Adding Multimedia Animations to Exercise Therapy Provides No Additional Benefit for Rotator Cuff–Related Shoulder Pain: A Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Participants
2.3. Sample Size
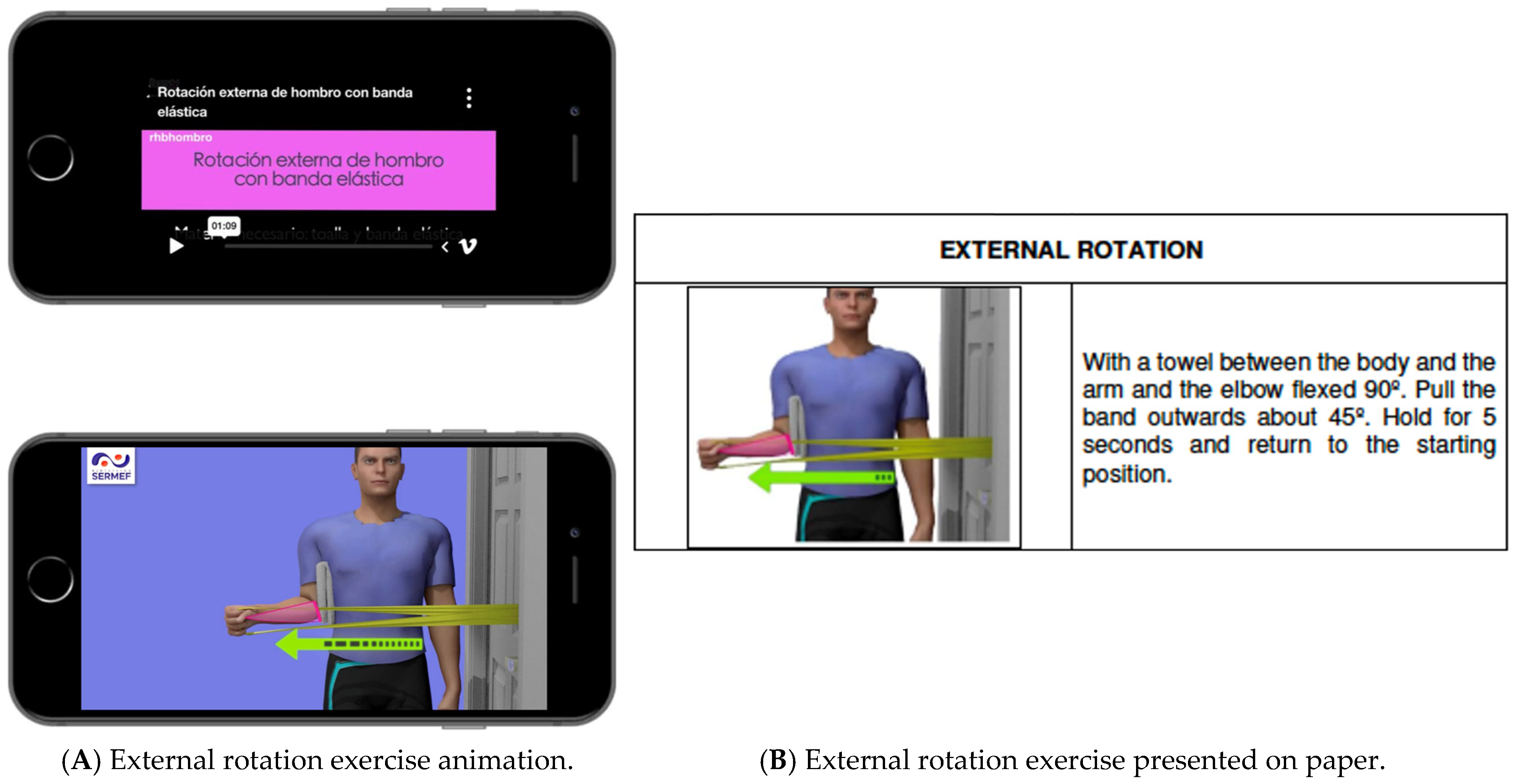
2.4. Interventions
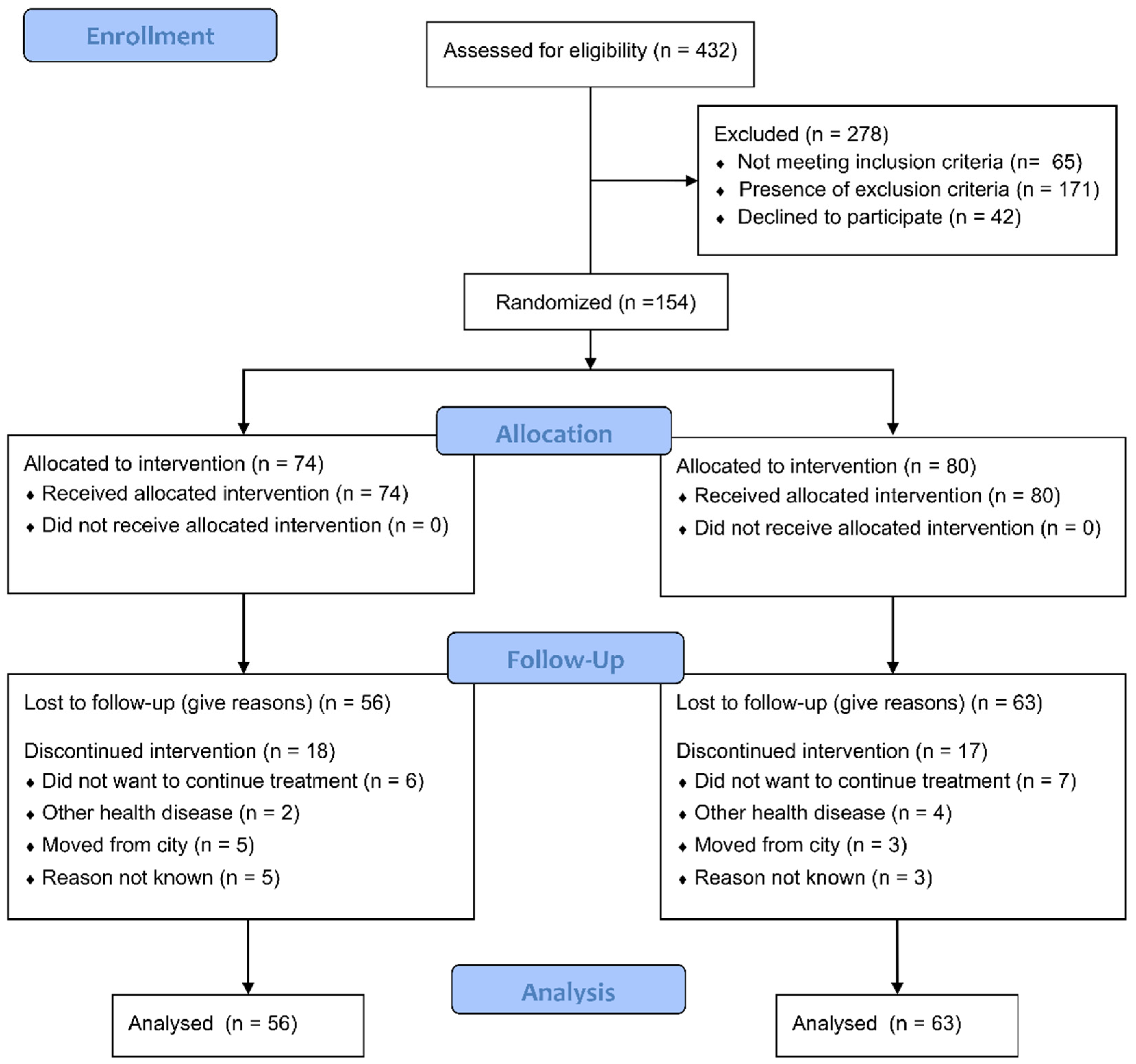
2.5. Randomization and Blinding
2.6. Outcomes
2.7. Statistical Analyses
3. Results
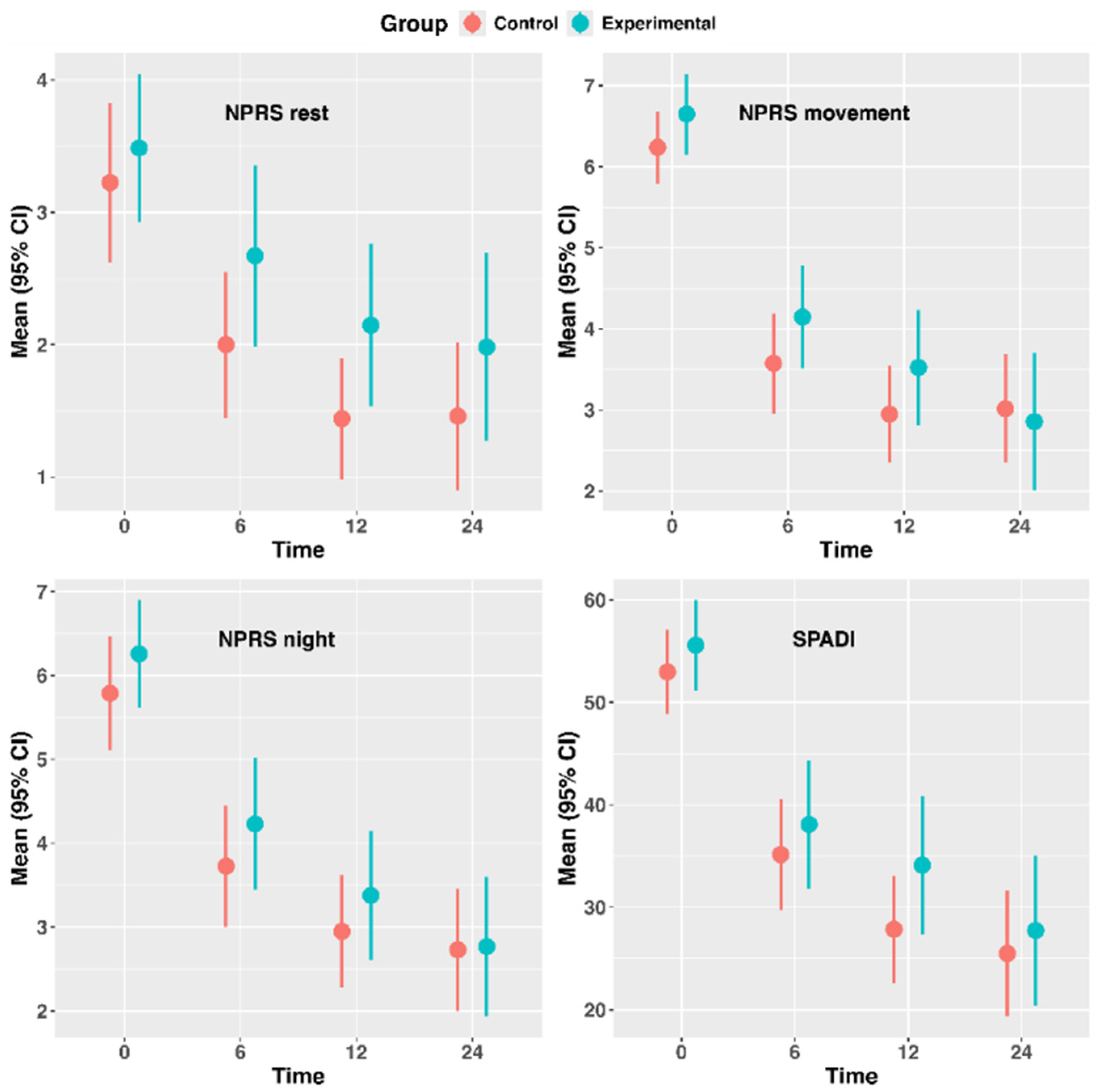
3.1. Between-Group Differences in Shoulder Pain and Disability Outcomes
3.2. Between-Group Differences in Perceived Improvement, Satisfaction and Expectations with Received Treatment and Adherence to the Exercise Program
3.3. Web-Based Application Perceptions
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CERT | Consensus on Exercise Reporting Template |
| NPRS | Numeric Pain Rating Scale |
| PGI-I | Patient Global Impression of Improvement |
| SPADI | Shoulder Pain and Disability Index |
| SUS | System Usability Scale |
| RCRSP | Rotator Cuff-Related Shoulder Pain |
References
- Lucas, J.; van Doorn, P.; Hegedus, E.; Lewis, J.; van der Windt, D. A Systematic Review of the Global Prevalence and Incidence of Shoulder Pain. BMC Musculoskelet. Disord. 2022, 23, 1073. [Google Scholar] [CrossRef]
- Hermans, J.; Luime, J.J.; Meuffels, D.E.; Reijman, M.; Simel, D.L.; Bierma-Zeinstra, S.M.A. Does This Patient With Shoulder Pain Have Rotator Cuff Disease? JAMA 2013, 310, 837. [Google Scholar] [CrossRef]
- Lewis, J. Rotator Cuff Related Shoulder Pain: Assessment, Management and Uncertainties. Man. Ther. 2016, 23, 57–68. [Google Scholar] [CrossRef]
- Sørensen, L.; van Tulder, M.; Johannsen, H.V.; Ovesen, J.; Enemark, U.; Blæhr, E.E.; Oestergaard, L.G. Costs of Shoulder Disorders in Denmark: A Nationwide Cost-of-Illness Study Investigating 617,334 Patients and Matched Controls. Pain 2022, 163, 2162–2171. [Google Scholar] [CrossRef] [PubMed]
