Endoscopic Assistance in Minimally Invasive Repair of Acute Achilles Ruptures: A Prospective Observational Study Comparing Endoscopic-Assisted, Minimally Invasive, and Open Techniques
Abstract
1. Introduction
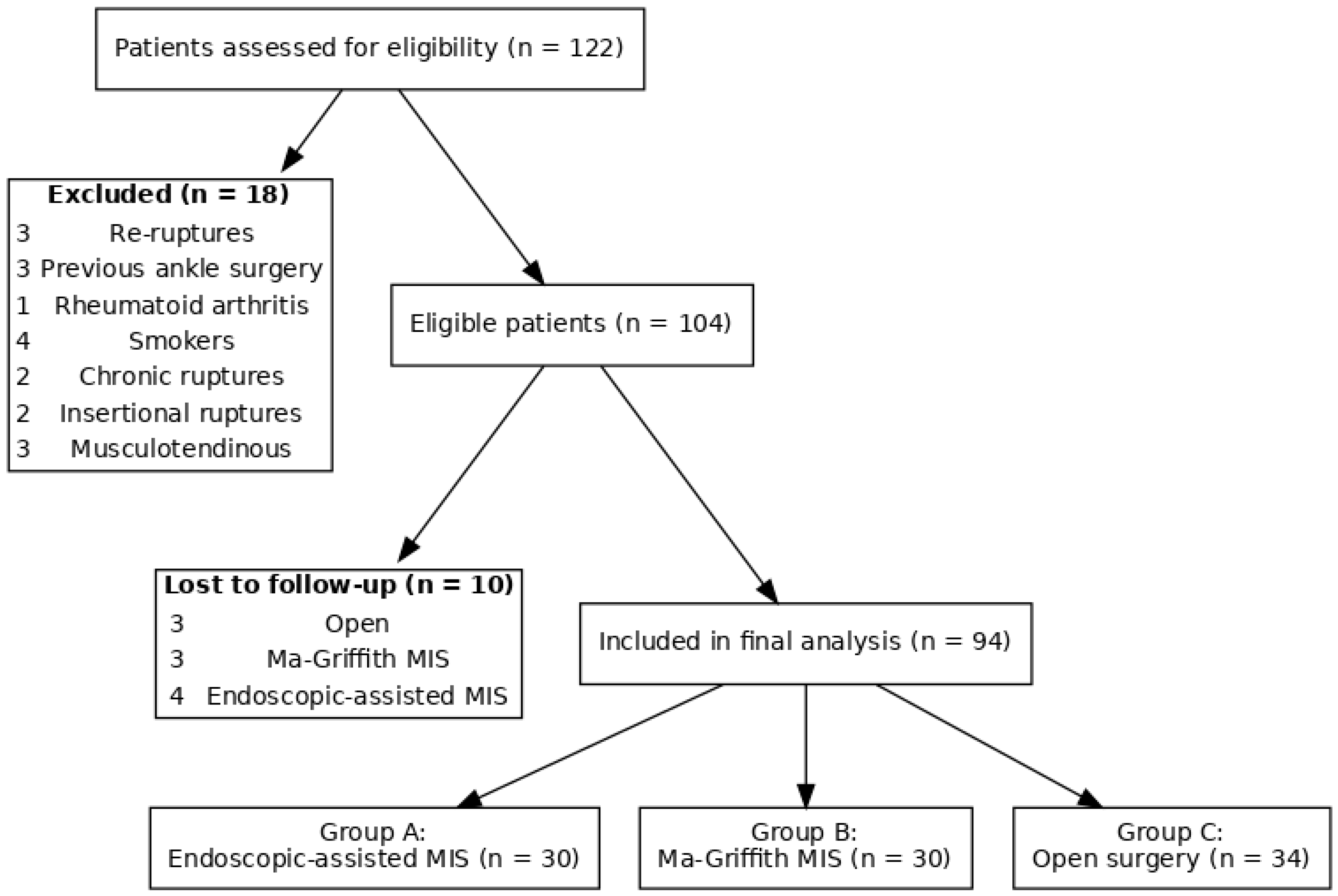
2. Materials and Methods
2.1. Patient Population and Criteria
- Group A: endoscopic-assisted minimally invasive technique.
- Group B: M-G/MISI.
