The Effect of Methamphetamine Use on Radiographic Vasospasm Following Angiogram-Negative Subarachnoid Hemorrhage: A Preliminary Retrospective Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design and Setting
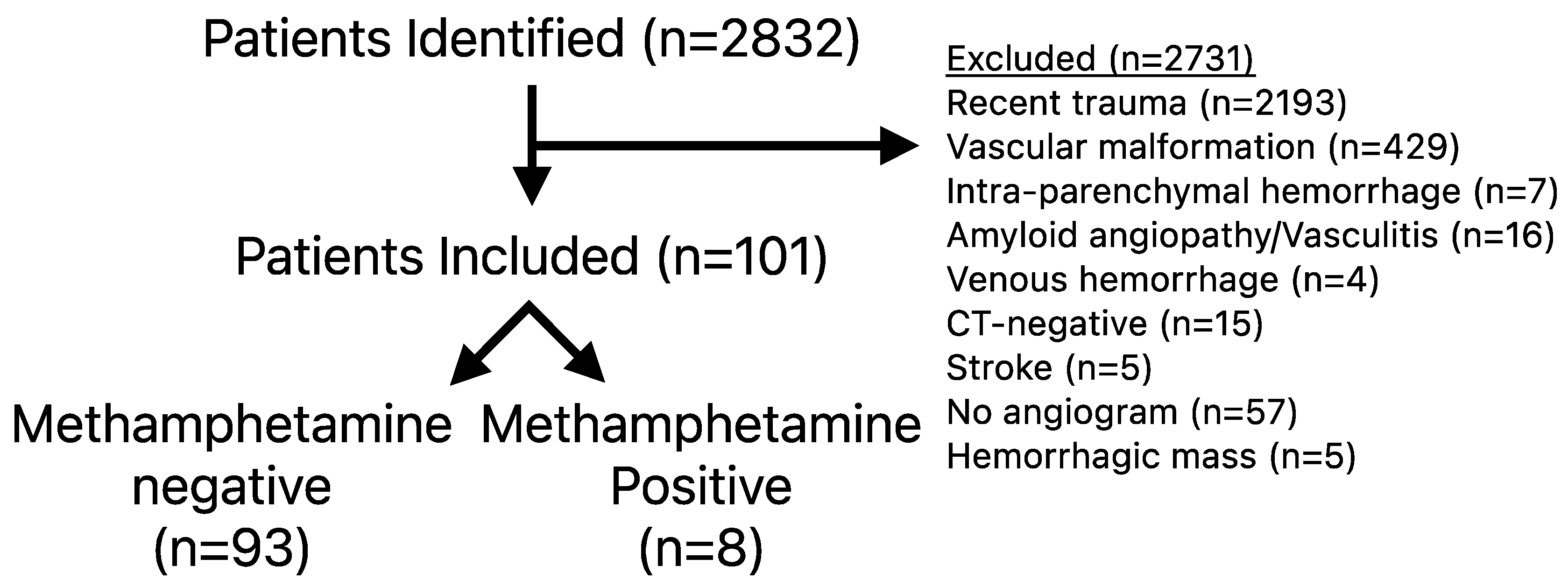
2.2. Subject Selection
2.3. Measures and Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data availability statement
Conflicts of Interest
References
- Han, B.; Compton, W.M.; Jones, C.M.; Einstein, E.B.; Volkow, N.D. Methamphetamine Use, Methamphetamine Use Disorder, and Associated Overdose Deaths Among US Adults. JAMA Psychiatry 2021, 78, 1329–1342. [Google Scholar] [CrossRef]
- Jones, C.M.; Compton, W.M.; Mustaquim, D. Morbidity and Mortality Weekly Report Patterns and Characteristics of Methamphetamine Use Among Adults United States, 2015–2018. Morb. Mortal. Wkly. Rep. 2020, 69, 317–323. [Google Scholar] [CrossRef]
- Huang, M.-C.; Yang, S.-Y.; Kuo, C.-J.; Huang, M.-C.; Chen, K.-Y.; Chen, Y.-Y.; Hung, Y.-N. Risk of Cardiovascular Diseases and Stroke Events in Methamphetamine Users: A 10-Year Follow-Up Study. J. Clin. Psychiatry 2016, 77, 1396–1403. [Google Scholar] [CrossRef]
- Noblett, D.; Hacein-Bey, L.; Waldau, B.; Ziegler, J.; Dahlin, B.; Chang, J. Increased rupture risk in small intracranial aneurysms associated with methamphetamine use. Interv. Neuroradiol. 2020, 27, 75–80. [Google Scholar] [CrossRef]
- Zhu, Z.; Osman, S.; Stradling, D.; Shafie, M.; Yu, W. Clinical characteristics and outcomes of methamphetamine-associated versus non-methamphetamine intracerebral hemorrhage. Sci. Rep. 2020, 10, 6375. [Google Scholar] [CrossRef] [PubMed]
- De Silva, D.A.; Wong, M.C.; Lee, M.P.; Chen, C.L.-H.; Chang, H.M. Amphetamine-Associated Ischemic Stroke: Clinical Presentation and Proposed Pathogenesis. J. Stroke Cerebrovasc. Dis. 2007, 16, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Beadell, N.C.; Thompson, E.M.; Delashaw, J.B.; Cetas, J.S. The deleterious effects of methamphetamine use on initial presentation and clinical outcomes in aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2012, 117, 781–786. [Google Scholar] [CrossRef]
- Li, K.; Barras, C.D.; Chandra, R.V.; Kok, H.K.; Maingard, J.T.; Carter, N.S.; Russell, J.H.; Lai, L.; Brooks, M.; Asadi, H. A Review of the Management of Cerebral Vasospasm After Aneurysmal Sub-arachnoid Hemorrhage. World Neurosurg. 2019, 126, 513–527. [Google Scholar] [CrossRef]
- Donaldson, L.; Edington, A.; Vlok, R.; Astono, I.; Iredale, T.; Flower, O.; Ma, A.; Davidson, K.; Delaney, A. The incidence of cerebral arterial vasospasm following aneurysmal subarachnoid haemorrhage: A systematic review and meta-analysis. Neuroradiology 2022, 64, 2381–2389. [Google Scholar] [CrossRef] [PubMed]