- Parikh, N.; Martinez, D.J.; Winer, I.; Costa, L.; Dua, D.; Trueman, P. Direct and Indirect Economic Burden Associated with Rotator Cuff Tears and Repairs in the US. Curr. Med. Res. Opin. 2021, 37, 1199–1211. [Google Scholar] [CrossRef]
- Monrad, N.; Ganestam, A.; Kallemose, T.; Barfod, K.W. Alarming Increase in the Registration of Degenerative Rotator Cuff-Related Lesions a Nationwide Epidemiological Study Investigating 244,519 Patients. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 188–194. [Google Scholar] [CrossRef] [PubMed]
- Lowry, V.; Lavigne, P.; Zidarov, D.; Matifat, E.; Cormier, A.A.; Desmeules, F. A Systematic Review of Clinical Practice Guidelines on the Diagnosis and Management of Various Shoulder Disorders. Arch. Phys. Med. Rehabil. 2023, 105, 411–426. [Google Scholar] [CrossRef] [PubMed]
- Kingston, G.; Gray, M.A.; Williams, G. A Critical Review of the Evidence on the Use of Videotapes or DVD to Promote Patient Compliance with Home Programmes. Disabil. Rehabil. Assist. Technol. 2010, 5, 153–163. [Google Scholar] [CrossRef]
- Emmerson, K.B.; Harding, K.E.; Taylor, N.F. Providing Exercise Instructions Using Multimedia May Improve Adherence but Not Patient Outcomes: A Systematic Review and Meta-Analysis. Clin. Rehabil. 2019, 33, 607–618. [Google Scholar] [CrossRef]
- O’Shea, A.; Drennan, J.; Littlewood, C.; Slater, H.; Sim, J.; McVeigh, J.G. Barriers and Facilitators Related to Self-Management of Shoulder: A Systematic Review and Qualitative Synthesis. Clin. Rehabil. 2022, 36, 1539. [Google Scholar] [CrossRef]
- Dickson, C.; de Zoete, R.M.J.; Berryman, C.; Weinstein, P.; Chen, K.K.; Rothmore, P. Patient-Related Barriers and Enablers to the Implementation of High-Value Physiotherapy for Chronic Pain: A Systematic Review. Pain. Med. 2023, 25, 104–115. [Google Scholar] [CrossRef]
- Burns, D.; Boyer, P.; Razmjou, H.; Richards, R.; Whyne, C. Adherence Patterns and Dose Response of Physiotherapy for Rotator Cuff Pathology: Longitudinal Cohort Study. JMIR Rehabil Assist. Technol. 2021, 8, e21374. [Google Scholar] [CrossRef]
