1. Introduction
Falls from height are classified as the second most common cause of blunt trauma, following motor vehicle accidents [
1]. They can be fatal and lead to violent death [
2,
3]. Fatal free falls (FFF) result from suicide, homicide, or accident [
4] with work-related incidents and intentional acts being the most common. These events account for a significant proportion of traumatic fatal injuries globally, comprising 23% to 56% of intentional deaths and 35% to 37% of construction work-related deaths [
5]. FFFs occur more frequently in urban settings, with balconies, buildings, and trees being the most common locations. Some studies have focused on analyzing the characteristics of individuals statistically associated with a higher occurrence of such incidents. These analyses indicate that men are most often affected, likely because they are more often involved in jobs that require work at significant heights than women. In contrast, women account for a higher proportion of suicide-related FFFs than men. The average age of individuals involved in these incidents varies considerably across studies, highlighting that people of all ages are at risk of FFFs [
6,
7].
Due to the numerous factors involved, the consequences of falls can vary. Outcomes depend on body mass, fall height, surface type, secondary impacts, point of first contact, and age-related comorbidities. The manner of the fall—whether intentional or accidental—also plays a crucial role [
8,
9]. Suicides tend to land on their feet, while accidental fallers reportedly have a higher frequency of skull and upper extremities fractures [
10]. Despite these differences, it has been observed that, in general, victims of FFF most commonly demonstrate fractures of the skull, vertebrae, and thoracic cavity, followed by fractures of the lower extremities, upper extremities, and pelvis [
11]. This suggests that victims of FFF show specific patterns of skeletal blunt force trauma. Such a distribution of injuries results from the unique force interactions involved [
12].
FFF is associated with high-energy vertical deceleration [
13]. Literature indicates that injury patterns are related to fall height and the kinetic energy at impact, as the body undergoes rapid deceleration upon striking the ground [
14]. During this process, kinetic energy is transferred to the ground and exerted back onto the body, resulting in injuries [
15]. Significant correlations have been established between the height of the fall, the energy imparted to the body during BFT, and the distribution and extent of skeletal injuries [
16].
Osseous injuries play a significant role in forensic pathology. These fractures can be identified using post-mortem computed tomography (PMCT) [
17], external body examination, and forensic autopsy. Forensic pathologists investigating victims of falls from height are required to evaluate injuries, establish correlations between injury severity and fall height, and assess the medico-legal aspects of the incident. Providing such information can be particularly challenging in several scenarios. First, in the absence of eyewitness accounts, determining whether a fall from height resulted from homicide, suicide, or an accident becomes more difficult. Another challenge arises from ambiguous injuries, which could suggest either a fall from height or other causes of violent death, such as motor vehicle accidents [
18,
19]. PMCT may play a significant role in addressing these difficulties. It serves as an essential complement to conventional autopsy in trauma victims, facilitating the detection of numerous additional injuries. PMCT has proven useful across a broad range of forensic applications, including the assessment of blunt-force injuries, firearm and sharp-force trauma, blast injuries, asphyxic injuries, pediatric deaths, and archaeological/anthropological examinations [
20,
21,
22]. However, there is a limited number of studies that include analyses of PMCT in victims of FFF and report fracture frequencies with anatomical detail. As that information might be the root of new correlations, this leaves gaps in our understanding of FFF.
Furthermore, complex pelvic injuries in fatal falls might be underreported in autopsy studies because the pelvis is not typically dissected. Using postmortem computed tomography, we identified complex blunt trauma patterns commonly associated with falls, including faller’s fractures, Bilateral pubic rami fractures, and pelvic injuries classified by the Young–Burgess system.
The faller’s fracture, typically seen in suicide jumpers, results from massive axial loading and presents as a horizontal sacral fracture with bilateral vertical extensions, forming an H-shaped pattern [
23]. Bilateral fractures of the superior and inferior pubic rami are often caused by falls in a position where the thighs are abducted [
24].
The Young–Burgess classification categorizes pelvic injuries into:
APC (anterior–posterior compression): progressing from pubic symphysis disruption to sacroiliac injury.
LC (lateral compression): associated with pubic rami and sacral ala or iliac wing fractures.
PAC (posterior–anterior compression): associated with faller’s fracture or double vertical fractures of the posterior aspect of the pelvis.
VS (vertical shear): from axial loading, causing vertical displacement of one hemipelvis and disruption of pelvic ligaments [
25,
26,
27].
This study aims to investigate whether FFF are characterized by a specific pattern of skeletal injuries that distinguishes them from other types of violent deaths. It also sought to determine whether such a pattern enables a reliable assessment of the cause and circumstances of death, thereby contributing to the improvement of postmortem diagnostics. The study includes an analysis of PMCT in FFF victims.
2. Materials and Methods
We analyzed 134 cases of fatal falls from 1 January 2016 to 7 September 2024, using the database of the Department and Institute of Forensic Medicine in Lublin, Poland.
Our inclusion criteria were death due to free fall onto hard, non-deformable surfaces. For this study, a free fall was defined as a vertical descent from a height occurring without intermediate obstacles, secondary impacts, or collisions with other structures. Falls involving multiple impacts or any intermediate obstructions (such as tree branches, balconies, or glass surfaces) were excluded from analysis. We excluded all cases of ground-level falls, defined as falls from the standing or sitting position without a vertical drop. The described injuries could not be attributed to any causes other than the fall itself. Furthermore, each analyzed case must have documented individual intrinsic variables (sex, age, body mass, height, pre-existing mental conditions, drug or alcohol use) and extrinsic variables (height of the fall, landing surface, time between the fall and death, and known cause of the fall). Any cases without complete documentation were excluded from the study. Within our department, it is standard procedure for all trauma-related cadavers to undergo PMCT before autopsy; consequently, all cases incorporated into this study had accessible scans. PMCT assessments were performed independently and blinded to autopsy results. Following both examinations, the findings were compared, and any inconsistencies were resolved during a second consensus evaluation of the available data.
Of the 134 cases initially reviewed, 16 were excluded as non–free-fall incidents (e.g., falls on stairs or falls obstructed by glass, furniture, or other objects), 13 as ground-level falls, 10 due to additional trauma sustained before the fall (such as assault or traffic accidents), and 16 because of incomplete documentation. Seventy-nine cases met the inclusion criteria for this study.
Using autopsy reports and PMCT, victims were assessed for skeletal injuries. The Department and Institute of Forensic Medicine in Lublin possess a Toshiba TSX-034A Astelion Advance Edition Computer Tomography system (Canon Medical Systems Corporation, Otawara, Tochigi, Japan) and a dedicated imaging data archiving subsystem (PACS) with scalable disk space (NAS), which provides access to all previously performed examinations. All cases were analyzed for skeletal trauma using the RadiAnt DICOM Viewer program (Version 2025.2, Medixant, 2025), which implements 3D reconstruction, alongside the Viterea diagnostic console certified for clinical diagnostics (MD) with an MD-class EIZO RX440 monitor (EIZO Corporation, Hakusan, Ishikawa, Japan).
