Differentiating Outcomes and Complications Between Extraplexal Tendon Transfers and Arthrodesis for Shoulder Reanimation Following Traumatic Brachial Plexus Injury: A Systematic Review and Proportional Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Literature Search
2.2. Study Eligibility Criteria
2.3. Screening and Data Extraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Study Characteristics and Demographics
3.2. Risk of Bias Assessment
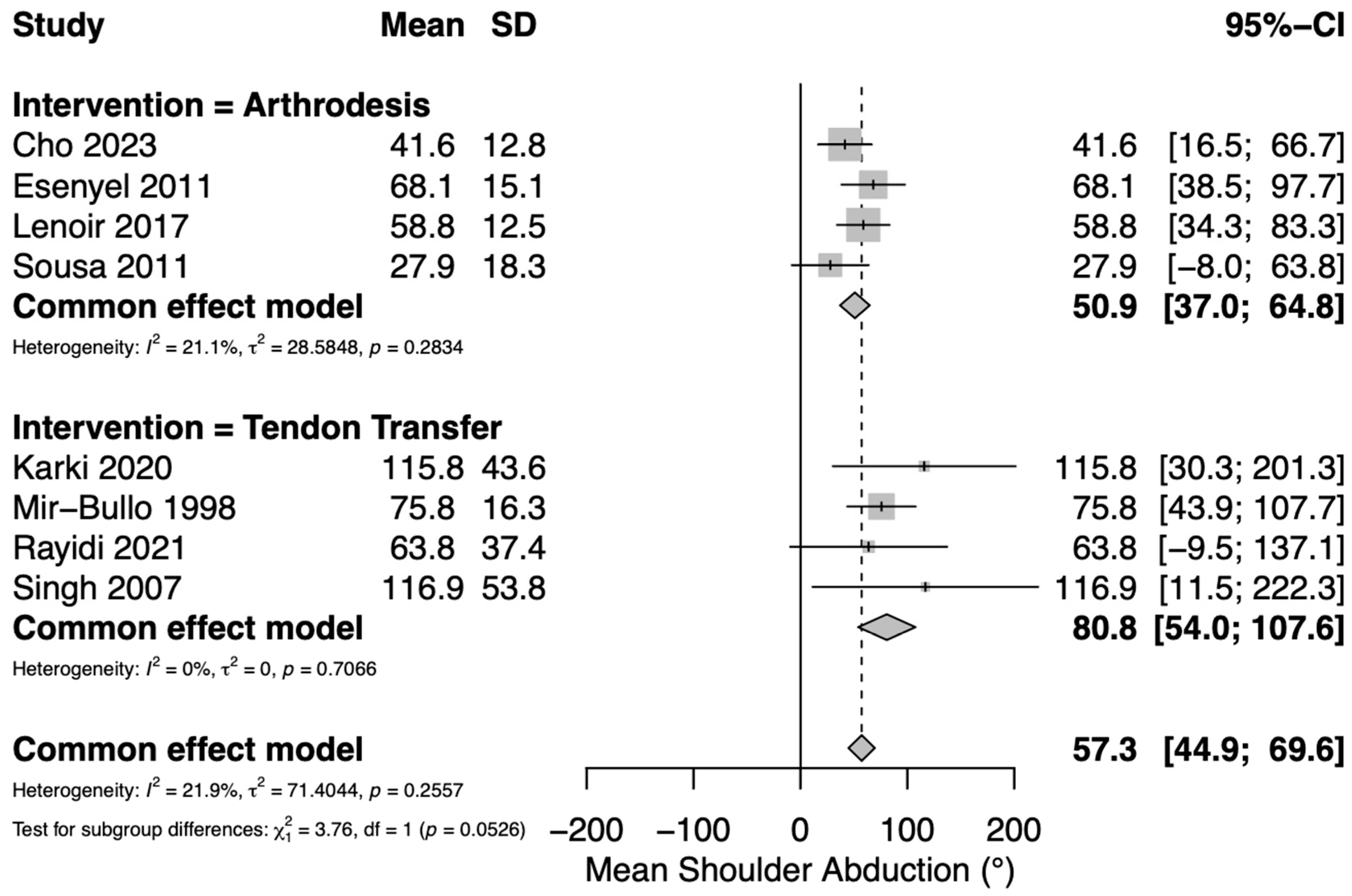
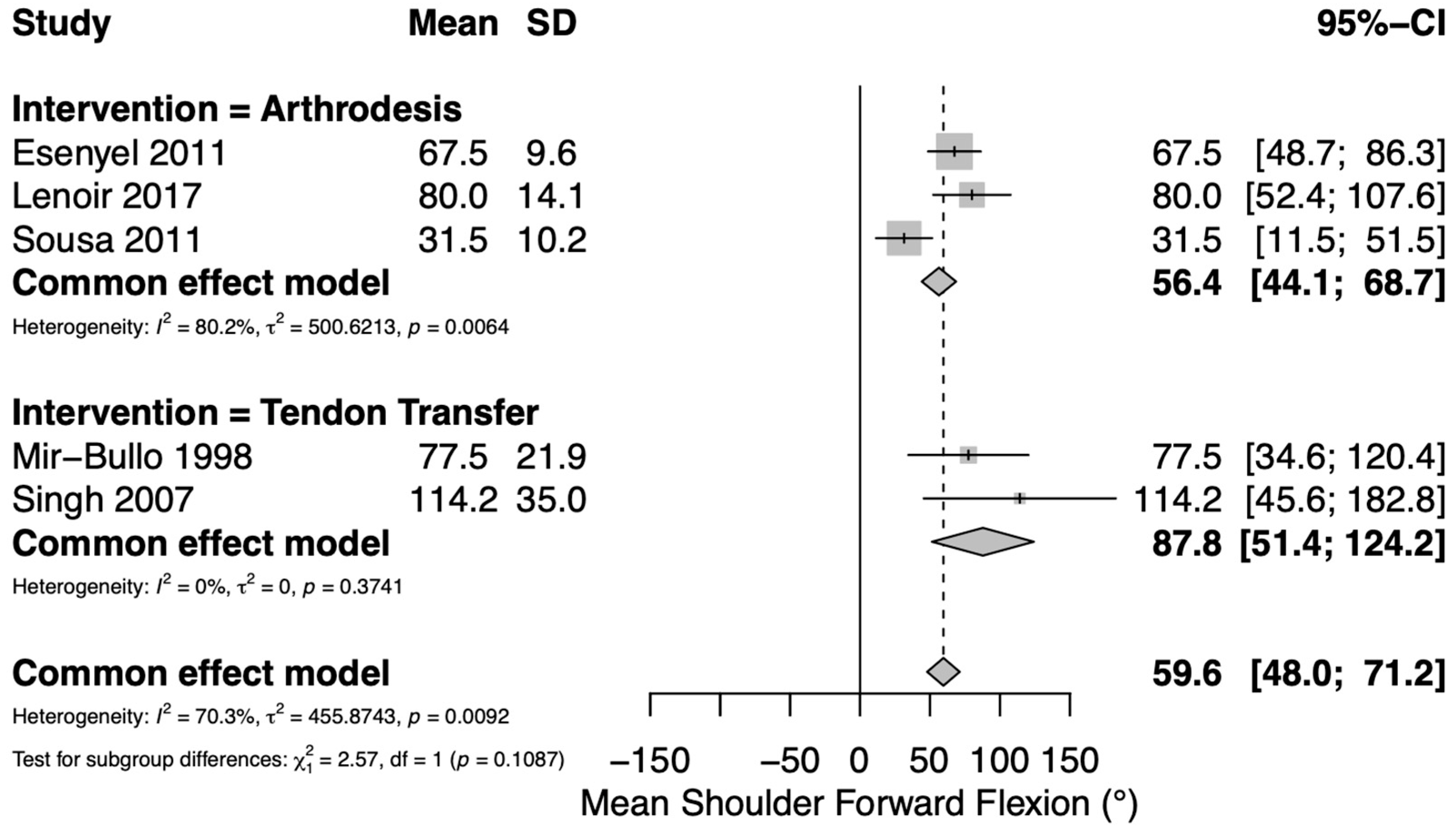
3.3. Range of Motion Outcomes
3.4. Patient-Reported Outcomes
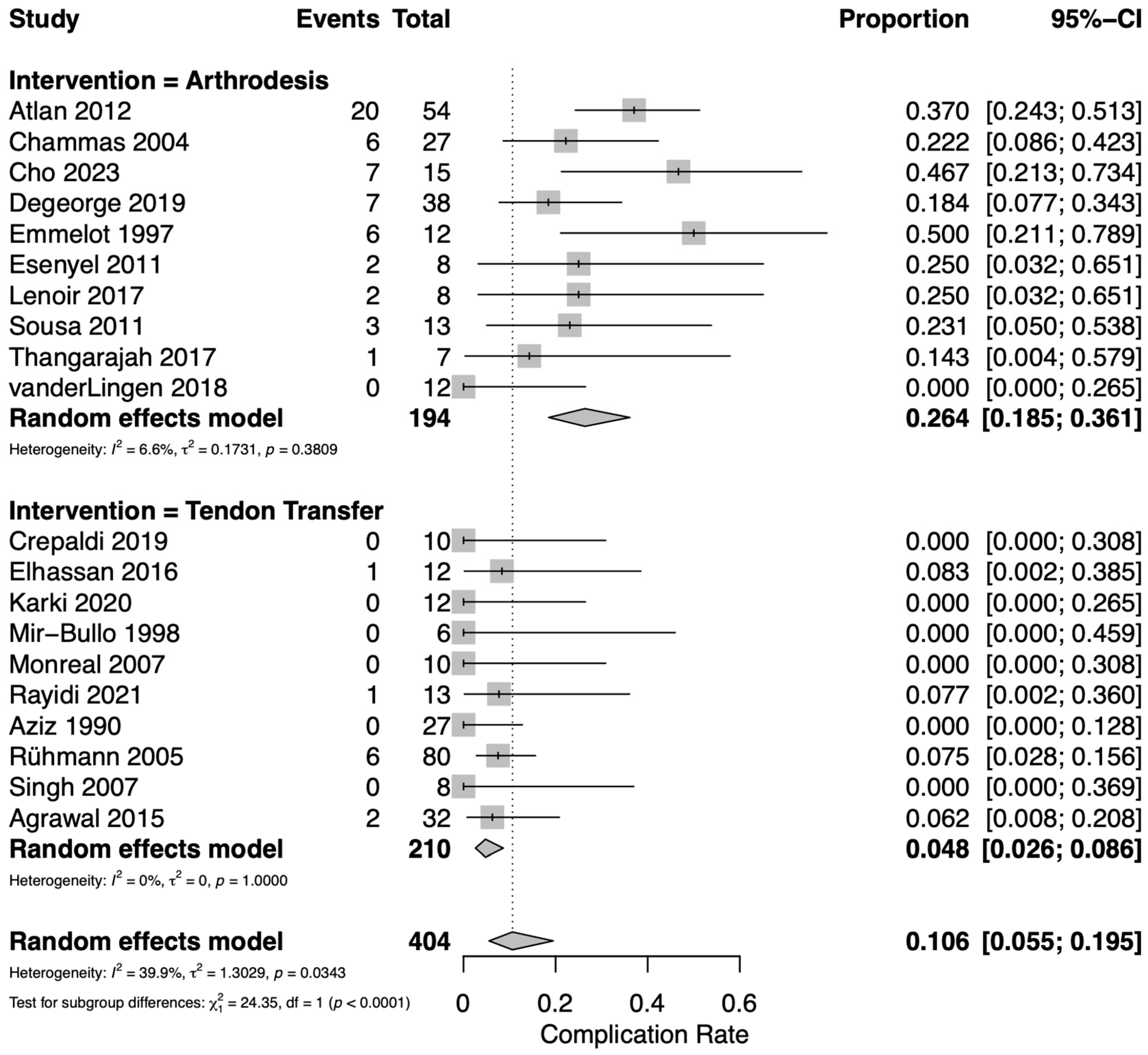
3.5. Complications
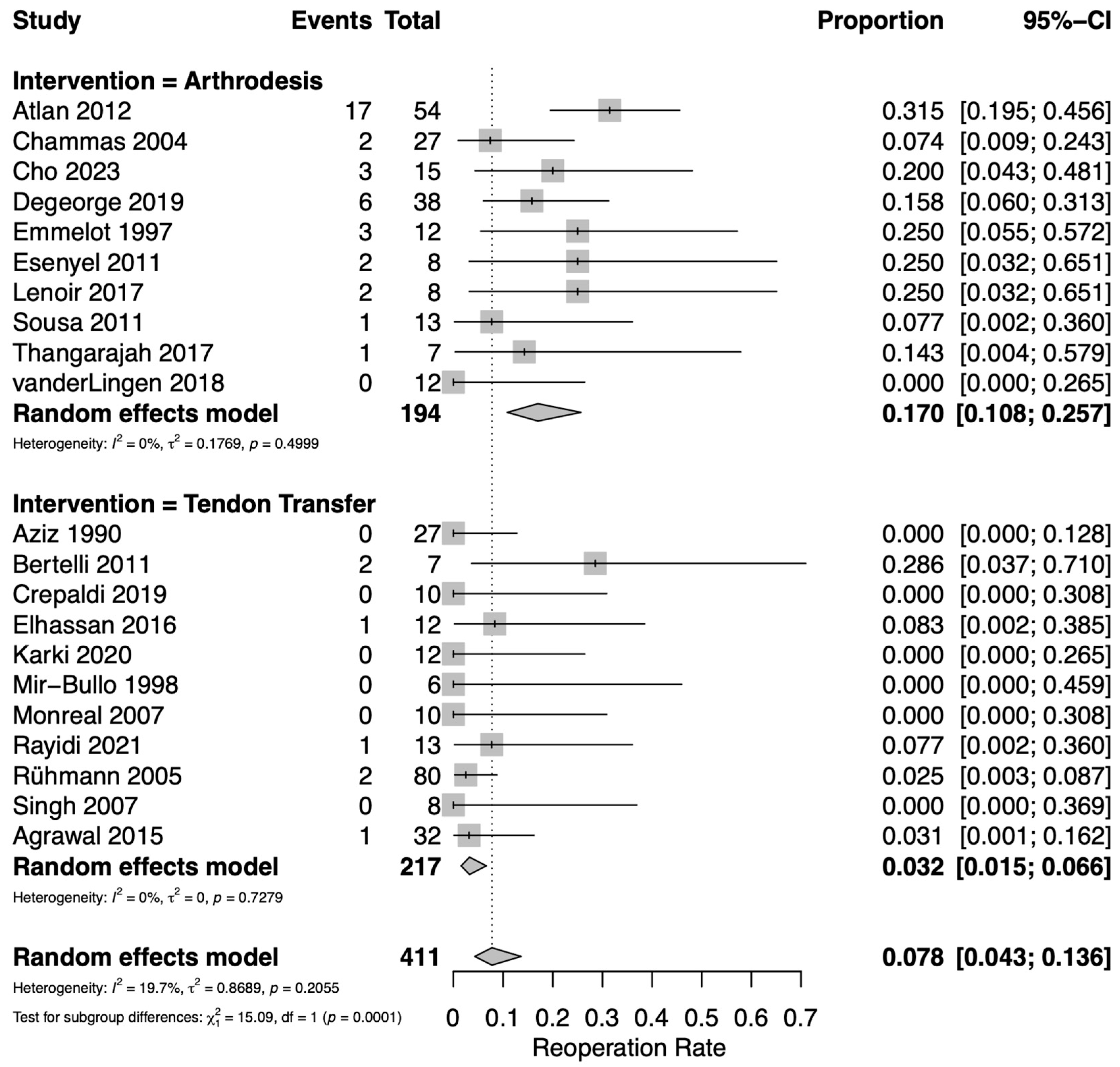
3.6. Reoperations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kaiser, R.; Waldauf, P.; Ullas, G.; Krajcova, A. Epidemiology, etiology, and types of severe adult brachial plexus injuries requiring surgical repair: Systematic review and meta-analysis. Neurosurg. Rev. 2020, 43, 443–452. [Google Scholar] [CrossRef]
- Kokkalis, Z.; Papagiannis, S.; Kouzelis, A.; Diamantakis, G.; Panagopoulos, A. Traumatic Bilateral Brachial Plexus Injury. Cureus 2022, 14, e24626. [Google Scholar] [CrossRef]
- Hems, T.E. Timing of surgical reconstruction for closed traumatic injury to the supraclavicular brachial plexus. J. Hand Surg. Eur. Vol. 2015, 40, 568–572. [Google Scholar] [CrossRef]
- Elhassan, B.; Bishop, A.T.; Hartzler, R.U.; Shin, A.Y.; Spinner, R.J. Tendon transfer options about the shoulder in patients with brachial plexus injury. J. Bone Jt. Surg. 2012, 94, 1391–1398. [Google Scholar] [CrossRef]
