Exercise-Based Prehabilitation Before Cardiac Surgery: A Systematic Review, Meta-Analysis, Meta-Regression, and Proposal for a Clinical Implementation Model
Abstract
1. Introduction
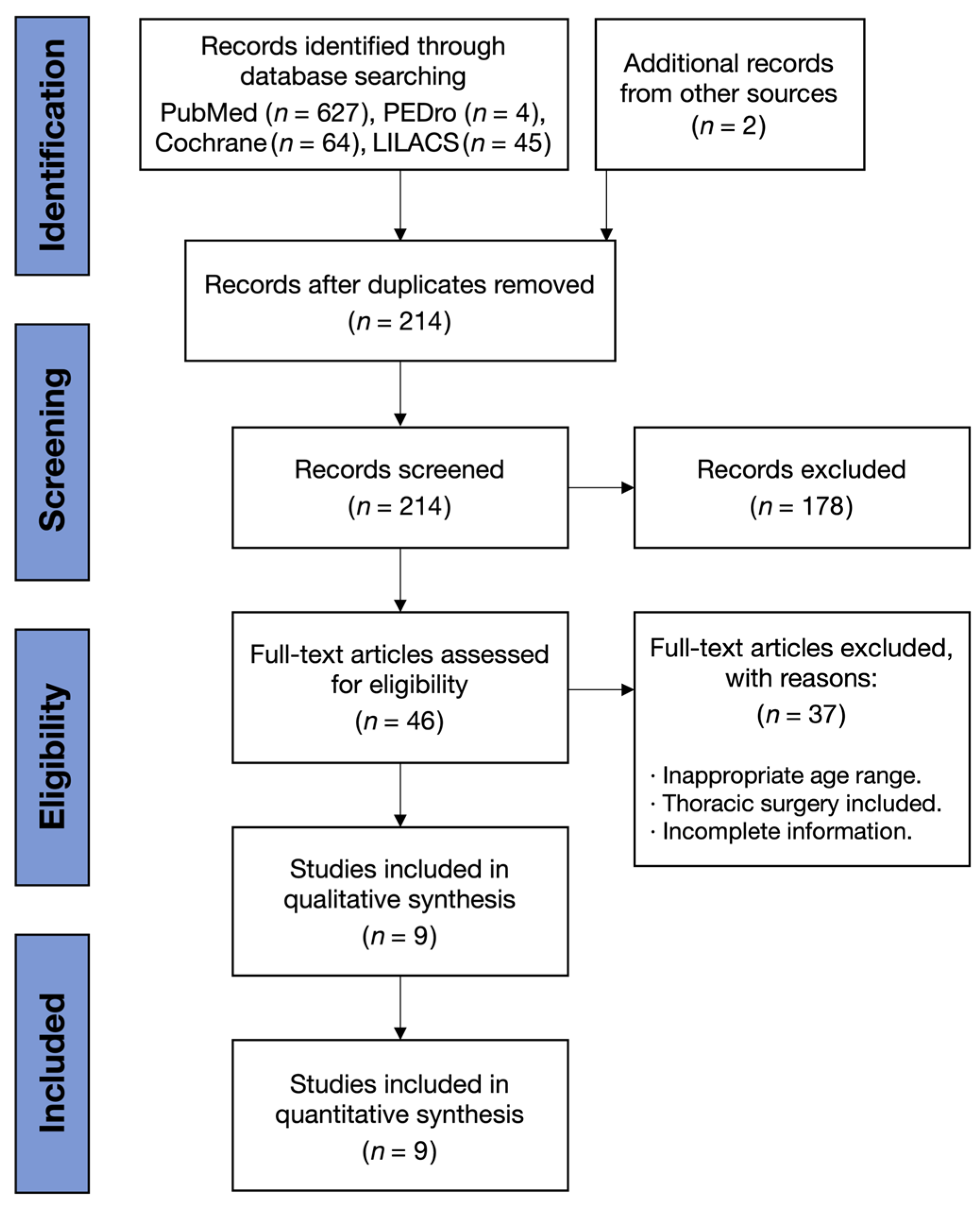
2. Materials and Methods
2.1. Search Strategy, Inclusion and Exclusion Criteria
2.2. Data Extraction
2.3. Risk of Bias Assessment
2.4. Quality of Evidence Assessment
2.5. Statistical Analysis
2.5.1. Meta-Regression
2.5.2. Subgroup Analyses
2.5.3. Sensitivity Analyses
3. Results
3.1. Study Characteristics
3.2. Characteristics of Prehabilitation Programs
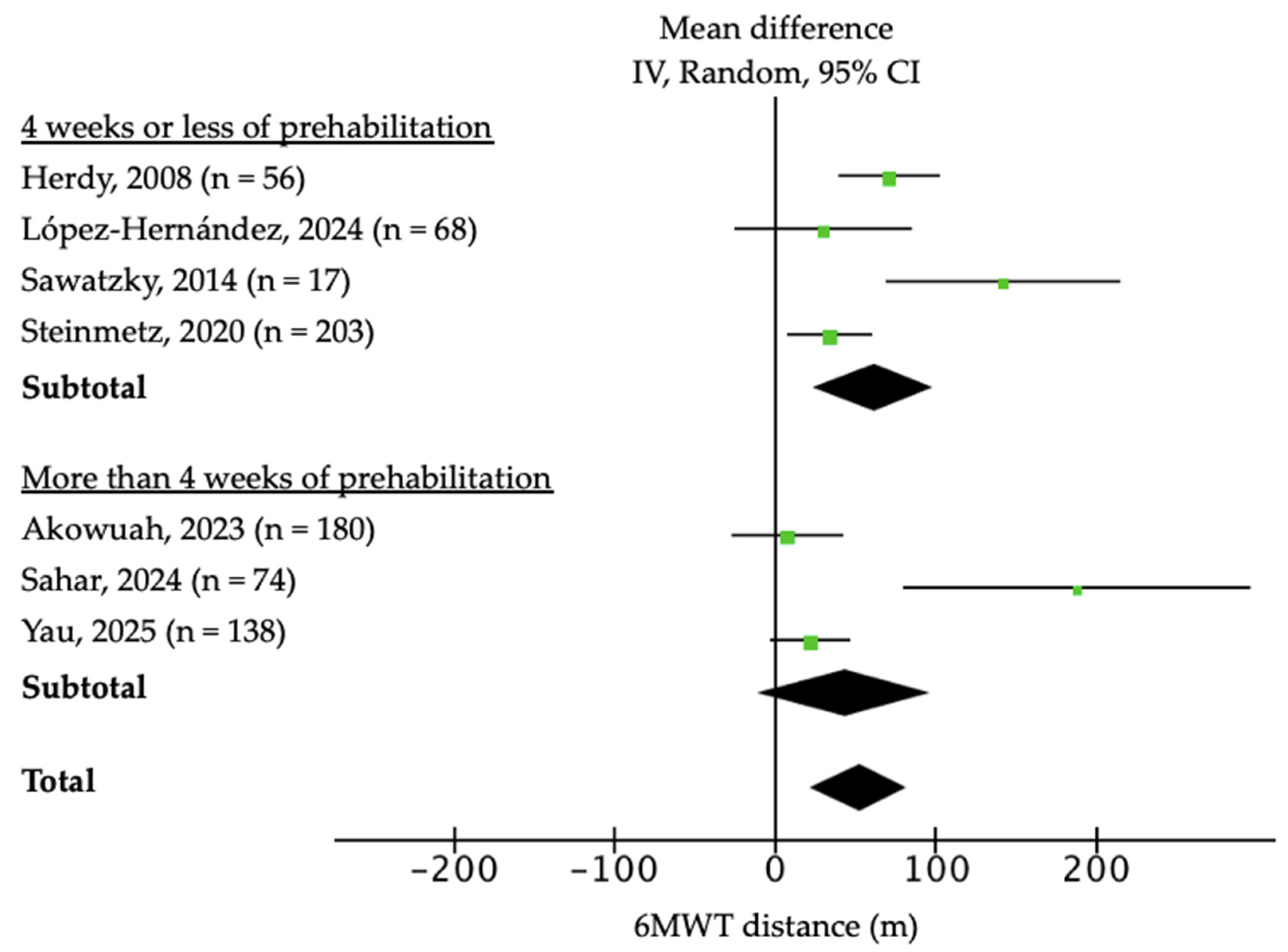
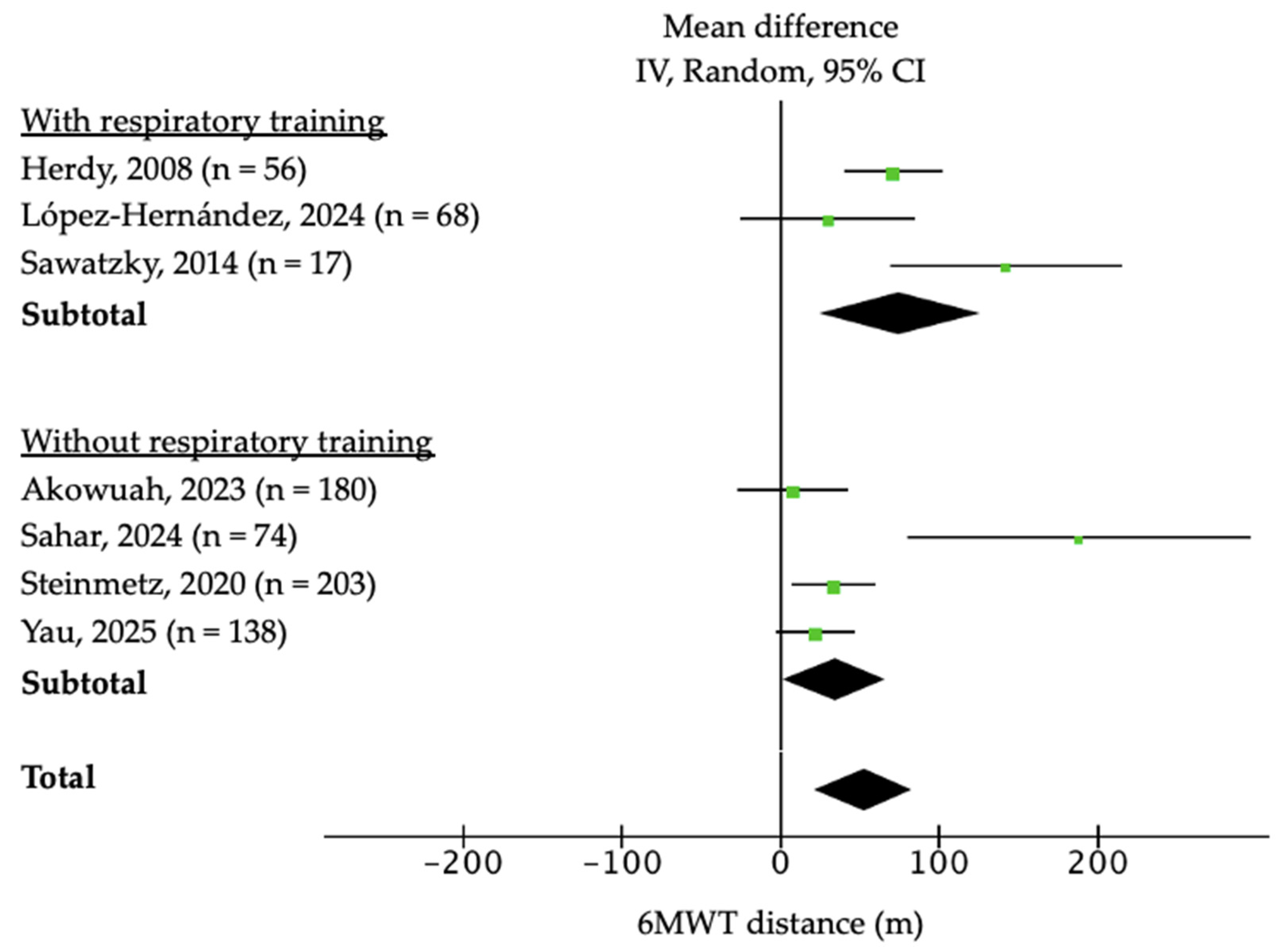
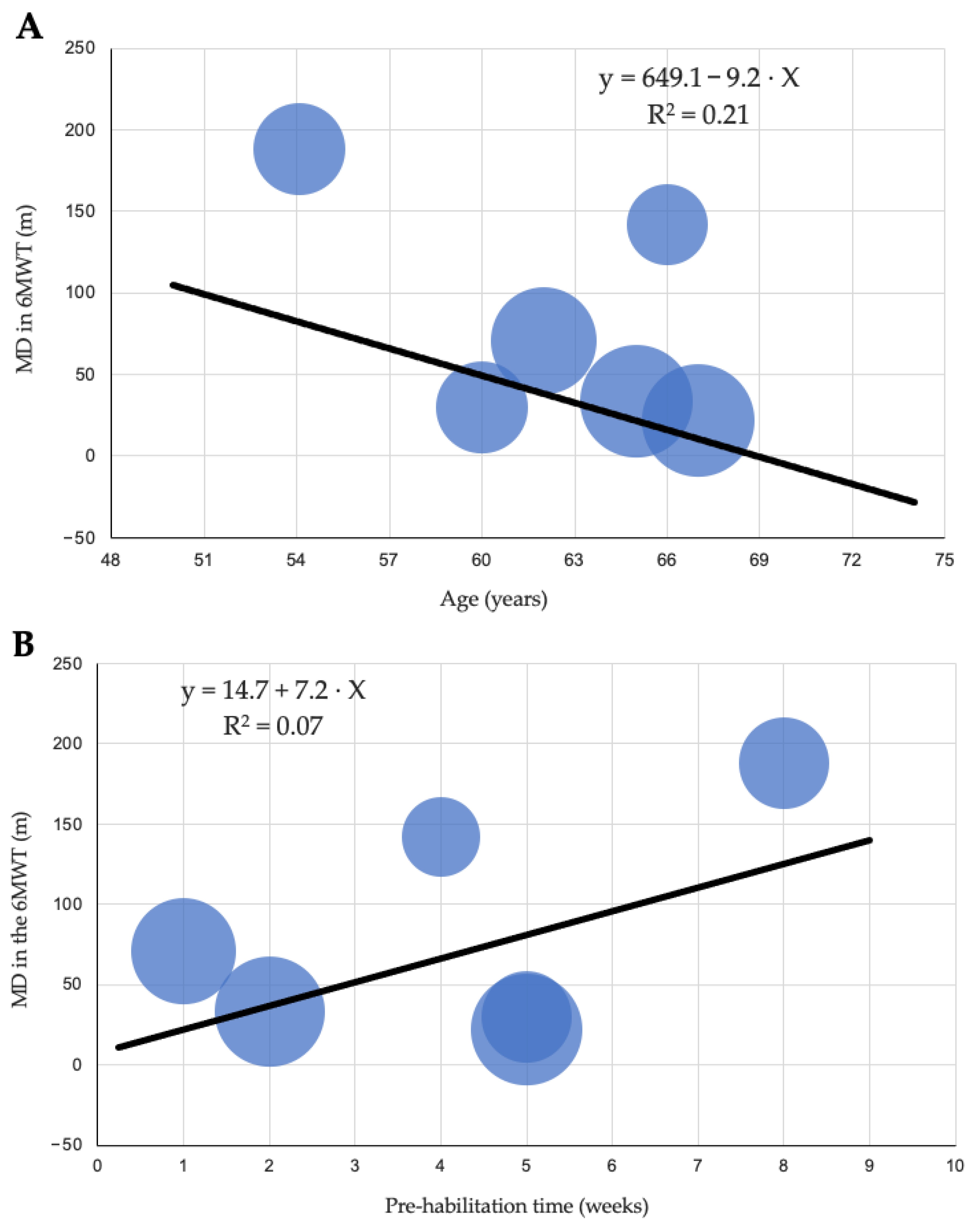
3.3. Functional Capacity
3.4. Frailty
3.5. Sarcopenia and Dynapenia
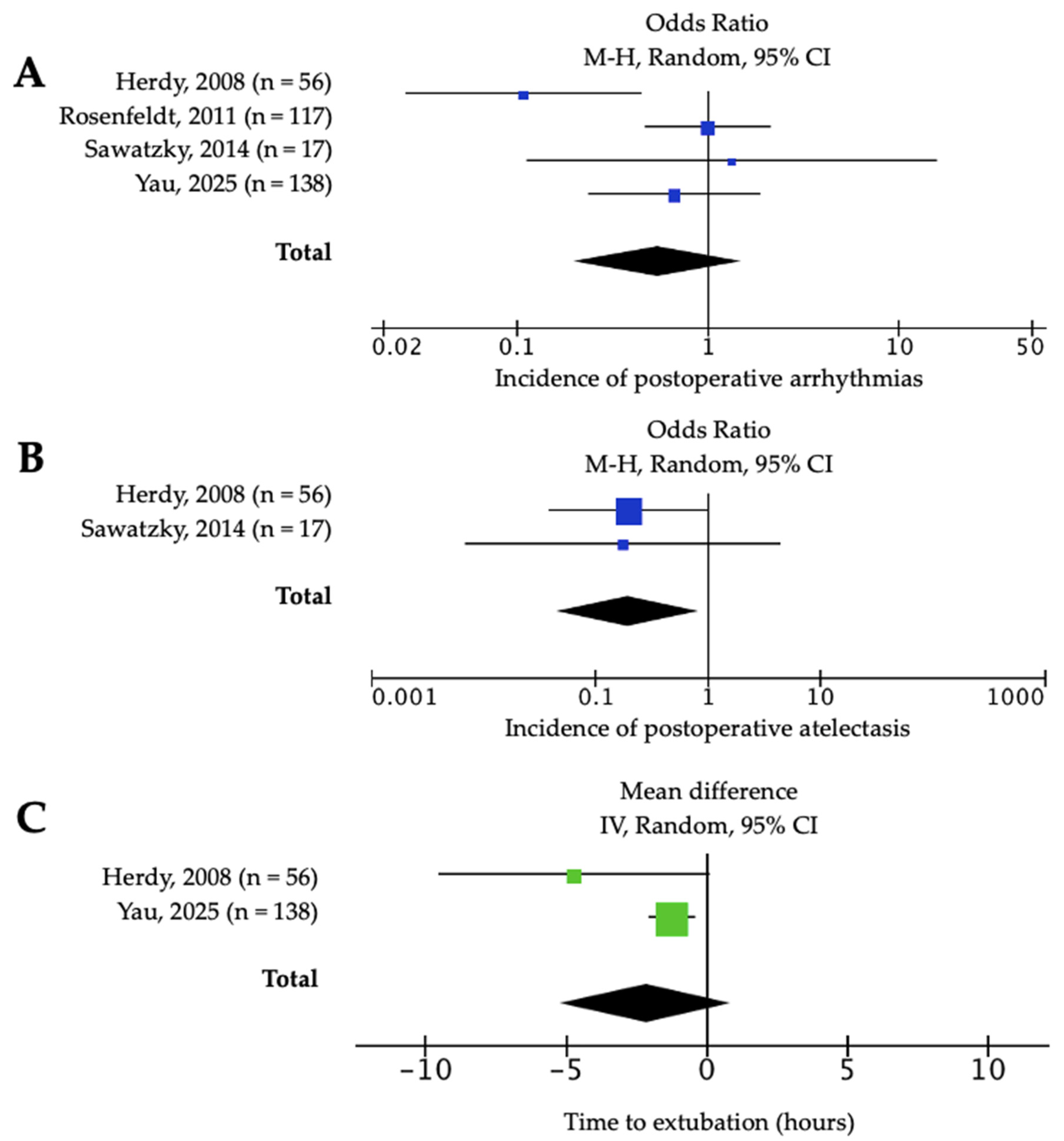
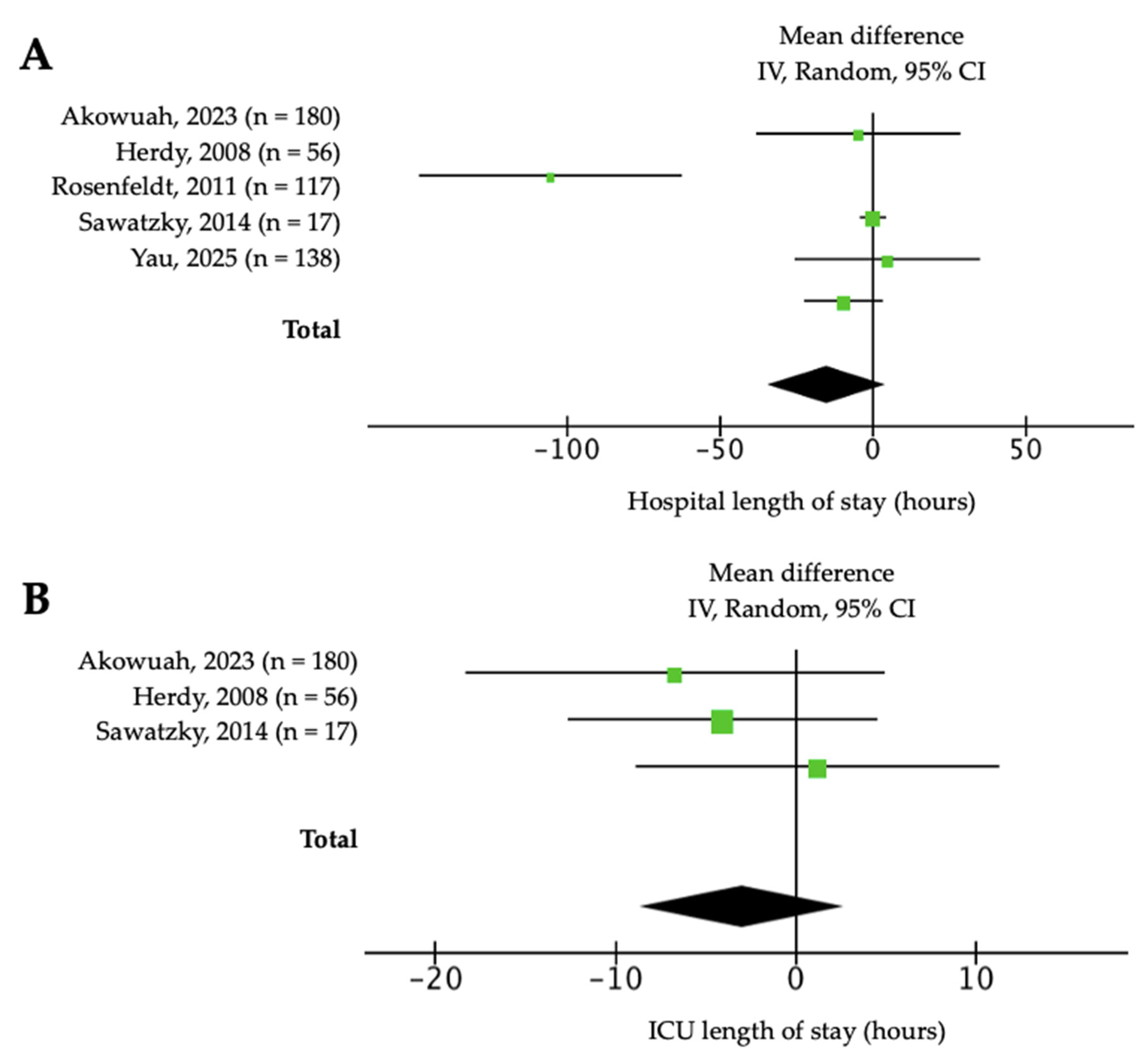
3.6. Postoperative Complications
3.7. Quality of Life
4. Discussion
4.1. Functional Capacity
4.2. Frailty
4.3. Sarcopenia and Dynapenia
4.4. Postoperative Complications
4.5. Quality of Life
4.6. Proposed Clinical Model of Prehabilitation in Cardiac Surgery and Future Perspectives
4.7. Strengths and Limitations
4.8. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Santa-Mina, D.; Clarke, H.; Ritvo, P.; Leung, Y.W.; Matthew, A.G.; Katz, J.; Trachtenberg, J.; Alibhai, S.M.H. Effect of total-body prehabilitation on postoperative outcomes: A systematic review and meta-analysis. Physiotherapy 2014, 100, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Carli, F.; Scheede-Bergdahl, C. Prehabilitation to enhance perioperative care. Anesthesiol. Clin. 2015, 33, 17–33. [Google Scholar] [CrossRef] [PubMed]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s guide to cardiopulmonary exercise testing in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef] [PubMed]
