Comparing Conduction System Pacing to Biventricular Upgrade in Pacemaker-Induced Cardiomyopathy: A Retrospective Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Procedure Description
2.3. Data Collection and Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
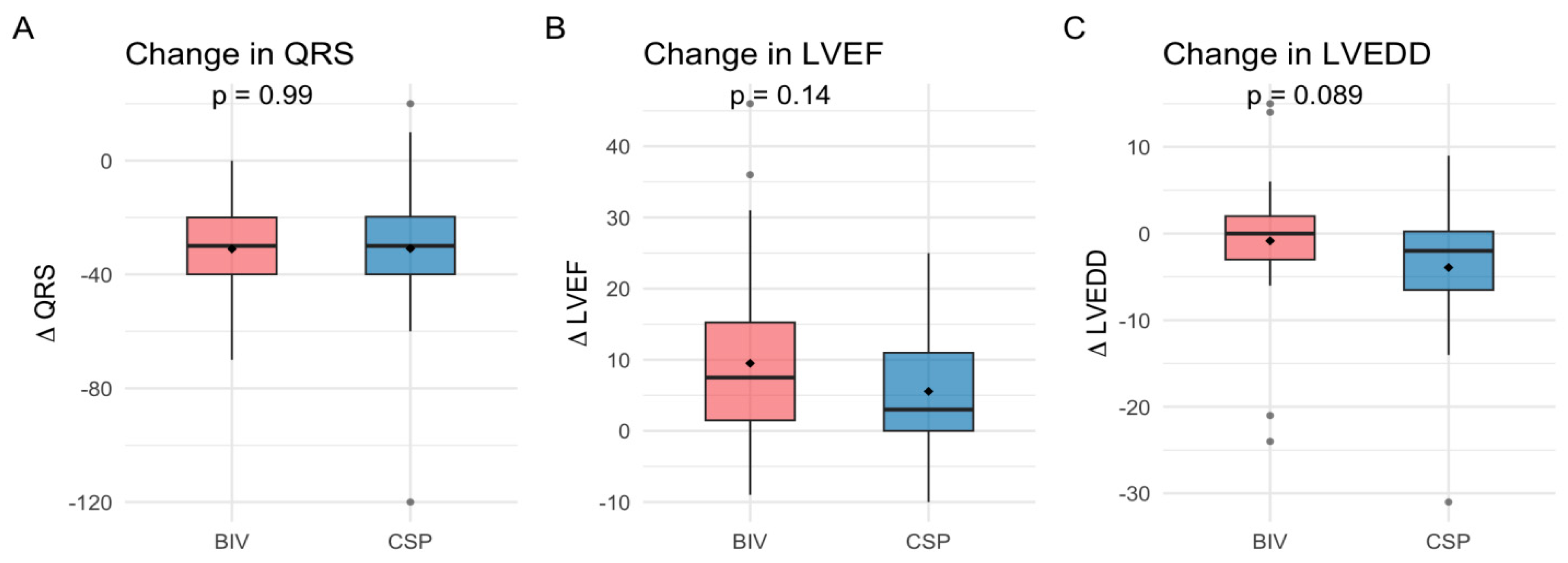
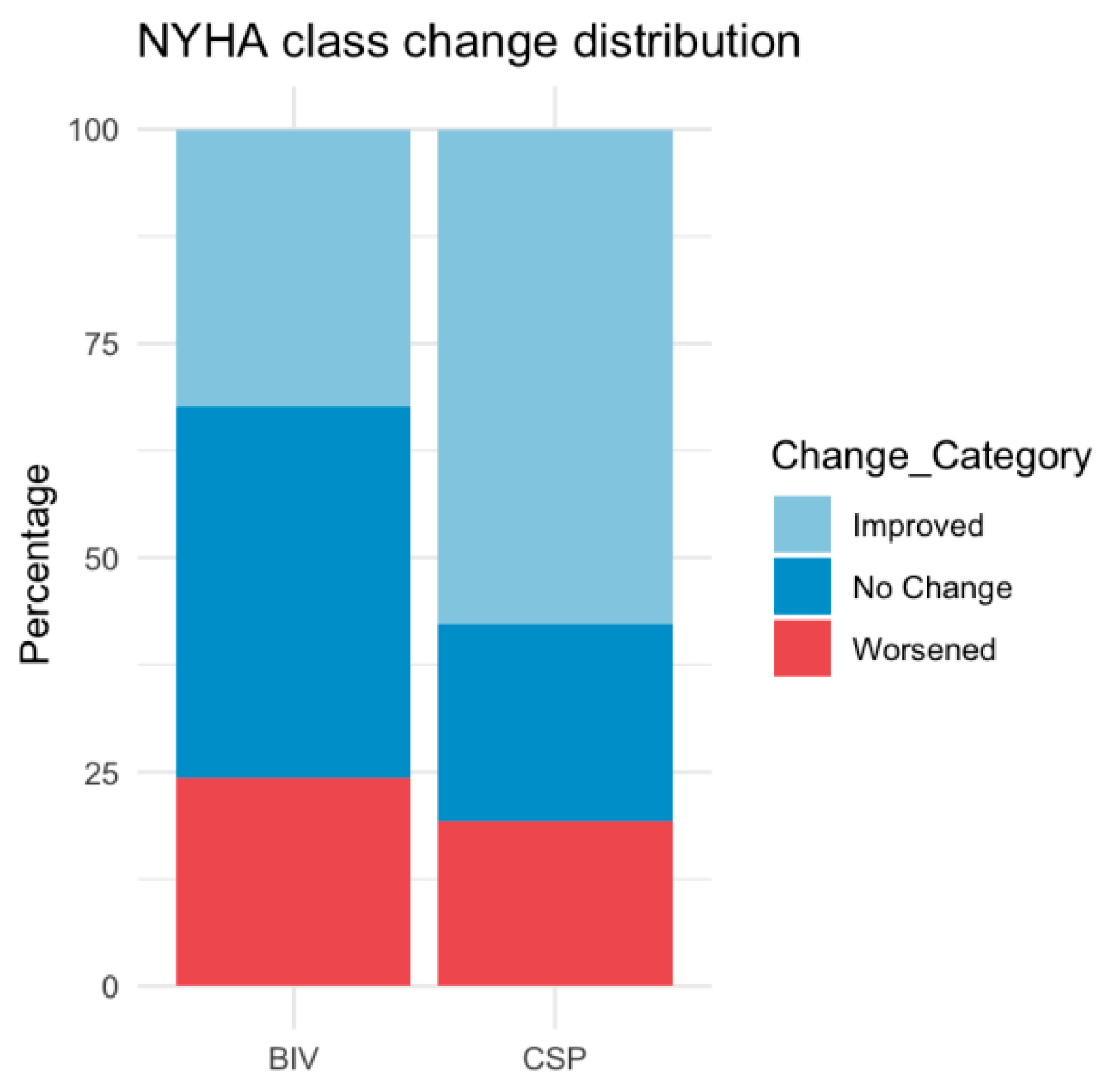
3.2. Procedural and Clinical Outcomes
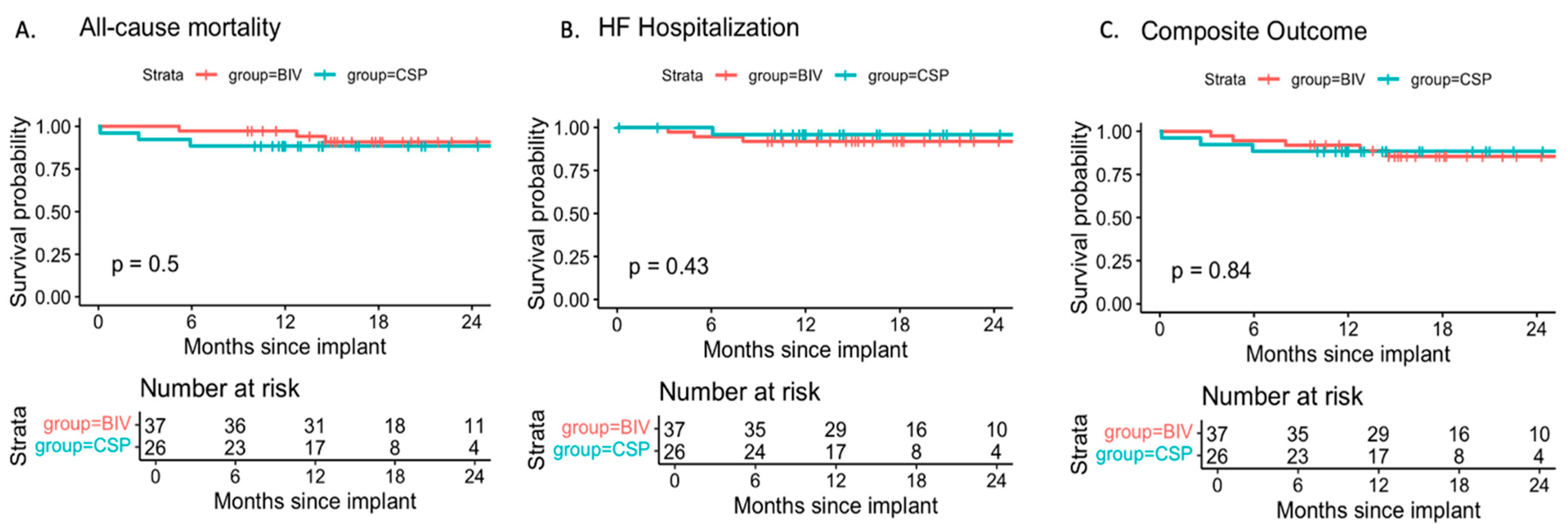
3.3. Heart Failure Hospitalization and All-Cause Mortality
3.4. Quality of Life
3.5. Financial Cost–Benefit
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with Prior Studies
4.3. Mechanistic Considerations
4.4. Cost Implications
4.5. Clinical Implications
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACEI | angiotensin-converting enzyme inhibitor |
| ACM | all-cause mortality |
| AF | atrial fibrillation |
| ANCOVA | analysis of covariance |
| APT | antiplatelet therapy |
| ARB | angiotensin II receptor blocker |
| ARNI | angiotensin receptor–neprilysin inhibitor |
| AV | atrioventricular |
| BIV | biventricular pacing (cardiac resynchronization therapy) |
| CIED | cardiac implantable electronic device |
| CKD | chronic kidney disease |
| CSP | conduction system pacing |
| HBP | His-bundle pacing |
| HFH | heart failure hospitalization |
| ICD | implantable cardioverter defibrillator |
| LAD | left atrial diameter |
| LBBB | left bundle branch block |
| LBBAP | left bundle branch area pacing |
| LV | left ventricular |
| LVEDD | left ventricular end-diastolic diameter |
| LVEF | left ventricular ejection fraction |
| MRA | mineralocorticoid receptor antagonist |
| NIVCD | nonspecific interventricular conduction disease |
| NYHA | New York Heart Association |
| PASP | pulmonary arterial systolic pressure |
| PICM | pacemaker-induced cardiomyopathy |
| QoL | quality of life |
| RAD | right atrial diameter |
| RBBB | right bundle branch block |
| RV | right ventricular |
| SDL | stylet-driven leads |
| SGLT2i | sodium–glucose co-transporter 2 inhibitor |
| SSS | sick sinus syndrome |
| TAPSE | tricuspid annular plane systolic excursion |
| TIA | transient ischemic attack |
| TR | tricuspid regurgitation |
| V6RWPeak time | V6 R-wave peak time |
| VP | ventricular pacing |
| ΔLVEF | change in left ventricular ejection fraction |
References
- Mond, H.G.; Proclemer, A. The 11th world survey of cardiac pacing and implantable cardioverter-defibrillators: Calendar year 2009—A World Society of Arrhythmia’s Project. Pacing Clin. Electrophysiol. 2011, 34, 1013–1027. [Google Scholar] [CrossRef]