- Major, D.H.; Røe, Y.; Grotle, M.; Jessup, R.L.; Farmer, C.; Småstuen, M.C.; Buchbinder, R. Content Reporting of Exercise Interventions in Rotator Cuff Disease Trials: Results from Application of the Consensus on Exercise Reporting Template (CERT). BMJ Open Sport. Exerc. Med. 2019, 5, e000656. [Google Scholar] [CrossRef]
- Kucksdorf, J.J.; Bartley, J.; Rhon, D.I.; Young, J.L. Reproducibility of Exercise Interventions in Randomized Controlled Trials for the Treatment of Rotator Cuff-Related Shoulder Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2023, 105, 770–780. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G. CONSORT 2010 Explanation and Elaboration: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Pérez-Porta, I.; Flórez-García, M.T.; García-Pérez, F.; Fernández-Matías, R.; Pérez-Manzanero, M.Á.; Araujo-Narváez, A.M.; Urraca-Gesto, M.A.; Fernández-Lagarejos, C.; Plaza-Manzano, G.; Pérez-Fernández, E.; et al. Effects of a Web Application Based on Multimedia Animations to Support Therapeutic Exercise for Rotator Cuff-Related Shoulder Pain: Protocol for an Open-Label Randomised Controlled Trial. BMJ Open 2024, 14, e085381–e085386. [Google Scholar] [CrossRef] [PubMed]
- Watts, A.R.; Williams, B.; Kim, S.W.; Bramwell, D.C.; Krishnan, J. Shoulder Impingement Syndrome: A Systematic Review of Clinical Trial Participant Selection Criteria. Shoulder Elb. 2017, 9, 31–41. [Google Scholar] [CrossRef]
- Membrilla-Mesa, M.D.; Cuesta-Vargas, A.I.; Pozuelo-Calvo, R.; Tejero-Fernández, V.; Martín-Martín, L.; Arroyo-Morales, M. Shoulder Pain and Disability Index: Cross Cultural Validation and Evaluation of Psychometric Properties of the Spanish Version. Health Qual. Life Outcomes 2015, 13, 200. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of Adult Pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthr. Care Res. 2011, 63, S240–S252. [Google Scholar] [CrossRef]