- Herdy, A.H.; Marcchi, P.L.; Vila, A.; Tavares, C.; Collaço, J.; Niebauer, J.; Ribeiro, J.P. Pre- and postoperative cardiopulmonary rehabilitation in hospitalized patients undergoing coronary artery bypass surgery: A randomized controlled trial. Am. J. Phys. Med. Rehabil. 2008, 87, 714–719. [Google Scholar] [CrossRef]
- Rosenfeldt, F.; Braun, L.; Spitzer, O.; Bradley, S.; Shepherd, J.; Bailey, M.; van der Merwe, J.; Leong, J.-Y.; Esmore, D. Physical conditioning and mental stress reduction—A randomised trial in patients undergoing cardiac surgery. BMC Complement. Altern. Med. 2011, 11, 20. [Google Scholar] [CrossRef]
- Sawatzky, J.V.; Kehler, D.S.; Ready, A.E.; Lerner, N.; Boreskie, S.; Lamont, D.; Luchik, D.; Arora, R.C.; A Duhamel, T. Prehabilitation program for elective coronary artery bypass graft surgery patients: A pilot randomized controlled study. Clin. Rehabil. 2014, 28, 648–657. [Google Scholar] [CrossRef]
- Waite, I.; Deshpande, R.; Baghai, M.; Massey, T.; Wendler, O.; Greenwood, S. Home-based preoperative rehabilitation (PREHAB) to improve physical function and reduce hospital length of stay for frail patients undergoing coronary artery bypass graft and valve surgery. J. Cardiothorac. Surg. 2017, 12, 91. [Google Scholar] [CrossRef]
- Steinmetz, C.; Bjarnason-Wehrens, B.; Baumgarten, H.; Walther, T.; Mengden, T.; Walther, C. Prehabilitation in patients awaiting elective coronary artery bypass graft surgery: Effects on functional capacity and quality of life: A randomized controlled trial. Clin. Rehabil. 2020, 34, 1256–1267. [Google Scholar] [CrossRef]
- Akowuah, E.F.; Wagnild, J.M.; Bardgett, M.; Prichard, J.G.; Mathias, A.; Harrison, S.L.; Ogundimu, E.O.; Hancock, H.C.; Maier, R.H. A randomised controlled trial of prehabilitation in patients undergoing elective cardiac surgery (PrEPS Trial). Anaesthesia 2023, 78, 1120–1128. [Google Scholar] [CrossRef]
- López-Hernández, A.; Gimeno-Santos, E.; Navarro-Ripoll, R.; Arguis, M.J.; Romano-Andrioni, B.; López-Baamonde, M.; Teres, S.; la Garza, M.S.-D.; Martinez-Palli, G. Differential response to preoperative exercise training in patients candidates to cardiac valve replacement. BMC Anesthesiol. 2024, 24, 280. [Google Scholar] [CrossRef]
