Trick or Treat(ment): Should We Still Fear Reperfusion Therapy in Anticoagulated Stroke Patients?—Comparable 90-Day Outcomes in a Propensity-Score-Matched Registry Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection and Measurements
2.3. Inclusion and Exclusion Criteria
2.4. Caliper-Matched Propensity Score Matching
2.5. Outcome Assessment
2.6. Statistical Analysis
2.7. Ethics Approval
3. Results
3.1. Baseline and Clinical Characteristics
3.2. Favorable Outcome
3.3. mRS-Shift
3.4. Mortality
3.5. Predictors of Outcome in the Matched Cohort
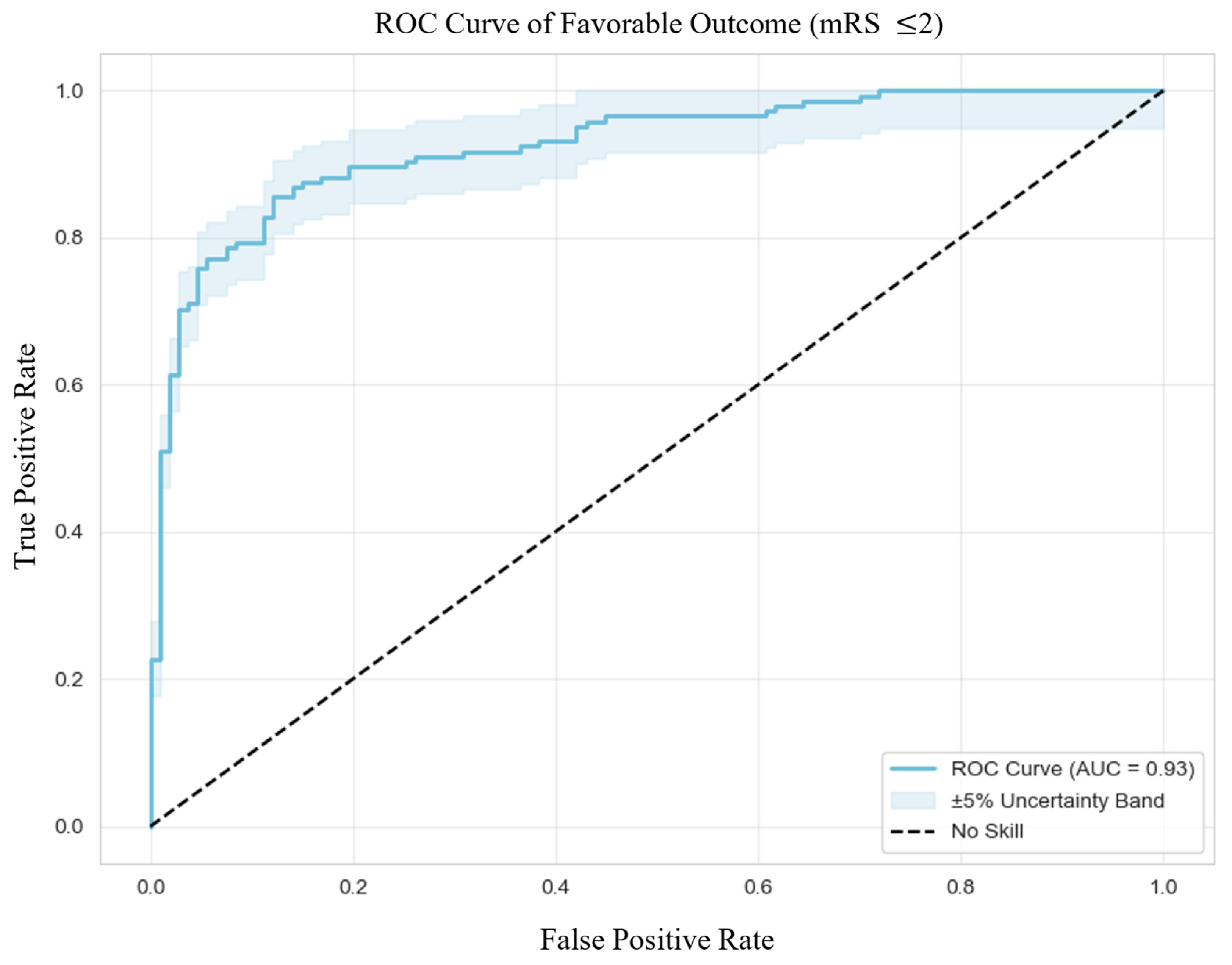
3.5.1. Favorable Outcome
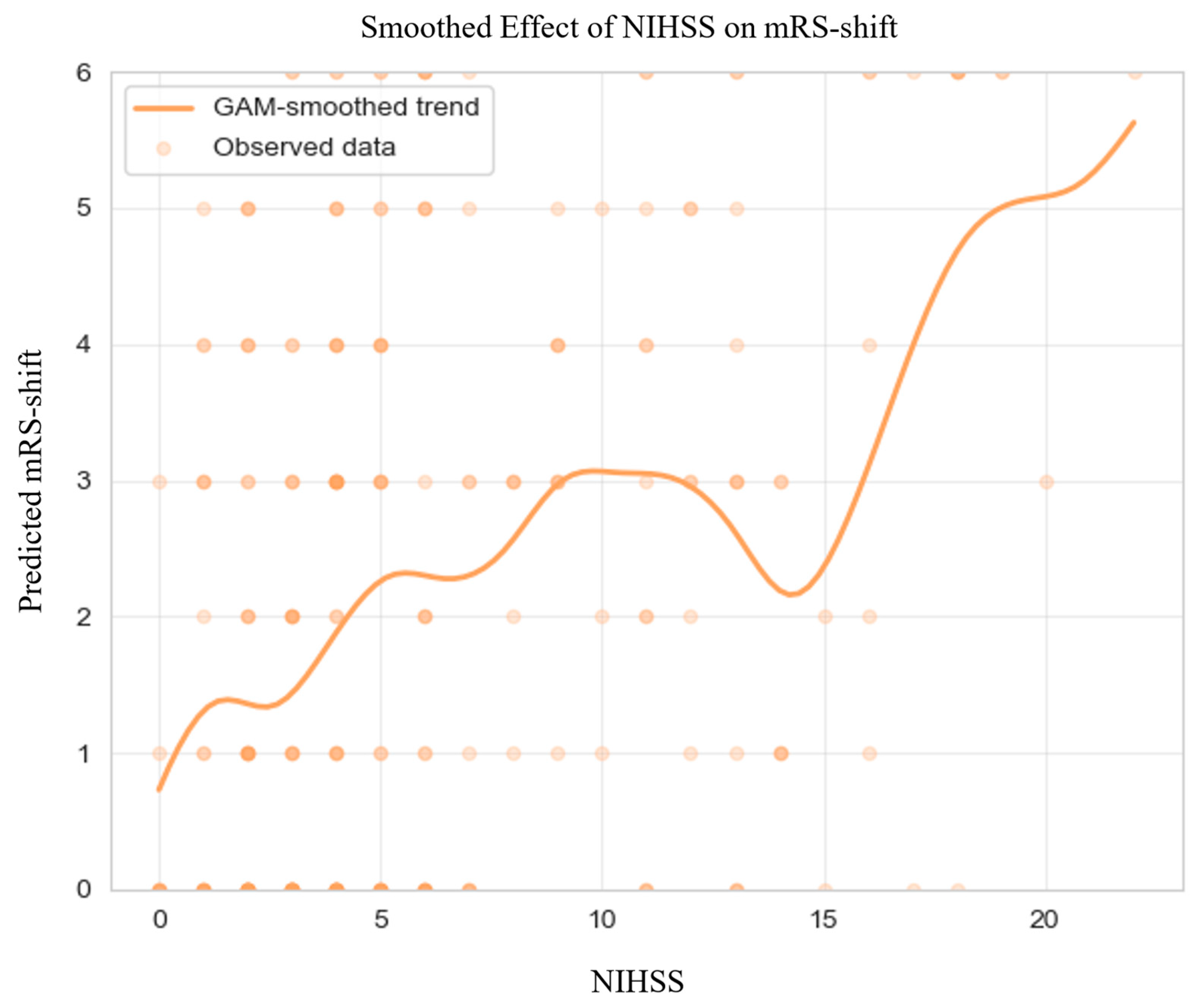
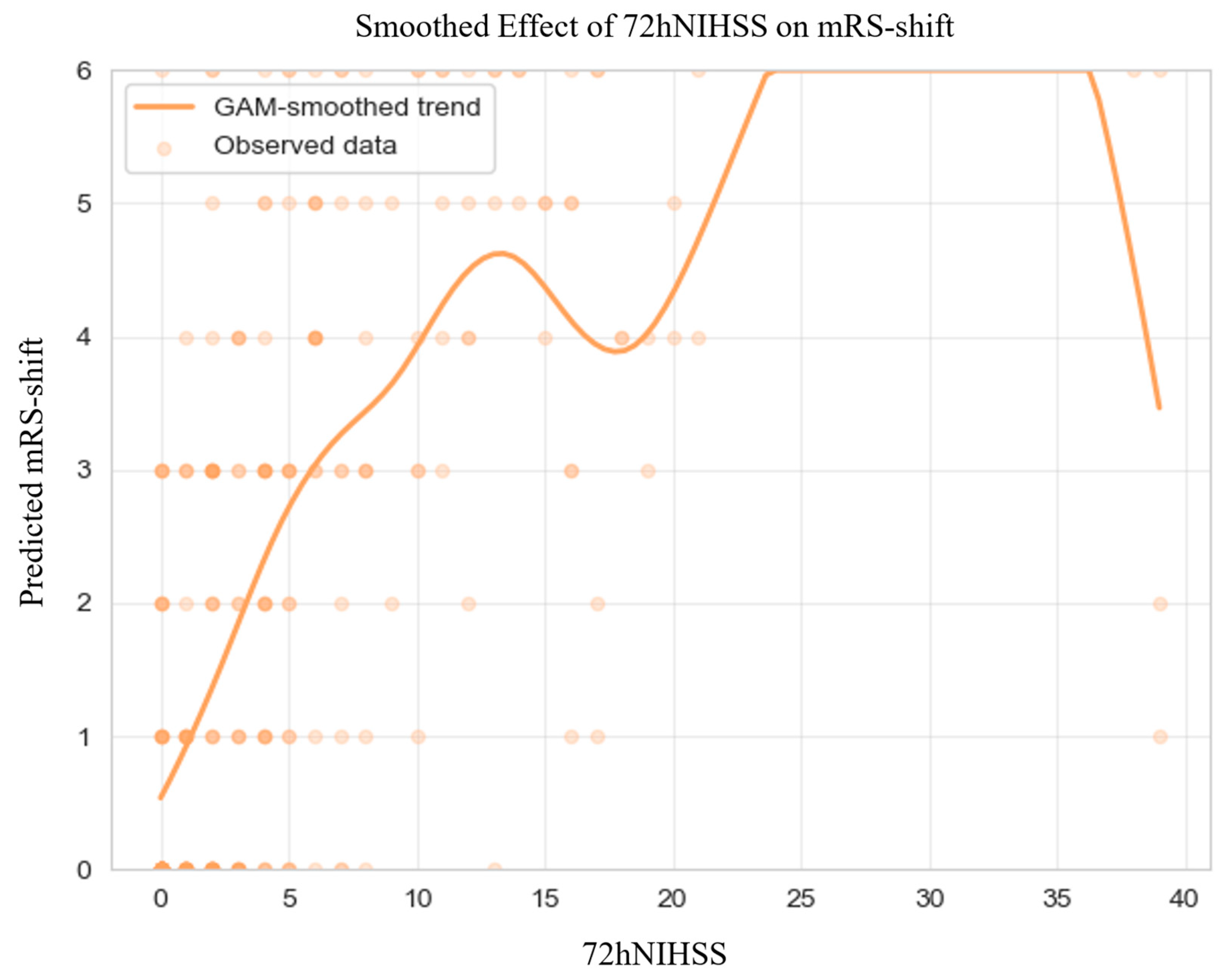
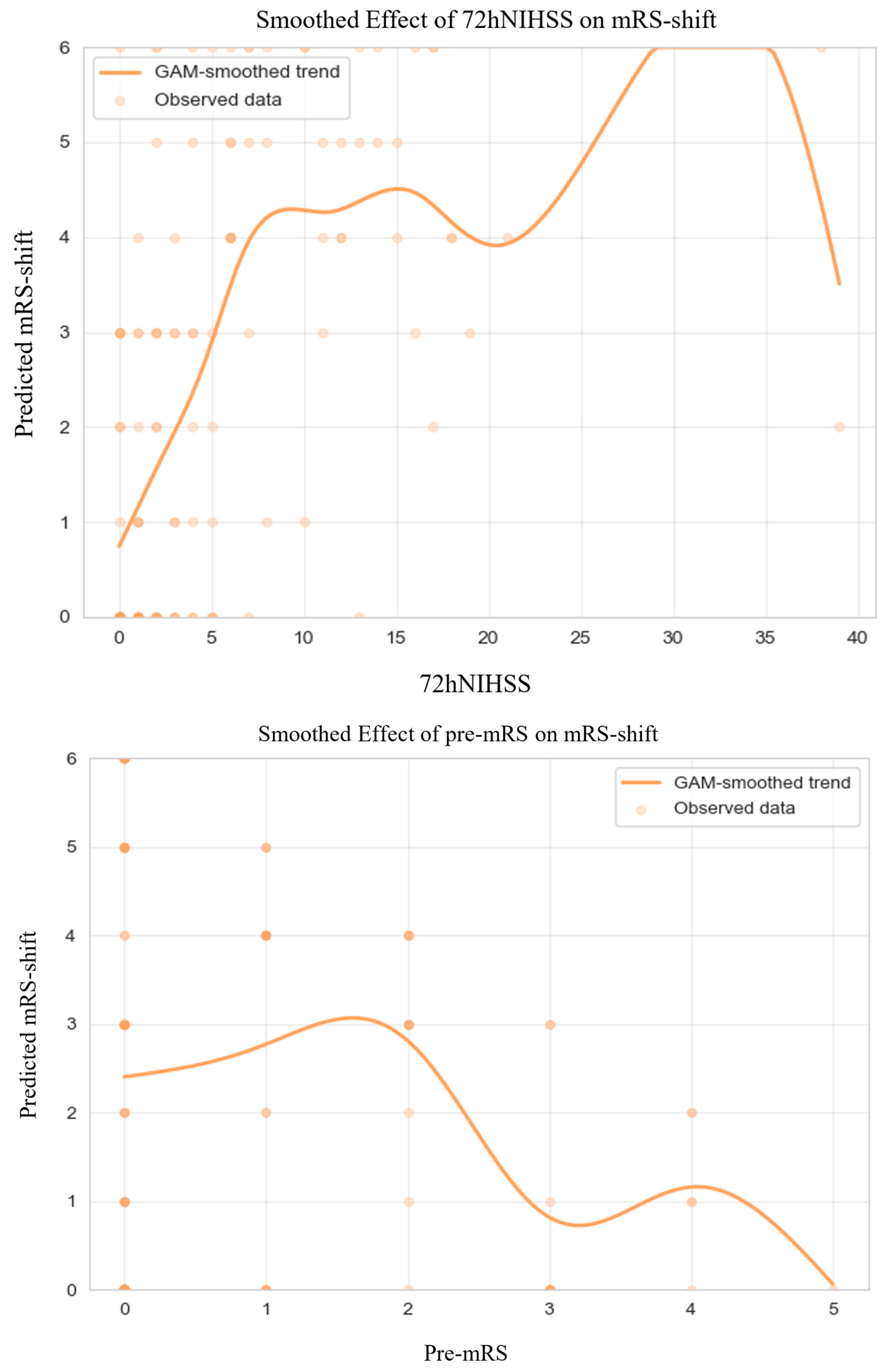
3.5.2. mRS-Shift
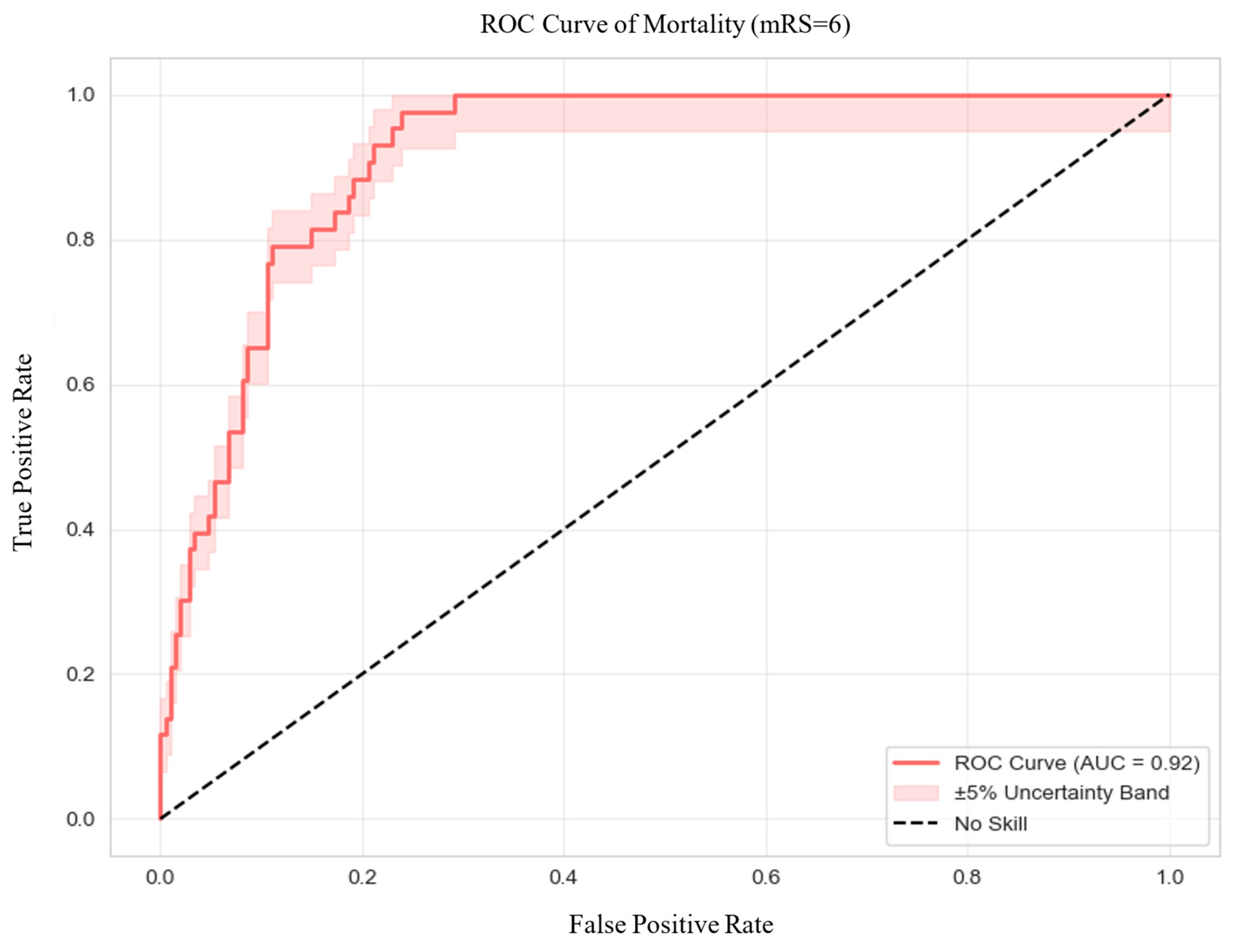
3.5.3. Mortality
3.6. Predictors of Outcome in Anticoagulated Patients
3.6.1. Favorable Outcome
3.6.2. mRS-Shift
3.6.3. Mortality
4. Discussion
4.1. Summary of Findings
4.2. Interpretation and Clinical Implications
4.3. Comparison with Existing Literature
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIS | acute ischemic stroke |
| DOAC | direct oral anticoagulant |
| VKA | vitamin K antagonist |
| IVT | intravenous thrombolysis |
| MT | mechanical thrombectomy |
| NIHSS | National Institutes of Health Stroke Scale |
| pre-mRS | pre-morbid modified Rankin Scale |
| mRS | modified Rankin Scale |
| GAM | generalized additive model |
| OR | odds ratio |
| CI | confidence interval |
| OAC | oral anticoagulant |
| ICH | intracranial hemorrhage |
| AHA/ASA | American Heart Association/American Stroke Association |
| ESO | European Stroke Organisation |
| INR | international normalized ratio |
| TINL | Transzlációs Idegtudományi Nemzeti Laboratórium |
| SMD | standardized mean difference |
| VR | variance ratio |
| SD | standard deviation |
| IQR | interquartile range |
| VIF | variance inflation factor |
| SC | standard care |
| aOR | adjusted odds ratio |
| LLR | log-likelihood ratio |
| AUC | area under the curve |
| DoF | degrees of freedom |
| AIC | Akaike information criterion |
