Multicenter European Data of Anatomical Parameters of the Anterior Eye Segment Measured with an Optical Biometer
Abstract
1. Introduction
2. Materials and Methods
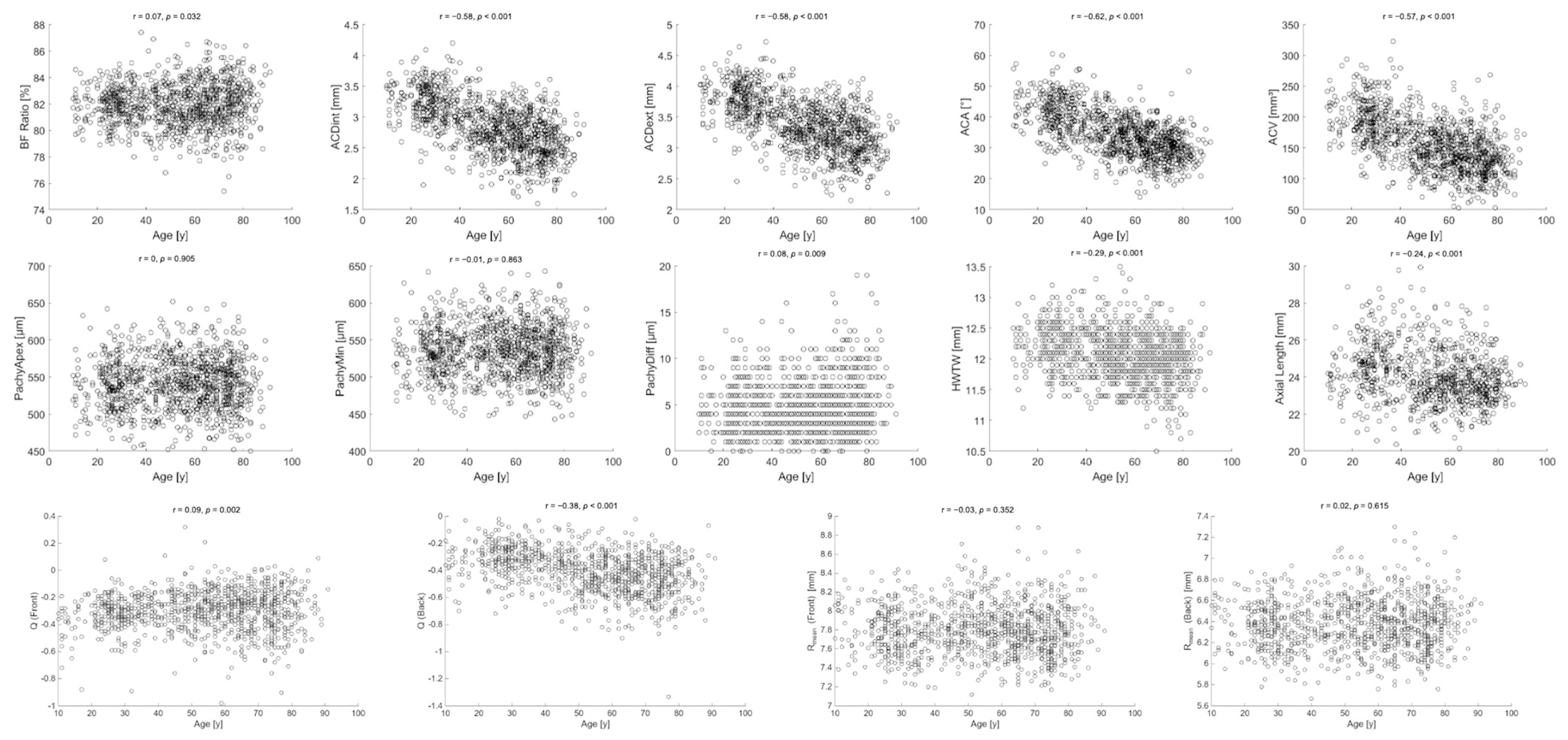
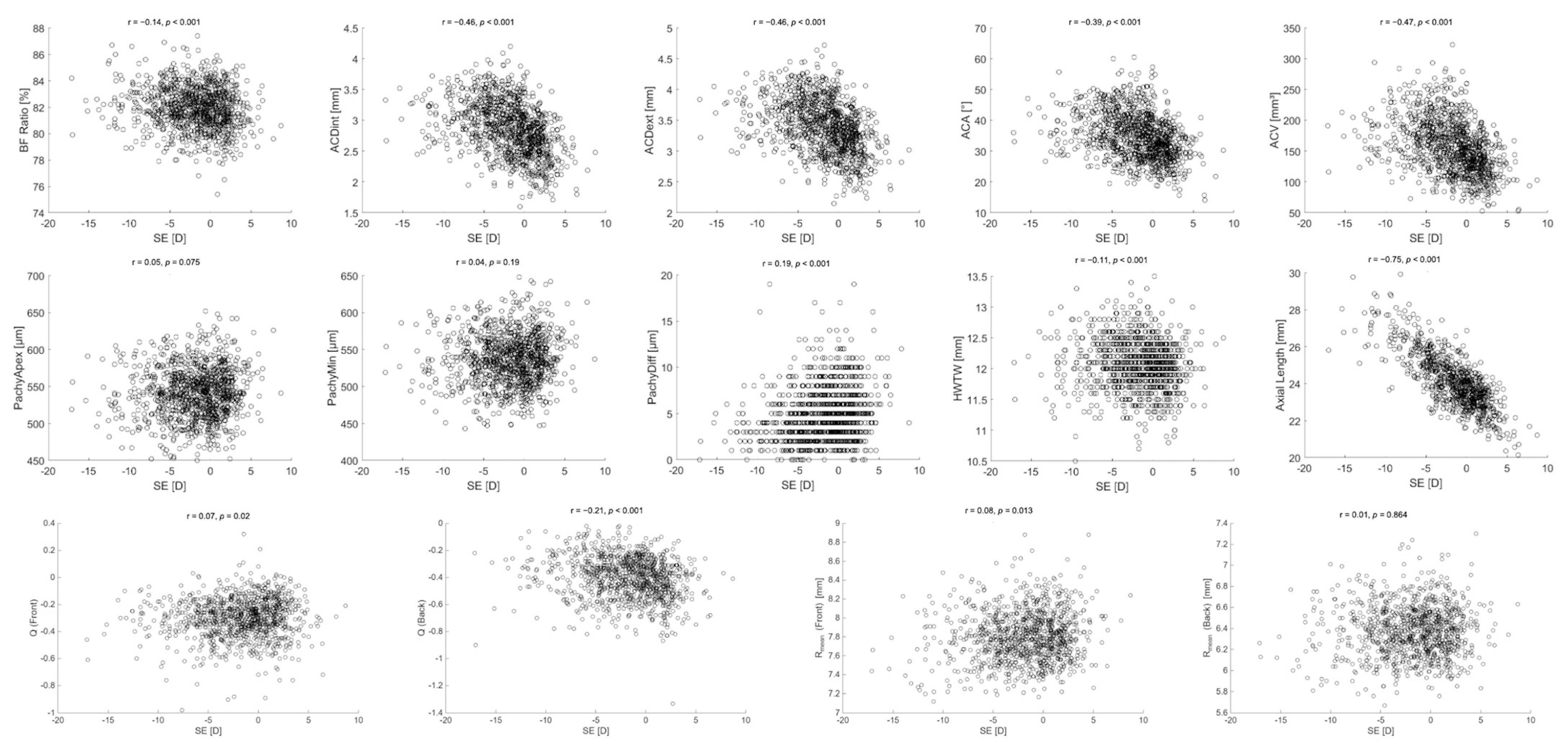
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tañá-Rivero, P.; Aguilar-Córcoles, S.; Tello-Elordi, C.; Pastor-Pascual, F.; Montés-Micó, R. Agreement between 2 Swept-Source OCT Biometers and a Scheimpflug Partial Coherence Interferometer. J. Cataract Refract. Surg. 2021, 47, 488–495. [Google Scholar] [CrossRef]
- Fotedar, R.; Wang, J.J.; Burlutsky, G.; Morgan, I.G.; Rose, K.; Wong, T.Y.; Mitchell, P. Distribution of Axial Length and Ocular Biometry Measured Using Partial Coherence Laser Interferometry (IOL Master) in an Older White Population. Ophthalmology 2010, 117, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A.; Markwell, E.L.; Kasthurirangan, S.; Pope, J.M.; Smith, G.; Swann, P.G. Age-Related Changes in Optical and Biometric Characteristics of Emmetropic Eyes. J. Vis. 2008, 8, 29. [Google Scholar] [CrossRef] [PubMed]