- Sahar, W.; Waseem, M.; Riaz, M.; Nazeer, N.; Ahmad, M.; Haider, Z. Effects of prehabilitation resistance training in mild to moderate clinically frail patients awaiting coronary artery bypass graft surgery. J. Investig. Med. 2024, 72, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Yau, D.K.W.; Ng, F.F.; Underwood, M.J.; Joynt, G.M.; Lee, A.; Wong, W.T.; Wong, S.S. Effect of exercise prehabilitation on quality of recovery after cardiac surgery: A randomised clinical trial. Br. J. Anaesth. 2025, 134, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, C.; Bjarnason-Wehrens, B.; Walther, T.; Schaffland, T.F.; Walther, C. Efficacy of prehabilitation before cardiac surgery: A systematic review and meta-analysis. Am. J. Phys. Med. Rehabil. 2023, 102, 323–330. [Google Scholar] [CrossRef]
- Yau, D.K.W.; Underwood, M.J.; Joynt, G.M.; Lee, A. Effect of preparative rehabilitation on recovery after cardiac surgery: A systematic review. Ann. Phys. Rehabil. Med. 2021, 64, 101391. [Google Scholar] [CrossRef]
- Jones, J.M.; Loubani, M.; Grant, S.W.; Goodwin, A.T.; Trivedi, U.; Kendall, S.; Jenkins, D.P. Cardiac surgery in older patients: Hospital outcomes during a 15-year period. Interact. Cardiovasc. Thorac. Surg. 2022, 34, 532–538. [Google Scholar] [CrossRef]
- Khan, M.S.; Anker, S.D.; Friede, T.; Jankowska, E.A.; Metra, M.; Piña, I.L.; Coats, A.J.; Rosano, G.; Roubert, B.; Goehring, U.-M.; et al. Minimal clinically important differences in 6-minute walk test in patients with HFrEF and iron deficiency. J. Card. Fail. 2023, 29, 760–770. [Google Scholar] [CrossRef]
- Keeratichananont, W.; Thanadetsuntorn, C.; Keeratichananont, S. Value of preoperative 6-minute walk test for predicting postoperative pulmonary complications. Ther. Adv. Respir. Dis. 2016, 10, 18–25. [Google Scholar] [CrossRef]
