Sleep Disturbances and Disorders in Children and Adolescents with Cerebral Palsy: A Narrative Review
Abstract
1. Introduction
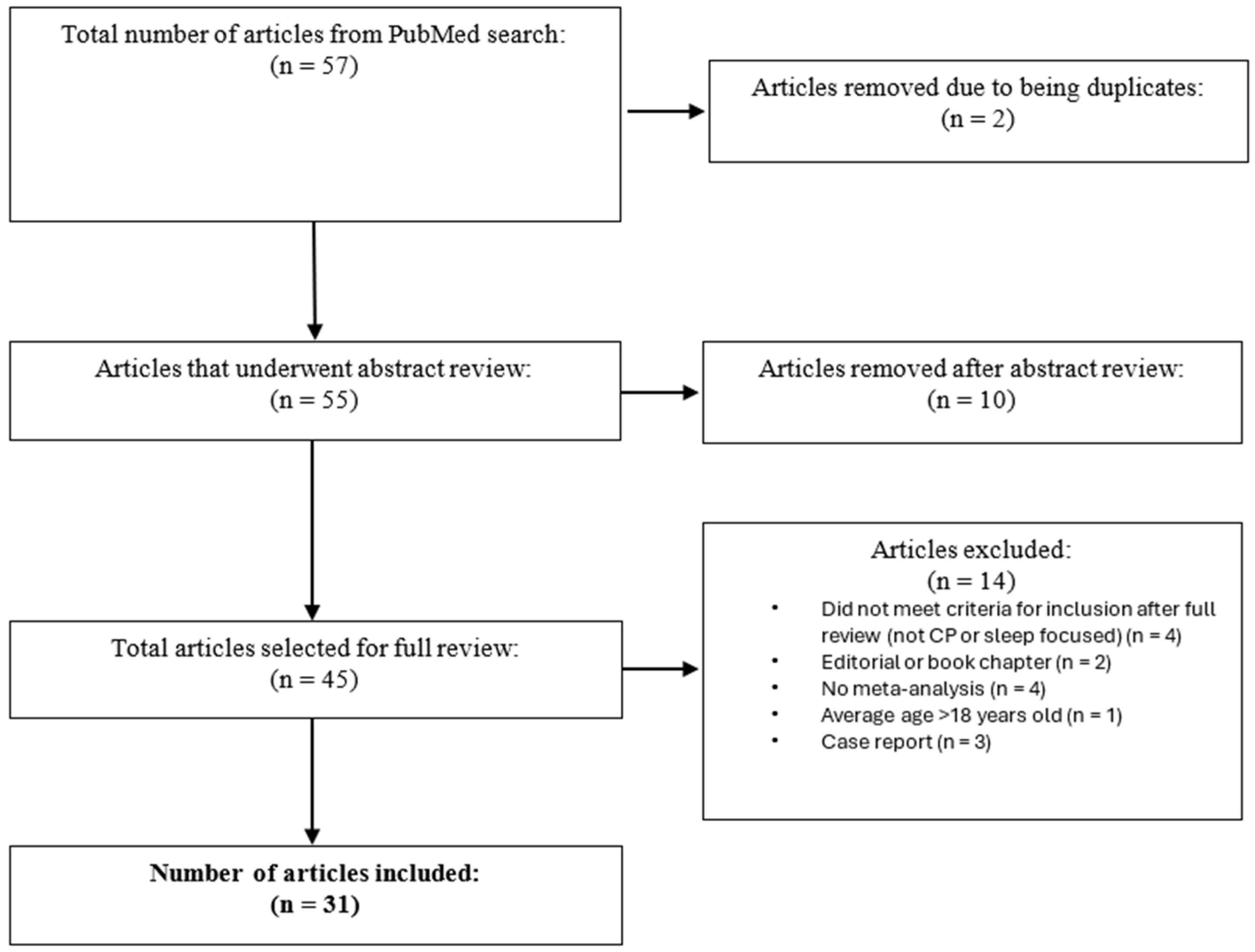
2. Materials and Methods
3. Results
3.1. Prevalence of Sleep Problems
3.2. Assessment of Sleep Concerns
3.3. Specific Sleep Concerns
3.4. Sleep and Behavior
3.5. Sleep and Pain
3.6. Sleep and Epilepsy
3.7. Sleep and Visual Impairment
3.8. Other Associated Factors, Conditions, and Sleep Problems
3.9. Sleep and Physical Activity
3.10. Sleep and Quality of Life
3.11. Effects on Caregivers
3.12. Sleep Interventions
3.12.1. Sleep Systems
3.12.2. Melatonin
3.12.3. Adenotonsillectomy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CP | Cerebral Palsy |
| GMFCS | Gross Motor Function Classification System |
| SDSC | Sleep Disturbance Scale for Children |
| DIMS | Disorder of Initiating and Maintaining Sleep |
| DA | Disorder of Arousal |
| SWTD | Sleep–Wake Transition Disorder |
| SNAKE | Sleep Questionnaire for Children with Severe Psychomotor Impairment |
References
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral Palsy. Nat. Rev. Dis. Primers 2016, 2, 15082. [Google Scholar] [CrossRef]
- Patel, D.R.; Bovid, K.M.; Rausch, R.; Ergun-Longmire, B.; Goetting, M.; Merrick, J. Cerebral Palsy in Children: A Clinical Practice Review. Curr. Probl. Pediatr. Adolesc. Health Care 2024, 54, 101673. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, S.; Goldsmith, S.; Webb, A.; Ehlinger, V.; Hollung, S.J.; McConnell, K.; Arnaud, C.; Smithers-Sheedy, H.; Oskoui, M.; Khandaker, G.; et al. Global Prevalence of Cerebral Palsy: A Systematic Analysis. Dev. Med. Child Neurol. 2022, 64, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- Vitrikas, K.; Dalton, H.; Breish, D. Cerebral Palsy: An Overview. Am. Fam. Physician 2020, 101, 213–220. [Google Scholar]
- Novak, I.; Hines, M.; Goldsmith, S.; Barclay, R. Clinical Prognostic Messages from a Systematic Review on Cerebral Palsy. Pediatrics 2012, 130, e1285–e1312. [Google Scholar] [CrossRef]
- Tessier, D.W.; Hefner, J.L.; Newmeyer, A. Factors Related to Psychosocial Quality of Life for Children with Cerebral Palsy. Int. J. Pediatr. 2014, 2014, 204386. [Google Scholar] [CrossRef]
- Newman, C.J.; O’Regan, M.; Hensey, O. Sleep Disorders in Children with Cerebral Palsy. Dev. Med. Child Neurol. 2007, 48, 564–568. [Google Scholar] [CrossRef]
- Hulst, R.Y.; Gorter, J.W.; Voorman, J.M.; Kolk, E.; Van Der Vossen, S.; Visser-Meily, J.M.A.; Ketelaar, M.; Pillen, S.; Verschuren, O. Sleep Problems in Children with Cerebral Palsy and Their Parents. Dev. Med. Child Neurol. 2021, 63, 1344–1350. [Google Scholar] [CrossRef]
- Sanguino, H.; Brunton, L.; Condliffe, E.G.; Kopala-Sibley, D.C.; Noel, M.E.; Mish, S.J.; McMorris, C.A. Sleep Characteristics of Children and Youth with Cerebral Palsy. J. Child Neurol. 2025, 40, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.; Jadhav, T.S. Prevalence of Sleep Disorders in Children with Cerebral Palsy; A Questionnaire-Based Observational Study. J. Pediatr. Neurosci. 2021, 16, 269–272. [Google Scholar] [CrossRef] [PubMed]
- Simard-Tremblay, E.; Constantin, E.; Gruber, R.; Brouillette, R.T.; Shevell, M. Sleep in Children with Cerebral Palsy: A Review. J. Child Neurol. 2011, 26, 1303–1310. [Google Scholar] [CrossRef]
- Horwood, L.; Li, P.; Mok, E.; Oskoui, M.; Shevell, M.; Constantin, E. Health-Related Quality of Life in Canadian Children with Cerebral Palsy: What Role Does Sleep Play? Sleep Med. 2019, 54, 213–222. [Google Scholar] [CrossRef] [PubMed]
- Petersen, S.; Reddihough, D.S.; Lima, S.; Harvey, A.; Newall, F. Barriers and Facilitators to Seeking Sleep Solutions for Children With Cerebral Palsy: A Qualitative Study. Front. Psychiatry 2021, 12, 729386. [Google Scholar] [CrossRef] [PubMed]
- Hulst, R.Y.; Voorman, J.M.; Pillen, S.; Ketelaar, M.; Visser-Meily, J.M.A.; Verschuren, O. Parental Perspectives on Care for Sleep in Children with Cerebral Palsy: A Wake-up Call. Disabil. Rehabil. 2022, 44, 458–467. [Google Scholar] [CrossRef]
- Horwood, L.; Li, P.; Mok, E.; Oskoui, M.; Shevell, M.; Constantin, E. Behavioral Difficulties, Sleep Problems, and Nighttime Pain in Children with Cerebral Palsy. Res. Dev. Disabil. 2019, 95, 103500. [Google Scholar] [CrossRef]
- Horwood, L.; Li, P.; Mok, E.; Shevell, M.; Constantin, E. A Systematic Review and Meta-Analysis of the Prevalence of Sleep Problems in Children with Cerebral Palsy: How Do Children with Cerebral Palsy Differ from Each Other and from Typically Developing Children? Sleep Health 2019, 5, 555–571. [Google Scholar] [CrossRef]
- Ostojic, K.; Paget, S.; Kyriagis, M.; Morrow, A. Acute and Chronic Pain in Children and Adolescents With Cerebral Palsy: Prevalence, Interference, and Management. Arch. Phys. Med. Rehabilitation 2020, 101, 213–219. [Google Scholar] [CrossRef]
