scholar] [CrossRef]
- Dhaenens, C.M.; Tran, H.; Frandemiche, M.L.; Carpentier, C.; Schraen-Maschke, S.; Sistiaga, A.; Goicoechea, M.; Eddarkaoui, S.; Van Brussels, E.; Obriot, H.; et al. Mis-Splicing of Tau Exon 10 in Myotonic Dystrophy Type 1 Is Reproduced by Overexpression of CELF2 but Not by MBNL1 Silencing. Biochim. Biophys. Acta-Mol. Basis Dis. 2011, 1812, 732–742. [Google Scholar] [CrossRef]
- Dhaenens, C.M.; Schraen-Maschke, S.; Tran, H.; Vingtdeux, V.; Ghanem, D.; Leroy, O.; Delplanque, J.; Vanbrussel, E.; Delacourte, A.; Vermersch, P.; et al. Overexpression of MBNL1 Fetal Isoforms and Modified Splicing of Tau in the DM1 Brain: Two Individual Consequences of CUG Trinucleotide Repeats. Exp. Neurol. 2008, 210, 467–478. [Google Scholar] [CrossRef]
- Hernández-Hernández, O.; Sicot, G.; Dinca, D.M.; Huguet, A.; Nicole, A.; Buée, L.; Munnich, A.; Sergeant, N.; Gourdon, G.; Gomes-Pereira, M. Synaptic Protein Dysregulation in Myotonic Dystrophy Type 1: Disease Neuropathogenesis beyond Missplicing. Rare Dis. 2013, 1, e25553. [Google Scholar] [CrossRef]
- Caillet-Boudin, M.-L.; Fernandez-Gomez, F.-J.; Tran, H.; Dhaenens, C.-M.; Buee, L.; Sergeant, N. Brain Pathology in Myotonic Dystrophy: When Tauopathy Meets Spliceopathy and RNAopathy. Front. Mol. Neurosci. 2014, 6, 57. [Google Scholar] [CrossRef]
- Aranda-Abreu, G.E.; Rojas-Durán, F.; Hernández-Aguilar, M.E.; Herrera-Covarrubias, D.; García-Hernández, L.I.; Toledo-Cárdenas, M.R.; Chi-Castañeda, D. The Role of Tau in Neuronal Function and Neurodegeneration. Neurol. Int. 2025, 17, 75. [Google Scholar] [CrossRef]
- Andreadis, A. Tau Splicing and the Intricacies of Dementia. J. Cell. Physiol. 2012, 227, 1220–1225. [Google Scholar] [CrossRef]
- Hansson, O.; Blennow, K.; Zetterberg, H.; Dage, J. Blood Biomarkers for Alzheimer’s Disease in Clinical Practice and Trials. Nat. Aging 2023, 3, 506–519. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; KC, N.; Paneque, A.; Cole, P.D. Tau, Glial Fibrillary Acidic Protein, and Neurofilament Light Chain as Brain Protein Biomarkers in Cerebrospinal Fluid and Blood for Diagnosis of Neurobiological Diseases. Int. J. Mol. Sci. 2024, 25, 6295. [Google Scholar] [CrossRef] [PubMed]
- Dong, R.; Yi, N.; Jiang, D. Advances in Single Molecule Arrays (SIMOA) for Ultra-Sensitive Detection of Biomolecules. Talanta 2024, 270, 125529. [Google Scholar] [CrossRef] [PubMed]
- Pais, M.V.; Forlenza, O.V.; Diniz, B.S. Plasma Biomarkers of Alzheimer’s Disease: A Review of Available Assays, Recent Developments, and Implications for Clinical Practice. J. Alzheimer’s Dis. Rep. 2023, 7, 355–380. [Google Scholar] [CrossRef]
- Janelidze, S.; Mattsson, N.; Palmqvist, S.; Smith, R.; Beach, T.G.; Serrano, G.E.; Chai, X.; Proctor, N.K.; Eichenlaub, U.; Zetterberg, H.; et al. Plasma P-Tau181 in Alzheimer’s Disease: Relationship to Other Biomarkers, Differential Diagnosis, Neuropathology and Longitudinal Progression to Alzheimer’s Dementia. Nat. Med. 2020, 26, 379–386. [Google Scholar] [CrossRef]
- Hansson, O. Biomarkers for Neurodegenerative Diseases. Nat. Med. 2021, 27, 954–963. [Google Scholar] [CrossRef]
- A Virata, M.C.; Catahay, J.A.; Lippi, G.; Henry, B.M. Neurofilament Light Chain: A Biomarker at the Crossroads of Clarity and Confusion for Gene-Directed Therapies. Neurodegener. Dis. Manag. 2024, 14, 227–239. [Google Scholar] [CrossRef]
