A Retrospective, Digital Evaluation of Tip and Torque of Teeth in Patients with Skeletal Class I, II and III Using Lateral Cephalograms, Orthopantomograms and Digitized Models
Abstract
1. Introduction
2. Materials and Methods
2.1. Cephalometric Measurements
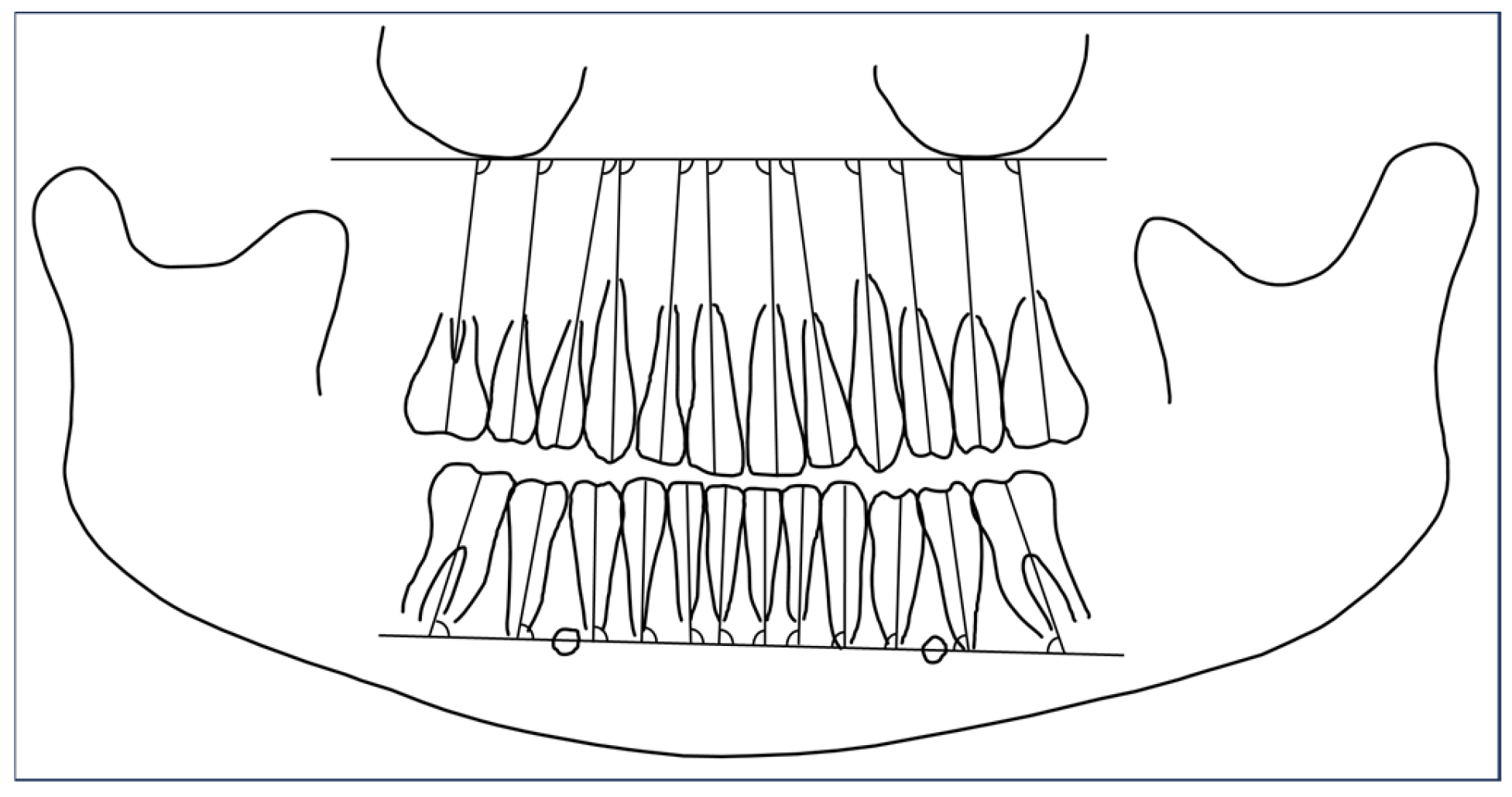
2.2. Investigation of Tip of Teeth Using Orthopantomograms
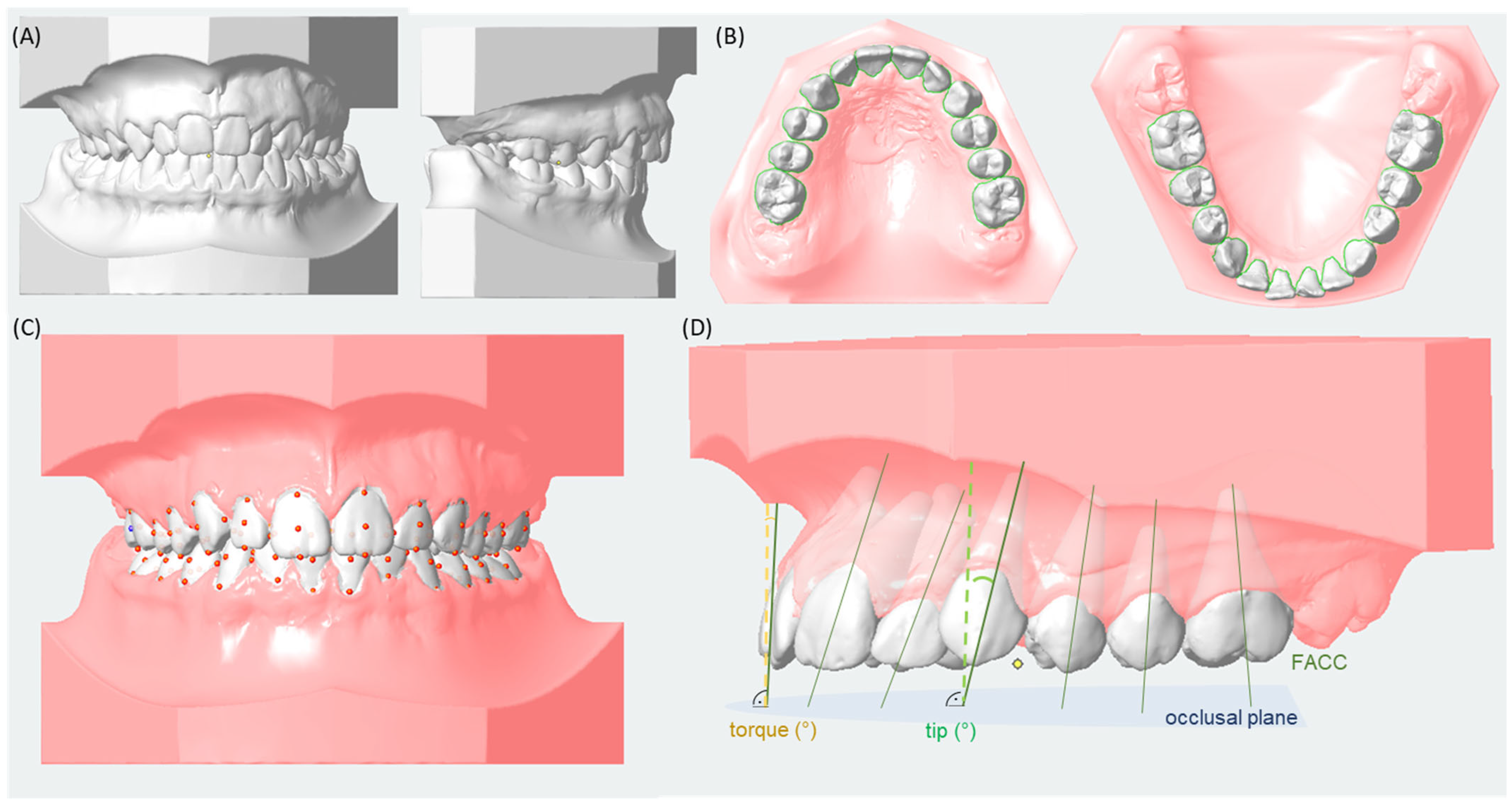