- Boswell, S.; Thorell, W.; Gogela, S.; Lyden, E.; Surdell, D. Angiogram-Negative Subarachnoid Hemorrhage: Outcomes Data and Review of the Literature. J. Stroke Cerebrovasc. Dis. 2013, 22, 750–757. [Google Scholar] [CrossRef]
- Chong, M.Y.; Martin, S.C.; Phang, I.; George, E.S.; Suttner, N.; Teo, M.K. The Prevalence of Cerebrovascular Abnormalities Detected in Various Diagnostic Subgroups of Spontaneous Subarachnoid Hemorrhage in the Modern Era. World Neurosurg. 2018, 111, e355–e361. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, M.K.; Gandhi, C.; Dragonette, J.; Schmidt, M.; Cole, C.; Santarelli, J.; Lehrer, R.; Al-Mufti, F.; Bowers, C.A. A comparison of frailty indices in predicting length of inpatient stay and discharge destination following angiogram-negative subarachnoid hemorrhage. Br. J. Neurosurg. 2020, 35, 402–407. [Google Scholar] [CrossRef]
- Alrohimi, A.; Davison, M.A.; Pandhi, A.; Abdulrazzak, M.A.; Wadden, D.; Bain, M.; Moore, N.; Hussain, M.S.; Toth, G. Aneurysmal Versus “Benign” Perimesencephalic Subarachnoid Hemorrhage. Stroke Vasc. Interv. Neurol. 2024, 4, e001166. [Google Scholar] [CrossRef]
- Al-Mufti, F.; Merkler, A.E.; Boehme, A.K.; Dancour, E.; May, T.; Schmidt, J.M.; Park, S.; Connolly, E.S.; Lavine, S.D.; Meyers, P.M.; et al. Functional Outcomes and Delayed Cerebral Ischemia Following Nonperimesencephalic Angiogram-Negative Subarachnoid Hemorrhage Similar to Aneurysmal Subarachnoid Hemorrhage. Neurosurgery 2017, 82, 359–364. [Google Scholar] [CrossRef]
- McIntyre, M.; Gandhi, C.; Dragonette, J.; Schmidt, M.; Cole, C.; Santarelli, J.; Lehrer, R.; Al-Mufti, F.; Bowers, C.A. Increasing Frailty Predicts Worse Outcomes and Increased Complications After Angiogram-Negative Subarachnoid Hemorrhages. World Neurosurg. 2020, 134, e181–e188. [Google Scholar] [CrossRef]
- Khwaja, A. KDIGO Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin. Pr. 2012, 120, c179–c184. [Google Scholar] [CrossRef] [PubMed]
- Student. The probable error of a mean. Biometrika 1908, 6, 1–25. [Google Scholar] [CrossRef]
- Neuhäuser, M.; Ruxton, G.D. The Choice Between Pearson’s χ2 Test and Fisher’s Exact Test for 2 × 2 Tables. Pharm. Stat. 2025, 24, e70012. [Google Scholar] [CrossRef]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar] [CrossRef]
- Moon, K.; Albuquerque, F.C.; Mitkov, M.; Ducruet, A.F.; Wilson, D.A.; Crowley, R.W.; Nakaji, P.; McDougall, C.G. Methamphetamine use is an independent predictor of poor outcome after aneurysmal subarachnoid hemorrhage. J. Neurointerv. Surg. 2014, 7, 346–350. [Google Scholar] [CrossRef]