- Gonzalez-Ortiz, F.; Kac, P.R.; Brum, W.S.; Zetterberg, H.; Blennow, K.; Karikari, T.K. Plasma Phospho-Tau in Alzheimer’s Disease: Towards Diagnostic and Therapeutic Trial Applications. Mol. Neurodegener. 2023, 18, 18. [Google Scholar] [CrossRef]
- Thomas, E.V.; Han, C.; Kim, W.J.; Asress, S.; Li, Y.; Taylor, J.A.; Gearing, M.; Fournier, C.N.; McEachin, Z.T.; Seyfried, N.T.; et al. ALS Plasma Biomarkers Reveal Neurofilament and PTau Correlate with Disease Onset and Progression. Ann. Clin. Transl. Neurol. 2025, 12, 714–723. [Google Scholar] [CrossRef]
- Abu-Rumeileh, S.; Scholle, L.; Mensch, A.; Großkopf, H.; Ratti, A.; Kölsch, A.; Stoltenburg-Didinger, G.; Conrad, J.; De Gobbi, A.; Barba, L.; et al. Phosphorylated Tau 181 and 217 Are Elevated in Serum and Muscle of Patients with Amyotrophic Lateral Sclerosis. Nat. Commun. 2025, 16, 2019. [Google Scholar] [CrossRef]
- Laforce, R.J.; Dallaire-Théroux, C.; Racine, A.M.; Dent, G.; Salinas-Valenzuela, C.; Poulin, E.; Cayer, A.M.; Bédard-Tremblay, D.; Rouleau-Bonenfant, T.; St-Onge, F.; et al. Tau Positron Emission Tomography, Cerebrospinal Fluid and Plasma Biomarkers of Neurodegeneration, and Neurocognitive Testing: An Exploratory Study of Participants with Myotonic Dystrophy Type 1. J. Neurol. 2022, 269, 3579–3587. [Google Scholar] [CrossRef] [PubMed]
- Nicoletti, T.F.; Rossi, S.; Vita, M.G.; Perna, A.; Guerrera, G.; Lino, F.; Iacovelli, C.; Di Natale, D.; Modoni, A.; Battistini, L.; et al. Elevated Serum Neurofilament Light Chain (NfL) as a Potential Biomarker of Neurological Involvement in Myotonic Dystrophy Type 1 (DM1). J. Neurol. 2022, 269, 5085–5092. [Google Scholar] [CrossRef] [PubMed]
- van der Plas, E.; Long, J.D.; Koscik, T.R.; Magnotta, V.; Monckton, D.G.; Cumming, S.A.; Gottschalk, A.C.; Hefti, M.; Gutmann, L.; Nopoulos, P.C. Blood-Based Markers of Neuronal Injury in Adult-Onset Myotonic Dystrophy Type 1. Front. Neurol. 2022, 12, 791065. [Google Scholar] [CrossRef] [PubMed]
- Winblad, S.; Månsson, J.E.; Blennow, K.; Jensen, C.; Samuelsson, L.; Lindberg, C. Cerebrospinal Fluid Tau and Amyloid Beta42 Protein in Patients with Myotonic Dystrophy Type 1. Eur. J. Neurol. 2008, 15, 947–952. [Google Scholar] [CrossRef]
- Peric, S.; Mandic-Stojmenovic, G.; Markovic, I.; Stefanova, E.; Ilic, V.; Parojcic, A.; Misirlic-Dencic, S.; Ostojic, M.; Rakocevic-Stojanovic, V.; Kostic, V. Cerebrospinal Fluid Biomarkers of Neurodegeneration in Patients with Juvenile and Classic Myotonic Dystrophy Type 1. Eur. J. Neurol. 2014, 21, 231–237. [Google Scholar] [CrossRef]
- Saak, A.; Benkert, P.; Akgün, K.; Willemse, E.; Kuhle, J.; Ziemssen, T.; Jackson, S.; Schaefer, J. Serum Neurofilament Light Chain: A Marker of Nervous System Damage in Myopathies. Front. Neurosci. 2021, 15, 791670. [Google Scholar] [CrossRef]
- Rossi, S.; Silvestri, G. Fluid Biomarkers of Central Nervous System (CNS) Involvement in Myotonic Dystrophy Type 1 (DM1). Int. J. Mol. Sci. 2023, 24, 2204. [Google Scholar] [CrossRef]
- Mizutani, Y.; Ohdake, R.; Tatebe, H.; Higashi, A.; Shima, S.; Ueda, A.; Ito, M.; Tokuda, T.; Watanabe, H. Associations of Alzheimer’s-Related Plasma Biomarkers with Cognitive Decline in Parkinson’s Disease. J. Neurol. 2023, 270, 5461–5474. [Google Scholar] [CrossRef]
- Simoa® PTau-181 V2 Advantage Kit HD-1/HD-X Data Sheet. Available online: https://www.quanterix.com/wp-content/uploads/2021/03/pTau-181-V2-Data-Sheet-HD-1-and-HD-X-Rev03.pdf (accessed on 3 November 2025).