This study’s analysis was divided into two sections based on the cause of the fall: suicide or accident. The gathered data were examined for bone fractures, first categorizing them into six main categories: head, spine, thorax, pelvis, upper limbs, and lower limbs. Fractures were further classified by creating additional anatomical subcategories, including individual bones and their respective parts. The study accounted for the height of the fall, dividing it into two classifications. The first classification is based on the literature and comprises two groups: falls from less than 3 m and falls from 3 m or more. The second classification consists of eight groups: falls less than or equal to 3 m, falls from 3 to 6 m, falls from 6 to 10 m, falls from 10 to 15 m, falls from 15 to 20 m, falls from 20 to 25 m, falls from 25 to 30 m, and falls of 30 m or higher. These groups were formed to perform a statistical analysis, as using regular intervals would yield insufficient subject numbers in each height group. In cases where the height of the fall was reported in stories instead of meters, it was assumed that a story is approximately 3 m high (3-story building = ground floor + 3 floors = 3 m + 3 × 3 m =12 m). The study also accounted for the kinetic energy of the fall, calculated from the potential energy using the formula Epot = mgh (m: body mass, g: acceleration due to gravity (9.81 m/s2), and h: height in m).
All data were analyzed using Statistica software (StatSoft, version 13), with statistical significance set at p ≤ 0.05. Depending on the type of data and its distribution (whether normal or not), various tests were employed, including Student’s t-test (T-test), Mann–Whitney U test (MWU), Chi-squared test (χ2 test), Spearman’s rank correlation coefficient (ρ), and Kruskal–Wallis test (ANOVA). To assess the influence of the studied variables, we used Binary Logistic Regression.
3. Results
Seventy-nine cases of fatal falls from height were analyzed, including 22 women (28%) and 57 men (72%). The average age was 54; the median was 55, including the minimum age of the fatal fall victim—17—and the maximum age of 93. The average BMI was 25.08 kg/m2, with a median of 24.11 kg/m2, ranging from 15.15 kg/m2 to 40.64 kg/m2.
Of the victims, 26 (32.91%) were under the influence of alcohol, including four women (18.18%) and 22 men (38.60%). The maximum concentration of alcohol in the victim’s blood was 7.48 g/L. Of the examined cases, mental illness was reported in 20 cases (25.32%), including 11 women (50%) and nine men (15.79%). The remaining 59 cases (74.68%), including 11 women (50%) and 48 men (84.21%), had no mental illness history. A psychiatric history was significantly more prevalent among females than among males (χ2 test, p = 0.0017). Additionally, individuals with mental illness tended to be under the influence of alcohol (χ2 test, p = 0.0116).
Of the examined cases of falling from a height, an accident occurred in 36 cases (45.57%), and a suicide occurred in 43 cases (54.43%). Among the deceased, there were 20 low falls (25.32%), including 2 women (9.09%) and 18 men (31.58%). Falls above 3 m were classified as high falls, which accounted for 59 cases (74.68%), including 20 female falls (90.91%) and 39 male falls (68.42%). High falls were divided into specific fall height ranges. The average fall was 22.30 m, the median was 7 m, the minimum fall height was 1.5 m, and the maximum fall height was 1000 m. Women, on average, fell from higher elevations than men (MWU, p = 0.0276); however, within the suicide group, men experienced falls from greater heights (MWU, p = 0.001).
The time of death varied from death on site- 46 cases (58.23%), including 13 among women (59.09% of surveyed women) and 33 among men (57.89%), to death after more than 10 days from fall—2 cases (2.53%), which were exclusively men (3.51%). The maximum time to death from a fall was 20 days. In one case, the exact time of death from the fall was unrecorded; however, it was known to occur within several hours. The collected data are presented in
Table 1.
Of the 79 cases of falls from height, 36 were caused by accident (45.57%), including four women (18.18% of all female falls) and 32 men (56.14% of all male falls). The minimum fall height was 1.5 m, and the maximum was 1000 m. The average height of fall was 5.94 m. Considering the presence of a parachutist who fell from a height of 1000 m in the accident, it is not included in the average due to its false inflation. The median was 4 m.
Falls from a low height occurred in 15 cases (41.67% of accident victims), all of whom were men (46.88% of accidents among men). Falls from a high height (3–15 m) occurred in 19 cases (52.78%), including 4 cases involving women (100%) and 15 among men (46.88%). Falls from a height higher than or equal to 15 m concerned 2 cases (5.56% of cases), all of which were exclusively among men (6.25% of men).
Of the accident victims, 17 of them were under the influence of alcohol (47.22% of accident victims), including one woman (25% of women) and 16 men (50% of men). Higher alcohol intoxication was statistically correlated with accidental deaths (χ
2 test,
p = 0.0133). Three victims had a documented mental illness (8.33% of accident victims), including one woman (25% women) and two men (6.25% of men). The particulars were presented in the
Table 2.
Of the 79 cases of fatal falls from height, 43 were caused by suicide (54.43%), including 18 women (81.82% of all female falls) and 25 men (43.86% of all male falls). The minimum fall height for suicide was 3 m, and the maximum was 33 m. The average height of falls was 12.88 m. The median was 9 m. Females were more likely to die by suicide, whereas males were more frequently victims of accidental falls (p = 0.0024). Additionally, a significant correlation was observed between fall height and manner of death, with suicides occurring from greater altitudes (MWU, p = 0.00013).
Falls from low height occurred in 5 cases (11.63% of suicide victims), including two among women (11.11% of women) and three among men (12% of men). Falls from a high height (3–15 m) occurred in 24 cases (55.81%), including nine among women (50%) and 15 among men (60%). Falls from a height of 15 m or higher were involved in 14 cases (32.56% of cases), including 7 cases among women (38.89% of women) and seven among men (28% of men). Furthermore, we found that suicides tend to have greater kinetic energy (MWU, p = 0.0044) and lower BMIs (MWU, p = 0.0163) than accidents.
Of the suicide victims, 9 of them were under the influence of alcohol (20.93% of suicide victims), including three among women (16.67% of women) and six among men (24% of men). Seventeen victims had documented mental illness (39.53% of suicide victims), including 10 among women (55.56% of women) and seven among men (28% of men). Psychiatric history had a positive correlation with suicide (χ
2 test,
p = 0.0015). The particulars were presented in the
Table 3.
Skull fractures occurred in 47 victims who fell from a height. We observed a bimodal distribution of skull fractures, with peaks at altitudes below 6 m and above 20 m (χ
2 test,
p = 0.010). Neurocranial fractures were more common among males (χ
2 test,
p = 0.003). Fracture frequencies are presented in
Table 4.
Positive correlation was found between maxillary fractures and both the height of the fall (MWU, p = 0.01) and its kinetic energy (MWU, p = 0.008). Additionally, fractures of the mandible showed positive correlations with the fall height category (MWU, p = 0.009) and the fall’s kinetic energy (MWU, p = 0.008). Furthermore, logistic regression analysis showed that as skull fractures increase, pelvic fractures decrease by almost 70% (OR = 1.065; 95% CI: 1.01–1.12; LRT: p = 0.011).
Comparison between injuries to the skull in suicides and accidents is shown in
Figure 1.
Table 5.
Skull fractures in accidental fatal falls.
Table 5.