- Somma, V.; Ha, F.J.; Palmer, S.; Mohamed, U.; Agarwal, S. Pacing-induced cardiomyopathy: A systematic review and meta-analysis of definition, prevalence, risk factors, and management. Heart Rhythm. 2023, 20, 282–290. [Google Scholar] [CrossRef]
- Merkely, B.; Hatala, R.; Wranicz, J.K.; Duray, G.; Földesi, C.; Som, Z.; Németh, M.; Goscinska-Bis, K.; Gellér, L.; Zima, E.; et al. Upgrade of right ventricular pacing to cardiac resynchronization therapy in heart failure: A randomized trial. Eur. Heart J. 2023, 44, 4259–4269. [Google Scholar] [CrossRef] [PubMed]
- Vamos, M.; Erath, J.W.; Bari, Z.; Vagany, D.; Linzbach, S.P.; Burmistrava, T.; Israel, C.W.; Duray, G.Z.; Hohnloser, S.H. Effects of Upgrade Versus De Novo Cardiac Resynchronization Therapy on Clinical Response and Long-Term Survival: Results from a Multicenter Study. Circ. Arrhythmia Electrophysiol. 2017, 10, e004471. [Google Scholar] [CrossRef]
- Duray, G.Z.; Israel, C.W.; Pajitnev, D.; Hohnloser, S.H. Upgrading to biventricular pacing/defibrillation systems in right ventricular paced congestive heart failure patients: Prospective assessment of procedural parameters and response rate. EP Europace 2008, 10, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Zizek, D.; Zlahtic, T.; Mrak, M.; Stublar, J.; Ivanovski, M.; Dzananovic, D.Z.; Cvijic, M.; Meznar, A.Z. Conduction system pacing vs. biventricular pacing for cardiac resynchronization: The CSP-SYNC randomized single centre study. EP Europace 2025, 27, euaf085.605. [Google Scholar] [CrossRef]
- Sussenbek, O.; Rademakers, L.; Waldauf, P.; Jurak, P.; Smisek, R.; Stros, P.; Poviser, L.; Vesela, J.; Plesinger, F.; Halamek, J.; et al. Left bundle branch area pacing results in more physiological ventricular activation than biventricular pacing in patients with left bundle branch block heart failure. Eur. Heart J. Suppl. 2023, 25 (Suppl. E), E17–E24. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, S.; Obeng-Gyimah, E.; Supple, G.E.; Schaller, R.; Lin, D.; Owens, A.T.; Epstein, A.E.; Dixit, S.; Marchlinski, F.E.; Frankel, D.S. Reversal of Pacing-Induced Cardiomyopathy Following Cardiac Resynchronization Therapy. JACC Clin. Electrophysiol. 2018, 4, 168–177. [Google Scholar] [CrossRef]
- Herweg, B.; Welter-Frost, A.; Vijayaraman, P. The evolution of cardiac resynchronization therapy and an introduction to conduction system pacing: A conceptual review. Europace 2021, 23, 496–510. [Google Scholar] [CrossRef]