- Del Rocio Sevilla-Gonzalez, M.; Loaeza, L.M.; Lazaro-Carrera, L.S.; Ramirez, B.B.; Rodríguez, A.V.; Peralta-Pedrero, M.L.; Almeda-Valdes, P. Spanish Version of the System Usability Scale for the Assessment of Electronic Tools: Development and Validation. JMIR Hum. Factors 2020, 7, e21161. [Google Scholar] [CrossRef] [PubMed]
- Lafrance, S.; Charron, M.; Roy, J.S.; Dyer, J.O.; Frémont, P.; Dionne, C.E.; MacDermid, J.C.; Tousignant, M.; Rochette, A.; Doiron-Cadri, P.; et al. Diagnosing, Managing, and Supporting Return to Work of Adults With Rotator Cuff Disorders: A Clinical Practice Guideline. J. Orthop. Sports Phys. Ther. 2022, 52, 647–664. [Google Scholar] [CrossRef]
- Powell, J.K.; Lewis, J.; Schram, B.; Hing, W. Is Exercise Therapy the Right Treatment for Rotator Cuff-Related Shoulder Pain? Uncertainties, Theory, and Practice. Musculoskelet. Care 2024, 22, e1879. [Google Scholar] [CrossRef] [PubMed]
- Dubé, M.O.; Lafrance, S.; Charron, M.; Mekouar, M.; Desmeules, F.; McCreesh, K.; Michener, L.A.; Grimes, J.; Shanley, E.; Roy, J.S. FITT Odyssey: A Scoping Review of Exercise Programs for Managing Rotator Cuff–Related Shoulder Pain. J. Orthop. Sports Phys. Ther. 2024, 54, 513–529. [Google Scholar] [CrossRef]
- Roddey, T.S.; Olson, S.L.; Gartsman, G.M.; Hanten, W.P.; Cook, K.F. A Randomized Controlled Trial Comparing 2 Instructional Approaches to Home Exercise Instruction Following Arthroscopic Full-Thickness Rotator Cuff Repair Surgery. J. Orthop. Sports Phys. Ther. 2002, 32, 548–559. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Chuang, T.Y.; Lin, P.C.; Lin, Y.K.; Chuang, Y.H. Effects of Messages Delivered by Mobile Phone on Increasing Compliance With Shoulder Exercises Among Patients With a Frozen Shoulder. J. Nurs. Scholarsh. 2017, 49, 429–437. [Google Scholar] [CrossRef]
- Maxwell, C.; Salsberg, J.; Robinson, K.; Desmeules, F.; Lowry, V.; Tetreault, C.; McCreesh, K. Fostering Adherence to Evidence-Based Care in the Management of Musculoskeletal Shoulder Pain: A Mixed-Methods Study. Phys. Ther. 2025, 105, pzae176. [Google Scholar] [CrossRef] [PubMed]