| RCT | randomized control trial |
| DO-IT | DOAC Intravenous Thrombolysis |
| SIFT | Safe IVT FXa |
References
- Feigin, V.L.; Abate, M.D.; Abate, Y.H.; ElHafeez, S.A.; Abd-Allah, F.; Abdelalim, A.; Abdelkader, A.; Abdelmasseh, M.; Abd-Elsalam, S.; Abdi, P.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. 2024, 23, 973–1003. [Google Scholar] [CrossRef]
- Hacke, W.; Kaste, M.; Bluhmki, E.; Brozman, M.; Dávalos, A.; Guidetti, D.; Larrue, V.; Lees, K.R.; Medeghri, Z.; Machnig, T.; et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. N. Engl. J. Med. 2008, 359, 1317–1329. [Google Scholar] [CrossRef]
- Turc, G.; Bhogal, P.; Fischer, U.; Khatri, P.; Lobotesis, K.; Mazighi, M.; Schellinger, P.D.; Toni, D.; de Vries, J.; White, P.; et al. European Stroke Organisation (ESO)—European Society for Minimally Invasive Neurological Therapy (ESMINT) Guidelines on Mechanical Thrombectomy in Acute Ischemic Stroke. J. Neurointerv. Surg. 2023, 15, e8. [Google Scholar] [CrossRef]
- Joglar, J.A.; Chung, M.K.; Armbruster, A.L.; Benjamin, E.J.; Chyou, J.Y.; Cronin, E.M.; Deswal, A.; Eckhardt, L.L.; Goldberger, Z.D.; Gopinathannair, R.; et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2024, 149, e167. [Google Scholar] [CrossRef] [PubMed]
- Emberson, J.; Lees, K.R.; Lyden, P.; Blackwell, L.; Albers, G.; Bluhmki, E.; Brott, T.; Cohen, G.; Davis, S.; Donnan, G.; et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. Lancet 2014, 384, 1929–1935. [Google Scholar] [CrossRef]
- Yaghi, S.; Willey, J.Z.; Cucchiara, B.; Goldstein, J.N.; Gonzales, N.R.; Khatri, P.; Kim, L.J.; Mayer, S.A.; Sheth, K.N.; Schwamm, L.H. Treatment and Outcome of Hemorrhagic Transformation After Intravenous Alteplase in Acute Ischemic Stroke: A Scientific Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2017, 48, e343–e361. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef]
- Berge, E.; Whiteley, W.; Audebert, H.; De Marchis, G.; Fonseca, A.C.; Padiglioni, C.; de la Ossa, N.P.; Strbian, D.; Tsivgoulis, G.; Turc, G. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur. Stroke J. 2021, 6, I–LXII. [Google Scholar] [CrossRef]