- Meiburg, R.; Rijks, J.H.J.; Beela, A.S.; Bressi, E.; Grieco, D.; Delhaas, T.; Luermans, J.G.L.; Prinzen, F.W.; Vernooy, K.; Lumens, J. Comparison of novel ventricular pacing strategies using an electro-mechanical simulation platform. EP Europace 2023, 25, euad144. [Google Scholar] [CrossRef]
- Glikson, M.; Burri, H.; Abdin, A.; Cano, O.; Curila, K.; De Pooter, J.; Diaz, J.C.; Drossart, I.; Huang, W.; Israel, C.W.; et al. European Society of Cardiology (ESC) clinical consensus statement on indications for conduction system pacing, with special contribution of the European Heart Rhythm Association of the ESC and endorsed by the Asia Pacific Heart Rhythm Society, the Canadian Heart Rhythm Society, the Heart Rhythm Society, and the Latin American Heart Rhythm Society. EP Europace 2025, 27, euaf050. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.-P.; Chen, Y.; Yang, Y.-H.; Li, G.-C.; Ma, C.-M.; Fa, Q.; Gao, L.-J.; Xia, Y.-L.; Dong, Y.-X. Conduction system pacing upgrade versus biventricular pacing on pacemaker-induced cardiomyopathy: A retrospective observational study. Front. Physiol. 2024, 15, 1355696. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Xu, S.; Wang, C.; Li, X.; Zhu, H.; Zeng, J.; Zhang, E.; Zou, J.; Fan, X. Effectiveness of upgrading to left bundle branch area pacing compared with biventricular pacing in patients with right ventricular pacing-induced cardiomyopathy. Heart Rhythm. 2025, 22. in press. [Google Scholar] [CrossRef] [PubMed]
- Burri, H.; Jastrzebski, M.; Cano, Ó.; Čurila, K.; de Pooter, J.; Huang, W.; Israel, C.; Joza, J.; Romero, J.; Vernooy, K.; et al. EHRA clinical consensus statement on conduction system pacing implantation: Endorsed by the Asia Pacific Heart Rhythm Society (APHRS), Canadian Heart Rhythm Society (CHRS), and Latin American Heart Rhythm Society (LAHRS). EP Europace 2023, 25, 1208–1236. [Google Scholar] [CrossRef]
- Huang, W.; Chen, X.; Su, L.; Wu, S.; Xia, X.; Vijayaraman, P. A beginner’s guide to permanent left bundle branch pacing. Heart Rhythm. 2019, 16, 1791–1796. [Google Scholar] [CrossRef]
- Jastrzębski, M.; Kiełbasa, G.; Cano, O.; Curila, K.; Heckman, L.; De Pooter, J.; Chovanec, M.; Rademakers, L.; Huybrechts, W.; Grieco, D.; et al. Left bundle branch area pacing outcomes: The multicentre European MELOS study. Eur. Heart J. 2022, 43, 4161–4173. [Google Scholar] [CrossRef]
- Liu, X.; Niu, H.-X.; Gu, M.; Chen, X.; Hu, Y.; Cai, M.; Zhang, N.; Zhao, J.; Zhou, X.; Gold, M.R.; et al. Contrast-enhanced image-guided lead deployment for left bundle branch pacing. Heart Rhythm. 2021, 18, 1318–1325. [Google Scholar] [CrossRef]