2.3. Three-Dimensional Tip and Torque Measurements Using Digital Analysis of Digitized Models
2.4. Statistics
3. Results
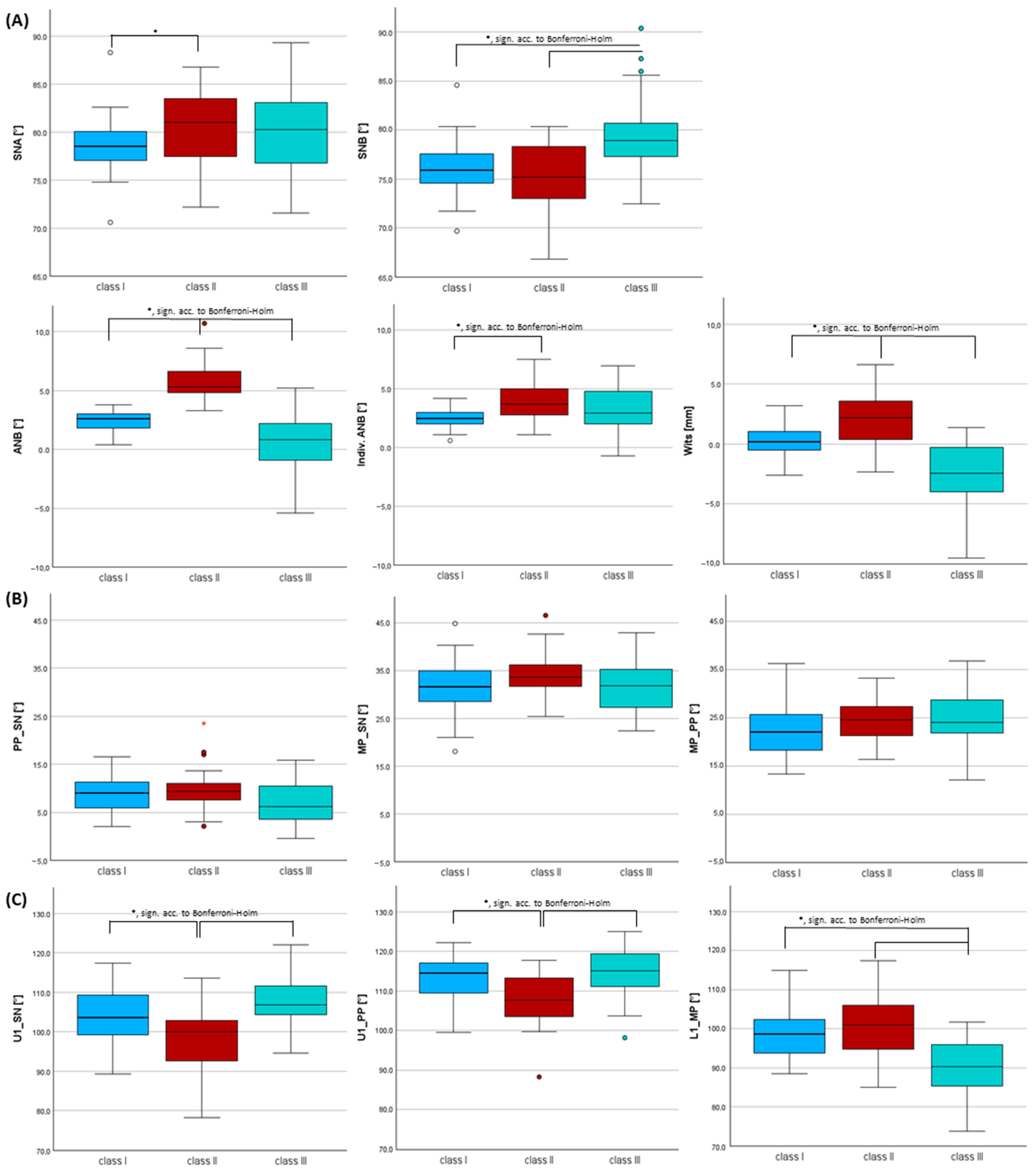
3.1. Characteristics of Skeletal Class I, II and III
3.2. Inclination of Incisors Using Cephalometric Measurements Within Each Skeletal Class
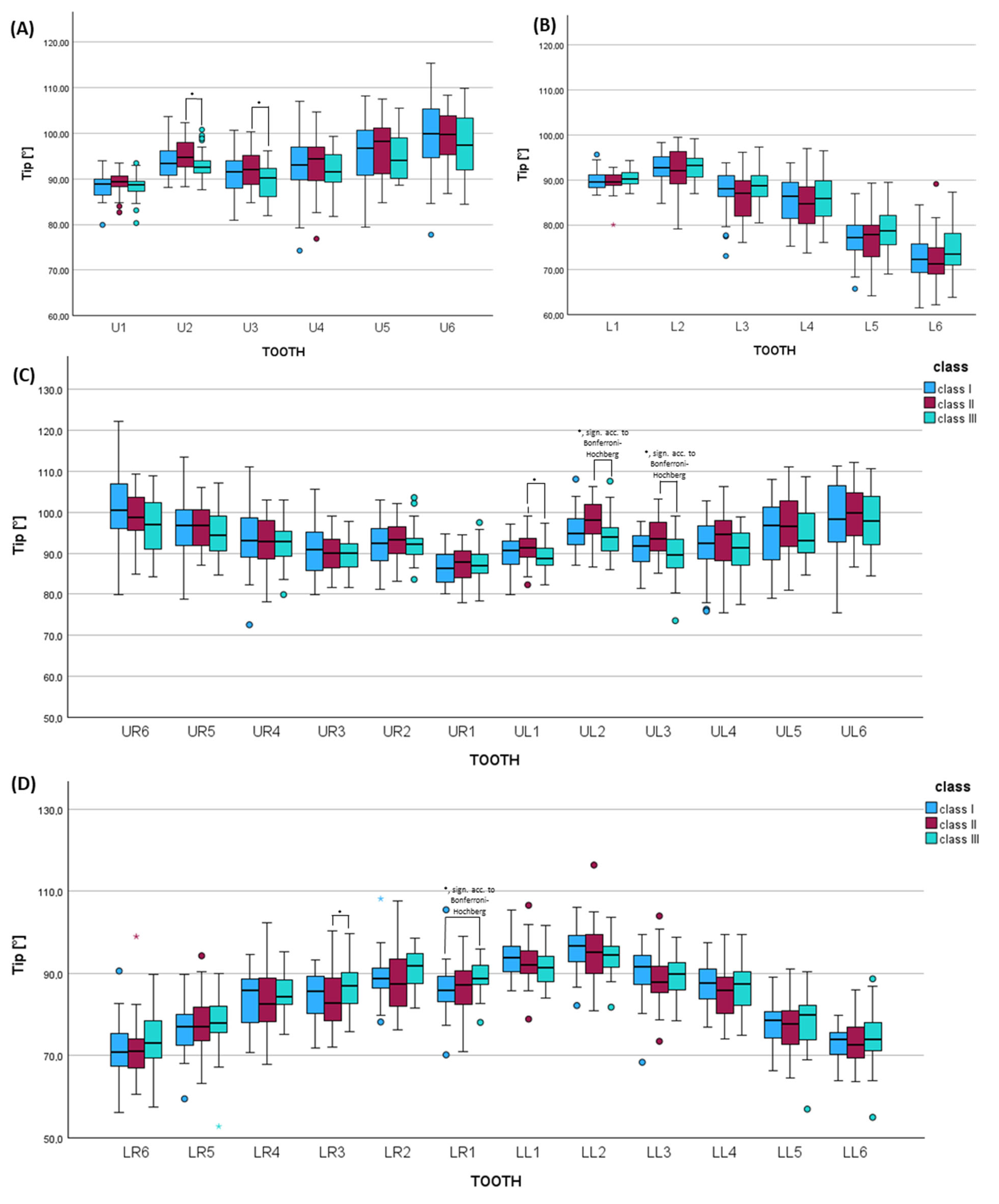
3.3. Orthopantomogram Analysis Considering Tip of the Long Axis of Teeth in Each Skeletal Class