- Olsen, T.; Arnarsson, A.; Sasaki, H.; Sasaki, K.; Jonasson, F. On the Ocular Refractive Components: The Reykjavik Eye Study. Acta Ophthalmol. Scand. 2007, 85, 361–366. [Google Scholar] [CrossRef]
- Lam, A.K.C.; Tse, J.S.H. Pentacam Anterior Chamber Parameters in Young and Middle-Aged Chinese. Clin. Exp. Optom. 2013, 96, 85–91. [Google Scholar] [CrossRef]
- Wong, T.Y.; Foster, P.J.; Ng, T.P.; Tielsch, J.M.; Johnson, G.J.; Seah, S.K.L. Variations in Ocular Biometry in an Adult Chinese Population in Singapore: The Tanjong Pagar Survey. Investig. Ophthalmol. Vis. Sci. 2001, 42, 73–80. [Google Scholar]
- Gilani, F.; Cortese, M.; Ambrósio, R.R.; Lopes, B.; Ramos, I.; Harvey, E.M.; Belin, M.W. Comprehensive Anterior Segment Normal Values Generated by Rotating Scheimpflug Tomography. J. Cataract Refract. Surg. 2013, 39, 1707–1712. [Google Scholar] [CrossRef]
- Orucoglu, F.; Akman, M.; Onal, S. Analysis of Age, Refractive Error and Gender Related Changes of the Cornea and the Anterior Segment of the Eye with Scheimpflug Imaging. Contact Lens Anterior Eye 2015, 38, 345–350. [Google Scholar] [CrossRef]
- Deshmukh, R.; Shrivastava, A.K.; Vaddavalli, P.K. Prevailing Practice Patterns in Keratoconus among Indian Ophthalmologists. Indian J. Ophthalmol. 2023, 71, 3229–3234. [Google Scholar] [CrossRef] [PubMed]
- Motlagh, M.N.; Moshirfar, M.; Murri, M.S.; Skanchy, D.F.; Momeni-Moghaddam, H.; Ronquillo, Y.C.; Hoopes, P.C. Pentacam® Corneal Tomography for Screening of Refractive Surgery Candidates: A Review of the Literature, Part I. Med. Hypothesis Discov. Innov. Ophthalmol. 2019, 8, 177–203. [Google Scholar]
- Boyd, B.M.; Bai, J.; Borgstrom, M.; Belin, M.W. Comparison of Chinese and North American Tomographic Parameters and the Implications for Refractive Surgery Screening. Asia-Pac. J. Ophthalmol. 2020, 9, 117–125. [Google Scholar] [CrossRef] [PubMed]
- OCULUS Pentacam® AXL Wave. Available online: https://www.pentacam.com/axl-wave/public/index.php (accessed on 21 July 2025).