- Simoa ® Neurology 4-Plex E Advantage Kit HD-X® Data Sheet. Available online: https://www.quanterix.com/wp-content/uploads/2020/12/Neurology-4-Plex-E-Data-Sheet-HD-X.pdf (accessed on 3 November 2025).
- Dogan, C.; De Antonio, M.; Hamroun, D.; Varet, H.; Fabbro, M.; Rougier, F.; Amarof, K.; Bes, M.C.A.; Bedat-Millet, A.L.; Behin, A.; et al. Gender as a Modifying Factor Influencing Myotonic Dystrophy Type 1 Phenotype Severity and Mortality: A Nationwide Multiple Databases Cross-Sectional Observational Study. PLoS ONE 2016, 11, e0148264. [Google Scholar] [CrossRef]
- Chakraborty, D.; Borthakur, S.; Sarkar, R.; Singh, M.D. Gender Disparities in Myotonic Dystrophy 1. Life Sci. 2025, 373, 123659. [Google Scholar] [CrossRef]
- Tsiknia, A.A.; Edland, S.D.; Sundermann, E.E.; Reas, E.T.; Brewer, J.B.; Galasko, D.; Banks, S.J. Sex Differences in Plasma P-Tau181 Associations with Alzheimer’s Disease Biomarkers, Cognitive Decline, and Clinical Progression. Mol. Psychiatry 2022, 27, 4314–4322. [Google Scholar] [CrossRef]
- Labonte, J.; Sugarman, M.A.; Pettway, E.; Zetterberg, H.; Blennow, K.; Ashton, N.J.; Karikari, T.K.; Aparicio, H.J.; Frank, B.; Tripodis, Y.; et al. Sex Differences on Tau, Astrocytic, and Neurodegenerative Plasma Biomarkers. J. Alzheimer’s Dis. 2025, 105, 443–452. [Google Scholar] [CrossRef]

| DM1, n = 40 | Control, n = 38 | p Value | |
|---|---|---|---|
| Age (years) | 47.5 [39, 50] | 68 [64, 73] | <0.0001 |
| Sex (male) | 45% | 50% | 0.83 |
| Education (years) | 12 [12, 14] | 14 [12, 16] | 0.008 |
| MMSE | 28.5 [25, 30] | 29 [28, 30] | 0.041 |
| Age at onset (years) | 28.5 [20, 39] | ||
| CTG repeat | 1500 [975, 2175] | ||
| mRS | 3 [2, 4] | ||
| CK | 195 [112, 291] (n = 38) | ||
| Wheelchair | 25.0% | 0% | 0.001 |
| Impaired glucose tolerance | 32.5% | 13.2% | 0.043 |
| Pacemaker | 7.5% | 0% | 0.158 |
| Ventilator | 12.5% | 0% | 0.010 |
| DM (n = 40) | Control (n = 38) | F | p Value | |
|---|---|---|---|---|
| Aβ42/40 | 0.0797 [0.0763–0.0865] | 0.0648 [0.0593–0.0754] | 16.4 | <0.0001 |
| GFAP | 66.5 [53.7–85.4] | 113.8 [81.2–146.7] | 0.59 | 0.4450 |
| NfL | 18.7 [13.0–27.1] | 12.8 [11.1–16.2] | 45.4 | <0.0001 |
| p-tau-181 | 6.32 [3.70–7.85] | 1.40 [1.18–1.91] | 45.1 | <0.0001 |
| Control | DM1 | |||||
|---|---|---|---|---|---|---|
| Male | Female | p-Value | Male | Female | p-Value | |
| n = 19 | n = 19 | n = 18 | n = 22 | |||
| Age | 70 [66.5–73.5] | 66 [63–39] | 0.016 | 41.5 [29.3–48] | 50 [45.25–52.5] | 0.005 |
| Years of Education | 16 [12–16] | 14 [12–14] | 0.019 | 12 [12–13.75] | 12 [12–14] | 0.271 |