- Group C: open surgery (Krackow suture).
2.2. Statistical Analyses
2.3. Surgical Techniques
2.3.1. Group A—Endoscopic-Assisted Minimally Invasive Technique
2.3.2. Group B—Ma-Griffith with Minimally Invasive Small Incision (M-G/MISI) Technique
2.3.3. Group C—Open Surgery (Krackow Suture)
2.4. Post-Operative Protocol
3. Results
3.1. Return to Drive, Work Activities, and Sport Activities
3.2. Clinical Outcomes: ATRS and AH-AOFAS
3.3. Complications
- Group A: 2 patients presented minimal paresthesia at the surgical site, resolved after three months conservatively. One patient with paresthesia developed a DVT and was treated with low molecular heparin.
- Group B: 4 patients complained of paresthesia at the surgical site, 2 patients complained of ankle stiffness. No major complication was reported.
- Group C: Two patients needed revision surgery because of infection with associated failure of the tendon suture, 20% suffered from postoperative ankle stiffness (Table 4).
4. Discussion
Challenges and Limitations
- Learning Curve and Cost Implications
- Patient Selection
- Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AT | Achilles tendon |
| MIS | minimally-invasive surgery |
| M-G/MISI | Ma-Griffith minimally invasive small incision |
| BMI | body mass index |
| ATRS | achilles tendon total rupture score |
| AH-AOFAS | American Orthopaedic Foot and Ankle Society Ankle-Hindfoot Score |
| RTD | return to driving |
| RTW | return to work |
| RTS | return to sports |
References
- Twaddle, B.C.; Poon, P. Early Motion for Achilles Tendon Ruptures: Is Surgery Important?: A Randomized, Prospective Study. Am. J. Sports Med. 2007, 35, 2033–2038. [Google Scholar] [CrossRef] [PubMed]
- Meulenkamp, B.; Woolnough, T.; Cheng, W.; Shorr, R.; Stacey, D.; Richards, M.; Gupta, A.B.; Fergusson, D.; Graham, I.D.P. What Is the Best Evidence to Guide Management of Acute Achilles Tendon Ruptures? A Systematic Review and Network Meta-Analysis of Randomized Controlled Trials. Clin. Orthop. Relat. Res. 2021, 479, 2119–2131. [Google Scholar] [CrossRef]
- Soroceanu, A.; Glazebrook, M.; Sidhwa, F.; Aarabi, S.; Kaufman, A. Surgical versus nonsurgical treatment of acute achilles tendon rupture: A meta-analysis of randomized trials. J. Bone Jt. Surg. 2012, 94, 2136–2143. [Google Scholar] [CrossRef]
- Keating, J.F.; Will, E.M. Operative versus non-operative treatment of acute rupture of tendo Achillis: A prospective randomised evaluation of functional outcome. J. Bone Jt. Surg.-Ser. B. 2011, 93-B, 1071–1078. [Google Scholar] [CrossRef]
- Morrey, B.F. Operative versus Nonoperative Treatment of Acute Achilles Tendon Ruptures: A Multicenter Randomized Trial Using Accelerated Functional Rehabilitation. Yearb. Orthop. 2011, 2011, 228–230. [Google Scholar] [CrossRef]
- Oliva, F.; Rugiero, C.; Via, A.G.; Baldassarri, M.; Bernardi, G.; Biz, C.; Bossa, M.; Buda, R.; Buonocore, D.; Chianca, V.; et al. I.S.Mu.L.T. Achilles tendon ruptures guidelines. Muscles Ligaments Tendons J. 2018, 3, 310–363. [Google Scholar] [CrossRef]
- Myhrvold, S.B.; Brouwer, E.F.; Andresen, T.K.M.; Rydevik, K.; Amundsen, M.; Grün, W.; Butt, F.; Valberg, M.; Ulstein, S.; Hoelsbrekken, S.E. Nonoperative or Surgical Treatment of Acute Achilles’ Tendon Rupture. N. Engl. J. Med. 2022, 386, 1409–1420. [Google Scholar] [CrossRef] [PubMed]