- Jastrzębski, M.; Kiełbasa, G.; Moskal, P.; Bednarek, A.; Kusiak, A.; Sondej, T.; Bednarski, A.; Rajzer, M.; Vijayaraman, P. Fixation beats: A novel marker for reaching the left bundle branch area during deep septal lead implantation. Heart Rhythm. 2021, 18, 562–569. [Google Scholar] [CrossRef]
- Jastrzębski, M. ECG and Pacing Criteria for Differentiating Conduction System Pacing from Myocardial Pacing. Arrhythmia Electrophysiol. Rev. 2021, 10, 172–180. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Janssen, M.F.; Pickard, A.S.; Golicki, D.; Gudex, C.; Niewada, M.; Scalone, L.; Swinburn, P.; Busschbach, J. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: A multi-country study. Qual. Life Res. 2013, 22, 1717–1727. [Google Scholar] [CrossRef]
- Kosztin, A.; Vamos, M.; Aradi, D.; Schwertner, W.R.; Kovacs, A.; Nagy, K.V.; Zima, E.; Geller, L.; Duray, G.Z.; Kutyifa, V.; et al. De novo implantation vs. upgrade cardiac resynchronization therapy: A systematic review and meta-analysis. Heart Fail. Rev. 2018, 23, 15–26. [Google Scholar] [CrossRef]
- Merkely, B.; Hatala, R.; Merkel, E.; Szigeti, M.; Veres, B.; Fábián, A.; Osztheimer, I.; Gellér, L.; Sasov, M.; Wranicz, J.K.; et al. Benefits of upgrading right ventricular to biventricular pacing in heart failure patients with atrial fibrillation. EP Europace 2024, 26, euae179. [Google Scholar] [CrossRef]
- Vijayaraman, P.; Sharma, P.S.; Cano, Ó.; Ponnusamy, S.S.; Herweg, B.; Zanon, F.; Jastrzebski, M.; Zou, J.; Chelu, M.G.; Vernooy, K.; et al. Comparison of Left Bundle Branch Area Pacing and Biventricular Pacing in Candidates for Resynchronization Therapy. JACC 2023, 82, 228–241. [Google Scholar] [CrossRef]
- Kim, J.A.; Kim, S.E.; Ellenbogen, K.A.; Vijayaraman, P.; Chelu, M.G. Clinical outcomes of conduction system pacing versus biventricular pacing for cardiac resynchronization therapy: A systematic review and meta-analysis. J. Cardiovasc. Electrophysiol. 2023, 34, 1718–1729. [Google Scholar] [CrossRef]
- Felix, I.F.; Collini, M.; Fonseca, R.; Guida, C.; Armaganijan, L.; Healey, J.S.; Carvalho, G. Conduction system pacing versus biventricular pacing in heart failure with reduced ejection fraction: A systematic review and meta-analysis of randomized controlled trials. Heart Rhythm. 2024, 21, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Osca, J.; Francisco-Pascual, J.; Martínez-Basterra, J.; Martínez, J.G.; Reis, H.; Oliveira, M.; Campos, B.; Balaguer, J.; Rubio, J.; Pavón-Jiménez, R.; et al. Response rate in cardiac resynchronization therapy patients implanted with a left ventricular quadripolar lead and the MultiPoint™ pacing feature early activated. QUARTO III. Eur. J. Clin. Investig. 2023, 53, e13935. [Google Scholar] [CrossRef] [PubMed]