- Zhang, D.; Garg, R.; Earp, B.E.; Blazar, P.; Dyer, G.S.M. Shoulder Arthrodesis versus Upper Trapezius Tran.sfer for Traumatic Brachial Plexus Injury: A Proportional Meta-Analysis. Adv. Orthop. 2021, 2021, 4445498. [Google Scholar] [CrossRef] [PubMed]
- Li, N.Y.; Wu, K.Y.; Loosbrock, M.F.; Bishop, A.T.; Spinner, R.J.; Shin, A.Y. Injury and Biological Factors Impact Shoulder Function following Autogenous Grafting of Spinal Nerves for Pan-Brachial Plexus Reconstruction. Plast. Reconstr. Surg. 2024, 154, 918e–927e. [Google Scholar] [CrossRef] [PubMed]
- Hermena, S.; Assaf, A.; Donaldson, O. Systematic Review With Meta-Analysis: Are Muscle Transfers a Satisfactory Treatment Option to Restore Shoulder Abduction in Delayed Adult Brachial Plexus Injuries? Cureus 2021, 13, e12914. [Google Scholar] [CrossRef] [PubMed]
- Noland, S.S.; Bishop, A.T.; Spinner, R.J.; Shin, A.Y. Adult Traumatic Brachial Plexus Injuries. J. Am. Acad. Orthop. Surg. 2019, 27, 705–716. [Google Scholar] [CrossRef]
- Adu-Kwarteng, K.; Cabell, G.H.; Hurley, E.T.; Amanah, A.Y.; Levin, J.M.; Lassiter, T.E.; Boachie-Adjei, Y.D.; Klifto, C.S.; Anakwenze, O. Glenohumeral arthrodesis outcomes and complications: A systematic review. J. Shoulder Elb. Surg. 2024, 33, 1418–1424. [Google Scholar] [CrossRef]
- Sobhi, S.; Bochat, K.; Booth, G.; Mattin, A.; Moniz, S. Clinical and Surgical Outcomes of Shoulder Arthrodesis. J. Clin. Med. 2024, 13, 4701. [Google Scholar] [CrossRef]