Skull fractures in accidental fatal falls.
| Damaged Structure | All Cases | % of Cases | Bilateral/Complex Injury |
|---|
| Sphenoid bone | 17 | 68 | 7—complex injury |
| Body of the sphenoid bone | 10 | 40 | - |
| Greater wing of the sphenoid bone | 12 | 48 | 5 |
| Pterygoid process of the sphenoid bone | 1 | 4 | 1 |
| Temporal bone | 15 | 60 | 5 |
| Petrous part of the sphenoid bone | 9 | 36 | 4 |
| Squamous part of the sphenoid bone | 11 | 44 | 2 |
| Occipital bone | 18 | 72 | |
| Posterior part of the occipital bone | 9 | 36 | 4—Anterior + posterior part |
| Anterior part of occipital bone | 13 | 52 | |
| Maxilla | 7 | 28 | 3 |
| Frontal bone | 5 | 20 | - |
| Parietal bone | 8 | 32 | 3 |
| Nasal bone | 3 | 12 | 2 |
| Ethmoid bone | 3 | 12 | - |
| Palatine bone | 1 | 4 | 0 |
| Vomer | 3 | 12 | - |
| Zygomatic bone | 4 | 16 | 0 |
| Separation of the zygomatic bone | 2 | 8 | 1 |
| Zygomatic arch | 7 | 28 | 1 |
| Mandible | 5 | 20 | - |
| Body of the mandible | 4 | 16 | 1—Body + Left and Right ramus |
| Ramus of the mandible | 3 | 12 | 1 |
Table 6.
Skull fractures in the suicide group.
Table 6.
Skull fractures in the suicide group.
| Damaged Structure | All Cases | % of Cases | Bilateral/Complex Injury |
|---|
| Sphenoid bone | 17 | 70.83 | 8—complex injury |
| Body of the sphenoid bone | 7 | 29.17 | - |
| Greater wing of the sphenoid bone | 14 | 58.33 | 4 |
| Pterygoid process of the sphenoid bone | 1 | 4.17 | 1 |
| Temporal bone | 15 | 62.5 | 7 |
| Petrous part of the sphenoid bone | 11 | 45.83 | 6 |
| Squamous part of the sphenoid bone | 14 | 58.33 | 3 |
| Occipital bone | 9 | 37.5 | |
| Posterior part of the occipital bone | 6 | 25 | 4—Anterior + posterior part |
| Anterior part of occipital bone | 7 | 29.17 | |
| Maxilla | 12 | 50 | 5 |
| Frontal bone | 11 | 45.83 | - |
| Parietal bone | 12 | 50 | 4 |
| Nasal bone | 5 | 20.83 | 4 |
| Ethmoid bone | 5 | 20.83 | - |
| Palatine bone | 3 | 12.5 | 2 |
| Vomer | 1 | 4.17 | - |
| Zygomatic bone | 8 | 33.33 | 3 |
| Separation of the zygomatic bone | 3 | 12.5 | 1 |
| Zygomatic arch | 12 | 50 | 2 |
| Mandible | 9 | 37.5 | |
| Body of the mandible | 8 | 33.33 | 0—Body + Left and Right ramus |
| Ramus of the mandible | 2 | 8.33 | 0 |
In statistical analysis, the anterior part of the occipital bone was fractured more frequently in suicides than in accidents (χ2 test, p = 0.043).
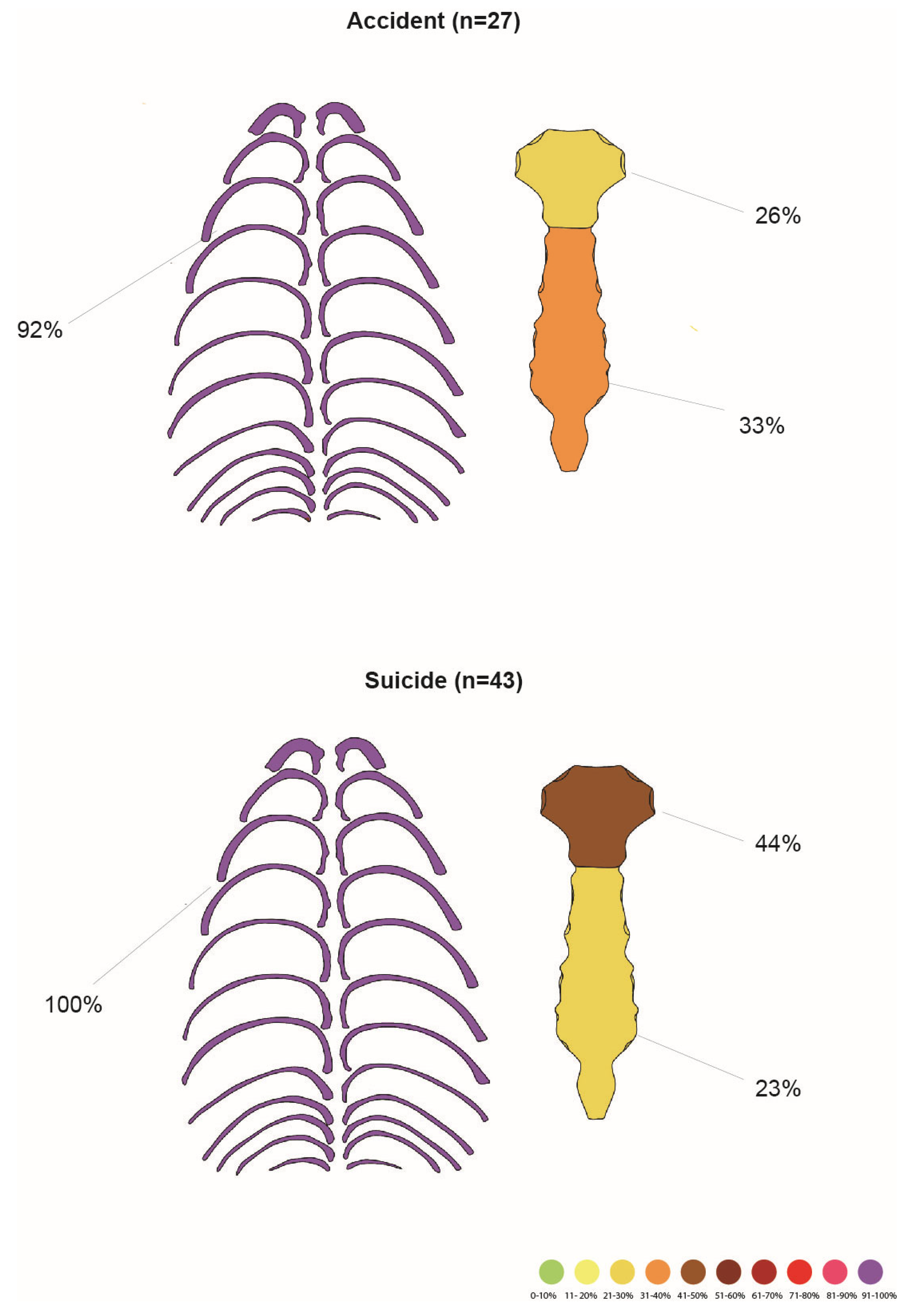
Among 79 cases of fatal falls, rib cage injury occurred in 70 cases (88.61% of all cases). The fracture frequencies in the studied population are shown in
Table 7.
Rib cage fractures increased with fall height (ANOVA, p = 0.00022) across categories of less than 3 m, 6–10 m, 20–25 m, and 25–30 m, with similar trends observed for individual rib fractures. Additionally, higher kinetic energy correlated with a greater total number of chest fractures (ρ, p = 0.0002). Males sustained rib cage fractures more frequently than females (MWU, p = 0.0066), and individuals with mental illness exhibited more severe rib cage injuries (MWU, p = 0.0123).