- Oka, S.; Ueda, N.; Ishibashi, K.; Noda, T.; Miyazaki, Y.; Wakamiya, A.; Shimamoto, K.; Nakajima, K.; Kamakura, T.; Wada, M.; et al. Significance of effective cardiac resynchronization therapy pacing for clinical responses: An analysis based on the effective cardiac resynchronization therapy algorithm. Heart Rhythm. 2023, 20, 1289–1296. [Google Scholar] [CrossRef]
- Shanks, M.; Delgado, V.; Ng, A.C.; Auger, D.; Mooyaart, E.A.; Bertini, M.; Marsan, N.A.; van Bommel, R.J.; Holman, E.R.; Poldermans, D.; et al. Clinical and echocardiographic predictors of nonresponse to cardiac resynchronization therapy. Am. Heart J. 2011, 161, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Kaza, N.; Htun, V.; Miyazawa, A.; Simader, F.; Porter, B.; Howard, J.P.; Arnold, A.D.; Naraen, A.; Luria, D.; Glikson, M.; et al. Upgrading right ventricular pacemakers to biventricular pacing or conduction system pacing: A systematic review and meta-analysis. EP Europace 2023, 25, 1077–1086. [Google Scholar] [CrossRef]
- Dobai, B.M.; Paiu, A.; Rudzik, R.; Sus, I.; Beke, I.; Danila, M.; Dobreanu, D. Psychosocial impact of COVID-19 pandemic on QUALITY of life among heart failure patients living with an ICD. Eur. J. Heart Fail. 2021, 23 (Suppl. S2), 2–322. [Google Scholar]
- Nicmanis, M.; Chur-Hansen, A.; Oxlad, M. The psychological, social, and quality of life outcomes of people with a cardiac implantable electronic device: An umbrella review. Eur. J. Cardiovasc. Nurs. 2024, 23, 441–451. [Google Scholar] [CrossRef]
- Willy, K.; Ellermann, C.; Reinke, F.; Rath, B.; Wolfes, J.; Eckardt, L.; Doldi, F.; Wegner, F.K.; Köbe, J.; Morina, N. The Impact of Cardiac Devices on Patients’ Quality of Life—A Systematic Review and Meta-Analysis. J. Cardiovasc. Dev. Dis. 2022, 9, 257. [Google Scholar] [CrossRef]
- Dobai, B.M.; Iantovics, L.B.; Paiu, A.; Dobreanu, D. Exploratory factor analysis for identifying CIEDs patients’ concerns during the COVID-19 pandemic in Europe. INDECS 2022, 20, 50–56. [Google Scholar] [CrossRef]
- Kutyifa, V.; Geller, L.; Bogyi, P.; Zima, E.; Aktas, M.K.; Ozcan, E.E.; Becker, D.; Nagy, V.K.; Kosztin, A.; Szilagyi, S.; et al. Effect of cardiac resynchronization therapy with implantable cardioverter defibrillator versus cardiac resynchronization therapy with pacemaker on mortality in heart failure patients: Results of a high-volume, single-centre experience. Eur. J. Heart Fail. 2014, 16, 1323–1330. [Google Scholar] [CrossRef] [PubMed]