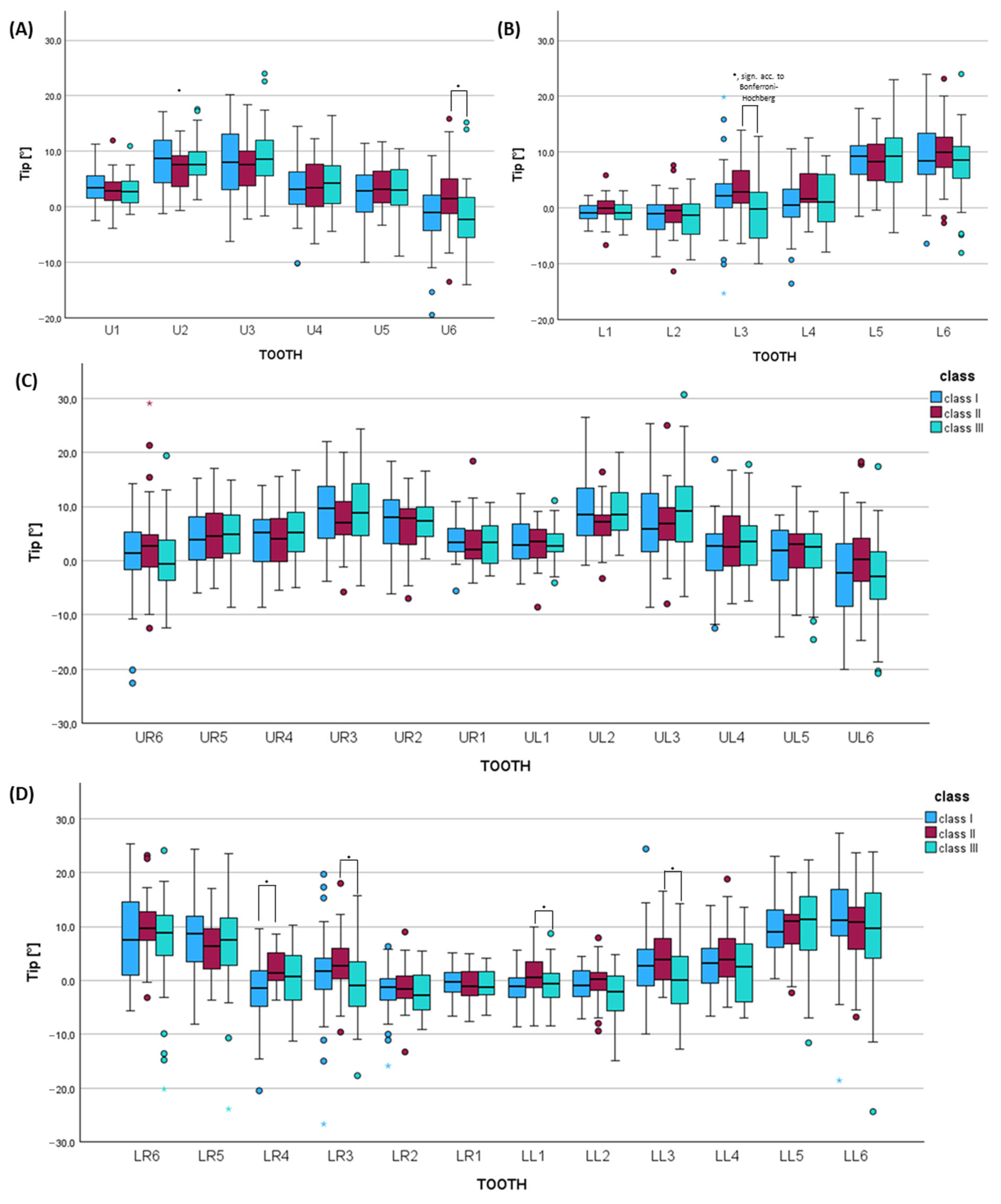
3.4. Digital Dental Cast Analysis Considering Tip of the Clinical Crown for Each Skeletal Class
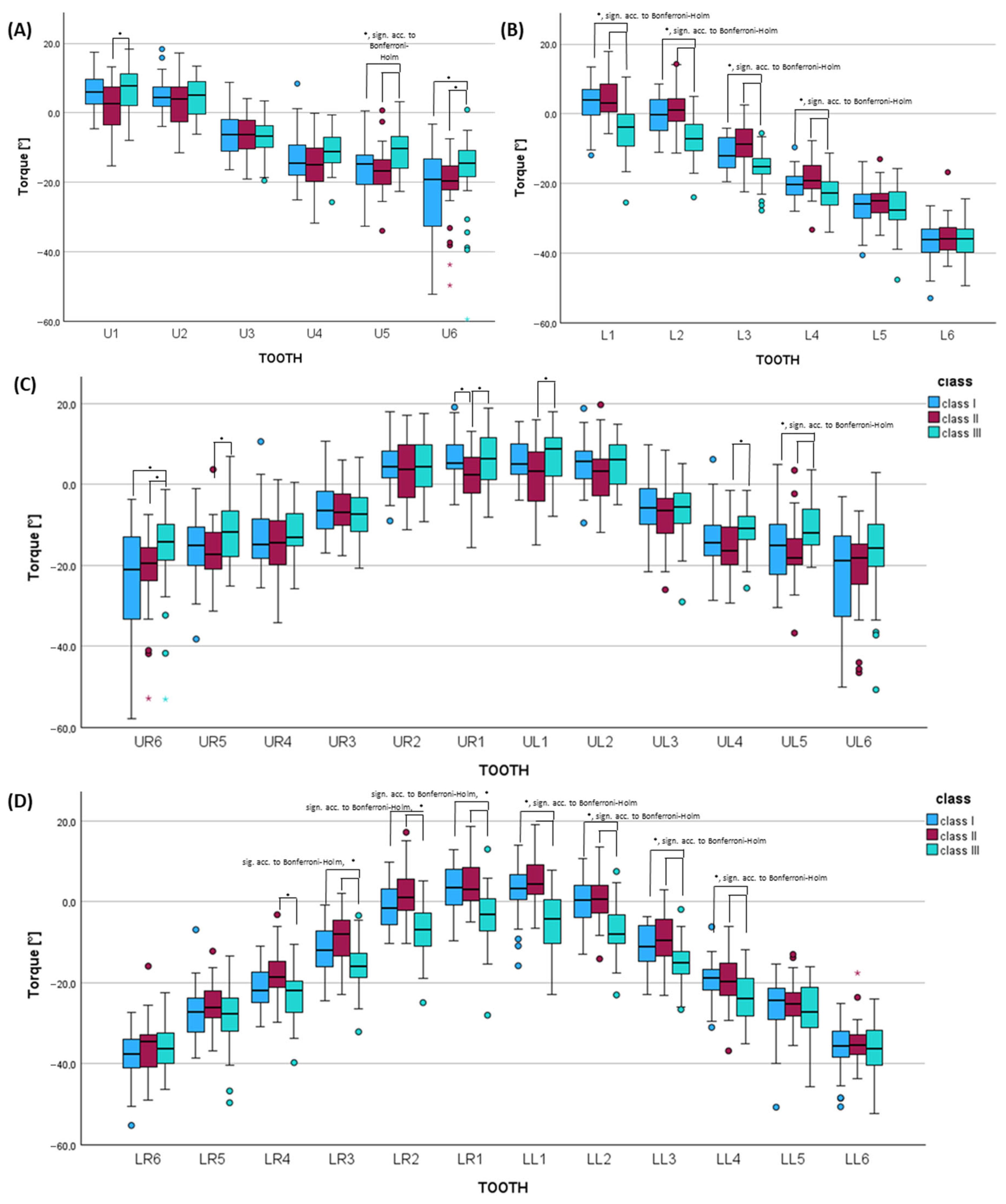
3.5. Digital Dental Cast Analysis Considering Torque of the Clinical Crown for Each Skeletal Class
4. Discussion
- (1)
- More retroinclined upper central incisors by ~7–9° vs. class III and by~−5–6° vs. class I (A);
- (2)
- More proclined lower incisors by ~11° compared to class III (A), which was also seen for the central and lateral incisors by 8–9° vs. class III (C);
- (3)
- Greater mesial tipping of lower canines by 3.5° vs. class III (C);
- (4)
- Greater palatal tipping of the upper second premolars by ~−6° vs. class III (C);
- (1)
- Greater proclination of upper central incisors by ~8° vs. class II (A);
- (2)
- More retroinclined incisors by ~−11° vs. class II and −8–9° vs. class I (A), which was also seen for the central and lateral incisors by −8–9° vs. class III and −6–7° vs. class I (C);
- (3)
- Greater distal tipping of lower canines by 3.5° vs. class II (C);
- (4)
- Greater buccal tipping of the upper second premolar by ~6° vs. class II (C);
- (5)
- Higher lingual tipping of canines and the first premolar in the lower jaw by −6.4° and −4.0° vs. class II (C).