Among 36 victims of the accident, 27 had a rib cage injury (75% of all accident victims). No statistical correlation was found between the height of the fall and rib cage injuries (MWU,
p = 0.513). Fracture frequencies are presented in
Table 8 and
Figure 2.
All 43 suicide fall victims suffered chest injuries. Bilateral rib fractures were significantly more frequent in suicides, while unilateral fractures were more prevalent in accidents (χ
2 test,
p = 0.0001). Fracture frequencies are presented in
Table 9.
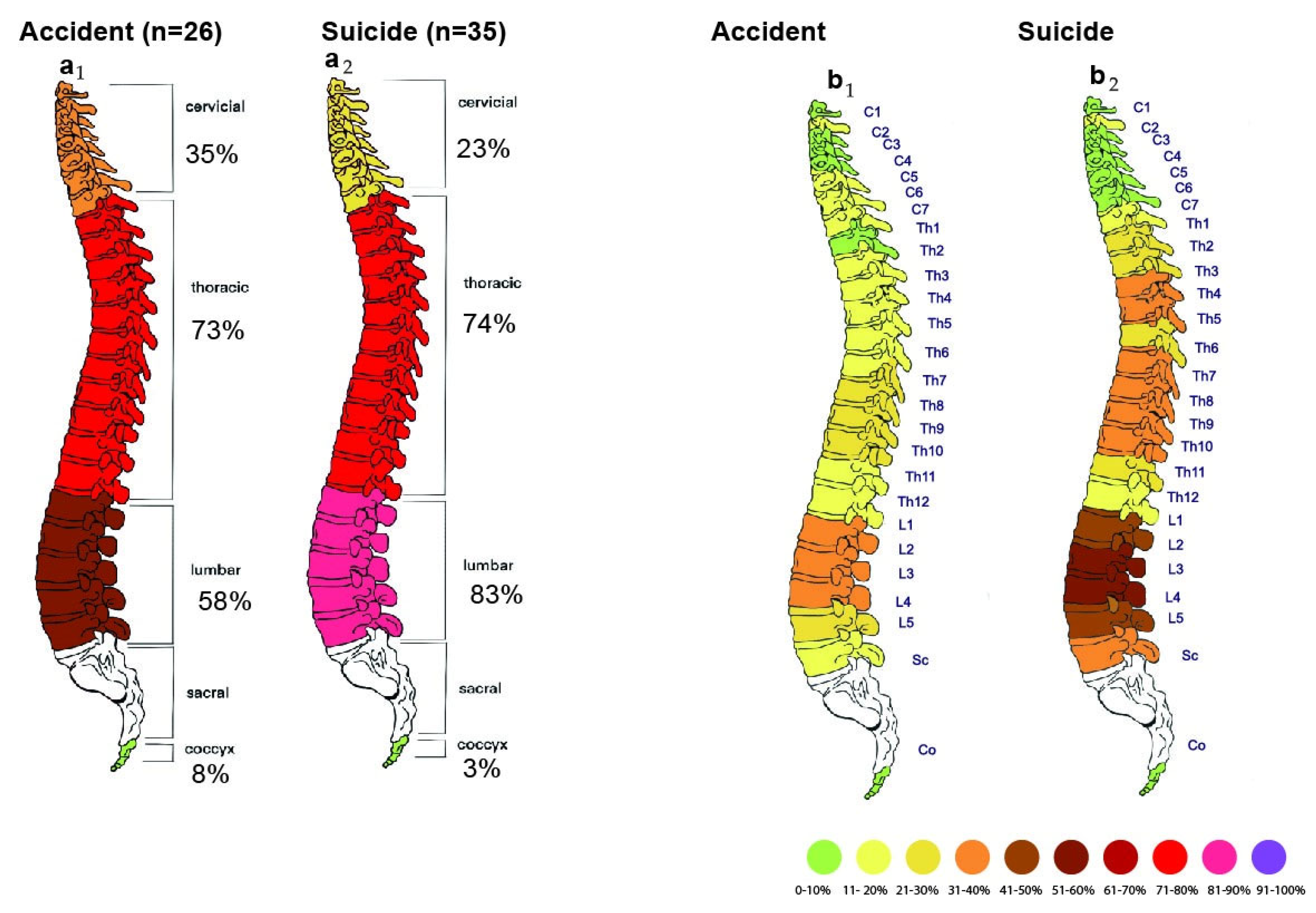
Among the 79 victims, 61 cases (77.22% of all cases) had a vertebral injury, including 18 women (81.82% of women) and 43 men (72.88% of men). Fracture frequencies are presented in
Table 10.
We observed a statistically significant correlation between the height of the fall and the presence of vertebral fractures (MWU, p = 0.043). Every meter fallen increased the chance for a spinal fracture by 8.7% (OR = 1.087; 95% CI: 0.99–1.20; LRT: p = 0.034). Moreover, the lumbar spine was the only spinal segment to show a correlation with fall height (MWU, p = 0.000004). The differences were most pronounced at height groups of less than 3 m, 20–25 m, and over 30 m. The most significant differences were observed between the less than 3 m and the above 30 m categories. Additionally, a relationship was found between vertebral fractures and the kinetic energy of the fall (MWU, p = 0.033).
Binary logistic regression revealed a strong and statistically significant association between sternocostal and vertebral fractures, with the odds of vertebral injury increasing nearly tenfold as the number of sternocostal fractures rose (OR = 9.67; 95% CI: 2.12–44.15; LRT p = 0.0024).
Comparison between spinal column injuries in accidents and suicides is shown in
Figure 3.
Among the 36 victims of the accident, 26 suffered spinal injuries (72.22% of all accident victims). Fracture frequencies are presented in
Table 11.
Among the 43 victims of a suicidal fall from a height, spinal injuries occurred in 35 cases (81.40% of all suicide victims). Fracture frequencies are presented in
Table 12.
Of the 38 individuals with pelvic fractures, a significant correlation was found with female sex (χ
2 test,
p = 0.026). Pelvic fracture frequencies are shown in
Table 13.
In the statistical analysis, we observed that fractures of the inferior pubic ramus were more likely to occur in individuals with lower BMI than in those without this damage (MWU, p = 0.035). Additionally, the base (MWU, p = 0.016) and middle part (MWU, p = 0.027) of the sacrum were more likely to be affected in cases with a lower BMI. Logistic regression analysis showed that body mass was a significant predictor of pelvic damage, and with every kg of mass, the probability of pelvic fracture decreased 5.4% 17.9% (OR = 0.95; 95% CI: 0.91–0.98; LRT: p = 0.0019). Another observation was that fractures of the pubis (χ2 test, p = 0.025), sacrum (χ2 test, p = 0.004), and ischium (χ2 test, p = 0.015) were more common in females than in males.
The study identified a significant relationship between the kinetic energy of a fall and fractures of the pelvis (MWU, p = 0.0001) and its specific regions, including the pubic bone (MWU, p = 0.001), bilateral pubic fractures (MWU, p = 0.006), the sacrum (MWU, p = 0.001), its middle part (MWU, p = 0.034), and the apex (MWU, p = 0.03). Additionally, kinetic energy was associated with pubic symphysis rupture (MWU, p = 0.018), Bilateral pubic rami fractures (MWU, p = 0.042), and upward displacement of pelvic structures (MWU, p = 0.015). Higher kinetic energy was observed in groups with these injuries. Every additional meter in height of the fall increased the chances of pelvic fractures by 17.9% (OR = 1.18; 95% CI: 1.076–1.29; LRT: p = 0.000011). Furthermore, individuals with shorter stature experienced a higher frequency of pelvic (T-test, p = 0.003), pubic bone (T-test, p = 0.003), inferior ramus (T-test, p = 0.003), superior ramus (T-test, p = 0.001), and sacral fractures (T-test, p = 0.003).