- Seiffge, D.J.; De Marchis, G.M.; Koga, M.; Paciaroni, M.; Wilson, D.; Cappellari, M.; Macha, K.; Tsivgoulis, G.; Ambler, G.; Arihiro, S.; et al. Ischemic Stroke despite Oral Anticoagulant Therapy in Patients with Atrial Fibrillation. Ann. Neurol. 2020, 87, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Seiffge, D.J.; Wilson, D.; Wu, T.Y.-H. Administering Thrombolysis for Acute Ischemic Stroke in Patients Taking Direct Oral Anticoagulants. JAMA Neurol. 2021, 78, 515. [Google Scholar] [CrossRef]
- Purrucker, J.C.; Hölscher, K.; Kollmer, J.; Ringleb, P.A. Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants. J. Clin. Med. 2020, 9, 2938. [Google Scholar] [CrossRef]
- Meinel, T.R.; Branca, M.; De Marchis, G.M.; Nedeltchev, K.; Kahles, T.; Bonati, L.; Arnold, M.; Heldner, M.R.; Jung, S.; Carrera, E.; et al. Prior Anticoagulation in Patients with Ischemic Stroke and Atrial Fibrillation. Ann Neurol. 2021, 89, 42–53. [Google Scholar] [CrossRef]
- Brott, T.; Adams, H.P.; Olinger, C.P.; Marler, J.R.; Barsan, W.G.; Biller, J.; Arnold, M.; Heldner, M.R.; Jung, S.; Carrera, E.; et al. Measurements of acute cerebral infarction: A clinical examination scale. Stroke 1989, 20, 864–870. [Google Scholar] [CrossRef]
- van Swieten, J.C.; Koudstaal, P.J.; Visser, M.C.; Schouten, H.J.; van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988, 19, 604–607. [Google Scholar] [CrossRef]
- The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue Plasminogen Activator for Acute Ischemic Stroke. N. Engl. J. Med. 1995, 333, 1581–1588. [Google Scholar] [CrossRef]
- Berkhemer, O.A.; Fransen, P.S.S.; Beumer, D.; van den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.H.; et al. A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef]