- Petersen, S.; Francis, K.L.; Reddihough, D.S.; Lima, S.; Harvey, A.; Newall, F. Sleep Problems and Solution Seeking for Children with Cerebral Palsy and Their Parents. J. Paediatr. Child Health 2020, 56, 1108–1113. [Google Scholar] [CrossRef]
- Smit, D.J.M.; Zwinkels, M.; Takken, T.; Hulst, R.Y.; de Groot, J.F.; Lankhorst, K.; Verschuren, O. Sleep Quantity and Its Relation with Physical Activity in Children with Cerebral Palsy; Insights Using Actigraphy. J. Paediatr. Child Health 2020, 56, 1618–1622. [Google Scholar] [CrossRef]
- Löwing, K.; Gyllensvärd, M.; Tedroff, K. Exploring Sleep Problems in Young Children with Cerebral Palsy—A Population-Based Study. Eur. J. Paediatr. Neurol. 2020, 28, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Dreier, L.A.; Kapanci, T.; Lonnemann, K.; Koch-Hogrebe, M.; Wiethoff-Ubrig, L.; Rauchenzauner, M.; Blankenburg, M.; Zernikow, B.; Wager, J.; Rostasy, K. Assessment of Sleep-Related Problems in Children with Cerebral Palsy Using the Snake Sleep Questionnaire. Children 2021, 8, 772. [Google Scholar] [CrossRef]
- Leader, G.; Molina Bonilla, P.; Naughton, K.; Maher, L.; Casburn, M.; Arndt, S.; Mannion, A. Complex Comorbid Presentations Are Associated with Harmful Behavior Problems among Children and Adolescents with Cerebral Palsy. Dev. Neurorehabil. 2021, 24, 25–34. [Google Scholar] [CrossRef]
- Obrecht, A.; Fischer de Almeida, M.; Maltauro, L.; Leite da Silva, W.D.; Bueno Zonta, M.; de Souza Crippa, A.C. The Relationship between Gross Motor Function Impairment in Cerebral Palsy and Sleeping Issues of Children and Caregivers. Sleep Med. 2021, 81, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Mohon, R.T.; Sawyer, K.; Pickett, K.; Bothwell, S.; Brinton, J.T.; Sobremonte-King, M.; Delrosso, L.M. Sleep-Related Breathing Disorders Associated with Intrathecal Baclofen Therapy to Treat Patients with Cerebral Palsy: A Cohort Study and Discussion. NeuroRehabilitation 2021, 48, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.P.; Boucaut, A.; Guppy, M.; Johnston, L.M. Children with Cerebral Palsy: A Cross-Sectional Study of Their Sleep and Their Caregiver’s Sleep Quality, Psychological Health and Well-Being. Child Care Health Dev. 2021, 47, 859–868. [Google Scholar] [CrossRef]
- Badaru, U.M.; Hassan, A.M.; Ahmad, R.Y.; Nuhu, J.M.; Lawal, I.U. Prevalence, Pattern and Impact of Sleep Disturbance on Quality of Life and Exercise Participation among Children with Cerebral Palsy in Kano City. Sleep Sci. 2021, 14, 348–356. [Google Scholar] [CrossRef]
- Xue, B.; Licis, A.; Boyd, J.; Hoyt, C.R.; Ju, Y.E.S. Validation of Actigraphy for Sleep Measurement in Children with Cerebral Palsy. Sleep Med. 2022, 90, 65–73. [Google Scholar] [CrossRef]
- Chia, A.Z.; Tan, Y.H.; Yeo, T.H.; Teoh, O.H.; Min, N.Z. Epidemiology and Risk Factors for Sleep Disturbances in Children and Youth with Cerebral Palsy: An ICF-Based Approach. Sleep Med. 2022, 96, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Leader, G.; Mooney, A.; Chen, J.L.; Whelan, S.; Naughton, K.; Maher, L.; Mannion, A. The Co-Occurrence of Autism Spectrum Disorder and Cerebral Palsy and Associated Comorbid Conditions in Children and Adolescents. Dev. Neurorehabil. 2022, 25, 289–297. [Google Scholar] [CrossRef]
- Wood, N.; Brown, S. An Exploratory Study: The Effects of Sleep Systems on Sleep Quality, Pain and Carer Goals for Non-Ambulant Children and Young People with Cerebral Palsy. J. Rehabil. Assist. Technol. Eng. 2022, 9, 20556683211070729. [Google Scholar] [CrossRef]
- Samota, P.; Singh, A.; Aggarwal, A.; Malhotra, R. Sleep Disorders and Quality of Life in Children with Cerebral Palsy. Indian J. Pediatr. 2023, 90, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Wolter, N.E.; Scheffler, P.; Li, C.; End, C.; McKinnon, N.K.; Narang, I.; Amin, R.; Chiang, J.; Matava, C.; Propst, E.J. Adenotonsillectomy for Obstructive Sleep Apnea in Children with Cerebral Palsy: Risks and Benefits. Int. J. Pediatr. Otorhinolaryngol. 2023, 174, 111743. [Google Scholar] [CrossRef]
- Gunaydin, E.I.; Tuncer, A. The Effect of Functional Independence Levels on Sleep and Constipation in Children with Cerebral Palsy. Rev. Assoc. Med. Bras. 2023, 69, e20230765. [Google Scholar] [CrossRef]
- Hulst, R.Y.; Gorter, J.W.; Obeid, J.; Voorman, J.M.; van Rijssen, I.M.; Gerritsen, A.; Visser-Meily, J.M.A.; Pillen, S.; Verschuren, O. Accelerometer-Measured Physical Activity, Sedentary Behavior, and Sleep in Children with Cerebral Palsy and Their Adherence to the 24-Hour Activity Guidelines. Dev. Med. Child Neurol. 2023, 65, 393–405. [Google Scholar] [CrossRef]
- van Rijssen, I.M.; Hulst, R.Y.; Gorter, J.W.; Gerritsen, A.; Visser-Meily, J.M.A.; Dudink, J.; Voorman, J.M.; Pillen, S.; Verschuren, O. Device-Based and Subjective Measurements of Sleep in Children with Cerebral Palsy: A Comparison of Sleep Diary, Actigraphy, and Bed Sensor Data. J. Clin. Sleep Med. 2023, 19, 35–43. [Google Scholar] [CrossRef]