- Deng, M.; Lan, L.; Chen, T.; Zhang, M.; Chen, J.; Jing, Q.; Jiang, Y. Evaluation of the B/F Ratio Distribution of Cataract Patients Without Corneal Abnormalities and Its Effect on Ocular Parameters. Clin. Investig. Med. 2021, 44, E46–E54. [Google Scholar] [CrossRef]
- Gharieb Ibrahim, H.M.; Gharieb, H.M.; Othman, I.S. Angle κ Measurement and Its Correlation with Other Ocular Parameters in Normal Population by a New Imaging Modality. Optom. Vis. Sci. 2022, 99, 580–588. [Google Scholar] [CrossRef]
- Hoffmann, P.C.; Hütz, W.W. Analysis of Biometry and Prevalence Data for Corneal Astigmatism in 23 239 Eyes. J. Cataract Refract. Surg. 2010, 36, 1479–1485. [Google Scholar] [CrossRef]
- Fam, H.-B.; Lim, K.-L. Validity of the Keratometric Index: Large Population-Based Study. J. Cataract Refract. Surg. 2007, 33, 686–691. [Google Scholar] [CrossRef]
- Tang, M.; Chen, A.; Li, Y.; Huang, D. Corneal Power Measurement with Fourier-Domain Optical Coherence Tomography. J. Cataract Refract. Surg. 2010, 36, 2115–2122. [Google Scholar] [CrossRef]
- Savini, G.; Hoffer, K.J.; Lomoriello, D.S.; Ducoli, P. Simulated Keratometry Versus Total Corneal Power by Ray Tracing: A Comparison in Prediction Accuracy of Intraocular Lens Power. Cornea 2017, 36, 1368–1372. [Google Scholar] [CrossRef]
- Hasegawa, A.; Kojima, T.; Yamamoto, M.; Kato, Y.; Tamaoki, A.; Ichikawa, K. Impact of the Anterior-Posterior Corneal Radius Ratio on Intraocular Lens Power Calculation Errors. Clin. Ophthalmol. 2018, 12, 1549–1558. [Google Scholar] [CrossRef]
- Huseynova, T.; Abdulaliyeva, F.; Lanza, M. Comparison of Scheimpflug Imaging Parameters between Steep and Keratoconic Corneas of Caucasian Eyes. Clin. Ophthalmol. 2016, 10, 603–608. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ambrósio, R.; Lopes, B.T.; Faria-Correia, F.; Salomão, M.Q.; Bühren, J.; Roberts, C.J.; Elsheikh, A.; Vinciguerra, R.; Vinciguerra, P. Integration of Scheimpflug-Based Corneal Tomography and Biomechanical Assessments for Enhancing Ectasia Detection. J. Refract. Surg. 2017, 33, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Almorín-Fernández-Vigo, I.; Sánchez-Guillén, I.; Fernández-Vigo, J.I.; Macarro-Merino, A.; Kudsieh, B.; Fernández-Vigo, C.; Fernández-Vigo, J.A. Normative Pentacam Anterior and Posterior Corneal Elevation Measurements: Effects of Age, Sex, Axial Length and White-to-White. Int. Ophthalmol. 2019, 39, 1955–1963. [Google Scholar] [CrossRef]
- Fu, T.; Song, Y.-W.; Chen, Z.-Q.; He, J.-W.; Qiao, K.; Sun, X.-F.; Zhang, H.; Wang, J.-M. Ocular Biometry in the Adult Population in Rural Central China: A Population-Based, Cross-Sectional Study. Int. J. Ophthalmol. 2015, 8, 812–817. [Google Scholar] [CrossRef]
- Rabsilber, T.M.; Khoramnia, R.; Auffarth, G.U. Anterior Chamber Measurements Using Pentacam Rotating Scheimpflug Camera. J. Cataract Refract. Surg. 2006, 32, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.K.; Pfeiffer, N.; Nickels, S.; Schulz, A.; Höhn, R.; Wild, P.S.; Binder, H.; Münzel, T.; Beutel, M.E.; Vossmerbaeumer, U. Distribution of Anterior Chamber Angle Width and Correlation with Age, Refraction, and Anterior Chamber Depth-The Gutenberg Health Study. Investig. Ophthalmol. Vis. Sci. 2016, 57, 3740–3746. [Google Scholar] [CrossRef] [PubMed]
