Rehabilitation Intervention for an Infant with Simple Epidermolysis Bullosa from NICU to Home Discharge: A Case Report
Abstract
1. Introduction
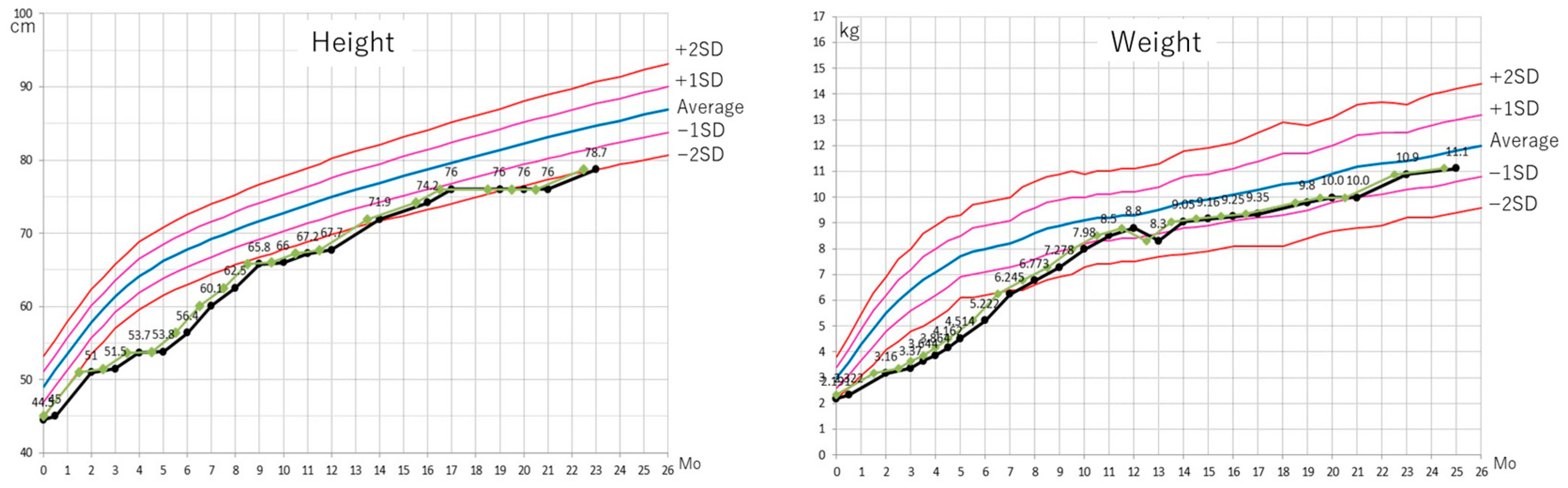
2. Case Presentation
2.1. Clinical Course Before the Initiation of Habilitation/Rehabilitation (Postnatal Days 0–81)
2.2. Rehabilitation Initiation with Minimal Contact (Phase I: Postnatal Days 81–107)
2.3. Gross Motor Training with Minimal Body Contact (Phase II: Postnatal Days 108–180)
2.4. Initiation of Functional Habilitation (Phase III: Postnatal Days 181–240)
2.5. Habilitation for Acquisition of Mobility and Fine Motor Skills (Phase IV: Postnatal Days 241–310)
2.6. Discharge (Phase V: Postnatal Day 311)
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| COVID-19 | Coronavirus Disease-19 |
| CPAP | Continuous Positive Airway Pressure |
| EB | Epidermolysis bullosa EB |
| NICU | Neonatal Intensive Care Unit |
| ROM | Range of Motion |
| SiPAP | Synchronized Inspiratory Positive Airway Pressure |
References
- Fine, J.D. Epidemiology of Inherited Epidermolysis Bullosa Based on Incidence and Prevalence Estimates From the National Epidermolysis Bullosa Registry. JAMA Dermatol. 2016, 152, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Bodemer, C.; Soussand, L.; Sandrin, A.; Khatim, A.; Sauvestre, A.; Elarouci, N.; Jannot, A.S. French data on the epidemiology and expert healthcare network for epidermolysis bullosa. J. Eur. Acad. Dermatol. Venereol. JEADV 2023, 37, e597–e599. [Google Scholar] [CrossRef]
- Kho, Y.C.; Rhodes, L.M.; Robertson, S.J.; Su, J.; Varigos, G.; Robertson, I.; Hogan, P.; Orchard, D.; Murrell, D.F. Epidemiology of epidermolysis bullosa in the antipodes: The Australasian Epidermolysis Bullosa Registry with a focus on Herlitz junctional epidermolysis bullosa. Arch. Dermatol. 2010, 146, 635–640. [Google Scholar] [CrossRef]
- Petrof, G.; Papanikolaou, M.; Martinez, A.E.; Mellerio, J.E.; McGrath, J.A.; Bardhan, A.; Harper, N.; Heagerty, A.; Ogboli, M.; Chiswell, C.; et al. The epidemiology of epidermolysis bullosa in England and Wales: Data from the national epidermolysis bullosa database. Br. J. Dermatol. 2022, 186, 843–848. [Google Scholar] [CrossRef]
- Kimura, T.; Hosoi, K.; Yoshida, K.; Ishiko, A.; Miyamoto, M.; Narita, M. A neonatal case of epidermolysis bullosa complicated by bronchomalacia. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2025, 67, e70156. [Google Scholar] [CrossRef]
- Kern, J.S.; Sprecher, E.; Fernandez, M.F.; Schauer, F.; Bodemer, C.; Cunningham, T.; Lowe, S.; Davis, C.; Sumeray, M.; Bruckner, A.L.; et al. Efficacy and safety of Oleogel-S10 (birch triterpenes) for epidermolysis bullosa: Results from the phase III randomized double-blind phase of the EASE study. Br. J. Dermatol. 2023, 188, 12–21. [Google Scholar] [CrossRef]