- Areerak, K.; Waongenngarm, P.; Janwantanakul, P. Factors Associated with Exercise Adherence to Prevent or Treat Neck and Low Back Pain: A Systematic Review. Musculoskelet. Sci. Pr. 2021, 52, 102333. [Google Scholar] [CrossRef]
- Malliaras, P.; Cridland, K.; Hopmans, R.; Ashton, S.; Littlewood, C.; Page, R.; Harris, I.; Skouteris, H.; Haines, T. Internet and Telerehabilitation-Delivered Management of Rotator Cuff–Related Shoulder Pain (INTEL Trial): Randomized Controlled Pilot and Feasibility Trial. JMIR mHealth uHealth 2020, 8, e24311. [Google Scholar] [CrossRef]
- Pak, S.S.; Janela, D.; Freitas, N.; Costa, F.; Moulder, R.; Molinos, M.; Areias, A.C.; Bento, V.; Cohen, S.P.; Yanamadala, V.; et al. Comparing Digital to Conventional Physical Therapy for Chronic Shoulder Pain: Randomized Controlled Trial. J. Med Internet Res. 2023, 25, e49236. [Google Scholar] [CrossRef]
- Timurtaş, E.; Selçuk, H.; Kartal, G.; Demirbüken, İ.; Polat, M.G. A Randomized Controlled Trial: Mobile App vs Videoconference Telerehabilitation for Rotator Cuff Tendinopathy. J. Telemed. Telecare 2025. [Google Scholar] [CrossRef]
| Group | Control (n = 80) | Experimental (n = 74) | ||||
|---|---|---|---|---|---|---|
| Variable | N | Mean | SD | N | Mean | SD |
| Age, years | 80 | 55.3 | 11.1 | 74 | 54.6 | 12.9 |
| BMI | 80 | 26.9 | 4.5 | 72 | 26.4 | 4.4 |
| Sex, Male | 29 | 36.2% | 34 | 45.9% | ||
| Education | ||||||
| Primary | 26 | 32.5% | 25 | 33.8% | ||
| Secondary | 21 | 26.3% | 27 | 36.5% | ||
| No education | 1 | 1.3% | ||||
| University | 32 | 40.0% | 22 | 29.7% | ||
| Pain side | ||||||
| Left | 25 | 31.3% | 28 | 37.8% | ||
| Right | 55 | 68.8% | 46 | 62.2% | ||
| Pain side equal dominant side | 53 | 66.3% | 46 | 62.2% | ||
| Previous PT | 3 | 3.8% | 6 | 8.1% | ||
| Previous analgesic | 34 | 42.5% | 42 | 56.8% | ||