- Saver, J.L.; Goyal, M.; Bonafe, A.; Diener, H.-C.; Levy, E.I.; Pereira, V.M.; Albers, G.W.; Cognard, C.; Cohen, D.J.; Hacke, W.; et al. Stent-Retriever Thrombectomy after Intravenous t-PA vs. t-PA Alone in Stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized Assessment of Rapid Endovascular Treatment of Ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Albers, G.W.; Marks, M.P.; Kemp, S.; Christensen, S.; Tsai, J.P.; Ortega-Gutierrez, S.; McTaggart, R.A.; Torbey, M.T.; Kim-Tenser, M.; Leslie-Mazwi, T.; et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N. Engl. J. Med. 2018, 378, 708–718. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Audebert, H.; Turc, G.; Cordonnier, C.; Christensen, H.; Sacco, S.; Sandset, E.C.; Ntaios, G.; Charidimou, A.; Toni, D.; et al. Consensus statements and recommendations from the ESO-Karolinska Stroke Update Conference, Stockholm 11–13 November 2018. Eur. Stroke J. 2019, 4, 307–317. [Google Scholar] [CrossRef]
- Bücke, P.; Jung, S.; Kaesmacher, J.; Goeldlin, M.B.; Horvath, T.; Prange, U.; Beyeler, M.; Fischer, U.; Arnold, M.; Seiffge, D.J.; et al. Intravenous thrombolysis in patients with recent intake of direct oral anticoagulants: A target trial analysis after the liberalization of institutional guidelines. Eur. Stroke J. 2024, 9, 959–967. [Google Scholar] [CrossRef]
- Kam, W.; Holmes, D.N.; Hernandez, A.F.; Saver, J.L.; Fonarow, G.C.; Smith, E.E.; Bhatt, D.L.; Schwamm, L.H.; Reeves, M.J.; Matsouaka, R.A.; et al. Association of Recent Use of Non–Vitamin K Antagonist Oral Anticoagulants With Intracranial Hemorrhage Among Patients with Acute Ischemic Stroke Treated with Alteplase. JAMA 2022, 327, 760. [Google Scholar] [CrossRef] [PubMed]
- Meinel, T.R.; Wilson, D.; Gensicke, H.; Scheitz, J.F.; Ringleb, P.; Goganau, I.; Kaesmacher, J.; Bae, H.-J.; Kim, D.Y.; Kermer, P.; et al. Intravenous Thrombolysis in Patients with Ischemic Stroke and Recent Ingestion of Direct Oral Anticoagulants. JAMA Neurol. 2023, 80, 233. [Google Scholar] [CrossRef] [PubMed]
- Boehme, C.; Mayer-Suess, L.; Mikšová, D.; Lang, W.; Knoflach, M.; Kiechl, S. Prime Time for a Trial Assessing Safety of Intravenous Thrombolysis in Patients Treated with Direct Oral Anticoagulants. Stroke 2024, 55, e149–e150. [Google Scholar] [CrossRef] [PubMed]