- Wagner, E.R.; McLaughlin, R.; Sarfani, S.; Cofield, R.H.; Sperling, J.W.; Sanchez-Sotelo, J.; Elhassan, B.T. Long-Term Outcomes of Glenohumeral Arthrodesis. J. Bone Jt. Surg. 2018, 100, 598–604. [Google Scholar] [CrossRef]
- Rayidi, V.K.R.; R, S.; Appaka, J. Functional Evaluation of Levator Scapulae Tendon to Supraspinatus in Adult Brachial Plexus Injuries. Indian J. Plast. Surg. 2021, 54, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Agrawal, N.K. Transfer of upper trapezius with clavicular segment for restoration of shoulder movements following injury to the brachial plexus. Plast. Aesthetic Res. 2015, 2, 346–349. [Google Scholar] [CrossRef]
- Atlan, F.; Durand, S.; Fox, M.; Levy, P.; Belkheyar, Z.; Oberlin, C. Functional outcome of glenohumeral fusion in brachial plexus palsy: A report of 54 cases. J. Hand Surg. 2012, 37, 683–688. [Google Scholar] [CrossRef]
- Aziz, W.; Singer, R.M.; Wolff, T.W. Transfer of the trapezius for flail shoulder after brachial plexus injury. J. Bone Jt. Surg. Br. 1990, 72, 701–704. [Google Scholar] [CrossRef]
- Bertelli, J.A. Upper and lower trapezius muscle transfer to restore shoulder abduction and external rotation in longstanding upper type palsies of the brachial plexus in adults. Microsurgery 2011, 31, 263–267. [Google Scholar] [CrossRef]
- Chammas, M.; Goubier, J.N.; Coulet, B.; Reckendorf, G.M.; Picot, M.C.; Allieu, Y. Glenohumeral arthrodesis in upper and total brachial plexus palsy. A comparison of functional results. J. Bone Jt. Surg. Br. 2004, 86, 692–695. [Google Scholar] [CrossRef] [PubMed]