Comparison between pelvic injury in accidents and suicides is shown in
Figure 4.
There were 11 cases of individuals who had a pelvic fracture as a result of an accident-related fall from a height. Fractures are presented in
Table 14.
The cohort of suicides with pelvic injuries included 27 individuals. Fracture frequencies in the suicide group are presented in
Table 15.
Cases of suicide, compared to accidents, showed a higher frequency of fractures in the pelvis (χ2 test, p = 0.004) and pubic bone (χ2 test, p = 0.005).
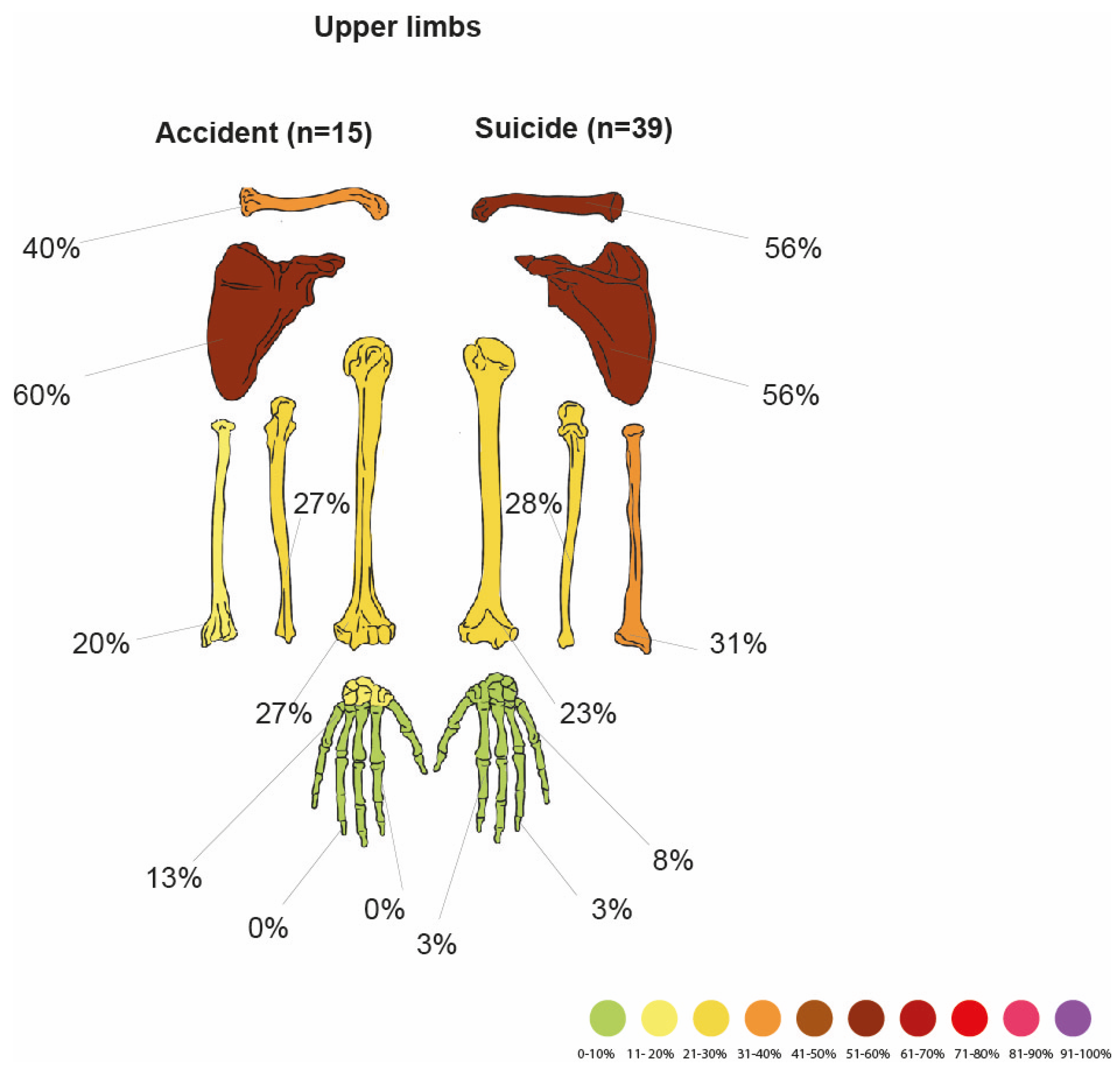
The group of people who suffered a fracture of the upper limb in an accident from height numbered 54. Fracture frequencies are presented in
Table 16.
A positive statistical correlation was found between upper limb fractures (MWU, p = 0.001), humerus fractures (MWU, p = 0.013), and forearm bone fractures (MWU, p = 0.038) with the height of the fall. Additionally, other components of the upper limb—scapula (unilateral MWU, p = 0.001; bilateral MWU, p = 0.004), clavicle (unilateral MWU, p = 0.008; bilateral MWU, p = 0.003), and ulna (MWU, p = 0.044)—showed similar relationships. For every additional meter fallen, the risk of upper limb damage increased 26% (OR = 1.26; 95% CI: 1.062–1.50; LRT: p = 0.00036). Meanwhile, no statistically significant correlation was observed between radial bone fractures and the fall category. Furthermore, differences in height categories between groups were more evident for bilateral fractures of the scapula and clavicle.
Statistical analysis indicated that victims with a fractured forearm (either the ulna, radius, or both) (MWU, p = 0.002), as well as those with fractures of the ulna (MWU, p = 0.01) and radius (MWU, p = 0.003), alone, had a lower BMI compared to those without such injuries. Moreover, the kinetic energy from falls was correlated with fractures of the scapula (MWU, p = 0.005), bilateral scapula fractures (MWU, p = 0.012), clavicle fractures (MWU, p = 0.018), bilateral clavicle fractures (MWU, p = 0.01), and humerus fractures (MWU, p = 0.016).
In comparison of these two groups, it was observed that fractures of the upper limb (χ2 test, p = 0.001), scapula (χ2 test, p = 0.018), clavicle (χ2 test, p = 0.004), and forearm (χ2 test, p = 0.033) are more common in suicides than in accidents. Analysis of logistic regression showed that suicides have an eight times higher risk of upper limb fracture than accidents (OR = 8.089; 95% CI: 2.17–30.19; LRT: p= 0.00083).
Among 79 victims, fractures in the lower limb (L.L.) occurred in 35 cases (44.30% of all cases). Fracture frequencies are presented in
Table 19.