- Køber, L.; Thune, J.J.; Nielsen, J.C.; Haarbo, J.; Videbæk, L.; Korup, E.; Jensen, G.; Hildebrandt, P.; Steffensen, F.H.; Bruun, N.E.; et al. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N. Engl. J. Med. 2016, 375, 1221–1230. [Google Scholar] [CrossRef]
- Karki, S.; Lakra, P.; Kumar, K.; Rao, S.J. Conduction System Pacing for Cardiac Resynchronization Therapy in Heart Failure with Reduced Ejection Fraction. J. Clin. Med. 2025, 14, 917. [Google Scholar] [CrossRef] [PubMed]
- Meier, C.; Israel, C.; Eisenblätter, M.; Hoyer, A.; Stoye, F.V.; Yilmaz, A.; Gielen, S. Safety of magnetic resonance imaging in patients with cardiac implantable electronic devices and abandoned or epicardial leads: A systematic review and meta-analysis. EP Europace 2024, 26, euae165. [Google Scholar] [CrossRef]
- Schaller, R.D.; Brunker, T.; Riley, M.P.; Marchlinski, F.E.; Nazarian, S.; Litt, H. Magnetic Resonance Imaging in Patients With Cardiac Implantable Electronic Devices With Abandoned Leads. JAMA Cardiol. 2021, 6, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Greenhill, M.J.; Rangan, P.; Su, W.; Weiss, J.P.; Zawaneh, M.; Unzek, S.; Tamarappoo, B.; Indik, J.; Tung, R.; Morris, M.F. MRI in Patients with Cardiovascular Implantable Electronic Devices and Fractured or Abandoned Leads. Radiol Cardiothorac Imaging 2024, 6, e230303. [Google Scholar] [CrossRef]
- Shah, K.; Pollema, T.; Birgersdotter-Green, U. Performance and outcomes of transvenous rotational lead extraction: Results from a prospective, monitored, global clinical study—“An evolution in extraction”. Heart Rhythm. O2 2021, 2, 122–123. [Google Scholar] [CrossRef] [PubMed]
| Clinical Variable | CSP (n = 26) | BIV (n = 37) | p |
|---|---|---|---|
| Age (years) | 75.9 ± 6.3 | 75 ± 7.4 | 0.77 |
| Male, n (%) | 18.0 (72) | 32 (86.5) | 0.17 |
| VP burden at baseline | 78.4 ± 30.2 | 88 ± 15.3 | 0.70 |
| Comorbidities, n (%) | |||
| Hypertension | 25 (100) | 36 (97.3) | 0.49 |
| Diabetes mellitus | 11 (44) | 25 (67.6) | 0.49 |
| Ischemic cardiomyopathy | 13 (50) | 15 (40.5) | 0.62 |
| Non-ischemic cardiomyopathy | 13 (50) | 22 (59.5) | 0.62 |
| COPD | 6 (24) | 2 (5.4) | 1.00 |
| Stroke/TIA | 4 (16) | 2 (5.4) | 1.00 |
| CKD * | 6 (24) | 2 (5.4) | 0.05 |
| Paroxysmal AF | 4 (16) | 5 (13.5) | 0.33 |
| Persistent AF | 2 (8) | 2 (5.4) | 1.00 |
| Permanent AF | 6 (24) | 12 (32.4) | 0.60 |
| NYHA class I | 4 (15.3) | 3 (8.1) | 0.43 |
| NYHA class II | 8 (30.8) | 21 (56.8) | 0.07 |