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Joshi, N.; Hamdan, A.M.; Fakhouri, W.D. Skeletal malocclusion: A developmental disorder with a life-long morbidity. J. Clin. Med. Res. 2014, 6, 399–408. [Google Scholar] [CrossRef]
- Slavicek, R. Das Kauorgan: Funktionen und Dysfunktionen; Gamma, Med.-Wiss.-Fortbildungs-Ges: Klosterneuburg, Austria, 2000. [Google Scholar]
- Liu, L.; Liu, Y.; Han, L.; Zhang, C.; Hou, P. Comparison of Different Decompensation Approaches on Facial Profile in Orthodontic–Orthognathic Treatment for Skeletal Class III Patients. Aesthetic Plast. Surg. 2023, 47, 1957–1966. [Google Scholar] [CrossRef]
- Wilmes, B.; Olthoff, G.; Drescher, D. Comparison of skeletal and conventional anchorage methods in conjunction with pre-operative decompensation of a skeletal class III malocclusion. J. Orofac. Orthop. 2009, 70, 297–305. [Google Scholar] [CrossRef]
- Lin, J.; Gu, Y. Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition. Angle Orthod. 2003, 73, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Sander, F.G.; Wichelhaus, A. Skelettale und dentale Veränderungen bei der Anwendung der Vorschubdoppelplatte. Fortschr. Kieferorthop. 1995, 56, 127–139. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.; Yiu, C.; Hu, A.; Hagg, U.; Wei, S.H.; Gunel, E. Cephalometric and occlusal changes following maxillary expansion and protraction. Eur. J. Orthod. 1998, 20, 237–254. [Google Scholar] [CrossRef] [PubMed]
- Andrews, L.F. The six keys to normal occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef]
- Lombardo, L.; Perri, A.; Arreghini, A.; Latini, M.; Siciliani, G. Three-dimensional assessment of teeth first-, second- and third-order position in Caucasian and African subjects with ideal occlusion. Prog. Orthod. 2015, 16, 11. [Google Scholar] [CrossRef]
- Kannabiran, P.; Thirukonda, G.J.; Mahendra, L. The crown angulations and inclinations in Dravidian population with normal occlusion. Indian J. Dent. Res. 2012, 23, 53–58. [Google Scholar] [CrossRef]
- Tong, H.; Kwon, D.; Shi, J.; Sakai, N.; Enciso, R.; Sameshima, G.T. Mesiodistal angulation and faciolingual inclination of each whole tooth in 3-dimensional space in patients with near-normal occlusion. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 604–617. [Google Scholar] [CrossRef]
- Wang, H.; Zhao, N.; Li, P.; Shen, G. A cone-beam computed tomography analysis of angulation and inclination of whole tooth and clinical crown in adults with normal occlusion. Orthod. Craniofac. Res. 2019, 22, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Sayago, E.; Espinar-Escalona, E.; Barrera-Mora, J.M.; Ruiz-Navarro, M.B.; Llamas-Carreras, J.M.; Solano-Reina, E. Lower incisor position in different malocclusions and facial patterns. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e343–e350. [Google Scholar] [CrossRef] [PubMed]
- Santana, L.; Motro, M.; Bamashmous, M.S.; Kantarci, A.; Will, L.A. Buccolingual angulation and intermolar width changes in the maxillary first molars of untreated growing children. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Huang, J.; Tang, X.; Zheng, L.; Yang, C. Anterior alveolar bone and tooth inclination in different skeletal patterns: A cone-beam computed tomography study. BMC Oral Health 2025, 25, 1210. [Google Scholar] [CrossRef]
- Dellinger, E.L. A scientific assessment of the straight-wire appliance. Am. J. Orthod. 1978, 73, 290–299. [Google Scholar] [CrossRef]
- Watanabe, K.; Koga, M. A morphometric study with setup models for bracket design. Angle Orthod. 2001, 71, 499–511. [Google Scholar] [CrossRef]
- Jotikasthira, D.; Sheffield, P.; Kalha, A.; Syed, Z. Crown angulation and inclination of Northern Thais with good occlusion. World J. Orthod. 2010, 11, 71–74. [Google Scholar]
- Duangtaweeesub, S.; Jotikasthira, D. Crown inclination and crown angulation of northern Thais with good occlusion. CM Dent. J. 2003, 24, 61–67. [Google Scholar]
- Proffit, W.R.; Fields, H.; Larson, B.; Sarver, D.M. Contemporary Orthodontics—E-Book; Mosby: St. Louis, MO, USA, 2018. [Google Scholar]
- Segner, D.; Hasund, A. Individualisierte Kephalometrie; Segner: Hamburg, Germany, 1998. [Google Scholar]