- Kim, S.H.; Jung, J.H.; Chang, M.C.; Park, D. The Effect of Intensive Rehabilitation Treatment on Sleep Disorder in Children with Motor Delays. BMC Pediatr. 2023, 23, 291. [Google Scholar] [CrossRef]
- Shearer, H.M.; Côtè, P.; Hogg-Johnson, S.; Fehlings, D.L. A Good Night’s Sleep: Pain Trajectories and Sleep Disturbance in Children with Cerebral Palsy. J. Clin. Sleep Med. 2024, 20, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Goldouzi, H.R.; Akhondian, J.; Beiraghi Toosi, M.; Mahrad Majd, H.; Shekari, S.; Babaei, M. The Effect of Melatonin on Sleep Disorders in Children with Cerebral Palsy A Randomized Clinical Trial. Iran. J. Child Neurol. 2024, 18, 51–59. [Google Scholar] [CrossRef]
- Whittingham, K.; Benfer, K.; Sakzewski, L.; Wotherspoon, J.; Burgess, A.; Comans, T.; Keramat, S.A.; Ware, R.S.; Boyd, R.N. Sleep Problems in a Population-Based Cohort of Primary School Age Children with Cerebral Palsy. Res. Dev. Disabil. 2024, 147, 104690. [Google Scholar] [CrossRef]
- Gerritsen, A.; Hulst, R.Y.; van Rijssen, I.M.; Obeid, J.; Pillen, S.; Gorter, J.W.; Verschuren, O. The Temporal and Bi-Directional Relationship between Physical Activity and Sleep in Ambulatory Children with Cerebral Palsy. Disabil. Rehabil. 2024, 46, 2821–2827. [Google Scholar] [CrossRef] [PubMed]
- Nisbet, L.C.; Davey, M.J.; Nixon, G.M. Periodic Limb Movements during Sleep in Children with Neuromuscular Disease or Cerebral Palsy—An Important Potential Contributor to Sleep-Related Morbidity. Sleep Med. 2024, 121, 58–62. [Google Scholar] [CrossRef]
- Matricciani, L.; Paquet, C.; Galland, B.; Short, M.; Olds, T. Children’s Sleep and Health: A Meta-Review. Sleep Med. Rev. 2019, 46, 136–150. [Google Scholar] [CrossRef]
- Shochat, T.; Cohen-Zion, M.; Tzischinsky, O. Functional Consequences of Inadequate Sleep in Adolescents: Asystematic Review. Sleep Med. Rev. 2014, 18, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Ji, X.; Pitt, S.; Wang, G.; Rovit, E.; Lipman, T.; Jiang, F. Childhood Sleep: Physical, Cognitive, and Behavioral Consequences and Implications. World J. Pediatr. 2024, 20, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Alrousan, G.; Hassan, A.; Pillai, A.A.; Atrooz, F.; Salim, S. Early Life Sleep Deprivation and Brain Development: Insights From Human and Animal Studies. Front. Neurosci. 2022, 16, 833786. [Google Scholar] [CrossRef]
- Riggins, T.; Ratliff, E.L.; Horger, M.N.; Spencer, R.M.C. The Importance of Sleep for the Developing Brain. Curr. Sleep Med. Rep. 2024, 10, 437–446. [Google Scholar] [CrossRef]
- Lam, L.T.; Lam, M.K. Sleep Disorders in Early Childhood and the Development of Mental Health Problems in Adolescents: A Systematic Review of Longitudinal and Prospective Studies. Int. J. Environ. Res. Public Health 2021, 18, 11782. [Google Scholar] [CrossRef] [PubMed]
- Winsor, A.A.; Richards, C.; Bissell, S.; Seri, S.; Liew, A.; Bagshaw, A.P. Sleep Disruption in Children and Adolescents with Epilepsy: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2021, 57, 101416. [Google Scholar] [CrossRef]
- Gibbon, F.M.; Maccormac, E.; Gringras, P. Sleep and Epilepsy: Unfortunate Bedfellows. Arch. Dis. Child 2019, 104, 189–192. [Google Scholar] [CrossRef]
- Whitney, R.; Sharma, S.; Ramachandrannair, R. Sudden Unexpected Death in Epilepsy in Children. Dev. Med. Child Neurol. 2023, 65, 1150–1156. [Google Scholar] [CrossRef]
- Allen, J.M.; Graef, D.M.; Ehrentraut, J.H.; Tynes, B.L.; Crabtree, V.M. Sleep and Pain in Pediatric Illness: A Conceptual Review. CNS Neurosci. Ther. 2016, 22, 880–893. [Google Scholar] [CrossRef] [PubMed]
- Mckinnon, C.T.; Meehan, E.M.; Harvey, A.R.; Antolovich, G.C.; Morgan, P.E. Prevalence and Characteristics of Pain in Children and Young Adults with Cerebral Palsy: A Systematic Review. Dev. Med. Child Neurol. 2019, 61, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Vinkel, M.N.; Rackauskaite, G.; Finnerup, N.B. Classification of Pain in Children with Cerebral Palsy. Dev. Med. Child Neurol. 2022, 64, 447–452. [Google Scholar] [CrossRef]
- Albinni, B.; de Zambotti, M.; Iacovides, S.; Baker, F.C.; King, C.D. The Complexities of the Sleep-Pain Relationship in Adolescents: A Critical Review. Sleep Med. Rev. 2023, 67, 101715. [Google Scholar] [CrossRef]
- Hollung, S.J.; Bakken, I.J.; Vik, T.; Lydersen, S.; Wiik, R.; Aaberg, K.M.; Andersen, G.L. Comorbidities in Cerebral Palsy: A Patient Registry Study. Dev. Med. Child Neurol. 2020, 62, 97–103. [Google Scholar] [CrossRef]
- Campbell, D.I.; Andrew, M.J. Gastrointestinal Problems in Children with Cerebral Palsy. In Cerebral Palsy: From Childhood to Adulthood, 4th ed.; Christos, P., Ed.; Springer: Cham, Switzerland, 2025; pp. 397–405. [Google Scholar] [CrossRef]