- Sedaghat, M.R.; Mohammad Zadeh, V.; Fadakar, K.; Kadivar, S.; Abrishami, M. Normative Values and Contralateral Comparison of Anterior Chamber Parameters Measured by Pentacam and Its Correlation with Corneal Biomechanical Factors. Saudi J. Ophthalmol. 2017, 31, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Yang, W.; Yang, C.; Sun, Q. Comparison of Anterior Chamber Depth Measured by Three Different Anterior Segment Analysis Systems. Photodiagn. Photodyn. Ther. 2025, 51, 104471. [Google Scholar] [CrossRef]
- He, M.; Huang, W.; Zheng, Y.; Alsbirk, P.H.; Foster, P.J. Anterior Chamber Depth in Elderly Chinese: The Liwan Eye Study. Ophthalmology 2008, 115, 1286–1290.e2. [Google Scholar] [CrossRef]
- Fontana, S.T.; Brubaker, R.F. Volume and Depth of the Anterior Chamber in the Normal Aging Human Eye. Arch. Ophthalmol. 1980, 98, 1803–1808. [Google Scholar] [CrossRef]
- Chen, H.-B.; Kashiwagi, K.; Yamabayashi, S.; Kinoshita, T.; Ou, B.; Tsukahara, S. Anterior Chamber Angle Biometry: Quadrant Variation, Age Change and Sex Difference. Curr. Eye Res. 1998, 17, 120–124. [Google Scholar] [CrossRef]
- Roshdy, M.M.S.; Wahba, S.S.; Elkitkat, R.S.; Hakim, A.M.; Fikry, R.R. Effect of Age on Pentacam Keratoconus Indices. J. Ophthalmol. 2018, 2018, 2016564. [Google Scholar] [CrossRef]
- Vitályos, G.; Kolozsvári, B.L.; Németh, G.; Losonczy, G.; Hassan, Z.; Pásztor, D.; Fodor, M. Effects of Aging on Corneal Parameters Measured with Pentacam in Healthy Subjects. Sci. Rep. 2019, 9, 3419. [Google Scholar] [CrossRef] [PubMed]
- Pediatric Eye Disease Investigator Group. Central Corneal Thickness in Children. Arch. Ophthalmol. 2011, 129, 1132–1138. [Google Scholar] [CrossRef] [PubMed]
- Baboolal, S.O.; Smit, D.P. South African Eye Study (SAES): Ethnic Differences in Central Corneal Thickness and Intraocular Pressure. Eye 2018, 32, 749–756. [Google Scholar] [CrossRef]
- Da Silva, F.; Linhares, J.M.M.; Lira, M. What Intrinsic Factors Affect the Central Corneal Thickness? Ophthalmic Physiol. Opt. 2025, 45, 315–332. [Google Scholar] [CrossRef]
- Kim, J.T.; Cortese, M.; Belin, M.W.; Ambrosio, R., Jr.; Khachikian, S.S. Tomographic Normal Values for Corneal Elevation and Pachymetry in a Hyperopic Population. J. Clin. Exp. Ophthalmol. 2011, 2, 130. [Google Scholar] [CrossRef]
- Alsaif, N.K.; Al-Sharif, E.M.; Alsaif, S.K.; Mousa, A.; Al-Muammar, A.M. Corneal Elevation Indices and Pachymetry Values of Saudi Myopes Using Scheimpflug Imaging. Saudi Med. J. 2020, 41, 168–176. [Google Scholar] [CrossRef]
- Maraghechi, G.; Ojaghi, H.; Amani, F.; Najafi, A. A Comparative Study of Pentacam Indices in Various Types and Severities of Refractive Error in Candidates for Photorefractive Keratectomy (PRK) Surgery. J. Med. Life 2022, 15, 810–818. [Google Scholar] [CrossRef]
- Nilagiri, V.K.; Lee, S.S.-Y.; Lingham, G.; Charng, J.; Yazar, S.; Hewitt, A.W.; Griffiths, L.R.; Sanfilippo, P.G.; Tsai, T.-H.; Mackey, D.A. Distribution of Axial Length in Australians of Different Age Groups, Ethnicities, and Refractive Errors. Transl. Vis. Sci. Technol. 2023, 12, 14. [Google Scholar] [CrossRef]
- Chen, M.-J.; Liu, Y.-T.; Tsai, C.-C.; Chen, Y.-C.; Chou, C.-K.; Lee, S.-M. Relationship between Central Corneal Thickness, Refractive Error, Corneal Curvature, Anterior Chamber Depth and Axial Length. J. Chin. Med. Assoc. 2009, 72, 133–137. [Google Scholar] [CrossRef]