| Group | Time | n | Mean | SD | Median | P25 | P75 | Min. | Max. |
|---|---|---|---|---|---|---|---|---|---|
| NPRS, rest | |||||||||
| Control | Baseline | 80 | 3.23 | 2.70 | 3 | 0.75 | 5 | 0 | 9 |
| 6 wk | 73 | 2 | 2.37 | 1 | 0 | 3 | 0 | 8 | |
| 12 wk | 59 | 1.44 | 1.75 | 1 | 0 | 2 | 0 | 6 | |
| 24 wk | 63 | 1.46 | 2.22 | 1 | 0 | 2 | 0 | 10 | |
| Experimental | Baseline | 74 | 3.49 | 2.42 | 4 | 2 | 5 | 0 | 10 |
| 6 wk | 61 | 2.67 | 2.67 | 1 | 0 | 5 | 0 | 9 | |
| 12 wk | 61 | 2.15 | 2.40 | 1 | 0 | 3 | 0 | 9 | |
| 24 wk | 56 | 1.98 | 2.65 | 1 | 0 | 3 | 0 | 9 | |
| NPRS, movement | |||||||||
| Control | Baseline | 80 | 6.24 | 1.99 | 6 | 5 | 8 | 0 | 10 |
| 6 wk | 73 | 3.58 | 2.64 | 3 | 2 | 5 | 0 | 10 | |
| 12 wk | 59 | 2.95 | 2.30 | 3 | 1 | 4.5 | 0 | 9 | |
| 24 wk | 63 | 3.02 | 2.66 | 2 | 1 | 4.5 | 0 | 10 | |
| Experimental | Baseline | 74 | 6.65 | 2.15 | 7 | 5 | 8 | 0 | 10 |
| 6 wk | 61 | 4.15 | 2.48 | 4 | 3 | 6 | 0 | 9 | |
| 12 wk | 61 | 3.52 | 2.77 | 3 | 1 | 6 | 0 | 9 | |
| 24 wk | 56 | 2.86 | 3.15 | 2 | 0 | 5.25 | 0 | 10 | |
| NPRS, night | |||||||||
| Control | Baseline | 80 | 5.79 | 3.06 | 6 | 3 | 8 | 0 | 10 |
| 6 wk | 73 | 3.72 | 3.08 | 3 | 1 | 7 | 0 | 10 | |
| 12 wk | 59 | 2.95 | 2.57 | 2 | 1 | 5 | 0 | 8 | |
| 24 wk | 63 | 2.73 | 2.88 | 2 | 0 | 4 | 0 | 10 | |
| Experimental | Baseline | 74 | 6.26 | 2.77 | 7 | 5 | 8 | 0 | 10 |
| 6 wk | 61 | 4.23 | 3.07 | 4 | 2 | 7 | 0 | 10 | |
| 12 wk | 61 | 3.38 | 3.01 | 3 | 1 | 6 | 0 | 10 | |
| 24 wk | 56 | 2.77 | 3.11 | 1.5 | 0 | 5.25 | 0 | 9 | |
| SPADI | |||||||||
| Control | Baseline | 80 | 52.96 | 18.62 | 51.57 | 40.58 | 67.11 | 9.23 | 89.17 |
| 6 wk | 73 | 35.13 | 23.09 | 29.23 | 16.15 | 58.46 | 0 | 92.5 | |
| 12 wk | 59 | 27.84 | 20.10 | 27.69 | 10.39 | 43.59 | 0 | 86.92 | |
| 24 wk | 63 | 25.48 | 24.37 | 20.77 | 5.39 | 34.62 | 0 | 96.92 | |
| Experimental | Baseline | 74 | 55.58 | 18.99 | 59.23 | 43.65 | 68.08 | 16.92 | 90.78 |
| 6 wk | 61 | 38.08 | 24.29 | 36.15 | 16.15 | 61.67 | 0 | 84.62 | |