- Bourchtein, E.; Langberg, J.M.; Eadeh, H.-M. A Review of Pediatric Nonpharmacological Sleep Interventions: Effects on Sleep, Secondary Outcomes, and Populations With Co-Occurring Mental Health Conditions. Behav. Ther. 2020, 51, 27–41. [Google Scholar] [CrossRef]
- Lunsford-Avery, J.R.; Bidopia, T.; Jackson, L.; Sloan, J.S. Behavioral Treatment of Insomnia and Sleep Disturbances in School-Aged Children and Adolescents. Psychiatr. Clin. N. Am. 2024, 47, 103–120. [Google Scholar] [CrossRef]
- de Almeida, M.F.; Mello, S.; Zonta, M.B.; Crippa, A.C. Cerebral Palsy and Sleep: Nonpharmacological Treatment and Impact on the Life of Caregivers—An Integrative Review. Arq. de Neuro-Psiquiatria 2024, 82, S00441781464. [Google Scholar] [CrossRef]
- Tanner, K.; Noritz, G.; Ayala, L.; Byrne, R.; Fehlings, D.; Gehred, A.; Letzkus, L.; Novak, I.; Rosenberg, N.; Vargus-Adams, J.; et al. Assessments and Interventions for Sleep Disorders in Infants With or at High Risk for Cerebral Palsy: A Systematic Review. Pediatr. Neurol. 2021, 118, 57–71. [Google Scholar] [CrossRef]
- Morgan, C.; Fetters, L.; Adde, L.; Badawi, N.; Bancale, A.; Boyd, R.N.; Chorna, O.; Cioni, G.; Damiano, D.L.; Darrah, J.; et al. Early Intervention for Children Aged 0 to 2 Years with or at High Risk of Cerebral Palsy: International Clinical Practice Guideline Based on Systematic Reviews. JAMA Pediatr. 2021, 175, 846–858. [Google Scholar] [CrossRef] [PubMed]
- Phillips, N.L.; Moore, T.; Teng, A.; Brookes, N.; Palermo, T.M.; Lah, S. Behavioral Interventions for Sleep Disturbances in Children with Neurological and Neurodevelopmental Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Sleep 2020, 43, zsaa040. [Google Scholar] [CrossRef] [PubMed]
- Hornsey, S.J.; Gosling, C.J.; Jurek, L.; Nourredine, M.; Telesia, L.; Solmi, M.; Butt, I.; Greenwell, K.; Muller, I.; Hill, C.M.; et al. Umbrella Review and Meta-Analysis: The Efficacy of Nonpharmacological Interventions for Sleep Disturbances in Children and Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2025, 64, 329–345. [Google Scholar] [CrossRef] [PubMed]
- De Pasquale, C.; El Kazzi, M.; Sutherland, K.; Shriane, A.E.; Vincent, G.E.; Cistulli, P.A.; Bin, Y.S. Sleep Hygiene—What Do We Mean? A Bibliographic Review. Sleep Med. Rev. 2024, 75, 101930. [Google Scholar] [CrossRef]
- Ogundele, M.O.; Yemula, C. Management of Sleep Disorders among Children and Adolescents with Neurodevelopmental Disorders: A Practical Guide for Clinicians. World J. Clin. Pediatr. 2022, 11, 239–252. [Google Scholar] [CrossRef]
- Malow, B.A.; Adkins, K.W.; Reynolds, A.; Weiss, S.K.; Loh, A.; Fawkes, D.; Katz, T.; Goldman, S.E.; Madduri, N.; Hundley, R.; et al. Parent-Based Sleep Education for Children with Autism Spectrum Disorders. J. Autism Dev. Disord. 2014, 44, 216–228. [Google Scholar] [CrossRef]
- Rigney, G.; Ali, N.S.; Corkum, P.V.; Brown, C.A.; Constantin, E.; Godbout, R.; Hanlon-Dearman, A.; Ipsiroglu, O.; Reid, G.J.; Shea, S.; et al. A Systematic Review to Explore the Feasibility of a Behavioural Sleep Intervention for Insomnia in Children with Neurodevelopmental Disorders: A Transdiagnostic Approach. Sleep Med. Rev. 2018, 41, 244–254. [Google Scholar] [CrossRef]
- Hutson, J.A.; Snow, L.A. Sleep Assessments for Children With Severe Cerebral Palsy: A Scoping Review. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100087. [Google Scholar] [CrossRef]
- Sivertsen, B.; Harvey, A.G.; Reichborn-Kjennerud, T.; Torgersen, L.; Ystrom, E.; Hysing, M. Later Emotional and Behavioral Problems Associated with Sleep Problems in Toddlers: A Longitudinal Study. JAMA Pediatr. 2015, 169, 575–582. [Google Scholar] [CrossRef]
- Liu, J.; Glenn, A.L.; Cui, N.; Raine, A. Longitudinal Bidirectional Association between Sleep and Behavior Problems at Age 6 and 11 Years. Sleep Med. 2021, 83, 290–298. [Google Scholar] [CrossRef]
- Astill, R.G.; Van der Heijden, K.B.; Van Ijzendoorn, M.H.; Van Someren, E.J.W. Sleep, Cognition, and Behavioral Problems in School-Age Children: A Century of Research Meta-Analyzed. Psychol. Bull. 2012, 138, 1109–1138. [Google Scholar] [CrossRef] [PubMed]
| Author/Year | Purpose | Study Design | Sample | Relevant Findings |
|---|---|---|---|---|
| Horwood, Li, Mok, Oskoui, Shevell, & Constantin (2019) [15] | Determine the prevalence of behavioral challenges in preschool- and school-aged children with CP and assess the association between behavioral challenges and sleep problems, nighttime pain, and child characteristics. | Cross-Sectional | Caregivers of 113 children with CP | Approximately 26% of children with CP had behavioral challenges. Sleep problems and nighttime pain were also associated with behavioral challenges. Sleep and behavioral problems were highly associated even when adjusting for nighttime pain and age. |