- Downs, W.B. Variations in facial relationships: Their significance in treatment and prognosis. Am. J. Orthod. 1948, 34, 812–840. [Google Scholar] [CrossRef]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Ishikawa, H.; Nakamura, S.; Iwasaki, H.; Kitazawa, S. Seven parameters describing anteroposterior jaw relationships: Postpubertal prediction accuracy and interchangeability. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 714–720. [Google Scholar] [CrossRef]
- Riedel, R.A. The relation of maxillary structures to cranium in malocclusion and in normal occlusion. Angle Orthod. 1952, 22, 142–145. [Google Scholar] [CrossRef]
- Panagiotidis, G.; Witt, E. Der individualisierte ANB-Winkel. Fortschr. Kieferorthop. 1977, 38, 408–416. [Google Scholar] [CrossRef]
- Jacobson, A. The “Wits” appraisal of jaw disharmony. Am. J. Orthod. 1975, 67, 125–138. [Google Scholar] [CrossRef]
- Ursi, W.J.; Almeida, R.R.; Tavano, O.; Henriques, J.F. Assessment of mesiodistal axial inclination through panoramic radiography. J. Clin. Orthod. 1990, 24, 166–173. [Google Scholar]
- Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Hochberg, Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988, 75, 800–802. [Google Scholar] [CrossRef]
- Menyhart, O.; Weltz, B.; Győrffy, B. MultipleTesting.com: A tool for life science researchers for multiple hypothesis testing correction. PLoS ONE 2021, 16, e0245824. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Academic Press: New York, NY, USA, 1969. [Google Scholar]
- Perini, T.A.; Oliveira, G.L.d.; Ornellas, J.d.S.; Oliveira, F.P.d. Technical error of measurement in anthropometry. Rev. Bras. Med. Esporte 2005, 11, 86–90. [Google Scholar] [CrossRef]
- Busato, M.C.; Mendonca, M.R.; Pereira, A.L.; Tondelli, P.M.; Cuoghi, O.A. Compensatory canine angulation in angle Class II and III patients. Braz. Oral Res. 2009, 23, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Han, B.; Li, S.; Na, B.; Ma, W.; Xu, T.M. Compensation trends of the angulation of first molars: Retrospective study of 1403 malocclusion cases. Int. J. Oral Sci. 2014, 6, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Ardani, I.; Wicaksono, A.; Hamid, T. The Occlusal Plane Inclination Analysis for Determining Skeletal Class III Malocclusion Diagnosis. Clin. Cosmet. Investig. Dent. 2020, 12, 163–171. [Google Scholar] [CrossRef]
- Bouwens, D.G.; Cevidanes, L.; Ludlow, J.B.; Phillips, C. Comparison of mesiodistal root angulation with posttreatment panoramic radiographs and cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 126–132. [Google Scholar] [CrossRef]
- Seidel, C.L.; Baumert, U.; Ost, F.; Sabbagh, H.; Wichelhaus, A. Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets. J. Clin. Med. 2025, 14, 3370. [Google Scholar] [CrossRef]
- Talari, K.; Goyal, M. Retrospective studies—Utility and caveats. J. R. Coll. Physicians Edinb. 2020, 50, 398–402. [Google Scholar] [CrossRef]
- Čelar, A.; Lettner, S.; Jonke, E. Anterior and Posterior Occlusal Plane Inclinations Differ Between Class II and Class III Mixed Dentitions-A Retrospective Cross-Sectional Study of a Morphological Characteristic. J. Clin. Med. 2025, 14, 6553. [Google Scholar] [CrossRef]
- Houston, W.J. The analysis of errors in orthodontic measurements. Am. J. Orthod. 1983, 83, 382–390. [Google Scholar] [CrossRef]
- Kamoen, A.; Dermaut, L.; Verbeeck, R. The clinical significance of error measurement in the interpretation of treatment results. Eur. J. Orthod. 2001, 23, 569–578. [Google Scholar] [CrossRef]
- Cooke, M.S.; Wei, S.H. Cephalometric errors: A comparison between repeat measurements and retaken radiographs. Aust. Dent. J. 1991, 36, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Ongkosuwito, E.M.; Katsaros, C.; van’t Hof, M.A.; Bodegom, J.C.; Kuijpers-Jagtman, A.M. The reproducibility of cephalometric measurements: A comparison of analogue and digital methods. Eur. J. Orthod. 2002, 24, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Batista, K.B.; Thiruvenkatachari, B.; Harrison, J.E.; O’Brien, K.D. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents. Cochrane Database Syst. Rev. 2018, 3, Cd003452. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, S.M.; Banks, P.; Wright, J.L. The use of myofunctional appliances in the UK: A survey of British orthodontists. Dent. Update 1998, 25, 302–308. [Google Scholar]