| NYHA class III | 12 (46.8) | 13 (35.1) | 0.43 |
| NYHA class IV | 2 (7.7) | 0 (0) | 0.16 |
| Primer pacing indication, n (%) | |||
| AV block | 25 (96.15) | 28 (75.67) | 0.07 |
| SSS | 3 (12) | 9 (24.3) | 0.34 |
| ECG characteristics | |||
| QRS duration (ms) | 163.3 ± 27.7 | 170.3 ± 23.9 | 0.22 |
| LBBB, n (%) | 6 (24.0) | 3 (8.1) | 0.14 |
| RBBB, n (%) | 3 (12.0) | 2 (5.4) | 0.29 |
| NIVCD, n (%) | 1 (4.0) | 1 (2.7) | 1.00 |
| Ventricular pacemaker rhythm, n (%) | 16 (64.0) | 32 (86.5) | 0.02 |
| Echocardiographic parameters | |||
| LVEF (%) | 34.5 ± 8.0 | 29.7 ± 7.6 | 0.01 |
| LVEDD (mm) | 57.0 ± 9.0 | 58.5 ± 6.8 | 0.45 |
| LAD (mm) | 57.9 ± 5.9 | 60.4 ± 7.9 | 0.16 |
| RAD (mm) | 57.3 ± 6.1 | 59.6 ± 7.0 | 0.19 |
| TAPSE (mm) | 16.5 ± 3.3 | 18.5 ± 4.3 | 0.06 |
| PSAP (mmHg) | 39.9 ± 13.7 | 45.1 ± 12.1 | 0.13 |
| Grade I of TR, n (%) | 14 (53.8) | 17 (45.9) | 0.60 |
| Grade II of TR, n (%) | 11 (42.3) | 15 (40.5) | 1.00 |
| Grade III of TR, n (%) | 1 (3.8) | 5 (13.5) | 0.38 |
| Baseline medication, n (%) | |||
| ACEI/ARB/ARNI | 24 (96.0) | 35 (94.6) | 0.50 |
| Beta blockers | 25 (100.0) | 35 (94.6) | 1.00 |
| SGLT2i | 18 (72.0) | 31 (83.8) | 0.12 |
| MRA | 10 (40.0) | 19 (51.4) | 0.39 |
| Loop diuretic | 17 (68.0) | 23 (62.2) | 0.27 |
| APT | 10 (40.0) | 11 (29.7) | 0.58 |
| Anticoagulant | 23 (92.0) | 25 (67.6) | 0.75 |
| Statins | 17 (68.0) | 29 (78.4) | 0.29 |
| Parameters | CSP (n = 26) | BIV (n = 37) | p |
|---|---|---|---|
| Procedure time (min) | 64.8 ± 7.4 | 68.4 ± 26.8 | 0.37 |
| Fluoroscopy time (min) | 7.1 ± 7.3 | 8.6 ± 5.1 | 0.03 |
| Number of leads implanted | 1.2 ± 0.4 | 1.3 ± 0.5 | 0.69 |
| More than one lead implanted, n (%) | 6 (23.1) | 10 (27) | 0.77 |
| New generator implanted, n (%) | 17 (65.38) | 37 (100) | 0.004 |
| ICD generator, n (%) | 6 (23.1) | 17 (45.9) | 0.11 |
| Baseline LV/CSP threshold (V) @ 0.5 ms | 1.2 ± 0.6 | 1.2 ± 0.8 | 1.00 |
| Baseline LV/CSP impedance (Ohm) | 626.3 ± 235.8 | 713.1 ± 303.5 | 0.54 |
| Follow-up LV/CSP threshold (V) @ 0.5 ms | 0.9 ± 0.5 | 1.2 ± 0.7 | 0.06 |
| Follow-up LV/CSP impedance (Ohm) | 521.8 ± 108.0 | 587.1 ± 185.3 | 0.40 |
| Baseline QRS (ms) | 163.3 ± 27.7 | 170.3 ± 23.9 | 0.22 |
| Follow-up QRS (ms) | 132.3 ± 14.2 | 139.2 ± 17.7 | 0.14 |
| Baseline NYHA class | 2.5 ± 0.9 | 2.3 ± 0.6 | 0.61 |
| Follow-up NYHA class | 2.0 ± 0.5 | 2.1 ± 0.9 | 0.89 |
| Baseline LVEDD (mm) | 57.0 ± 9.0 | 58.5 ± 6.8 | 0.45 |
| Follow-up LVEDD (mm) | 53.2 ± 8.6 | 54.8 ± 7.8 | 0.49 |
| Baseline LVEF (%) | 34.5 ± 8.0 | 29.7 ± 7.6 | 0.01 |