- Aleksandrowicz, M.; Kozniewska, E. Hyponatremia as a risk factor for microvascular spasm following subarachnoid hemorrhage. Exp. Neurol. 2022, 355, 114126. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.L.; Josephson, S.A.; Lee, H.S.; Smith, W.S. Cerebrovascular Complications of Methamphetamine Abuse. Neurocrit. Care 2009, 10, 295–305. [Google Scholar] [CrossRef] [PubMed]
- O’kEefe, E.L.; Dhore-Patil, A.; Lavie, C.J. Early-Onset Cardiovascular Disease From Cocaine, Amphetamines, Alcohol, and Marijuana. Can. J. Cardiol. 2022, 38, 1342–1351. [Google Scholar] [CrossRef] [PubMed]
| Overall (n = 101) Mean ± Standard Error of the Mean (SEM) or Number (%) | MA-Negative (n = 93) | MA-Positive (n = 8) | OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Age (years) | 59.7 ± 1.2 | 60.8 ± 1.2 | 47.5 ± 3.3 | - | 0.004 |
| Male | 59 (58.4%) | 55 (59%) | 4 (50%) | 0.7 (0.2–2.9) | 0.716 |
| Ever smoker | 55 (55%) | 47 (52%) | 7 (88%) | 6.6 (0.8–55.5) | 0.068 |
| Perimesencephalic hemorrhage distribution | 51 (51%) | 49 (53%) | 2 (25%) | 0.30 (0.06–1.56) | 0.160 |
| Hunt and Hess score | 2.0 ± 0.07 | 2.0 ± 0.8 | 1.9 ± 0.2 | - | 0.585 |
| Modified Fisher Score | 2.5 ± 0.1 | 2.5 ± 0.1 | 2.6 ± 0.4 | - | 0.846 |
| World Federation of Neurological Surgeons score | 1.5 ± 0.1 | 1.6 ± 0.1 | 1.3 ± 0.2 | - | 0.149 |
| Body mass index (kg/m2) | 30.16 ± 2.08 | 29.9 ± 2.2 | 33.4 ± 3.9 | - | 0.446 |
| Frailty (mFI-11) | 1.37 ± 0.14 | 1.4 ± 0.2 | 1.3 ± 0.3 | - | 0.674 |
| Angiogram with unrelated/unruptured lesion | 13 (13%) | 12 (13%) | 1 (13%) | 0.96 (0.11–8.54) | >0.999 |
| Required ventriculostomy | 38 (38%) | 34 (37%) | 4 (50%) | 1.74 (0.41–7.39) | 0.470 |
| Neurologically intact on arrival | 68 (67%) | 62 (67%) | 6 (75%) | 1.50 (0.29–7.87) | >0.999 |
| Anti-thrombotic use | 8 (8%) | 8 (8.6%) | 0 (0.0%) | - | >0.999 |
| Aspirin use | 27 (27%) | 26 (28%) | 1 (13%) | 0.37 (0.04–3.14) | 0.678 |
| Age | Sex | Current Smoker | ANSAH Type | Modified Fisher Score | Hunt and Hess Score | Radiographic Vasospasm | Clinical Vasospasm | Intact on Discharge | Hypertonic Saline Use | Need for Shunt | Inpatient Length of Stay in Days | Days of Nicardipine | Stroke | Discharge Destination |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 56 | Male | Yes | NPH | 2 | 2 | Yes | Yes | Yes | Yes | No | 12 | 2 | Yes | Home |
| 57 | Male | Yes | NPH | 1 | 2 | Yes | Yes | No | Yes | No | 15 | 2 | Yes | Death |
| 50 | Male | Yes | NPH | 1 | 2 | Yes | No | Yes | Yes | Yes | 14 | 0 | No | Home |
| 38 | Female | Yes | NPH | 4 | 3 | Yes | Yes | Yes | Yes | Yes | 12 | 1 | No | Home |
| 49 | Male | Yes | PMH | 1 | 1 | Yes | No | Yes | Yes | No | 11 | 1 | Yes | Home |
| 54 | Female | No | NPH | 1 | 1 | Yes | Yes | Yes | Yes | No | 13 | 1 | Yes | Home |
| 30 | Female | Yes | NPH | 1 | 2 | No | No | Yes | No | No | 7 | 1 | No | Home |
| 46 | Female | Yes | PMH | 3 | 2 | Yes | No | Yes | Yes | No | 11 | 2 | No | Home |