- Matusevicius, M.; Säflund, M.; Balestrino, M.; Cappellari, M.; Ferrandi, D.; Ghoreishi, A.; Peeters, A.; Rand, V.; De Michele, M.; Vilionskis, A.; et al. Intravenous Thrombolysis in Patients Taking Direct Oral Anticoagulation Treatment Before Stroke Onset: Results from the Safe Implementations of Treatments in Stroke International Stroke Registry. Ann. Neurol. 2025, 97, 1205–1214. [Google Scholar] [CrossRef]
- Liang, H.; Wang, X.; Quan, X.; Qin, B.; Zhang, J.; Liang, S.; Liang, Z. Safety and efficacy of intravenous thrombolysis in patients with acute ischemic stroke taking direct oral anticoagulants prior to stroke: A meta-analysis. J. Neurol. 2023, 270, 4192–4200. [Google Scholar] [CrossRef]
- L’Allinec, V.; Sibon, I.; Mazighi, M.; Labreuche, J.; Kyheng, M.; Boissier, E.; Roy, M.; Gory, B.; Dargazanli, C.; Desal, H.; et al. MT in anticoagulated patients. Neurology 2020, 94, E842–E850. [Google Scholar] [CrossRef]
- Küpper, C.; Feil, K.; Wollenweber, F.A.; Tiedt, S.; Herzberg, M.; Dorn, F.; Liebig, T.; Dieterich, M.; Kellert, L. Endovascular stroke treatment in orally anticoagulated patients: An analysis from the German Stroke Registry-Endovascular Treatment. J. Neurol. 2021, 268, 1762–1769. [Google Scholar] [CrossRef]
- Goldhoorn, R.-J.B.; van de Graaf, R.A.; van Rees, J.M.; Lingsma, H.F.; Dippel, D.W.J.; Hinsenveld, W.H.; Postma, A.; van den Wijngaard, I.; van Zwam, W.H.; van Oostenbrugge, R.J.; et al. Endovascular Treatment for Acute Ischemic Stroke in Patients on Oral Anticoagulants. Stroke 2020, 51, 1781–1789. [Google Scholar] [CrossRef]
| Non-Anticoagulated (n = 718) | Anticoagulated (n = 148) | p-Value | Matched Non-Anticoagulated (n = 126) | Matched Anticoagulated (n = 126) | p-Value | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age (years), mean ± SD | 69.69 ± 12.14 | 76.46 ± 11.05 | <0.001 * | 74.94 ± 10.37 | 75.66 ± 10.78 | 0.578 |
| Sex, male, n (%) | 356 (49.6) | 64 (43.2) | 0.189 | 51 (40.5) | 51 (40.5) | 0.999 |
| Clinical Characteristics | ||||||
| Pre-mRS score, median [IQR] | 0 [0–1] | 0 (0–2) | 0.018 * | 0 (0–1) | 0 (0–1) | 0.889 |
| NIHSS score at admission, median [IQR] | 5 [3–8] | 5 [3–11] | 0.071 | 4 (3–7) | 4 (2–9) | 0.904 |