- Hartog, J.; Dijkstra, S.; Dieperink, W.; Hoekstra, T.; Fleer, J.; Van-der-Woude, L.H.V.; Van-der-Harst, P.; Nijsten, M.; Mariani, M.A.; Blokzijl, F. Muscle strength trajectories and their association with postoperative health-related quality of life in patients undergoing coronary artery bypass grafting surgery: A prospective cohort study. BMC Cardiovasc. Disord. 2023, 23, 20. [Google Scholar] [CrossRef]
- Moran, J.; Guinan, E.; McCormick, P.; Larkin, J.; Mockler, D.; Hussey, J.; Moriarty, J.; Wilson, F. The ability of prehabilitation to influence postoperative outcome after intra-abdominal operation: A systematic review and meta-analysis. Surgery 2016, 160, 1189–1201. [Google Scholar] [CrossRef]
- Xavier, D.M.; Abreu, R.A.L.; Corrêa, F.G.; Silva, W.T.; Silva, S.N.; Galvao, E.L.; Junior, M.N.G. Effects of respiratory muscle training in post-COVID-19 patients: A systematic review and meta-analysis of randomized controlled trials. BMC Sports Sci. Med. Rehabil. 2024, 16, 49. [Google Scholar] [CrossRef]
- Hurtado-Borrego, J.C.; Monteagudo-Santamaría, M.; Martínez-González-Moro, I.; Martínez-Bermúdez, C.M. Perfil de fragilidad asociado a factores de riesgo cardiovascular de pacientes candidatos a cirugía cardíaca en un programa de prehabilitación. Cir. Cardiov. 2025, 32, 119–124. [Google Scholar] [CrossRef]
- Nakano, M.; Nomura, Y.; Suffredini, G.; Bush, B.; Tian, J.; Yamaguchi, A.; Walston, J.; Hasan, R.; Mandal, K.; Schena, S.; et al. Functional outcomes of frail patients after cardiac surgery: An observational study. Anesth. Analg. 2020, 130, 1534–1544. [Google Scholar] [CrossRef]
- Clark, B.C.; Manini, T.M. Sarcopenia ≠ dynapenia. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Narici, M.V.; Lauretani, F.; Nouvenne, A.; Colizzi, E.; Mantovani, M.; Corsonello, A.; Landi, F.; Meschi, T.; Maggio, M. Assessing sarcopenia with vastus lateralis muscle ultrasound: An operative protocol. Aging Clin. Exp. Res. 2018, 30, 1437–1443. [Google Scholar] [CrossRef] [PubMed]