| 12 wk | 60 | 34.10 | 26.13 | 27.69 | 12.07 | 58.08 | 0 | 87.69 | |
| 24 wk | 56 | 27.73 | 27.47 | 18.08 | 3.66 | 47.69 | 0 | 90 | |
| Patient’s expectations | |||||||||
| Control | Baseline | 78 | 8.83 | 1.45 | 9 | 8 | 10 | 2 | 10 |
| 3 wk | 74 | 8.81 | 1.58 | 9 | 8 | 10 | 2 | 10 | |
| 6 wk | 69 | 8.54 | 1.93 | 9 | 8 | 10 | 2 | 10 | |
| Experimental | Baseline | 72 | 8.65 | 1.91 | 9 | 8 | 10 | 1 | 10 |
| 3 wk | 66 | 8.15 | 1.99 | 9 | 8 | 10 | 2 | 10 | |
| 6 wk | 59 | 8.19 | 2.51 | 9 | 8 | 10 | 0 | 10 | |
| Patient’s satisfaction | |||||||||
| Control | 6 wk | 69 | 7.91 | 1.96 | 8 | 7 | 9 | 2 | 10 |
| 24 wk | 53 | 7.89 | 1.94 | 8 | 7 | 10 | 3 | 10 | |
| Experimental | 6 wk | 59 | 7.76 | 2.35 | 8 | 7 | 10 | 0 | 10 |
| 24 wk | 51 | 7.80 | 2.32 | 9 | 6 | 10 | 1 | 10 | |
| Time | Original Dataset | Imputed Dataset | ||||
|---|---|---|---|---|---|---|
| Adjusted Between-Group Mean Difference * | Lower 95% CI | Upper 95% CI | Adjusted Between-Group Mean Difference * | Lower 95% CI | Upper 95% CI | |
| NPRS, rest | ||||||
| 6 wk | −0.49 | −1.25 | 0.27 | −0.47 | −1.25 | 0.31 |
| 12 wk | −0.17 | −0.95 | 0.61 | −0.29 | −1.02 | 0.45 |
| 24 wk | −0.37 | −1.18 | 0.43 | −0.38 | −1.23 | 0.46 |
| NPRS, movement | ||||||
| 6 wk | −0.46 | −1.35 | 0.43 | −0.32 | −1.18 | 0.54 |
| 12 wk | −0.17 | −1.08 | 0.74 | −0.18 | −1.04 | 0.67 |
| 24 wk | 0.30 | −0.64 | 1.23 | 0.16 | −0.84 | 1.15 |
| NPRS, night | ||||||
| 6 wk | −0.27 | −1.22 | 0.67 | −0.28 | −1.33 | 0.77 |
| 12 wk | 0.17 | −0.80 | 1.14 | 0.01 | −1.00 | 1.02 |
| 24 wk | 0.27 | −0.73 | 1.26 | 0.15 | −0.90 | 1.20 |
| SPADI | ||||||
| 6 wk | −0.74 | −8.25 | 6.77 | −0.86 | −8.48 | 6.76 |
| 12 wk | −1.54 | −9.22 | 6.14 | −1.72 | −8.84 | 5.41 |
| 24 wk | −0.29 | −8.16 | 7.57 | −0.54 | −9.02 | 7.93 |
| Patients’ expectations | ||||||
| 3 wk | 0.53 | −0.05 | 1.11 | 0.52 | −0.07 | 1.10 |
| 6 wk | 0.20 | −0.40 | 0.80 | 0.45 | −0.13 | 1.04 |
| Patients’ satisfaction with received treatment | ||||||