- Guide, S.V.; Gonzalez, M.E.; Bagci, I.S.; Agostini, B.; Chen, H.; Feeney, G.; Steimer, M.; Kapadia, B.; Sridhar, K.; Quesada Sanchez, L.; et al. Trial of Beremagene Geperpavec (B-VEC) for Dystrophic Epidermolysis Bullosa. N. Engl. J. Med. 2022, 387, 2211–2219. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.Y.; Marinkovich, M.P.; Wiss, K.; McCarthy, D.; Truesdale, A.; Chiou, A.S.; Eid, E.; McIntyre, J.K.; Bailey, I.; Furukawa, L.K.; et al. Prademagene zamikeracel for recessive dystrophic epidermolysis bullosa wounds (VIITAL): A two-centre, randomised, open-label, intrapatient-controlled phase 3 trial. Lancet 2025, 406, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Bellon, N.; Bataille, P.; Bonigen, J.; Charbit-Henrion, F.; Dietrich, C.; Polivka, L.; Hadj-Rabia, S.; Leite de Moraes, M.; Bodemer, C. Experience of dupilumab treatment in inherited epidermolysis bullosa: A short series. J. Am. Acad. Dermatol. 2024, 91, 373–376. [Google Scholar] [CrossRef]
- Dou, L.; Chen, F.; He, W.; Wang, J.; Wang, C.; Chen, X.; Peng, X.; Wang, L.; Ye, Y.; Li, M. Efficacy and Safety of Dupilumab Monotherapy in Patients with Dystrophic Epidermolysis Bullosa: A Retrospective Study of 8 Cases. J. Dermatol. 2025, 52, 1159–1165. [Google Scholar] [CrossRef]
- Natsuga, K.; Shinkuma, S.; Hsu, C.K.; Fujita, Y.; Ishiko, A.; Tamai, K.; McGrath, J.A. Current topics in Epidermolysis bullosa: Pathophysiology and therapeutic challenges. J. Dermatol. Sci. 2021, 104, 164–176. [Google Scholar] [CrossRef]
- Chan, J.M.; Weisman, A.; King, A.; Maksomski, S.; Shotwell, C.; Bailie, C.; Weaver, H.; Bodan, R.; Guerrero, E.; Zmazek, M.; et al. Occupational therapy for epidermolysis bullosa: Clinical practice guidelines. Orphanet J. Rare Dis. 2019, 14, 129. [Google Scholar] [CrossRef]
- Weisman, A.; Chan, J.M.; LaPointe, C.; Sjoholm, K.; Steinau, K.; Artus, K.; Widhiati, S.; Bodan, R.; Wood, M.; Salas-Alanis, J.C.; et al. Physiotherapy for epidermolysis bullosa: Clinical practice guidelines. Orphanet J. Rare Dis. 2021, 16, 406. [Google Scholar] [CrossRef] [PubMed]
- Feldmann, R.; Weglage, J.; Frosch, M. Cognitive function in patients with epidermolysis bullosa: Social adjustment and emotional problems. Klin. Padiatr. 2012, 224, 22–25. [Google Scholar] [CrossRef]
- Boesen, M.L.; Bygum, A.; Hertz, J.M.; Zachariassen, G. Newborn with severe epidermolysis bullosa: To treat or not to treat? BMJ Case Rep. 2016, 2016, bcr2016214727. [Google Scholar] [CrossRef]
- Goldschneider, K.R.; Lucky, A.W. Pain management in epidermolysis bullosa. Dermatol. Clin. 2010, 28, 273–282. [Google Scholar] [CrossRef]
- Manjunath, S.; Mahajan, R.; De, D.; Handa, S.; Attri, S.; Behera, B.N.; Bhasin, S.L.; Bolia, R. The severity of malnutrition in children with epidermolysis bullosa correlates with disease severity. Sci. Rep. 2021, 11, 16827. [Google Scholar] [CrossRef] [PubMed]