- Ong, Q.; Anwar, H.; El-Angbawi, A. Contemporary Twin Block appliance wear protocols: A survey of UK orthodontists. J. Orthod. 2024, 51, 70–78. [Google Scholar] [CrossRef]
- Uysal, T.; Baysal, A.; Yagci, A. Evaluation of speed, repeatability, and reproducibility of digital radiography with manual versus computer-assisted cephalometric analyses. Eur. J. Orthod. 2009, 31, 523–528. [Google Scholar] [CrossRef]
- Albarakati, S.F.; Kula, K.S.; Ghoneima, A.A. The reliability and reproducibility of cephalometric measurements: A comparison of conventional and digital methods. Dentomaxillofac. Radiol. 2012, 41, 11–17. [Google Scholar] [CrossRef]
- Goracci, C.; Ferrari, M. Reproducibility of measurements in tablet-assisted, PC-aided, and manual cephalometric analysis. Angle Orthod. 2014, 84, 437–442. [Google Scholar] [CrossRef]
- Gul Amuk, N.; Karsli, E.; Kurt, G. Comparison of dental measurements between conventional plaster models, digital models obtained by impression scanning and plaster model scanning. Int. Orthod. 2019, 17, 151–158. [Google Scholar] [CrossRef]
- Vogel, A.B.; Kilic, F.; Schmidt, F.; Rubel, S.; Lapatki, B.G. Dimensional accuracy of jaw scans performed on alginate impressions or stone models: A practice-oriented study. J. Orofac. Orthop. 2015, 76, 351–365. [Google Scholar] [CrossRef]
- Andrews, L.F. Straight Wire—The Concept and Appliance; LA Wells Co.: San Diego, CA, USA, 1989. [Google Scholar]
- Knösel, M.; Attin, R.; Kubein-Meesenburg, D.; Sadat-Khonsari, R. Cephalometric assessment of the axial inclination of upper and lower incisors in relation to the third-order angle. J. Orofac. Orthop. 2007, 68, 199–209. [Google Scholar] [CrossRef]
- Vardimon, A.D.; Lambertz, W. Statistical evaluation of torque angles in reference to straight-wire appliance (SWA) theories. Am. J. Orthod. 1986, 89, 56–66. [Google Scholar] [CrossRef]
- Jiménez Caro, M.d.C.; Villafranca, C.; Álvarez Suárez, A.; Vega Álvarez, J.A.; Cobo Plana, J.M. Are the orthodontic basis wrong? Revisiting two of the keys to normal oclusion (Crown Inclination and Crown Angulation) in the Andrews Series. In Orthodontics—Basic Aspects and Clinical Considerations; Bourzgui, F., Ed.; InTech: Rijeka, Croatia, 2012; pp. 53–68. [Google Scholar]
- Coşkun, İ.; Kaya, B. Appraisal of the relationship between tooth inclination, dehiscence, fenestration, and sagittal skeletal pattern with cone beam computed tomography. Angle Orthod. 2019, 89, 544–551. [Google Scholar] [CrossRef]
- Sangcharearn, Y.; Ho, C. Maxillary incisor angulation and its effect on molar relationships. Angle Orthod. 2007, 77, 221–225. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seidel, C.L.; Kelemenova, K.; Baumert, U.; Wichelhaus, A.; Sabbagh, H. A Retrospective, Digital Evaluation of Tip and Torque of Teeth in Patients with Skeletal Class I, II and III Using Lateral Cephalograms, Orthopantomograms and Digitized Models. J. Clin. Med. 2025, 14, 7738. https://doi.org/10.3390/jcm14217738
Seidel CL, Kelemenova K, Baumert U, Wichelhaus A, Sabbagh H. A Retrospective, Digital Evaluation of Tip and Torque of Teeth in Patients with Skeletal Class I, II and III Using Lateral Cephalograms, Orthopantomograms and Digitized Models. Journal of Clinical Medicine. 2025; 14(21):7738. https://doi.org/10.3390/jcm14217738
Chicago/Turabian StyleSeidel, Corinna L., Karolina Kelemenova, Uwe Baumert, Andrea Wichelhaus, and Hisham Sabbagh. 2025. "A Retrospective, Digital Evaluation of Tip and Torque of Teeth in Patients with Skeletal Class I, II and III Using Lateral Cephalograms, Orthopantomograms and Digitized Models" Journal of Clinical Medicine 14, no. 21: 7738. https://doi.org/10.3390/jcm14217738
APA StyleSeidel, C. L., Kelemenova, K., Baumert, U., Wichelhaus, A., & Sabbagh, H. (2025). A Retrospective, Digital Evaluation of Tip and Torque of Teeth in Patients with Skeletal Class I, II and III Using Lateral Cephalograms, Orthopantomograms and Digitized Models. Journal of Clinical Medicine, 14(21), 7738. https://doi.org/10.3390/jcm14217738