| Horwood, Li, Mok, Shevell, & Constantin (2019) [16] | Review and conduct a meta-analysis of the literature to determine the prevalence of sleep problems in children with CP, including prevalence in various subgroups. | Meta-Analysis | 23 English or French studies included, representing 2908 children with CP | Older children with CP had higher rates of sleep problems than younger children; children with more severe CP phenotype had more sleep problems than children with milder phenotype; and children with CP and additional comorbidities such as epilepsy and auditory, visual, and cognitive impairments had more sleep problems than children without comorbidities. The effects of comorbidities on sleep were not consistent across all studies reviewed. |
| Ostojic, Paget, Kyriagis, & Morrow (2020) [17] | Determine the prevalence, impact, and management of pain in children with CP. | Cross-Sectional | 280 children with CP between the ages of 5 and 18 years old and their caregivers | Acute pain was reported by 67.1% of participants and chronic pain was reported by 31.4% of participants. Pain frequently interferes with sleep. |
| Petersen, Francis, Reddihough, Lima, Harvey, & Newall (2020) [18] | Determine the frequency and type of sleep problems for children with CP with their parents. Explore whether and from whom parents seek help for sleep concerns. Determine whether the parents who sought help found the advice/treatment effective. | Population-Based Cohort (Online) Survey | 126 parents/caregivers of children with CP | Sleep is a problem for half the cohort studied. Parents of children with CP who have sleep problems are more likely to have problems with sleep themselves. GMFCS level does not seem to be related to sleep problems (problems were reported across all levels). Help for sleep problems is not always effective (effective ~30% of the time). |
| Smit, Zwinkels, Takken, Hulst, de Groot, Lankhorst., & Verschuren (2020) [19] | Explore the relationship between sleep quantity, sleep quality, physical activity, and sedentary behavior in children with CP, in addition to assessing their sleep quantity. | Cross-Sectional | 36 children with spastic CP with an average age of 15 years old | Sedentary behavior is correlated with sleep quantity in children with CP. Children with CP in this sample were getting the recommended duration of sleep. |
| Löwing, Gyllensvärd, & Tedroff (2020) [20] | Describe and explore insomnia in children with CP ages 5–10. | Explorative Cross-Sectional Design | 118 children with CP included in first part of study (medical records review); 95 parents/caregivers of the original 118 participated in second part of study (pre-structured telephone interview) | Insomnia was present to a high extent in this cohort. Sleep problems were reported across all subtypes and GMFCS levels but were most common in level V and those with dyskinetic CP. Sleep problems were moderately associated with the presence of seizures. Pain was highly correlated with sleep problems. A relationship could exist between sleep problems and motor limitations/GMFCS levels. |
| Hulst, Gorter, Voorman, Kolk, Van Der Vossen, Visser-Meily, Ketelaar, Pillen, & Verschuren (2021) [8] | Describe the frequency and type of parent-reported sleep problems. Describe parent-reported satisfaction with their sleep and child sleep. Describe child factors related to sleep problems. Compare sleep outcomes between typically developing children and those with CP. | Multicenter Cross-Sectional Study with Comparison Group | 90 children with CP and their parents; comparison group included 157 typically developing children and their parents | Children with CP were more likely to have sleep problems than typically developing children (72.2% vs. 46.4%), and these problems are more significant for non-ambulatory children. These problems more significantly impact daily functioning for children with CP. These problems result in less parental satisfaction in their child’s sleep. No significant difference between parents of children with CP and parents of typically developing children in their own sleep satisfaction or sleep deprivation. Non-ambulatory children with CP also experience greater impairment in daily functioning related to sleep problems than ambulatory children with CP. |
| Kulkarni & Jadhav (2021) [10] | Examine prevalence and pattern of sleep disorders in children with CP. | Questionnaire-Based Observational Study | 200 children with CP between the ages of 1 and 14 years old; children with health problems involving cardiorespiratory system, gastroesophageal reflux, epilepsy, or children taking anticonvulsant medications were excluded | Of the sample, 62% of had a pathological total sleep score on the Sleep Disturbance Scale for Children. Disorders of initiating and maintaining sleep occurred in 78.2% of participants who had a pathological sleep score. Those with GMFCS V and with quadriplegia were impacted most severely. |