- Cho, A.B.; Choi, H.J.; Ferreira, C.H.V.; Yoshinobu Kiyohara, L.; Bersani Silva, G.; Sorrenti, L. Shoulder Arthrodesis for Traumatic Brachial Plexus Injuries: Functional Outcomes and Complications. Hand 2023, 18 (Suppl. 1), 6s–13s. [Google Scholar] [CrossRef]
- Crepaldi, B.E.; Neto, J.Q.L.; Rezende, M.R.; Júnior, R.M.; Scarcella, D.S. Lower Trapezius Transfer for Patients With Brachial Plexus Injury. Hand 2019, 14, 179–186. [Google Scholar] [CrossRef]
- Degeorge, B.; Lazerges, C.; Chammas, P.E.; Coulet, B.; Lacombe, F.; Chammas, M. Comparison of spinal accessory nerve transfer to supra-scapular nerve vs. shoulder arthrodesis in adults with brachial plexus injury. Orthop. Traumatol. Surg. Res. 2019, 105, 1555–1561. [Google Scholar] [CrossRef] [PubMed]
- Elhassan, B.T.; Wagner, E.R.; Spinner, R.J.; Bishop, A.T.; Shin, A.Y. Contralateral Trapezius Transfer to Restore Shoulder External Rotation Following Adult Brachial Plexus Injury. J. Hand Surg. 2016, 41, e45–e51. [Google Scholar] [CrossRef] [PubMed]
- Emmelot, C.H.; Nielsen, H.K.; Eisma, W.H. Shoulder fusion for paralyzed upper limb. Clin. Orthop. Relat. Res. 1997, 340, 95–101. [Google Scholar] [CrossRef]
- Esenyel, C.Z.; Oztürk, K.; Imren, Y.; Ayanoğlu, S. Shoulder arthrodesis with plate fixation. Acta Orthop. Traumatol. Turc. 2011, 45, 412–420. [Google Scholar] [CrossRef]
- Karki, D.; Muthukumar, V.; Dash, S.; Singh, A.K. Trapezius Transfer to Restore Shoulder Function in Traumatic Brachial Plexus Injury: Revisited and Modified. J. Hand Surg. Asian-Pac. Vol. 2020, 25, 143–152. [Google Scholar] [CrossRef]