- Dent, E.; Morley, J.E.; Cruz-Jentoft, A.J.; Arai, H.; Kritchevsky, S.B.; Guralnik, J.; Bauer, J.M.; Pahor, M.; Clark, B.C.; Cesari, M.; et al. International Clinical Practice Guidelines for Sarcopenia (ICFSR): Screening, diagnosis and management. J. Nutr. Health Aging 2018, 22, 1148–1161. [Google Scholar] [CrossRef]
- Steinmtez, C.; Krause, L.; Sulejmanovic, S.; Kaumkötter, S.; Mengden, T.; Grefe, C.; Knoglinger, E.; Reiss, N.; Brixius, K.; Bjarnason-Wehrens, B. The prevalence and impact of sarcopenia in older cardiac patients undergoing inpatient cardiac rehabilitation—Results from a prospective, observational cohort pre-study. BMC Geriatr. 2024, 94. [Google Scholar] [CrossRef]
- Wang, J.; Li, H.; Yan, W.; Xue, N.; Yin, J.; Yin, S. Prehabilitation interventions for cardiac surgery to prevent postoperative pulmonary complications: Systematic review and meta-analysis. Iran. J. Public Health 2024, 53, 2167–2179. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Jaffer, A.; Yang, K.; Ebrahim, A.; Brown, A.N.; EL-Andari, R.; Dokollari, A.; Gregory, A.J.; Adams, C.; Kent, W.D.T.; Fatehi Hassanabad, A. Optimizing recovery in cardiac surgery: A narrative review of enhanced recovery after surgery protocols and clinical outcomes. Med. Sci. 2025, 13, 128. [Google Scholar] [CrossRef]
- Praz, F.; Borger, M.A.; Lanz, J.; Marin-Cuartas, M.; Abreu, A.; Adamo, M.; Marsan, N.A.; Barili, F.; Bonaros, N.; Cosyns, B.; et al. 2025 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2025, 46, 489–599. [Google Scholar] [CrossRef]
- Gao, W.; Li, H.; Chen, Y.; Zhang, Y.; Zhang, M.; Jin, J. Effectiveness of a short-term multimodal prehabilitation program in adult patients awaiting selective cardiac surgery: Protocol for an open-label, pilot, randomized controlled trial. Front. Cardiovasc. Med. 2023, 10, e039885. [Google Scholar] [CrossRef] [PubMed]