| Overall (n = 101) Mean ± SEM or Number (%) | Meth-Negative (n = 93) | Meth-Positive (n = 8) | OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Radiographic vasospasm | 42 (41.6%) | 35 (38%) | 7 (88%) | 11.6 (1.4–98.3) | 0.008 |
| Neurologic deficit during stay (clinical vasospasm) | 30 (30%) | 26 (28%) | 4 (50%) | 2.58 (0.60–11.1) | 0.233 |
| Discharge home | 78 (77%) | 71 (77%) | 7 (88%) | 2.17 (0.25–18.6) | 0.678 |
| Repeat angiogram obtained | 87 (86%) | 79 (85%) | 8 (100%) | - | 0.595 |
| Repeat angiogram positive for culprit lesion | 2 (2%) | 2 (2.5%) | 0 (0%) | - | >0.999 |
| Intra-arterial verapamil given | 8 (8%) | 7 (7.9%) | 1 (13%) | 1.67 (0.18–15.6) | 0.511 |
| Stroke on any imaging | 30 (30%) | 26 (28%) | 4 (50%) | 2.58 (0.60–11.1) | 0.233 |
| Death within 30 days | 5 (5%) | 4 (4%) | 1 (13%) | 3.18 (0.31–32.4) | 0.344 |
| Death prior to discharge | 3 (3%) | 2 (2%) | 1 (13%) | 6.50 (0.15–0.52) | 0.221 |
| Neurologically intact on discharge | 86 (85%) | 79 (85%) | 7 (88%) | 1.24 (0.141–10.9) | >0.999 |
| Days requiring nicardipine | 1.6 ± 0.2 | 1.6 ± 0.2 | 1.5 ± 0.4 | - | 0.879 |
| Received hypertonic saline | 49 (49%) | 42 (45%) | 7 (88%) | 8.50 (1.01–71.9) | 0.028 |
| Need for shunting | 9 (9%) | 7 (8%) | 2 (25%) | 4.10 (0.69–24.2) | 0.149 |
| ICU length of stay (days) | 9.7 ± 0.5 | 9.7 ± 0.6 | 10.0 ± 0.9 | - | 0.756 |
| Ward length of stay (days) | 2.4 ± 5.2 | 2.5 ± 0.5 | 1.1 ± 0.5 | - | 0.074 |
| Hospital length of stay (days) | 12.0 ± 7.4 | 12.0 ± 0.8 | 11.9 ± 0.9 | - | 0.945 |
| Total Cost ($) | 192,615 ± 7493 | 190,807 ± 8052 | 213,419 ± 12,886 | - | 0.416 |
| Overall (n = 101) Mean ±SEM or Number (%) | Meth-Negative (n = 93) | Meth-Positive (n = 8) | OR (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Any complication | 31(31%) | 27 (29%) | 4 (50%) | 2.4 (0.6–10.5) | 0.245 |
| Stroke requiring thrombectomy | 2 (2%) | 2 (2.2%) | 0 (0.0%) | - | >0.999 |
| Positive blood culture | 3 (3%) | 3 (3.2%) | 0 (0.0%) | - | >0.999 |
| Positive cerebrospinal fluid culture | 2 (2%) | 2 (2.2%) | 0 (0.0%) | - | >0.999 |
| Urinary tract infection | 17 (17%) | 15 (16%) | 2 (25%) | 1.7 (0.3–9.4) | 0.619 |
| Vasopressor use | 6 (6%) | 5 (5.4%) | 1 (13%) | 2.5 (0.3–25.6) | 0.399 |
| ICU bounce-back | 1 (1%) | 1 (1.1%) | 0 (0.0%) | - | >0.999 |
| Groin complication | 0 (0%) | 0 (0%) | 0 (0%) | - | >0.999 |
| Non-neurosurgical surgery (excluding tracheostomy/gastrostomy) | 0 (0%) | 0 (0%) | 0 (0%) | - | >0.999 |
| Acute kidney injury | 13 (13%) | 13 (14%) | 0 (0.0%) | - | 0.592 |
| Clinical seizure | 4 (4%) | 3 (3.2%) | 1 (13%) | 4.3 (0.4–47) | 0.285 |
| Central line infection | 0 (0%) | 0 (0%) | 0 (0%) | - | >0.999 |
| Pneumonia | 4 (4%) | 3 (3.2%) | 1 (13%) | 4.3 (0.4–47) | 0.285 |