- Lenoir, H.; Williams, T.; Griffart, A.; Lazerges, C.; Chammas, M.; Coulet, B.; Le Nen, D. Arthroscopic arthrodesis of the shoulder in brachial plexus palsy. J. Shoulder Elb. Surg. 2017, 26, e115–e121. [Google Scholar] [CrossRef]
- Mir-Bullo, X.; Hinarejos, P.; Mir-Batlle, P.; Busquets, R.; Carrera, L.; Navarro, A. Trapezius transfer for shoulder paralysis. 6 patients with brachial plexus injuries followed for 1 year. Acta Orthop. Scand. 1998, 69, 69–72. [Google Scholar] [CrossRef]
- Monreal, R.; Paredes, L.; Diaz, H.; Leon, P. Trapezius transfer to treat flail shoulder after brachial plexus palsy. J. Brachial Plex. Peripher. Nerve Inj. 2007, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- Rühmann, O.; Schmolke, S.; Bohnsack, M.; Carls, J.; Wirth, C.J. Trapezius transfer in brachial plexus palsy. J. Bone Jt. Surg. Ser. B 2005, 87, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Karki, D. Modified trapezius transfer technique for restoration of shoulder abduction in brachial plexus injury. Indian J. Plast. Surg. 2007, 40, 39–46. [Google Scholar] [CrossRef]
- Sousa, R.; Pereira, A.; Massada, M.; Trigueiros, M.; Lemos, R.; Silva, C. Shoulder arthrodesis in adult brachial plexus injury: What is the optimal position? J. Hand Surg. Eur. Vol. 2011, 36, 541–547. [Google Scholar] [CrossRef]
- Thangarajah, T.; Lambert, S.M. Glenohumeral arthrodesis for late reconstruction of flail shoulder in patients with traumatic supraclavicular brachial plexus palsy. Shoulder Elb. 2017, 9, 266–271. [Google Scholar] [CrossRef]