- Goodlin, G.T.; Steinbeck, L.; Bergfeld, D.; Haselhorst, A. Adaptive cycling: Classification, adaptations, and biomechanics. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Neto, M.; Durães, A.R.; Conceição, L.S.R.; Correia-dos-Reis, H.; Neves, V.R.; Martinez, B.P.; Carvalho, V.O. High intensity interval training versus moderate intensity continuous training on exercise capacity and quality of life in patients with coronary artery disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1696–1707. [Google Scholar] [CrossRef]
- Maroto-Izquierdo, S.; Bautista, I.J.; Pérez-Guerrero, A.; Redondo-Delgado, P.; Jauregui-Fajardo, I.; Simó, V.; Aldecoa, C. Effects of Prehabilitation Concurrent Exercise on Functional Capacity in Colorectal Cancer Patients: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 1119. [Google Scholar] [CrossRef]
- Cursino-de-Moura, J.F.; Oliveira, C.B.; Coelho-Figueira, A.P.F.; Elkins, M.R.; Pacagnelli, F.L. Preoperative respiratory muscle training reduces the risk of pulmonary complications and the length of hospital stay after cardiac surgery: A systematic review. J. Physiother. 2024, 70, 16–24. [Google Scholar] [CrossRef]
- Katsura, M.; Kuriyama, A.; Takeshima, T.; Fukuhara, S.; Furukawa, T.A. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst. Rev. 2015, 10, CD010356. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weekset, L.; et al. PRISMA Extension for Scoping Reviews (PRISMAScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
| Authors | Sample Size (n) | Country | Age (Years) | Sex (% Male) | CV Risk Factors | Surgery Type | Main Outcomes |
|---|---|---|---|---|---|---|---|
| Herdy et al. (2008) [4] | 56 | Brazil | 61 ± 10 | 72% | Smoking | CABG | Improvement in 6MWT after prehabilitation |
| Rosenfeldt et al. (2011) [5] | 117 | Australia | 65.2 ± 6 | 74% | DM | CABG (61%), VD (39%) | Need for longer-lasting prehabilitation programs to impact quality of life |