| NIHSS score at 72 h, median [IQR] | 2 [0–7] | 4 [1–11] | 0.030 * | 3 (2–7) | 3 (1–7) | 0.926 |
| ICH, n (%) | 33 (4.6) | 8 (5.4) | 0.573 | 8 (6.4) | 5 (4.0) | 0.571 |
| Etiology, cardioembolic, n (%) | 193 (26.9) | 109 (73.7) | <0.001 * | 38 (30.2) | 95 (75.4) | <0.001 * |
| Onset-to-door time (min), median [IQR] | 310 [102–826] | 309 [158–821] | 0.503 | 265 [96–847] | 285 [101–731] | 0.865 |
| Plasma glucose (mmol/l), mean ± SD | 7.69 ± 2.96 | 7.45 ± 2.86 | 0.147 | 7.81 ± 3.42 | 7.15 ± 1.86 | 0.350 |
| Medical History, n (%) | ||||||
| Hypertension | 580 (80.8) | 139 (93.9) | <0.001 * | 120 (95.2) | 120 (95.2) | 0.999 |
| Diabetes mellitus | 244 (34.0) | 59 (39.9) | 0.020 * | 47 (37.3) | 47 (37.3) | 0.999 |
| Recanalization Therapy, n (%) | ||||||
| IVT | 190 (26.5) | 5 (3.4) | <0.001 * | 39 (30.9) | 5 (4.0) | <0.001 * |
| MT | 124 (17.3) | 39 (26.4) | 0.014 * | 16 (12.7) | 32 (25.4) | 0.016 * |
| IVT + MT | 62 (8.6) | 6 (4.1) | 0.086 | 10 (7.9) | 5 (4.0) | 0.287 |
| Before Matching | After Matching | |
|---|---|---|
| Age | 0.583 | 0.067 |
| Sex | 0.127 | 0.000 |
| Pre-mRS score | 0.190 | 0.013 |
| NIHSS score at admission | 0.241 | 0.053 |
| NIHSS score at 72 h | 0.174 | 0.029 |
| Hypertension | 0.403 | 0.000 |
| Diabetes mellitus | 0.122 | 0.000 |
| Before Matching | After Matching | |
|---|---|---|
| Age | 0.829, p < 0.001 * | 1.080, p = 0.999 |
| Sex | 0.987, p = 0.680 | 1.000, p = 0.999 |
| Pre-mRS score | 1.227, p = 0.214 | 0.995, p = 0.999 |
| NIHSS score at admission | 1.703, p = 0.037 * | 1.294, p = 0.907 |
| NIHSS score at 72 h | 1.209, p = 0.084 | 1.052, p = 0.963 |
| Hypertension | 0.369, p = 0.026 * | 1.000, p = 0.999 |
| Diabetes mellitus | 1.074, p = 0.764 | 1.000, p = 0.999 |
| Variable | Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Anticoagulation status | 0.4417 | 0.346 | −0.477 to 1.360 |
| Age | 0.0183 | 0.393 | −0.024 to 0.060 |
| Sex | 0.8660 | 0.043 * | 0.026 to 1.706 |
| Pre-stroke mRS score | 1.4207 | <0.001 * | 0.896 to 1.945 |
| NIHSS score at admission | 0.1072 | 0.035 * | 0.008 to 0.207 |