- van der Lingen, M.A.J.; de Joode, S.; Schotanus, M.G.M.; Grimm, B.; van Nie, F.A.; Speth, L.; Samijo, S.K. Satisfied patients after shoulder arthrodesis for brachial plexus lesions even after 20 years of follow-up. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1089–1094. [Google Scholar] [CrossRef]
- Elhassan, B.; Bishop, A.; Shin, A.; Spinner, R. Shoulder tendon transfer options for adult patients with brachial plexus injury. J. Hand Surg. 2010, 35, 1211–1219. [Google Scholar] [CrossRef]
- Desai, V.; Stambulic, T.; Daneshvar, P.; Bicknell, R.T. Lower trapezius tendon transfer for irreparable rotator cuff injuries: A scoping review. JSES Rev. Rep. Tech. 2023, 3, 1–9. [Google Scholar] [CrossRef]
- Scalise, J.J.; Iannotti, J.P. Glenohumeral arthrodesis after failed prosthetic shoulder arthroplasty. J. Bone Jt. Surg. 2008, 90, 70–77. [Google Scholar] [CrossRef]

| Age (Years) | FU (Months) | Age of Lesion (Mean, Range) | Type of Tendon Transfer | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Year | LOE | N | Male, % | Mean | Range | Mean | Range | ||
| Arthrodesis | ||||||||||
| Atlan [18] | 2012 | 3 | 54 | 100 | 24 | 18–51 | 42 | 3–81 | 31 (7–57) | |
| Chammas [21] | 2004 | 3 | 27 | 93 | 25 | 17–37 | 71 | 33 | ||
| Cho [22] | 2023 | 4 | 15 | 93 | 31.6 | 20–47 | 40.9 | 10–94 | ||
| Degeorge [24] | 2019 | 3 | 38 | 30 | 18–60 | 58.1 | 24–188 | |||
| Emmelot [26] | 1997 | 3 | 12 | 83 | 19 | 16–26 | 84 | 6–108 | 32 | |
| Esenyel [27] | 2011 | 4 | 8 | 88 | 39.3 | 22–68 | 66.6 | 47–96 | ||