| MMSE | 29 [28, 29] | 29 [28.5–30] | 0.142 | 26 [23.3–29] | 29 [27.25–40] | 0.043 |
| Aβ42/40 | 0.064 [0.059–0.070] | 0.064 [0.060–0.072] | 0.290 | 0.079 [0.073–0.081] | 0.083 [0.078–0.088] | 0.050 |
| GFAP | 85.2 [76.7–120.8] | 130.0 [113.8–146.9] | 0.031 | 64.8 [54.3–76.1] | 72.5 [53.1–97.4] | 0.167 |
| NfL | 14.80 [11.95–19.15] | 11.51 [10.24–13.93] | 0.033 | 25.12 [12.90–32.68] | 16.85 [13.52–21.63] | 0.089 |
| p-tau181 | 1.33 [1.16–1.70] | 1.58 [1.26–2.01] | 0.207 | 7.02 [5.16–8.71] | 5.028 [3.21–6.73] | 0.029 |
| Age | Onset Age | mRS | CTG | CK | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Rho | p Value | Rho | p Value | Rho | p Value | Rho | p Value | Rho | p Value | |
| Aβ42/40 | −0.0303 | 0.8525 | −0.1774 | 0.2735 | −0.0041 | 0.9801 | −0.1813 | 0.2630 | 0.2943 | 0.7290 |
| GFAP | 0.5087 | 0.0008 | 0.3371 | 0.0334 | 0.2225 | 0.1675 | 0.1141 | 0.4834 | −0.2666 | 0.1056 |
| NfL | 0.4370 | 0.0048 | 0.4382 | 0.0047 | 0.3968 | 0.0113 | 0.2728 | 0.0885 | −0.2930 | 0.0742 |
| p-tau181 | −0.1337 | 0.4107 | −0.2422 | 0.1321 | 0.1415 | 0.3837 | 0.0076 | 0.9629 | 0.5779 | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, M.P.; Tatebe, H.; Takada, H.; Nakayama, T.; Kobayashi, M.; Yoshida, K.; Kuru, S.; Kira, N.; Kubota, T.; Mizutani, Y.; et al. Plasma Neurofilament Light Chain and Phosphorylated Tau Are Elevated in Myotonic Dystrophy Type 1. J. Clin. Med. 2025, 14, 8197. https://doi.org/10.3390/jcm14228197
Takahashi MP, Tatebe H, Takada H, Nakayama T, Kobayashi M, Yoshida K, Kuru S, Kira N, Kubota T, Mizutani Y, et al. Plasma Neurofilament Light Chain and Phosphorylated Tau Are Elevated in Myotonic Dystrophy Type 1. Journal of Clinical Medicine. 2025; 14(22):8197. https://doi.org/10.3390/jcm14228197
Chicago/Turabian StyleTakahashi, Masanori P., Harutsugu Tatebe, Hiroto Takada, Takahiro Nakayama, Michio Kobayashi, Kosuke Yoshida, Satoshi Kuru, Natsuki Kira, Tomoya Kubota, Yasuaki Mizutani, and et al. 2025. "Plasma Neurofilament Light Chain and Phosphorylated Tau Are Elevated in Myotonic Dystrophy Type 1" Journal of Clinical Medicine 14, no. 22: 8197. https://doi.org/10.3390/jcm14228197
APA StyleTakahashi, M. P., Tatebe, H., Takada, H., Nakayama, T., Kobayashi, M., Yoshida, K., Kuru, S., Kira, N., Kubota, T., Mizutani, Y., Watanabe, H., Takado, Y., & Tokuda, T. (2025). Plasma Neurofilament Light Chain and Phosphorylated Tau Are Elevated in Myotonic Dystrophy Type 1. Journal of Clinical Medicine, 14(22), 8197. https://doi.org/10.3390/jcm14228197