| Intubation during admission | 12 (12%) | 10 (11%) | 2 (25%) | 2.8 (0.5–16) | 0.241 |
| Gastrostomy tube | 1 (1%) | 1 (1.1%) | 0 (0%) | - | >0.999 |
| Tracheostomy tube | 1 (1%) | 1 (1.1%) | 0 (0%) | - | >0.999 |
| Pulmonary embolism | 1 (1%) | 1 (1.1%) | 0 (0%) | - | >0.999 |
| Deep vein thrombosis | 3 (3%) | 2 (2.2%) | 1 (13%) | 6.5 (0.52–81) | 0.221 |
| Radiographic Vasospasm | Clinical Vasospasm | Discharge Home | ||||
|---|---|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| Age | 1.0 (0.9–1.0) | 0.126 | 1.0 (1.0–1.1) | 0.186 | 0.9 (0.9–1.0) | 0.051 |
| Sex | 2.8 (1.0–7.6) | 0.045 | 1.3 (0.5–3.7) | 0.618 | 0.5 (0.1–2.0) | 0.345 |
| Hunt and Hess Score | ||||||
| Grade 1 | Reference | 0.040 | Reference | 0.005 | Reference | 0.002 |
| Grade 2 | 3.3 (0.8–14.4) | 0.110 | 1.6 (0.4–6.3) | 0.505 | 0.3 (0.05–2.0) | 0.224 |
| Grade 3 | 15.6 (1.8–137.1) | 0.013 | 15.2 (2.1–110.4) | 0.007 | 0.02 (0.002–0.2) | 0.003 |
| Grade 4 | 14.7 (1.4–150.4) | 0.023 | 25.0 (2.1–294.0) | 0.010 | 0.01 (0.001–0.2) | 0.003 |
| Modified Fisher Score | ||||||
| Grade 1 | Reference | 0.139 | Reference | 0.945 | Reference | 0.099 |
| Grade 2 | 1.1 (0.3–4.6) | 0.885 | 1.4 (0.3–6.9) | 0.680 | 4.2 (0.3–64.6) | 0.307 |
| Grade 3 | 0.2 (0.05–0.9) | 0.031 | 1.5 (0.4–5.9) | 0.560 | 0.2 (0.05–1.1) | 0.071 |
| Grade 4 | 0.7 (0.2–2.4) | 0.589 | 1.3 (0.3–5.1) | 0.698 | 0.9 (0.2–5.3) | 0.949 |
| Methamphetamine Use | 18.8 (1.7–210.5) | 0.017 | 5.1 (0.9–28.7) | 0.063 | 1.3 (0.1–15.6) | 0.843 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McIntyre, M.K.; Cheaney, B.; Liu, J.; Dogan, A.; Sanusi, O. The Effect of Methamphetamine Use on Radiographic Vasospasm Following Angiogram-Negative Subarachnoid Hemorrhage: A Preliminary Retrospective Analysis. J. Clin. Med. 2025, 14, 7921. https://doi.org/10.3390/jcm14227921
McIntyre MK, Cheaney B, Liu J, Dogan A, Sanusi O. The Effect of Methamphetamine Use on Radiographic Vasospasm Following Angiogram-Negative Subarachnoid Hemorrhage: A Preliminary Retrospective Analysis. Journal of Clinical Medicine. 2025; 14(22):7921. https://doi.org/10.3390/jcm14227921
Chicago/Turabian StyleMcIntyre, Matthew K., Barry Cheaney, Jesse Liu, Aclan Dogan, and Olabisi Sanusi. 2025. "The Effect of Methamphetamine Use on Radiographic Vasospasm Following Angiogram-Negative Subarachnoid Hemorrhage: A Preliminary Retrospective Analysis" Journal of Clinical Medicine 14, no. 22: 7921. https://doi.org/10.3390/jcm14227921
APA StyleMcIntyre, M. K., Cheaney, B., Liu, J., Dogan, A., & Sanusi, O. (2025). The Effect of Methamphetamine Use on Radiographic Vasospasm Following Angiogram-Negative Subarachnoid Hemorrhage: A Preliminary Retrospective Analysis. Journal of Clinical Medicine, 14(22), 7921. https://doi.org/10.3390/jcm14227921