| Lenoir [29] | 2017 | 4 | 8 | 100 | 33 | 26–58 | 28 | 12–40 | 46 (21–93) | |
| Sousa [34] | 2011 | 4 | 13 | 85 | 46 | 35–68 | 101 | 13–149 | ||
| Thangarajah [35] | 2017 | 4 | 7 | 86 | 48 | 28–80 | 98 | 27–197 | 60 (30–96) | |
| van der Lingen [36] | 2018 | 4 | 12 | 92 | 46 | 27–61 | 238 | |||
| Tendon Transfer | ||||||||||
| Agrawal [17] | 2015 | 2 | 32 | 23.5 | 17–42 | 8.25 | Upper trap | |||
| Aziz [19] | 1990 | 4 | 27 | 85 | 31.2 | 14–58 | 14.6 | 6–46 | 31.3 (6–120) | Upper trap |
| Bertelli [20] | 2011 | 4 | 7 | 100 | 27.6 | 21–41 | 11.7 | 6–36 | Upper + lower trap | |
| Crepaldi [23] | 2019 | 2 | 10 | 100 | 24 | 6 | 15.1 | Lower trap | ||
| Elhassan [4] | 2012 | 4 | 52 | 79 | 27 | 20–69 | 19 | 12–28 | Lower trap | |
| Elhassan [25] | 2016 | 4 | 12 | 83 | 35 | 19–59 | 23 | 12–37 | 19 | Lower trap |
| Karki [28] | 2020 | 4 | 12 | 100 | 26.7 | 21–34 | 6 | 24 (14–36) | Upper trap | |
| Mir-Bullo [30] | 1998 | 4 | 6 | 100 | 28 | 20–42 | 19 | 12–25 | 31 (12–57) | Upper trap |
| Monreal [31] | 2007 | 4 | 10 | 80 | 28.3 | 17–41 | 17.5 | 16–52 | 37.2 (14–75) | Upper trap |
| Rayidi [12] | 2021 | 4 | 13 | 100 | 30 | 17–47 | 12 | Levator scapulae | ||
| Rühmann [32] | 2005 | 4 | 80 | 86 | 31 | 18–69 | 28.8 | 9.6–96 | 73.2 (9.6–444) | Upper trap |
| Singh [33] | 2007 | 4 | 8 | 88 | 31.5 | 18–50 | 15.3 | 10–24 | 20.3 (11–36) | Upper trap |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lauck, B.J.; Cathey, J.M.; Mobley, J.; Kim, J.K.; Hurley, E.T.; Crook, B.S.; Saltzman, E.B.; Li, N.Y. Differentiating Outcomes