| NIHSS score at 72 h | 0.5210 | <0.001 * | 0.343 to 0.699 |
| Etiology, cardioembolic | −0.0044 | 0.992 | −0.872 to 0.863 |
| Hypertension | 1.7742 | 0.069 | −0.140 to 3.688 |
| Diabetes mellitus | 0.4666 | 0.256 | −0.338 to 1.272 |
| IVT | 0.0903 | 0.865 | −0.954 to 1.135 |
| MT | 0.0407 | 0.946 | −1.128 to 1.209 |
| IVT + MT | −0.7414 | 0.425 | −2.564 to 1.082 |
| Variable | Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Anticoagulation status | 0.8562 | 0.125 | −0.237 to 1.949 |
| Age | 0.0445 | 0.131 | −0.013 to 0.102 |
| Sex | −0.4154 | 0.409 | −1.401 to 0.570 |
| Pre-stroke mRS score | −0.0785 | 0.673 | −0.443 to 0.286 |
| NIHSS score at admission | 0.1772 | <0.001 * | 0.092 to 0.262 |
| NIHSS score at 72 h | 0.2075 | <0.001 * | 0.120 to 0.295 |
| Etiology, cardioembolic | 0.3235 | 0.548 | −0.732 to 1.379 |
| Hypertension | −0.1735 | 0.879 | −2.414 to 2.067 |
| Diabetes mellitus | 0.9030 | 0.065 | −0.056 to 1.862 |
| IVT | 0.1266 | 0.876 | −1.469 to 1.722 |
| MT | −0.5796 | 0.313 | −1.706 to 0.546 |
| IVT + MT | −0.8911 | 0.351 | −2.764 to 0.982 |
| Variable | Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Atrial fibrillation | 0.3466 | 0.718 | −1.532 to 2.225 |
| Previous stroke | 0.5961 | 0.472 | −1.029 to 2.222 |
| Age | 0.0026 | 0.946 | −0.072 to 0.077 |
| Sex | −1.0821 | 0.154 | −2.570 to 0.406 |
| Pre-stroke mRS score | −2.0189 | 0.001 * | −3.188 to −0.849 |
| NIHSS score at admission | −0.1298 | 0.107 | −0.288 to 0.028 |
| NIHSS score at 72 h | −0.5987 | <0.001 * | −0.915 to −0.282 |
| Etiology, cardioembolic | −0.2166 | 0.784 | −1.768 to 1.335 |
| Hypertension | −2.0567 | 0.241 | −5.491 to 1.378 |
| Diabetes mellitus | −0.7042 | 0.356 | −2.198 to 0.790 |
| IVT | 1.3349 | 0.421 | −1.915 to 4.585 |
| MT | −0.8451 | 0.424 | −2.919 to 1.228 |
| IVT + MT | −2.2298 | 0.180 | −5.487 to 1.027 |
| Type of anticoagulant | 1.2983 | 0.140 | −0.427 to 3.023 |
| Variable | Coefficient | p-Value | 95% CI |
|---|---|---|---|
| Atrial fibrillation | 0.1055 | 0.890 | −1.386 to 1.597 |
| Previous stroke | −0.1026 | 0.892 | −1.586 to 1.381 |