Lower limb fractures were positively correlated with the kinetic energy of the fall (MWU, p = 0.000021) and female sex (χ2 test, p = 0.00158). Fractures of the right (χ2 test, p = 0.00352) and left (χ2 test, p = 0.048) femurs, as well as the right (χ2 test,, p = 0.00148) and left (χ2 test, p = 0.00025) tibias, right (χ2 test, p = 0.00148) and left (χ2 test, p = 0.01631) fibulae were positively associated with the height of the fall. For every meter, the probability of lower limb damage increased 12% (OR = 1.12; 95% CI: 1.022–1.23; LRT: p = 0.00086)
The sums of all left (ρ, p = 0.000001) and right (ρ, p = 0.000016) L.L. fractures were correlated with the height of the fall. Additionally, bilateral lower limb fractures occurred in 18 cases, which were strongly associated with the height of the fall (ANOVA, p = 0.0003). Fractures in the right foot (tarsals, metatarsals, and digits) also showed a positive correlation with the height of the fall (ρ, p = 0.004278) and, additionally, with a suicidal manner of death (MWU, p = 0.0154). We found a statistically significant correlation between left L.L. injury and mental illness (MWU, p = 0.00415).
Logistic regression analysis showed that the presence of lower limb fractures increased the probability of pelvic fractures by over three times (OR = 3.21; 95% CI: 1.044–9.86; LRT: p = 0.040)—moreover, the best predictors for the L.L damage were upper limb fractures (OR = 14.0; 95% CI: 2.88–68.058; LRT: p = 0.000073).
Comparison of lower limb damage in accidental and suicidal fatal falls is shown in
Figure 6. Note that the accident group is significantly smaller.
Of the 35 cases with lower limb injuries, 7 were victims of accidents (20% had damaged lower limbs). Fracture frequencies are presented in
Table 20.
Of the 35 cases with lower limb injuries, 28 of them occurred as a result of a suicidal fall from a height (80% damaged L.L.). Fractures in the suicides are presented in
Table 21.
Injuries to both the right (MWU, p = 0.00283) and left (MWU, p = 0.000146) L.L. were significantly more common in suicides; this was also true for the right femur (χ2 test, p = 0.02904). Fractures of both the right (χ2 test, p = 0.01567) and left (χ2 test, p = 0.00535) tibia, as well as the right (χ2 test, p = 0.01567) and left fibula (χ2 test, p = 0.00078), showed a positive correlation with suicide cases. Bilateral lower limb fractures were found in 16 cases; they were more frequent in suicides than accidents (χ2 test, p = 0.00278). Logistic regression analysis shows that suicides had a four times higher risk of lower limb fracture than accidents (OR = 3.96; 95% CI: 1.20–13.13; LRT: p = 0.022).
4. Discussion
Our study population was consistent with previous reports. The majority of participants were male, with a male-to-female ratio of 2.6:1. Men outnumbered women across all categories of fatality, a trend consistent with most prior studies, further reinforcing that FFF primarily affects men. High-risk occupations, particularly in construction, are predominantly held by males. In the case of suicides, men tend to prefer more lethal and violent methods, such as FFF. Contrary to the previous literature, suicides were more prominent in our sample than accidents [
15,
28,
29,
30].
The BMI distribution was approximately normal, with most individuals classified as normal weight or overweight and a small proportion as obese or underweight [
6].
Alcohol is the most frequently encountered toxin in accidental FFF, as well as a fairly common drug among suicide victims [
31]. Our study seems to confirm this notion, with almost ½ of the included accidental and ¼ of the suicidal falls being under the influence. Moreover, statistical analysis revealed that alcohol intoxication was correlated positively with accidents and had no connection with suicides (χ
2 test,
p = 0.0133). Alcohol causes postural instability, which increases the risk of accidental FFF [
32]. Suicide victims often plan their actions and approach the jump cool-minded. Furthermore, this notion ties in with the observed interplay between alcohol and mental illness. In our study, the mentally ill victims were less likely to test positive for alcohol and more likely to commit suicide. The widespread accessibility of alcohol may also contribute to accidental fatalities.
Previous research has established a correlation between the use of psychoactive substances and upper limb fractures, indicating that uncontrolled flailing movements during falls may contribute to such injuries [
11]. Nevertheless, our study did not reproduce this finding. A plausible explanation is the predominance of alcohol consumption within our cohort, as opposed to substances with more pronounced psychostimulant effects. Alcohol, acting as a central nervous system depressant, impairs reaction time and reduces reflex responses [
33]. Consequently, individuals under the influence may be less likely to demonstrate protective reflexes during a fall, thereby decreasing the risk of upper limb fractures.
Mental illness typically concerns suicide victims of FFF, with little to no cases of accidents. It is also more common among women. Despite that, FFF are more common among males, both suicidal and accidental [
30,
34,
35]. Our study confirms that over 50% of females have a known psychiatric history, and males outnumber females in both manner-of-death groups. Mental illness was also connected with suicidal intention and the lower height of the fall. Many psychiatric diseases cause suicidal thoughts. However, the exact causes of why one would choose falling over other methods of suicide are a complicated issue [
32].
The average fall height of 22.30 m, with a median of 7 m, illustrates the diversity of fall heights among the included victims. Our study seems to be in accordance with the literature, where most fatal falls occur at heights of less than 10 m [
7,
18]. Similarly, the notion that higher falls are more common among suicide victims was confirmed by our work. Individuals seeking a place to jump from usually choose higher altitudes to ensure lethality [
36]. Women had statistically higher falls, most probably because most of them were in the suicide group.
The general injury pattern in our work is broadly consistent with that observed in the literature. It primarily concerns the axial skeleton, with the chest being the most commonly damaged part [
37]. Amid many contradictory results, most works agree that rib fractures are the most frequently encountered in FFF. Ribs are directly or indirectly affected in every impact position and type of landing surface. Because of their location and susceptibility, FFF without them is unlikely [
9,
12,
38]. The probability of a rib fracture increases with the height of the fall and kinetic energy, an effect confirmed in our work [
39]. This also explains the significantly higher frequency of rib cage fractures among males, as FFF in this group were characterized by greater BMIs. Furthermore, bilateral rib fractures were shown to be more common in suicides and unilateral fractures in accidents. This effect was previously observed and is likely a byproduct of the impact position. Individuals attempting suicide by jumping from a height may employ various techniques, such as running and jumping, stepping off the edge, hanging and releasing, diving head-first, or falling backward intentionally. These controlled or semi-controlled actions often result in a feet-first or buttocks-first landing. In contrast, accidental falls—typically resulting from slips, trips, or unintended loss of balance—more frequently lead to lateral or whole-body impacts, reflecting the unpredictable and unprepared nature of such events. Thus, injuries in suicidal FFF are more symmetrical, and in accidental FFF, they are shifted to one side [
38]. The statistical correlation between an increase in rib fractures and mental illness was not described in previous literature. It might stem from differences in impact positions and higher overall altitudes in this group. This effect warrants further investigation.
Skull fractures in the FFF literature have three different distributions depending on the height of the fall, bimodal [
5,
16], linear rising [
6,
40], and linear falling [
41]. Bimodal distribution—cranial fractures are more prevalent in falls below 10–15 m, less common between 10 and 20 m, and reemerge in falls exceeding 20 m. Experimental and modeling investigations have demonstrated that the initial position predominantly influences the ultimate impact orientation, with impacts to the head being more likely in short falls and landings to the feet or sides more common at intermediate heights due to body angular rotation. At significantly high falls, even impacts to the feet can transmit sufficient energy to induce cranial fractures.