| Sawatzky et al. (2014) [6] | 17 | Canada | 64 ± 8 | 80% | HTN, DM, DLP | CABG | Significant improvement in functional capacity after prehabilitation (6MWT, gait speed test), as well as greater adherence to physical exercise. No differences in postoperative complications |
| Waite et al. (2017) [7] | 20 | England | >65 | Not reported | Not reported | CABG and VD | Significant improvement in functional capacity (6MWT, SPPB) and frailty status (CFS reduction) |
| Steinmetz et al. (2020) [8] | 203 | Germany | 67.1 ± 8 | Not reported | HTN, DM, DLP, smoking | CABG | Significant improvement in functional capacity and quality of life after prehabilitation (6MWT, TUGT) |
| Akowuah et al. (2023) [9] | 180 | England | 50–70 | 82% | Not reported | CABG (56.7%), AVD (41.7%), MVD (15.4%), TVD (1.1%), aortic pathology (10%), others (5%) | No differences in functional capacity improvement after prehabilitation (only in those with dynapenia). Improvement observed in inspiratory muscle strength |
| López-Hernández et al. (2024) [10] | 68 | Spain | 71 ± 10 | 69% | Not reported | Aortic VD (58.8%), mitral VD (42.2%) | Significant improvement in functional capacity in 6MWT, handgrip strength test, and endurance time (ET) on cycle ergometer after prehabilitation |
| Sahar et al. (2024) [11] | 74 | Pakistan | 54 ± 6 | 83% | DM, smoking | CABG | Improved surgical outcomes after strength training. No significant differences in frailty status |
| Yau et al. (2025) [12] | 138 | China | 64 ± 10 | 69% | DM | CABG (53%), VD (47%) | Improvement in functional capacity (6MWT) without an increase in adverse events after surgery |
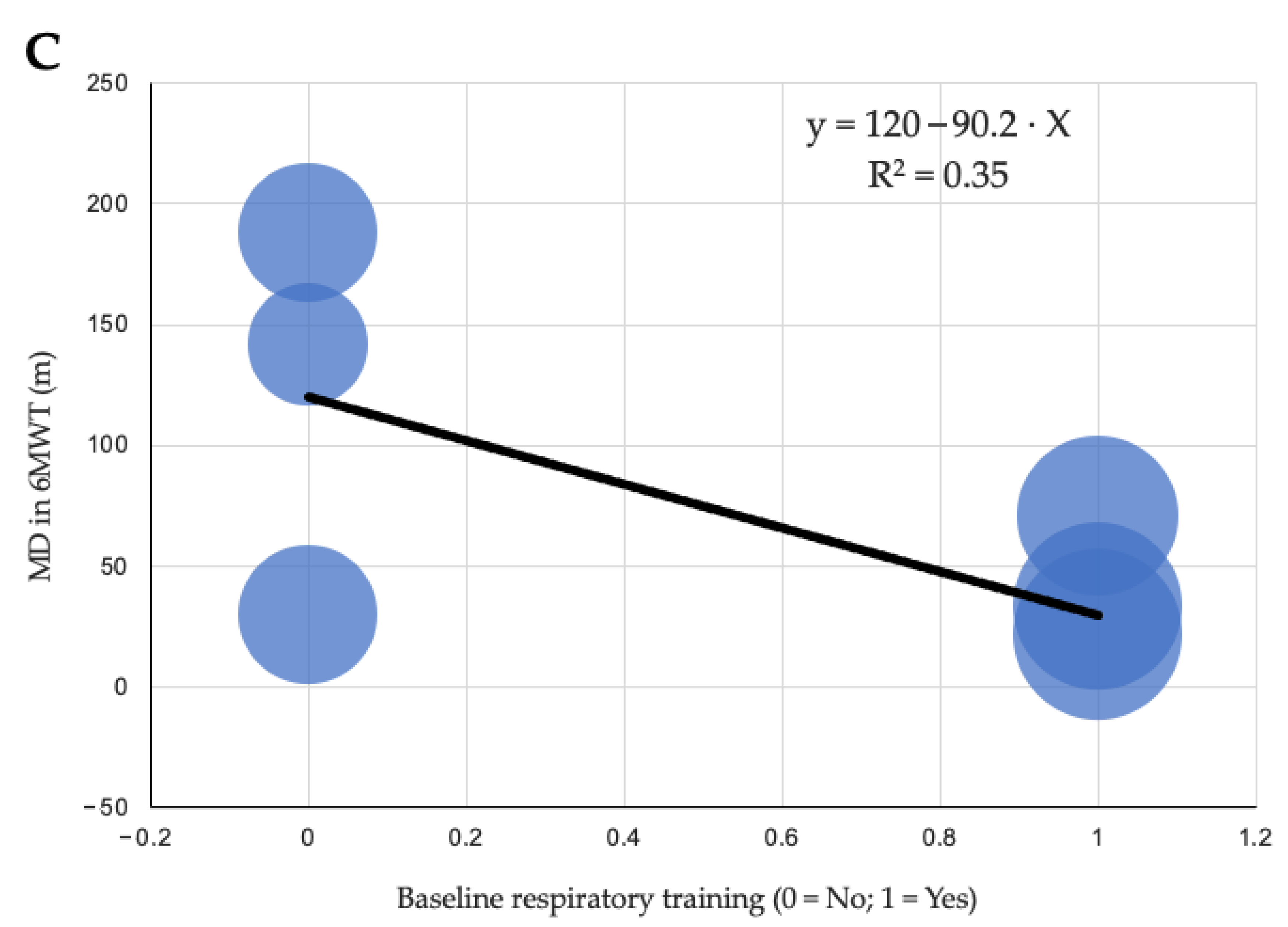
| Model | Participants | β Coefficient | 95% CI | Adjusted R2 | p Value |
|---|---|---|---|---|---|
| Program duration (weeks) | 873 | 14.76 | [−9.5, 39] | 0.07 | 0.287 |
| Age (years) | 873 | −9.26 | [−20.6, 2.1] | 0.21 | 0.169 |
| Respiratory training (yes vs. no) | 873 | −90.25 | [−176.9, −3.6] | 0.352 | 0.094 |