| Age | 0.0690 | 0.076 | −0.007 to 0.145 |
| Sex | −1.0762 | 0.086 | −2.306 to 0.154 |
| Pre-stroke mRS score | −0.1025 | 0.690 | −0.607 to 0.402 |
| NIHSS score at admission | 0.1209 | 0.028 * | 0.013 to 0.228 |
| NIHSS score at 72 h | 0.1689 | 0.001 * | 0.065 to 0.272 |
| Etiology, cardioembolic | 0.0117 | 0.987 | −1.365 to 1.388 |
| Hypertension | −0.1276 | 0.920 | −2.603 to 2.348 |
| Diabetes mellitus | 0.8259 | 0.215 | −0.479 to 2.130 |
| IVT | 0.5256 | 0.750 | −2.703 to 3.754 |
| MT | 0.3485 | 0.623 | −1.041 to 1.738 |
| IVT + MT | 1.1625 | 0.471 | −1.998 to 4.323 |
| Type of anticoagulant | −0.5735 | 0.426 | −1.987 to 0.840 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seetge, J.; Cséke, B.; Karádi, Z.N.; Bosnyák, E.; Jozifek, E.J.; Szapáry, L. Trick or Treat(ment): Should We Still Fear Reperfusion Therapy in Anticoagulated Stroke Patients?—Comparable 90-Day Outcomes in a Propensity-Score-Matched Registry Study. J. Clin. Med. 2025, 14, 8146. https://doi.org/10.3390/jcm14228146
Seetge J, Cséke B, Karádi ZN, Bosnyák E, Jozifek EJ, Szapáry L. Trick or Treat(ment): Should We Still Fear Reperfusion Therapy in Anticoagulated Stroke Patients?—Comparable 90-Day Outcomes in a Propensity-Score-Matched Registry Study. Journal of Clinical Medicine. 2025; 14(22):8146. https://doi.org/10.3390/jcm14228146
Chicago/Turabian StyleSeetge, Jessica, Balázs Cséke, Zsófia Nozomi Karádi, Edit Bosnyák, Eszter Johanna Jozifek, and László Szapáry. 2025. "Trick or Treat(ment): Should We Still Fear Reperfusion Therapy in Anticoagulated Stroke Patients?—Comparable 90-Day Outcomes in a Propensity-Score-Matched Registry Study" Journal of Clinical Medicine 14, no. 22: 8146. https://doi.org/10.3390/jcm14228146
APA StyleSeetge, J., Cséke, B., Karádi, Z. N., Bosnyák, E., Jozifek, E. J., & Szapáry, L. (2025). Trick or Treat(ment): Should We Still Fear Reperfusion Therapy in Anticoagulated Stroke Patients?—Comparable 90-Day Outcomes in a Propensity-Score-Matched Registry Study. Journal of Clinical Medicine, 14(22), 8146. https://doi.org/10.3390/jcm14228146