- El Hachem, M.; Caldaro, T.; Lara-Corrales, I.; Pope, E.; Jones, R.; Bageta, M.L.; Heaton, J.; Martinez, A.E.; Ferreira da Rocha, A.C.; Bodemer, C.; et al. Management of oesophageal strictures in inherited epidermolysis bullosa: A clinical practice guideline. Br. J. Dermatol. 2025, 193, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K. Management of infant epidermolysis bullosa with daily life guidance for parents and cooperation with visiting nurses. Jpn. WOCM 2014, 18, 354–357. [Google Scholar]
- Kwon, A.; Hwang, A.; Miller, C.H.; Reimer-Taschenbrecker, A.; Paller, A.S. Osteoporosis and bone health in pediatric patients with epidermolysis bullosa: A scoping review. Pediatr. Dermatol. 2024, 41, 385–402. [Google Scholar] [CrossRef]
- Case-Smith, J.; Arbesman, M. Evidence-based review of interventions for autism used in or of relevance to occupational therapy. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2008, 62, 416–429. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.J.; Anzalone, M.E.; Lane, S.J.; Cermak, S.A.; Osten, E.T. Concept evolution in sensory integration: A proposed nosology for diagnosis. Am. J. Occup. Ther. Off. Publ. Am. Occup. Ther. Assoc. 2007, 61, 135–140. [Google Scholar] [CrossRef]
- Della Longa, L.; Gliga, T.; Farroni, T. Tune to touch: Affective touch enhances learning of face identity in 4-month-old infants. Dev. Cogn. Neurosci. 2019, 35, 42–46. [Google Scholar] [CrossRef]
- Als, H. A synactive model of neonatal behavioral organization. Phys. Occup. Ther. Pediatr. 1986, 6, 3–55. [Google Scholar] [CrossRef]
- Pajardi, G.; Pivato, G.; Rafanelli, G. Rehabilitation in recessive dystrophic epidermolysis bullosa. Tech. Hand Up. Extrem. Surg. 2001, 5, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Winnicott, D. The Maturational Processes and the Facilitating Environment: Studies in the Theory of Emotional Development; International Universities Press: London, UK, 1965. [Google Scholar]
| Normal Motor Development | Standard | Case |
|---|---|---|
| Head rotation in supine | 1 Mo | 3 Mo |
| Brief head lift in prone | 6 Mo | |
| Grasping objects placed in the hand | 4 Mo | 6 Mo |
| Supporting head on elbows in prone | 5 Mo | 7 Mo |
| Sitting with hands supporting the body for several seconds | 6 Mo | 9 Mo |
| Grasping feet in supine | 10 Mo | |
| Reaching out to grasp objects | 6 Mo | |
| Supporting body weight with one hand in prone (and reaching with the other) | 7 Mo | 9 Mo |
| Reaching for objects to the side while seated | 8 Mo | 9 Mo |
| Visual tracking and person recognition | 7 Mo | |
| Maintaining seated position | 10 Mo |
| Phase (Postnatal Days) | Developmental/Clinical Issues | Restriction Status | Habilitation/Rehabilitation Strategy |
|---|---|---|---|
| I (81–107) | Mobility restricted by wound dressings (elbow, knee). Limb growth delay. Constant supine posture. Hypertonicity in the lower back. | Habilitation/Rehabilitation contact allowed. | (a) Positioning: To facilitate spontaneous activities. (b) Minimal Range-of-Motion (ROM) exercises. |