- Rozema, J.J.; Ní Dhubhghaill, S. Age-Related Axial Length Changes in Adults: A Review. Ophthalmic Physiol. Opt. 2020, 40, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Klyce, S.D.; Zheng, X.; Maeda, N.; Kuroda, T.; Ide, C. Gender- and Age-Related Differences in Corneal Topography. Cornea 2001, 20, 270. [Google Scholar] [CrossRef]
- Jiang, L.; Du, Z.; Sun, W.; Zhu, S.; Xiong, L.; Fang, X.; Zhou, J.; Zhang, Q.; Lei, X.; Zeng, Q.; et al. Associations between Corneal Curvature and Other Anterior Segment Biometrics in Young Myopic Adults. Sci. Rep. 2024, 14, 8305. [Google Scholar] [CrossRef]
- Placide, J.; Neves Da Silva, H.V.; McCabe, S.E.; Ronquillo, Y.C.; Moshirfar, M. Agreement of Anterior Segment Measurements between Four Diagnostic Imaging Devices in Myopic Patients. Expert Rev. Med. Devices 2021, 18, 1235–1243. [Google Scholar] [CrossRef] [PubMed]
- Chalkiadaki, E.; Gartaganis, P.S.; Ntravalias, T.; Giannakis, I.; Manousakis, E.; Karmiris, E. Agreement in Anterior Segment Measurements between Swept-Source and Scheimpflug-Based Optical Biometries in Keratoconic Eyes: A Pilot Study. Ther. Adv. Ophthalmol. 2022, 14, 25158414211063283. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Singh, P. Intraocular Lens Power Calculation. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Uhm, S.Y.; Do, T.P.; Lam, B.; Kheirkhah, A. Comparison of Corneal Pachymetry and Anterior Chamber Dimension Between Hispanic and Non-Hispanic Populations. Investig. Ophthalmol. Vis. Sci. 2022, 63, 2389-A0192. [Google Scholar]
- Wang, D.; Qi, M.; He, M.; Wu, L.; Lin, S. Ethnic Difference of the Anterior Chamber Area and Volume and Its Association with Angle Width. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3139–3144. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Board on Behavioral, Cognitive, and Sensory Sciences. The Rise in Myopia: Exploring Possible Contributors and Investigating Screening Practices, Policies, and Programs: Proceedings of a Workshop—In Brief; Casola, L., Ed.; The National Academies Collection: Reports Funded by National Institutes of Health; National Academies Press (US): Washington, DC, USA, 2024; ISBN 978-0-309-71789-2. [Google Scholar]

| Variable | Median (Min, Max) | Mean ± SD |
|---|---|---|
| Age (years) | 56.0 (10.0, 91.0) | 52.9 ± 19.5 |
| Spherical Equivalent (D) | −1.25 (−17.11, 8.72) | −1.81 ± 3.76 |
| BF Ratio (%) | 81.90 (75.40, 87.40) | 81.94 ± 1.60 |
| ACDint (mm) | 2.85 (1.60, 4.20) | 2.86 ± 0.43 |
| ACDext (mm) | 3.40 (2.15, 4.72) | 3.40 ± 0.43 |
| ACA (°) | 34.3 (14.1, 60.5) | 34.8 ± 7.4 |
| ACV (mm3) | 154.20 (52.70, 322.80) | 156.82 ± 43.16 |
| PachyApex (µm) | 541.0 (450.0, 652.0) | 541.3 ± 34.0 |
| PachyMin (µm) | 536.0 (443.0, 648.0) | 536.5 ± 34.0 |
| PachyDiff (µm) | 4.0 (0.0, 19.0) | 4.8 ± 2.9 |
| Axial Length (mm) | 23.94 (20.15, 29.93) | 24.11 ± 1.47 |
| HWTW (mm) | 12.10 (10.50, 13.50) | 12.06 ± 0.41 |
| Q (front) | −0.29 (−0.98, 0.32) | −0.30 ± 0.15 |
| Q (back) | −0.39 (−1.33, −0.02) | −0.41 ± 0.15 |
| Rmean (front) (mm) | 7.79 (7.12, 8.88) | 7.80 ± 0.26 |
| Rmean (back) (mm) | 6.38 (5.67, 7.30) | 6.38 ± 0.24 |
| Parameter | Female Median [95% CI], Min, Max | Male Median [95% CI], Min, Max | p-Value |