| Follow-up LVEF (%) | 40.1 ± 8.9 | 39.3 ± 13.2 | 0.45 |
| Parameters | CSP (n = 26) |
|---|---|
| V6RWPeak time (ms) | 82.5 ± 15.9 |
| Presence of R’ in V1 (v1R’) | 23 (88.5%) |
| His bundle pacing | 2 (7.7%) |
| Left anterior fascicular pacing | 2 (7.7%) |
| Left septal fascicular pacing | 9 (34.6%) |
| Left posterior fascicular pacing | 5 (19.2%) |
| Left ventricular septal pacing | 7 (26.9%) |
| Outcome | HR (CSP vs. BIV) | 95% CI | p-Value |
|---|---|---|---|
| All-Cause Mortality | 1.74 | 0.35–8.73 | 0.50 |
| HF Hospitalization | 0.42 | 0.05–3.82 | 0.44 |
| HF Hospitalization (Adjusted for baseline LVEF) | 0.66 | 0.07–6.43 | 0.72 |
| Composite (ACM + HFH) | 0.87 | 0.22–3.51 | 0.85 |
| Quality of Life | CSP | BIV | p |
|---|---|---|---|
| Self-reported Health on a scale 0–100 | 46.5 ± 34.9 | 41.6 ± 31.9 | 0.46 |
| Any level of issue with mobility, n (%) | 11 (42.3) | 20 (54.1) | 1.00 |
| Any level of issue with self care, n (%) | 3 (11.5) | 8 (21.6) | 1.00 |
| Any level of issue with usual activities, n (%) | 6 (23.1) | 8(21.6) | 0.95 |
| Any level of pain/discomfort, n (%) | 5 (19.2) | 15 (40.5) | 0.85 |
| Any level of anxiety or depression, n (%) | 3 (11.5) | 8.0 (21.6) | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dobai, B.M.; Polgár, B.; Gémesi, M.; Bogdan, M.; Vigh, N.; Turáni, M.; Duray, G.Z.; Bógyi, P. Comparing Conduction System Pacing to Biventricular Upgrade in Pacemaker-Induced Cardiomyopathy: A Retrospective Observational Study. J. Clin. Med. 2025, 14, 7745. https://doi.org/10.3390/jcm14217745
Dobai BM, Polgár B, Gémesi M, Bogdan M, Vigh N, Turáni M, Duray GZ, Bógyi P. Comparing Conduction System Pacing to Biventricular Upgrade in Pacemaker-Induced Cardiomyopathy: A Retrospective Observational Study. Journal of Clinical Medicine. 2025; 14(21):7745. https://doi.org/10.3390/jcm14217745
Chicago/Turabian StyleDobai, Bernadett Miriam, Balázs Polgár, Márk Gémesi, Manuella Bogdan, Nikolett Vigh, Mirjam Turáni, Gábor Zoltán Duray, and Péter Bógyi. 2025. "Comparing Conduction System Pacing to Biventricular Upgrade in Pacemaker-Induced Cardiomyopathy: A Retrospective Observational Study" Journal of Clinical Medicine 14, no. 21: 7745. https://doi.org/10.3390/jcm14217745
APA StyleDobai, B. M., Polgár, B., Gémesi, M., Bogdan, M., Vigh, N., Turáni, M., Duray, G. Z., & Bógyi, P. (2025). Comparing Conduction System Pacing to Biventricular Upgrade in Pacemaker-Induced Cardiomyopathy: A Retrospective Observational Study. Journal of Clinical Medicine, 14(21), 7745. https://doi.org/10.3390/jcm14217745