| II (108–180) | Developmental delay: Partial neck control. Exacerbation of tracheomalacia requiring CPAP administration. | Positioning restrictions gradually eased. | (a) Minimal-contact motor development procedures (including sitting training). (b) Non-physical pulmonary rehabilitation. |
| III (181–240) | Developmental delay: Inability to lift head in prone, limited object grasp/visual tracking. Impaired thoracic muscle flexibility/coordination. Exacerbation of tracheomalacia requiring SiPAP administration. | Any training with contact allowed (with minimal amount). | (a) Initial assessment of motor development and functional issues. (b) Gross motor training. (c) Hands-on respiratory rehabilitation. (d) Focused instruction for caregivers (e.g., assisted sitting position). |
| IV (241–310) | Developmental delay in gross and fine motor skills. Insufficient upper limb and trunk coordination. | Specific restrictions eliminated. | (a) Gross motor training. (b) Trunk–upper limb coordination training. (c) Further structuring of the inpatient living environment. |
| V (311) (Discharge) | Developmental delay: Partial sitting achieved; crawling and standing not acquired. Mild hypertonicity and mild ROM restriction in the trunk. | Home Discharge. | Caregiver Instruction: Ensure sensory input (fingers, buttocks, plantar surface); recognize center of gravity; positioning to facilitate upper limb and abdominal muscle movements; prone posture; trunk ROM with reaching training; gross motor development. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sakai, T.; Tashiro, S.; Karasuyama, A.; Kimura, T.; Narita, M.; Yamada, S. Rehabilitation Intervention for an Infant with Simple Epidermolysis Bullosa from NICU to Home Discharge: A Case Report. J. Clin. Med. 2025, 14, 8012. https://doi.org/10.3390/jcm14228012
Sakai T, Tashiro S, Karasuyama A, Kimura T, Narita M, Yamada S. Rehabilitation Intervention for an Infant with Simple Epidermolysis Bullosa from NICU to Home Discharge: A Case Report. Journal of Clinical Medicine. 2025; 14(22):8012. https://doi.org/10.3390/jcm14228012
Chicago/Turabian StyleSakai, Tetsuo, Syoichi Tashiro, Aki Karasuyama, Toshihiko Kimura, Masami Narita, and Shin Yamada. 2025. "Rehabilitation Intervention for an Infant with Simple Epidermolysis Bullosa from NICU to Home Discharge: A Case Report" Journal of Clinical Medicine 14, no. 22: 8012. https://doi.org/10.3390/jcm14228012
APA StyleSakai, T., Tashiro, S., Karasuyama, A., Kimura, T., Narita, M., & Yamada, S. (2025). Rehabilitation Intervention for an Infant with Simple Epidermolysis Bullosa from NICU to Home Discharge: A Case Report. Journal of Clinical Medicine, 14(22), 8012. https://doi.org/10.3390/jcm14228012