This bimodal pattern contrasts with findings from other studies, which report a linear increase in skull fractures correlating with fall height. Such discrepancies may be attributable to differing ratios of accidental to suicidal falls. Suicides originating from various heights and positions tend to produce more linear distributions, whereas accidental falls—generally lower and more uniform in trajectory—tend to display bimodality. Further comparative research is warranted to substantiate this observation. Finally, some studies report only a decrease in skull fractures with increasing fall height. These might reflect heterogeneity across studies.
Our study falls into the first category, arguing that at lower heights, fallers have little time for the body to rotate. Consequently, the head or upper part of the chest strikes the ground first, leading to cranial fractures. At mid-range (10–20 m), the body has more time to rotate, often landing in a way that spares the skull. However, the potential energy transmitted through the axial skeleton at greater heights becomes significant enough to cause cranial fractures, regardless of the exact impact position.
Skull base fractures typically occur at a distance from the initial point of impact, whereas skull vault fractures are generally found closer to the site of contact. This spatial relationship is influenced by factors such as the victim’s body height and the specific mechanics of the fall. However, the diagnostic value of this distinction is limited. The most common fracture type—linear fractures—can occur both proximally and distally from the impact zone. In such cases, identifying skull base and vault fractures may offer the only anatomical clues to the location and dynamics of the impact [
42,
43]. The absence of sphenoid fractures among the aforementioned statistical connections may be due to protection from direct impact by the zygomatic arch.
The statistical association between higher BMIs and posterior occipital fractures is quite puzzling, as no such association has been previously described in FFF. Being overweight was even shown to decrease the probability of head and neck injuries [
6]. We hypothesize that this effect is best explained by higher potential energies, as per the formula Epot = mgh. Further research is needed to elaborate on those findings.
The inverse association between pelvic and cranial fractures likely reflects biomechanical differences in impact dynamics. During head-first impacts, the cranial region absorbs the majority of kinetic energy, thereby reducing the transmission of force to the pelvis. The facial skeleton received limited attention in previous FFF studies. Some articles have noticed a correlation between the height of the fall and the resulting fractures [
14,
38]. But this was not universally attested [
44]. Our study found statistical correlations between maxillary and mandible fractures, the height of the fall, and kinetic energy, suggesting that facial skeleton injuries may provide helpful forensic clues. Impacts other than feet, knees, or buttocks first should, at least in some cases, injure salient elements of the facial skeleton [
45]. This relationship also suggests that the facial skeleton was not damaged in the “second impact” after bouncing off the ground.
The spine was the second most frequently injured region in our study, a finding that differs from most reports in the current literature [
46,
47]. This discrepancy may be attributed to the use of postmortem PMCT, which enhances the detection of deep fractures.
Spinal fractures are known to correlate with fall height, as fall-related injuries predominantly affect the axial skeleton [
44,
48]. Given this, we expected kinetic energy to be associated with spinal injuries. Interestingly, when analyzing specific spinal regions, only the lumbar vertebrae showed a significant correlation with fall height. This stands with previous studies on living individuals that have identified the thoracolumbar junction as the most commonly fractured area in fall-related injuries [
49]. No correlations were found for specific parts of each vertebra, suggesting that their relation with other variables is either complex or unpredictable.
The strong association between spinal and thoracic trauma revealed by logistic regression is anatomically and biomechanically plausible, as the axial skeleton is primarily affected in falls from height. In all impact orientations, the vertebrae absorb a substantial portion of the impact energy. Pelvic fractures pose a significant risk due to the potential for severe hemorrhage. They typically occur in feet-first, buttocks-first, or whole-body impacts, which arise from either direct horizontal deceleration or indirect vertical force transmission, primarily through the femur. Consequently, these injuries are often centered around major joints— sacroiliac joints and pubic symphysis, although they differ structurally, being partly fibrous and cartilaginous, respectively [
9,
29,
38]. Pelvis fractures increase with the height of the fall and are more common among suicides [
50]. Although not all studies find this relationship [
18].
Our study confirmed that the incidence of pelvic (
p = 0.001), pubic (
p = 0.003), and sacral (
p = 0.008) fractures increases with fall height. However, kinetic energy showed a stronger correlation, as expected given its critical role in trauma severity. Nearly all severe pelvic injuries were linked to higher kinetic energy levels. Lower body height is connected to lower bone mineral density [
51]. This might explain why shorter individuals are statistically more likely to experience pelvic fractures.
Logistic regression identified key predictors of skeletal injuries in fatal falls. Both body mass and fall height significantly influenced pelvic fractures; each extra kilogram decreased pelvic injury odds by 5.4% (OR = 0.95; p = 0.0019), while each additional meter increased the odds by 17.9% (OR = 1.18; p < 0.001). The presence of lower limb fractures more than tripled the odds of pelvic fractures (OR = 3.21; p = 0.040). Fall height also predicted lower limb injuries (OR = 1.12/meter; p < 0.001), with upper limb fractures strongly linked (OR = 14.0; p < 0.001). Suicides significantly raised the odds of upper limb (OR = 8.09; p < 0.001) and lower limb fractures (OR = 3.96; p = 0.022) compared to accidental falls. Thoracic trauma markedly increased the likelihood of spinal injury, with vertebral fractures nearly tenfold when sternocostal fractures were present (OR = 9.67; p = 0.0024).
Interestingly, our findings contradict previous research suggesting that obesity serves as a protective factor against specific injuries, including pelvic fractures [
52]. This discrepancy may be explained by the heterogeneity of the studied populations and the role of body fat as padding. Additionally, our study reinforces the well-documented association between pelvic fractures and suicidal falls. Possibly because of the association between higher falls and suicides explored earlier.
Bilateral pubic rami fracture was present in ⅕ of all pelvic injuries in our study group, which is much more common than in clinical literature. As fatal falls tend to happen with greater kinetic energy and more extensive injuries, this is not surprising [
53]. The low incidence of fallers’ fractures aligns with the existing literature, establishing it as a rare but characteristic finding [
23]. No statistical correlations were found for these injuries.
According to the Young and Burgess classification, lateral compression injuries were the most prevalent in our study, consistent with the current literature. In real-life falls, it is rare for individuals to land in a perfectly vertical or horizontal posture with symmetrical force distribution. Instead, victims often strike the ground on their side or buttock, introducing a lateral force vector that drives inward rotation of the hemipelvis, leading to characteristic coronal-plane fractures of the pubic rami and sacrum.
Anterior–posterior compression injuries were the second most frequent. This is likely due to the wide variability in landing positions during high-energy falls. Victims who land in a semi-upright, supine, or extended-leg position may transmit front-to-back forces through the pelvis, resulting in symphysis pubis widening and disruption of the pelvic floor and sacroiliac ligaments, consistent with APC injury patterns. Such mechanisms are commonly observed in falls from height involving axial loading combined with torso hyperextension or leg abduction.
Vertical shear injuries, caused by asymmetrical axial loading (e.g., landing on one leg), were rare. This supports the notion that such unilateral, high-magnitude impacts are relatively uncommon in fatal falls. Likewise, posterior–anterior compression patterns—resulting from a posteriorly directed force—are infrequent.