| Dreier, Kapanci, Lonnemann, Koch-Hogrebe, Wiethoff-Ubrig, Rauchenzauner, Blankenburg, Zernikow, Wager, & Rostasy (2021) [21] | Explore sleep of children with CP. Considering the impact motor impairment and comorbidities, explore potential sleep problems in children with different CP subtypes. | Hospital-Based, Prospective Study | 100 children with CP between the ages of 2 and 18 years old | Associations were found between gross motor functioning and fine motor functioning and CP comorbidities. Functional impairment (as measured by gross or fine motor functioning) is more crucial for sleep concerns than CP or CP subtype. |
| Leader, Molina Bonilla, Naughton, Maher, Casburn, Arndt, & Mannion (2021) [22] | Identify frequency of GI symptoms, sleep problems, internalizing/externalizing symptoms, and ASD symptoms in a sample of children with CP. Examine impact of comorbidities on frequency and severity of behavior problems in this sample. | Parent-Completed Questionnaires | 104 youth with CP | A high frequency of behavior problems, sleep problems, gastrointestinal symptoms, ASD symptoms, and internalizing/externalizing symptoms was found in this sample. Relationships were found between the following: sleep problems and behavior problems; GI symptoms and sleep problems; and GI symptoms and internalizing/externalizing problems. Behavior problems were predicted by sleep problems, internalizing/externalizing symptoms, ID, and ASD symptoms. |
| Petersen, Reddihough, Lima, Harvey, & Newall (2021) [13] | Examine the impact/experience of sleep disturbance in addition to the experience of seeking sleep solutions or treatment for caregivers of children with CP. | Semi-Structured Qualitative Parent Interviews with Thematic Analysis | 19 parents of children with CP | Sleep is often not a significant priority for caregivers or health professionals due to other health concerns. Parents experience difficulties and challenges in finding effective sleep interventions for their children with CP. Children’s needs are often different from what parents are provided by systems and services. |
| Obrecht, Fischer de Almeida, Maltauro, Leite da Silva, Bueno Zonta, & de Souza Crippa (2021) [23] | Investigated the influence of gross motor function impairment on sleep disturbances of children with CP, their need for nocturnal support, and caregiver quality of sleep. | Cross-Sectional | 87 children with CP | A total of 52% of children had inadequate scores in at least one factor of a sleep measure, 64% of children were taking meds that had the potential to interfere with sleep, and 44.8% of children received nocturnal support from caregivers. Children with greater gross motor impairment needed more nocturnal support. Among caregivers, 62.1% were found to have poor sleep quality. |
| Mohon, Sawyer, Pickett, Bothwell, Brinton, Sobremonte-King, & DelRosso (2021) [24] | Determine prevalence of sleep-related breathing disorders in children with CP who are receiving intrathecal baclofen therapy. | Retrospective Chart Review | 87 children with CP. Medical records were reviewed from the Children’s Hospital Colorado and Seattle Children’s Hospital between January 1st, 1995, and December 31st, 2019. Participants had to have been receiving intrathecal baclofen therapy and had at least one nocturnal polysomnography performed. | Over 82% of participants had one or more nighttime symptoms as measured on a sleep-related breathing disorder screening questionnaire. There was no worsening or improvement in sleep-related breathing disorder symptoms. |
| Lang, Boucaut, Guppy, & Johnston (2021) [25] | Examine relationship between sleep problems in children with CP, caregiver sleep, and caregiver psychological health. | Cross-Sectional | 94 caregivers of children with CP | Poor sleep quality was reported in 71% of caregivers. Sleep problems were reported in 51% of children. Children’s sleep problems and their need for nighttime attention contributed to parental sleep quality. The factor most associated with need for nighttime support was motor impairment. Caregiver sleep quality was significantly associated with their psychological health. |
| Badaru, Hassan, Ahmad, Nuhu, & Lawal (2021) [26] | Examine the prevalence of sleep disturbance in children with CP and assess the impact of sleep disturbance on exercise participation and quality of life. | Cross-Sectional | 200 children with CP and 200 siblings of children with CP | A total of 31.5% of children with CP had a sleep disturbance, and these children suffered more sleep disturbance than their siblings. This sleep disturbance had a negative impact on these children’s quality of life in addition to a negative impact on their ability to participate in exercises both at home and in a clinic-based setting. |