| Equipment | Intensity | Duration | Progression | Exercises | |
|---|---|---|---|---|---|
| Aerobic | Cycle ergometer | Moderate
| 25–30 min | Increase time by 2–3 min per week | MICT (standard) or HIIT (for selected patients with good tolerance) |
| Strength | Dumbbells, ankle weights, elastic bands | 50–60% 1RM | 2–3 sets of 8–12 reps | Increase load by 5–10% every 1–2 weeks |
|
| Respiratory | Incentive spirometer | 30–50% of initial MIP | 3 sets of 10 deep inspirations, twice daily | Increase resistance by 5–10% per week | Maximal inspirations against resistance, diaphragmatic breathing with resistance, lower costal expansions |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hurtado-Borrego, J.C.; Bayonas-Ruiz, A.; Bonacasa, B. Exercise-Based Prehabilitation Before Cardiac Surgery: A Systematic Review, Meta-Analysis, Meta-Regression, and Proposal for a Clinical Implementation Model. J. Clin. Med. 2025, 14, 8195. https://doi.org/10.3390/jcm14228195
Hurtado-Borrego JC, Bayonas-Ruiz A, Bonacasa B. Exercise-Based Prehabilitation Before Cardiac Surgery: A Systematic Review, Meta-Analysis, Meta-Regression, and Proposal for a Clinical Implementation Model. Journal of Clinical Medicine. 2025; 14(22):8195. https://doi.org/10.3390/jcm14228195
Chicago/Turabian StyleHurtado-Borrego, Juan Carlos, Adrián Bayonas-Ruiz, and Bárbara Bonacasa. 2025. "Exercise-Based Prehabilitation Before Cardiac Surgery: A Systematic Review, Meta-Analysis, Meta-Regression, and Proposal for a Clinical Implementation Model" Journal of Clinical Medicine 14, no. 22: 8195. https://doi.org/10.3390/jcm14228195
APA StyleHurtado-Borrego, J. C., Bayonas-Ruiz, A., & Bonacasa, B. (2025). Exercise-Based Prehabilitation Before Cardiac Surgery: A Systematic Review, Meta-Analysis, Meta-Regression, and Proposal for a Clinical Implementation Model. Journal of Clinical Medicine, 14(22), 8195. https://doi.org/10.3390/jcm14228195