Upper limb injuries remain highly contested in the literature. Some studies see them as almost random and without a specific pattern [
39,
41], and others connect them with the height of the fall [
12,
15,
54]. Our study aligns with the latter. The body’s defense mechanisms include extending the arms in preparation for impact, which increases the risk of fractures in both the first and second impacts. Although a feet-first landing is the most common, any other position would also involve this reflex [
55]. The strong correlation between bilateral clavicle and scapular fractures, fall height, and kinetic energy may be attributed to their proximity to the axial skeleton and the body’s impact position. This suggests that these fractures could serve as potential markers for estimating fall altitude. Additionally, given that suicidal falls typically involve higher kinetic energies, this factor likely contributes to the increased frequency of clavicle and scapular fractures observed in suicides. Suicides had an increased probability of upper limb fractures compared to accidents (OR = 8.089). Additionally, upper limb fractures were the best predictor for lower limb fractures. These relations might stem from the overall higher kinetic energy of suicide falls.
In the study, fractures of the pelvis and its bones, excluding the iliac bone, were more frequently noted in females than in males. Fractures of the forearm and radial bone showed analogous patterns. Furthermore, we observed a correlation between lower BMIs and pelvic injuries. These relationships can be explained by the higher risk of osteoporosis in females and the typical fracture sites, namely the pelvis and forearm. Moreover, lower BMI may reflect frail bones [
56].
As expected, fractures of the lower limbs—both unilateral and bilateral—were primarily influenced by the height of the fall and the associated kinetic energy. Interestingly, the presence of such fractures was the most distinguishing factor between low and very high falls, suggesting that lower limb fractures could serve as a valuable indicator in altitude estimation.
Notably, in suicides, both individual and bilateral lower limb fractures were significantly more frequent than in accidental falls (OR = 3.96), likely due to differences in impact positioning. Suicide victims may initiate a free fall through multiple mechanisms, including running and jumping, stepping over an edge, hanging and releasing, or leaning forward from a height. The majority of these actions lead to a descent feet-first, which, in the absence of substantial body rotation, probably explains the high incidence of lower limb injuries documented in such cases. This aligns with previous literature. Some studies have proposed that fractures of the dominant lower limb are more common in fatal fall suicides, as the final step before jumping is typically taken with the dominant leg, increasing its likelihood of striking the ground first [
57,
58]. Our findings reinforce this idea, showing that nearly all lower limb bones exhibited a correlation with fall height and suicidal intent, except for the left femur and foot. Specifically, fractures of the right femur and foot were more prevalent in suicides but not in accidents, possibly reflecting the dominance-related mechanism mentioned earlier. However, recent studies have not consistently supported this association [
12], highlighting the need for further research to clarify these findings.
The discrepancies between our results and earlier studies may arise from methodological and population differences. In contrast to many previous reports that included mixed fall types or impacts on deformable surfaces, our dataset was restricted to free falls onto rigid, non-deformable substrates, which likely resulted in more extensive skeletal trauma. Moreover, the use of high-resolution PMCT enabled the identification of subtle or incomplete fractures that might have been missed in autopsy-based investigations. Differences in demographic structure—particularly age distribution and the predominance of urban falls in our material—may also have influenced injury configurations. Together, these factors could explain part of the variation in reported fracture prevalence and distribution across studies.
Our study had several limitations. The sample size was relatively small, and many cases were excluded due to missing data, such as fall height or an unclear cause of death. This may have introduced bias in the reported fracture frequencies and their statistical correlations. Rare fractures might have been overlooked. Additionally, PMCT has limitations in detecting fractures in thin or less ossified bones, including the ethmoid bone. Given the unique nature of forensic cases, studied populations tend to be heterogeneous, making it challenging to generalize findings across different groups. This study standardized the surface type to impact on hard, non-deformable surfaces. Fracture patterns resulting from deformable or yielding surfaces require separate examination to determine potential differences. Toxicological parameters, particularly alcohol levels, were analyzed in relation to the manner of death. The body position at impact could not be reliably documented retrospectively, as all included fatal falls lacked direct witnesses; therefore, it was not assessed. This limitation may have influenced the interpretation of specific fracture patterns observed in our study.
Furthermore, free-fall trauma remains unpredictable due to the multitude of variables influencing each incident. Statistical analysis may identify certain fractures and correlations as more characteristic of suicidal or accidental falls; however, the overall skeletal injury patterns exhibit considerable overlap between the two groups. Consequently, the correlations established in this study should not be regarded as universally diagnostic. Instead, our findings should be interpreted as offering a set of supportive indicators—arguments for or against a particular manner of death—within the broader context of forensic evaluation. This study primarily analyzed fracture frequencies in fatal falls for each bone. Additionally, we identified novel relationships between key variables and specific injuries, including correlations between facial skeletal fractures and fall height, posterior occipital bone fractures and BMI, and the association between the cause of the fall and the fractured side of the body. Many of our findings align with previous research, and in several cases, we were able to refine them to the level of individual bones. Furthermore, we uncovered new insights that may help differentiate between suicides and accidental falls.
From a clinical perspective, our findings might be helpful for emergency care and trauma support. The most essential findings are presented in
Table 22.
Although the finding that the number and severity of injuries increase with both the height of the fall and the resulting increase in kinetic energy is not novel, our study identified several anatomical regions that are particularly prone to injury. These include the facial skeleton, the occipital and temporal bones, the lumbar vertebrae, the ribs, and the lower limb bones. Recognizing these vulnerable areas may help clinicians assess and plan treatment for victims of free-fall injuries.
Understanding how intrinsic factors such as BMI and sex influence injury patterns can further inform risk assessment and clinical expectations. Emergency physicians and trauma care personnel should also be aware of the distinct differences between suicidal and accidental fall injuries. Suicidal falls tend to produce more severe, bilateral, and complex fractures; therefore, patients presenting after a suspected suicide attempt by fall should be managed as high-priority trauma cases. Extensive injuries involving both the axial and appendicular skeletons are to be anticipated. Notably, facial fractures may compromise airway patency, while spinal trauma often requires urgent stabilization.
In subsequent care, the evaluation of injury distribution may also contribute to the differentiation between suicidal and accidental mechanisms. Because suicidal individuals may sometimes misrepresent their intent, awareness of these characteristic patterns may aid both in accurate medico-legal interpretation and in the planning of appropriate psychiatric follow-up and preventive interventions. Postmortem CT is not the sole emerging technique capable of augmenting fall investigations. Biomechanical experiments have been successfully employed to distinguish between conflicting reports of the incident (e.g., accidental versus homicidal falls). Furthermore, computer-based simulations have recreated fracture patterns that were subsequently verified during autopsy in numerous cases. Similar results were achieved by Henningsen et al.: subject-specific finite-element head models were used to predict PMCT and autopsy findings, with relative success. Collectively, these methodologies underscore promising new avenues for reconstructing and interpreting free-fall events [
59,
60,
61].
Future studies should further explore bone fractures using post-mortem computed tomography. This approach will enable forensic experts to replace ambiguous terms, such as “limb fracture,” with more precise descriptions. Recent advancements in artificial intelligence are promising in this regard, with AI models being used to assess fracture morphology [
62].
Additionally, the correlation between body mass index and fractures of the skull and pelvis needs further investigation. Our findings related to the maxilla and mandible should also be examined more closely. The effects of intoxication and mental illness on fracture patterns should be examined in greater detail. Ongoing research should aim to identify new markers for accidental and suicidal fatal falls. The topic of homicidal fatal falls requires comprehensive study, as such cases are rare; conducting a multicenter study could provide a larger sample size for analysis.