| Xue, Licis, Boyd, Hoyt, & Ju (2022) [27] | Validate the use of actigraphy in children with CP and assess their sleep patterns. | Cross-Sectional Cohort Study | 13 children with CP and 13 children without CP between the ages of 2 and 17 years old | Actigraphy was shown to be a valid tool for assessing sleep in children with CP. Sleep efficiency and duration were worse in children with CP. Author-developed algorithms demonstrated increased specificity and accuracy compared to existing algorithms. |
| Zh Chia, Tan, Yeo, Teoh, & Min Ng (2022) [28] | Describe sleep problems in a local population of children with CP. | Cross-Sectional | 151 participants with CP ages 1–24 (median age = 6.18) | Of the participants, 46% had difficulty with one or more aspects of sleep. GMFCS level V and involuntary muscle contractions were significant factors in sleep problems. |
| Leader, Mooney, Chen, Whelan, Naughton, Maher, & Mannion (2022) [29] | Examined frequency of comorbidities in children with ASD alone, CP alone, and those with comorbid CP and ASD. | Screening Study | 96 children with a diagnosis of CP, ASD, or comorbid CP and ASD | Significant group differences in sleep problems, social communication, and adaptive behavior. ID significantly predicted levels of adaptive behavior. |
| Hulst, Voorman, Pillen, Ketelaar, Visser-Meily, & Verschuren (2022) [14] | Explore the perspective of parents regarding sleep care for their children with CP. | Inductive Thematic Analysis of Semi-Structured Interviews | 18 parents of children with CP between the ages of 1 and 8 years old. Four of the parents had a child above the age of 8 years old and were asked to reflect on the time their child was between 1 and 8 years old | All parents interviewed expressed that they had a range of concerns or needs when caring for the sleep of their child with CP. Parents expressed concerns about caring for their child during both the day and night, perceived difficulties or deficiencies in healthcare, and had limited knowledge of or attention to sleep concerns from healthcare professionals. The authors called for a wakeup call to these parent-identified concerns and shortcomings in healthcare. |
| Wood & Brown (2022) [30] | Examine the impact of sleep systems on sleep quality/quantity and pain for youth with CP, in addition to examining the outcome for caregivers. | Exploratory Study | 4 children with CP (average age of 11.5 years old) | While pain levels remained unchanged following introduction of the sleep system, sleep quantity either improved or stayed the same as baseline. |
| Samota, Singh, Aggarwal, & Malhotra (2023) [31] | Assess the relationship between sleep disorders and quality of life in children with CP. | Cross-Sectional | 117 children with CP and additional control group (n = 117) of age- and gender-matched children without CP | Sleep disorders were more prevalent in children with CP compared to controls, and this experience of a sleep disorder was associated with a decreased quality of life for children with CP. |
| Wolter, Scheffler, Li, End, McKinnon, Narang, Amin, Chiang, Matava, & Propst (2023) [32] | Assess outcomes of adenotonsillectomy for obstructive sleep apnea in children with CP. | Retrospective Chart Review | 97 children with CP were assessed for sleep disordered breathing, and 74 underwent polysomnography. Perioperative data was available in 23 children with CP, and these children were compared to 23 age-matched children without CP. | The obstructive apnea–hypopnea index was improved for children with CP following adenotonsillectomy, but children with CP had higher rates of post-adenotonsillectomy complications. |
| Gunaydin & Tuncer (2023) [33] | Examine the impact of level of functional independence on sleep and constipation in children with CP. | Cross-Sectional Observational Study | 60 children with CP between the ages of 4 and 18 years old | Lower levels of functional independence were associated with worse sleep and symptoms of constipation in children with CP. |
| Hulst, Gorter, Obeid, Voorman, van Rijssen, Gerritsen, Visser-Meily, Pillen, & Verschuren (2023) [34] | Using actigraphy, describe and measure 24 h activities of children with CP, and examine adherence to the 24 h activity guidelines. | Cross-Sectional Observational Study | 54 children with CP aged between 3 and 12 years old | Adherence to the 24 h guidelines was low. In total, 35% of the sample met age-appropriate sleep duration recommendations. Only 5.9% of children met the combined 24 h guidelines for both physical activity and sleep. |