| 6 wk | 0.08 | −0.66 | 0.81 | 0.37 | −0.38 | 1.13 |
| 24 wk | −0.03 | −0.84 | 0.78 | −0.06 | −0.80 | 0.67 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Porta, I.; García-Pérez, F.; Pérez-Manzanero, M.Á.; Urraca-Gesto, M.A.; Araujo-Narváez, A.; Velasco-Arribas, M.; Navarro-Santana, M.J.; Plaza-Manzano, G.; Pérez-Fernández, E.; Flórez-García, M.T. Adding Multimedia Animations to Exercise Therapy Provides No Additional Benefit for Rotator Cuff–Related Shoulder Pain: A Randomized Clinical Trial. J. Clin. Med. 2025, 14, 7964. https://doi.org/10.3390/jcm14227964
Pérez-Porta I, García-Pérez F, Pérez-Manzanero MÁ, Urraca-Gesto MA, Araujo-Narváez A, Velasco-Arribas M, Navarro-Santana MJ, Plaza-Manzano G, Pérez-Fernández E, Flórez-García MT. Adding Multimedia Animations to Exercise Therapy Provides No Additional Benefit for Rotator Cuff–Related Shoulder Pain: A Randomized Clinical Trial. Journal of Clinical Medicine. 2025; 14(22):7964. https://doi.org/10.3390/jcm14227964
Chicago/Turabian StylePérez-Porta, Irene, Fernando García-Pérez, María Ángeles Pérez-Manzanero, María Alicia Urraca-Gesto, Aurora Araujo-Narváez, María Velasco-Arribas, Marcos José Navarro-Santana, Gustavo Plaza-Manzano, Elia Pérez-Fernández, and Mariano Tomás Flórez-García. 2025. "Adding Multimedia Animations to Exercise Therapy Provides No Additional Benefit for Rotator Cuff–Related Shoulder Pain: A Randomized Clinical Trial" Journal of Clinical Medicine 14, no. 22: 7964. https://doi.org/10.3390/jcm14227964
APA StylePérez-Porta, I., García-Pérez, F., Pérez-Manzanero, M. Á., Urraca-Gesto, M. A., Araujo-Narváez, A., Velasco-Arribas, M., Navarro-Santana, M. J., Plaza-Manzano, G., Pérez-Fernández, E., & Flórez-García, M. T. (2025). Adding Multimedia Animations to Exercise Therapy Provides No Additional Benefit for Rotator Cuff–Related Shoulder Pain: A Randomized Clinical Trial. Journal of Clinical Medicine, 14(22), 7964. https://doi.org/10.3390/jcm14227964