|---|---|---|---|
| Age (years) | 53.0 [16.0–81.8], Min = 10.0, Max = 91.0 | 60.0 [15.7–84.0], Min = 11.0, Max = 89.0 | <0.001 *** |
| SE (D) | −1.32 [−11.25–4.01], Min = −17.11, Max = 6.38 | −1.18 [−9.71–4.16], Min = −13.99, Max = 8.72 | 0.956 |
| BF Ratio (%) | 81.90 [78.70–84.78], Min = 76.80, Max = 86.90 | 82.00 [78.60–85.13], Min = 75.40, Max = 87.40 | 0.494 |
| ACDint (mm) | 2.83 [2.04–3.62], Min = 1.77, Max = 3.89 | 2.88 [1.98–3.72], Min = 1.60, Max = 4.20 | 0.026 * |
| ACDext (mm) | 3.37 [2.60–4.17], Min = 2.29, Max = 4.41 | 3.43 [2.56–4.25], Min = 2.15, Max = 4.72 | 0.018 * |
| ACA (°) | 34.1 [21.7–48.6], Min = 15.7, Max = 55.7 | 34.6 [22.5–51.0], Min = 14.1, Max = 60.5 | 0.144 |
| ACV (mm3) | 147.90 [82.22–238.38], Min = 52.70, Max = 283.40 | 157.80 [86.46–261.85], Min = 55.20, Max = 322.80 | <0.001 *** |
| PachyApex (µm) | 540.0 [477.0–605.8], Min = 452.0, Max = 642.0 | 542.0 [475.3–618.7], Min = 450.0, Max = 652.0 | 0.128 |
| PachyMin (µm) | 536.0 [473.2–602.8], Min = 447.0, Max = 642.0 | 537.0 [471.9–612.4], Min = 443.0, Max = 648.0 | 0.211 |
| PachyDiff (µm) | 4.0 [1.0–11.0], Min = 0.0, Max = 16.0 | 5.0 [1.0–12.0], Min = 0.0, Max = 19.0 | 0.006 ** |
| Axial Length (mm) | 23.65 [21.47–27.17], Min = 20.15, Max = 28.72 | 24.22 [21.96–27.72], Min = 20.71, Max = 29.93 | <0.001 *** |
| HWTW (mm) | 12.00 [11.26–12.70], Min = 10.50; Max = 13.50 | 12.20 [11.30–13.00] Min = 10.70; Max = 13.40 | <0.001 *** |
| Q (front) | −0.30 [−0.59–−0.06], Min = −0.98, Max = 0.32 | −0.28 [−0.64–−0.02], Min = −0.89, Max = 0.11 | 0.395 |
| Q (back) | −0.39 [−0.71–−0.11], Min = −1.33, Max = −0.03 | −0.39 [−0.76–−0.16]. Min = −0.87, Max = −0.02 | 0.347 |
| Rmean (front) (mm) | 7.75 [7.27–8.28], Min = 7.12, Max = 8.88 | 7.87 [7.43–8.40], Min = 7.17, Max = 8.88 | <0.001 *** |
| Rmean (back) (mm) | 6.32 [5.91–6.83], Min = 5.67, Max = 7.30 | 6.44 [6.00–6.90], Min = 5.76, Max = 7.24 | <0.001 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niknahad, A.; Son, H.-S.; Auffarth, G.U.; Blöck, L.; Savini, G.; Coutinho, C.P.; Fernández, J.; Łabuz, G. Multicenter European Data of Anatomical Parameters of the Anterior Eye Segment Measured with an Optical Biometer. J. Clin. Med. 2025, 14, 8192. https://doi.org/10.3390/jcm14228192
Niknahad A, Son H-S, Auffarth GU, Blöck L, Savini G, Coutinho CP, Fernández J, Łabuz G. Multicenter European Data of Anatomical Parameters of the Anterior Eye Segment Measured with an Optical Biometer. Journal of Clinical Medicine. 2025; 14(22):8192. https://doi.org/10.3390/jcm14228192
Chicago/Turabian StyleNiknahad, Ava, Hyeck-Soo Son, Gerd U. Auffarth, Louise Blöck, Giacomo Savini, Catarina P. Coutinho, Joaquín Fernández, and Grzegorz Łabuz. 2025. "Multicenter European Data of Anatomical Parameters of the Anterior Eye Segment Measured with an Optical Biometer" Journal of Clinical Medicine 14, no. 22: 8192. https://doi.org/10.3390/jcm14228192
APA StyleNiknahad, A., Son, H.-S., Auffarth, G. U., Blöck, L., Savini, G., Coutinho, C. P., Fernández, J., & Łabuz, G. (2025). Multicenter European Data of Anatomical Parameters of the Anterior Eye Segment Measured with an Optical Biometer. Journal of Clinical Medicine, 14(22), 8192. https://doi.org/10.3390/jcm14228192