- Cetti, R.; Christensen, S.E.; Ejsted, R.; Jensen, N.M.; Jorgensen, U. Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am. J. Sports Med. 1993, 21, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Möller, M.; Movin, T.; Granhed, H.; Lind, K.; Faxén, E.; Karlsson, J. Acute rupture of tendon Achillis. A prospective randomised study of comparison between surgical and non-surgical treatment. J. Bone Jt. Surg. Br. 2001, 83, 843–848. [Google Scholar] [CrossRef]
- Thevendran, G.; Sarraf, K.M.; Patel, N.K.; Sadri, A.; Rosenfeld, P. The ruptured Achilles tendon: A current overview from biology of rupture to treatment. Musculoskelet. Surg. 2013, 97, 9–20. [Google Scholar] [CrossRef]
- Seow, D.; Yasui, Y.; Calder, J.D.F.; Kennedy, J.G.; Pearce, C.J. Treatment of Acute Achilles Tendon Ruptures: A Systematic Review and Meta-analysis of Complication Rates with Best- and Worst-Case Analyses for Rerupture Rates. Am. J. Sports Med. 2021, 49, 3728–3748. [Google Scholar] [CrossRef]
- Clanton, T.; Stake, I.K.; Bartush, K.; Jamieson, M.D. Minimally Invasive Achilles Repair Techniques. Orthop. Clin. N. Am. 2020, 51, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.S.; Kadakia, A.R. Minimally Invasive Treatments of Acute Achilles Tendon Ruptures. Foot Ankle Clin. 2019, 24, 399–424. [Google Scholar] [CrossRef]
- Grassi, A.; Amendola, A.; Samuelsson, K.; Svantesson, E.; Romagnoli, M.; Bondi, A.; Massimiliano, M.; Stefano, Z. Minimally Invasive Versus Open Repair for Acute Achilles Tendon Rupture: Meta-Analysis Showing Reduced Complications, with Similar Outcomes, After Minimally Invasive Surgery. J. Bone Jt. Surg. Am. 2018, 100, 1969–1981. [Google Scholar] [CrossRef] [PubMed]
- Deng, H.; Cheng, X.; Yang, Y.; Fang, F.; He, J.; Tian, Y.; Li, T.; Xiao, Y.; Feng, Y.; Wang, P.; et al. Rerupture outcome of conservative versus open repair versus minimally invasive repair of acute Achilles tendon ruptures: A systematic review and meta-analysis. PLoS ONE 2023, 18, e0285046. [Google Scholar] [CrossRef] [PubMed]
- Čretnik, A.; Kosanović, M.; Smrkolj, V. Percutaneous versus open repair of the ruptured Achilles tendon: A comparative study. Am. J. Sports Med. 2005, 33, 1369–1379. [Google Scholar] [CrossRef]
- Gatz, M.; Driessen, A.; Eschweiler, J.; Tingart, M.; Migliorini, F. Open versus minimally-invasive surgery for Achilles tendon rupture: A meta-analysis study. Arch. Orthop. Trauma Surg. 2021, 141, 383–401. [Google Scholar] [CrossRef]
- Attia, A.K.; Mahmoud, K.; d’Hooghe, P.; Bariteau, J.; Labib, S.A.; Myerson, M.S. Outcomes and Complications of Open Versus Minimally Invasive Repair of Acute Achilles Tendon Ruptures: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Am. J. Sports Med. 2023, 51, 825–836. [Google Scholar] [CrossRef]
- American Orthopaedic Foot & Ankle Society. POSTION STATEMENT Management of Acute Achilles Tendon Ruptures; American Orthopaedic Foot & Ankle Society: Schaumburg, IL, USA, 2024; pp. 1–10. [Google Scholar]
- Fortis, A.P.; Dimas, A.; Lamprakis, A.A. Repair of Achilles Tendon Rupture Under Endoscopic Control. Arthrosc.-J. Arthrosc. Relat. Surg. 2008, 24, 683–688. [Google Scholar] [CrossRef]
- Rungprai, C.; Phisitkul, P. Outcomes and Complications Following Endoscopically Assisted Percutaneous Achilles Tendon Repair. Arthrosc.-J. Arthrosc. Relat. Surg. 2018, 34, 1262–1269. [Google Scholar] [CrossRef]