and Complications Between Extraplexal Tendon Transfers and Arthrodesis for Shoulder Reanimation Following Traumatic Brachial Plexus Injury: A Systematic Review and Proportional Meta-Analysis. J. Clin. Med. 2025, 14, 7911. https://doi.org/10.3390/jcm14227911
Lauck BJ, Cathey JM, Mobley J, Kim JK, Hurley ET, Crook BS, Saltzman EB, Li NY. Differentiating Outcomes and Complications Between Extraplexal Tendon Transfers and Arthrodesis for Shoulder Reanimation Following Traumatic Brachial Plexus Injury: A Systematic Review and Proportional Meta-Analysis. Journal of Clinical Medicine. 2025; 14(22):7911. https://doi.org/10.3390/jcm14227911
Chicago/Turabian StyleLauck, Bradley J., Jackson M. Cathey, Julian Mobley, Joshua K. Kim, Eoghan T. Hurley, Bryan S. Crook, Eliana B. Saltzman, and Neill Y. Li. 2025. "Differentiating Outcomes and Complications Between Extraplexal Tendon Transfers and Arthrodesis for Shoulder Reanimation Following Traumatic Brachial Plexus Injury: A Systematic Review and Proportional Meta-Analysis" Journal of Clinical Medicine 14, no. 22: 7911. https://doi.org/10.3390/jcm14227911
APA StyleLauck, B. J., Cathey, J. M., Mobley, J., Kim, J. K., Hurley, E. T., Crook, B. S., Saltzman, E. B., & Li, N. Y. (2025). Differentiating Outcomes and Complications Between Extraplexal Tendon Transfers and Arthrodesis for Shoulder Reanimation Following Traumatic Brachial Plexus Injury: A Systematic Review and Proportional Meta-Analysis. Journal of Clinical Medicine, 14(22), 7911. https://doi.org/10.3390/jcm14227911