| van Rijssen, Hulst, Gorter, Gerritsen, Visser-Meily, Dudink, Voorman, Pillen, & Verschuren (2023) [35] | Examine how device-based and subjective assessments of sleep relate or compare to one another in children with CP. | Cross-Sectional Observational Study | 38 children with CP aged between 2 and 12 years old | Poor agreement was found between sleep diaries, actigraphy, and a bed sensor on many aspects measured. Actigraphy only had satisfactory agreement for total time in bed with the bed sensor and sleep diaries. The bed sensor only had satisfactory agreement for total time in bed and total sleep time with the sleep diaries. With consideration of these discrepancies, the authors recommended using both subjective and device-based measures to assess sleep in children with CP. |
| Kim, Jung, Chang, & Park (2024) [36] | Examine the effect of an intensive rehabilitation program on sleep problems in children with developmental delays. | Prospective Design | 36 children with developmental delays, 19 of which had CP | The intensive rehabilitation program was associated with significant improvement in difficulties initiating and maintaining sleep; however, no significant improvement in other areas, as measured by the Sleep Disturbance Scale for Children, was found. |
| Shearer, Côté, Hogg-Johnson, & Fehlings (2024) [37] | Prospectively measure the association between pain intensity trajectory and sleep disturbance. | Cohort study | 89 children with CP | An association between pain intensity trajectory and increased sleep problems was only supported for those with the most severe pain, who reported the most significant sleep disturbance. Children with decreasing pain had less perceived sleep disturbance, even if their pain level was higher at the start. Children with moderate to severe pain had greater sleep disturbance, which also worsened with time. |
| Goldouzi, Akhondian, Beiraghi Toosi, Mehrad Majd, Shekari, & Babaei (2024) [38] | Examine the effect of melatonin on sleep disorders in children with CP. | Double-blind clinical trial | 50 children with CP between the ages of 2 and 12 years old randomly assigned to the melatonin or control group | A significant effect of melatonin on sleep disorders was reported for this sample. The most significant effect of melatonin was on the duration of time to fall asleep, and melatonin was also associated with an increased sleep duration. |
| Whittingham, Benfer, Sakzewski, Wotherspoon, Burgess, Comans, Keramat, Ware, & Boyd (2024) [39] | To study sleep problems in population sample of children with CP. | Cross-Sectional | 86 children with CP | Sleep problems in children with CP are common, with 44% of participants in the clinical range for disordered sleep. Sleep problems were associated with pain-related quality of life, child behavior, and epilepsy. |
| Gerritsen, Hulst, van Rijssen, Obeid, Pillen, Gorter, & Verschuren (2024) [40] | Examine the bidirectional and temporal relationship between physical activity and sleep in children with CP who are ambulatory. | Cross-Sectional | 51 children with CP between the ages of 3 and 12 years old | Children with CP who are ambulatory may not sleep better after physical activity. This relationship is complex in children with CP and should be further investigated. |
| Nisbet, Davey, & Nixon (2024) [41] | Assess the prevalence of periodic limb movements in children with CP or neuromuscular diseases. | Retrospective Review and Analysis | 239 children, 114 of which had CP and 125 had neuromuscular diseases | Elevated periodic limb movement index was reported at a higher prevalence in children with CP or a neuromuscular disease, at 9.6% in each group. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rausch, R.A.; Miller, C.; Hensler, A.; Goetting, M.G.; Patel, D.R. Sleep Disturbances and Disorders in Children and Adolescents with Cerebral Palsy: A Narrative Review. J. Clin. Med. 2025, 14, 7828. https://doi.org/10.3390/jcm14217828
Rausch RA, Miller C, Hensler A, Goetting MG, Patel DR. Sleep Disturbances and Disorders in Children and Adolescents with Cerebral Palsy: A Narrative Review. Journal of Clinical Medicine. 2025; 14(21):7828. https://doi.org/10.3390/jcm14217828
Chicago/Turabian StyleRausch, Rebecca A., Caroline Miller, Amelia Hensler, Mark G. Goetting, and Dilip R. Patel. 2025. "Sleep Disturbances and Disorders in Children and Adolescents with Cerebral Palsy: A Narrative Review" Journal of Clinical Medicine 14, no. 21: 7828. https://doi.org/10.3390/jcm14217828
APA StyleRausch, R. A., Miller, C., Hensler, A., Goetting, M. G., & Patel, D. R. (2025). Sleep Disturbances and Disorders in Children and Adolescents with Cerebral Palsy: A Narrative Review. Journal of Clinical Medicine, 14(21), 7828. https://doi.org/10.3390/jcm14217828