- Doral, M.N.; Bozkurt, M.; Turhan, E.; Ayvaz, M.; Atay, Ö.A.; Üzümcügil, A.; Leblebicioğlu, G.; Kaya, D.; Aydoğ, T. Percutaneous suturing of the ruptured Achilles tendon with endoscopic control. Arch. Orthop. Trauma Surg. 2009, 129, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Lui, T.H. Editorial Commentary: Is Endoscopy Really Helpful During Repair of Acute Rupture of the Achilles Tendon? Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 1270–1271. [Google Scholar] [CrossRef]
- Krackow, K.A.; Thomas, S.C.; Jones, L.C. A new stitch for ligament-tendon fixation. Brief note. J. Bone Jt. Surg. 1986, 68, 764–766. [Google Scholar] [CrossRef]
- Carmont, M.R.; Maffulli, N. Modified percutaneous repair of ruptured Achilles tendon. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 199–203. [Google Scholar] [CrossRef]
- Ma, G.W.C.; Griffith, T.G. Percutaneous repair of acute closed ruptured Achilles tendon: A new technique. Clin. Orthop. Relat. Res. 1977, 128, 247–255. [Google Scholar] [CrossRef]
- Yu, H.; Wang, F.; Xie, J.; Yao, Y.; Jing, J.; Li, J. The Reinforced Ma–Griffith Method Combined with Minimally Invasive Small-Incision Suture for Acute Achilles Tendon Rupture. Orthop. Surg. 2022, 14, 315–322. [Google Scholar] [CrossRef]
- Turgut, A.; Günal, I.; Maralcan, G.; Köse, N.; Göktürk, E. Endoscopy, assisted percutaneous repair of the Achilles tendon ruptures: A cadaveric and clinical study. Knee Surg. Sports Traumatol. Arthrosc. 2002, 10, 130–133. [Google Scholar] [CrossRef]
- Nilsson-Helander, K.; Thomeé, R.; Grävare-Silbernagel, K.; Thomeé, P.; Faxén, E.; Eriksson, B.I.; Karlsson, J. The Achilles tendon Total Rupture Score (ATRS): Development and validation. Am. J. Sports Med. 2007, 35, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Chiu, C.-H.; Yeh, W.-L.; Tsai, M.-C.; Chang, S.-S.; Hsu, K.-Y.; Chan, Y.-S. Endoscopy-assisted percutaneous repair of acute Achilles tendon tears. Foot Ankle Int. 2013, 34, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Halasi, T.; Tállay, A.; Berkes, I. Percutaneous Achilles tendon repair with and without endoscopic control. Knee Surg. Sports Traumatol. Arthrosc. 2003, 11, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Del Buono, A.; Volpin, A.; Maffulli, N. Minimally invasive versus open surgery for acute Achilles tendon rupture: A systematic review. Br. Med. Bull. 2014, 109, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Čukelj, F.; Blažević, D.; Čukelj, F.; Sabalić, S.; Benčić, I.; Ćuti, T.; Pivalica, D.; Bakota, B.; Vidović, D. Comparison of percutaneous and open repair of Achilles tendon rupture: Results and complications from a single institution. BMC Surg. 2024, 24, 47. [Google Scholar] [CrossRef] [PubMed]
- Karabinas, P.K.; Benetos, I.S.; Lampropoulou-Adamidou, K.; Romoudis, P.; Mavrogenis, A.F.; Vlamis, J. Percutaneous versus open repair of acute Achilles tendon ruptures. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 607–613. [Google Scholar] [CrossRef]
- Manent, A.; López, L.; Corominas, H.; Santamaría, A.; Domínguez, A.; Llorens, N.; Sales, M.; Videla, S. Acute Achilles Tendon Ruptures: Efficacy of Conservative and Surgical (Percutaneous, Open) Treatment-A Randomized, Controlled, Clinical Trial. J. Foot Ankle Surg. 2019, 58, 1229–1234. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Cho, T.; Mustapha, R.; Phillips, T.; Hoffman, B.; Brown, C.; Liu, J. Achilles tendon rupture treated with open versus percutaneous repair: A Narrative review. J. Orthop. Rep. 2024, 3, 100357. [Google Scholar] [CrossRef]
- Henríquez, H.; Muñoz, R.; Carcuro, G.; Bastías, C. Is percutaneous repair better than open repair in acute Achilles tendon rupture? Clin. Orthop. Relat. Res. 2012, 470, 998–1003. [Google Scholar] [CrossRef]
- Maempel, J.F.; Clement, N.D.; Wickramasinghe, N.R.; Duckworth, A.D.; Keating, J.F. Operative repair of acute Achilles tendon rupture does not give superior patient-reported outcomes to nonoperative management. Bone Jt. J. 2020, 102-B, 933–940. [Google Scholar] [CrossRef]
| Total | Group A | Group B | Group C | |
|---|---|---|---|---|
| N° patients | 94 | 30 | 30 | 34 |
| Sex (M:F) | 60:34 | 23:13 | 19:10 | 18:11 |
| Age (years) | 42.54 (18–78) | 43.32 (24–66) | 40.21 (18–69) | 43.35 (22–78) |
| BMI (mean values) | 26.63 | 26.54 | 25.00 | 27.12 |
| Follow-up (months) | 32 (24–60) | 32 (24–56) | 31 (24–60) | 31 (24–58) |
| Group A | Group B | Group C | p Value | |
|---|---|---|---|---|
| RTD | 72.18 ± 15.9 | 66.00 ± 14.5 | 82.33 ± 18.1 | p = 0.013 |
| RTW | 44.24 ± 11.1 | 35.64 ± 8.9 | 51.12 ± 12.8 | p < 0.0001 |
| RTS | 202.83 ± 54.8 | 208.00 ± 56.2 | 219.00 ± 59.1 | p = 0.46 |
| Group A | Group B | Group C | p Value | |
|---|---|---|---|---|
| ATRS score | 79.33 ± 11.2 | 87.64 ± 9.1 | 72.75 ± 13.4 | p < 0.0001 |
| AH-AOFAS score | 96.28 ± 6.6 | 96.44 ± 5.3 | 94.02 ± 7.3 | p = 0.41 |
| Total | Group A | Group B | Group C | p Value | |
|---|---|---|---|---|---|
| Minor | |||||
| Post-op paresthesia | 10 | 2 | 4 | 4 | p = 0.67 |
| Shoe discomfort | 5 | 2 | 1 | 2 | p = 0.83 |
| Major | |||||
| DVT | 1 | 1 | 0 | 0 | p = 0.34 |
| Infection | 2 | 1 | 0 | 1 | p = 0.61 |
| Axono/neurotmesis | 0 | 0 | 0 | 0 | p = 0.43 |
| Rate of reoperation | 2 | 0 | 0 | 2 | p = 0.16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceccarini, P.; Donantoni, M.; Lucchetta, L.; Marinozzi, A.; Antinolfi, P.; Rinonapoli, G.; Caraffa, A. Endoscopic Assistance in Minimally Invasive Repair of Acute Achilles Ruptures: A Prospective Observational Study Comparing Endoscopic-Assisted, Minimally Invasive, and Open Techniques. J. Clin. Med. 2025, 14, 8117. https://doi.org/10.3390/jcm14228117
Ceccarini P, Donantoni M, Lucchetta L, Marinozzi A, Antinolfi P, Rinonapoli G, Caraffa A. Endoscopic Assistance in Minimally Invasive Repair of Acute Achilles Ruptures: A Prospective Observational Study Comparing Endoscopic-Assisted, Minimally Invasive, and Open Techniques. Journal of Clinical Medicine. 2025; 14(22):8117. https://doi.org/10.3390/jcm14228117
Chicago/Turabian StyleCeccarini, Paolo, Marco Donantoni, Lorenzo Lucchetta, Andrea Marinozzi, Pierluigi Antinolfi, Giuseppe Rinonapoli, and Auro Caraffa. 2025. "Endoscopic Assistance in Minimally Invasive Repair of Acute Achilles Ruptures: A Prospective Observational Study Comparing Endoscopic-Assisted, Minimally Invasive, and Open Techniques" Journal of Clinical Medicine 14, no. 22: 8117. https://doi.org/10.3390/jcm14228117
APA StyleCeccarini, P., Donantoni, M., Lucchetta, L., Marinozzi, A., Antinolfi, P., Rinonapoli, G., & Caraffa, A. (2025). Endoscopic Assistance in Minimally Invasive Repair of Acute Achilles Ruptures: A Prospective Observational Study Comparing Endoscopic-Assisted, Minimally Invasive, and Open Techniques. Journal of Clinical Medicine, 14(22), 8117. https://doi.org/10.3390/jcm14228117






