Wealth, Unemployment, Social Investment, and Risk of ST-Segment Elevation Myocardial Infarction—An Ecological Analysis of a Low-Cardiovascular-Risk European Region
Abstract
1. Introduction
2. Patients and Methods
2.1. Population and Study Design
2.2. Sample Analyzed
2.3. Data Sources
- -
- Sociodemographic variables: population, mean age, rate of ageing, female-to-male ratio, average income, gross domestic product per capita, unemployment rate, percentage of people employed in financial services, number of foreign immigrants per 1000 inhabitants.
- -
- - Social investment: public hospitals in the population, non-university students per teacher/school unit, health centers per 10,000 inhabitants, public libraries per 10,000 inhabitants.
2.4. Statistical Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CM | Community of Madrid |
| CIM | Código Infarto Madrid |
| GDP | Gross domestic product per capita |
| IHD | Ischemic heart disease |
| iSTEMI | Average incidence rate of STEMI |
| STEMI | ST-segment elevation myocardial infarction |
References
- GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: A systematic analysis for the global burden of disease study 2021. Lancet 2024, 403, 2133–2161. [Google Scholar] [CrossRef]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Karamzad, N.; Singh, K.; Carson-Chahhoud, K.; Adams, C.; Nejadghaderi, S.A.; Almasi-Hashiani, A.; Sullman, M.J.M.; Mansournia, M.A.; Bragazzi, N.L.; et al. Burden of ischemic heart disease and its attributable risk factors in 204 countries and territories, 1990–2019. Eur. J. Prev. Cardiol. 2022, 29, 420–431. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef]
- Khaing, W.; Vallibhakara, S.A.; Attia, J.; McEvoy, M.; Thakkinstian, A. Effects of education and income on cardiovascular outcomes: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 1032–1042. [Google Scholar] [CrossRef]
- García-Lledó, A.; Rodríguez-Martín, S.; Tobías, A.; García-de-Santiago, E.; Ordobás-Gavín, M.; Ansede-Cascudo, J.C.; Alonso-Martín, J.; de Abajo, F.J. Relationship Between Influenza, Temperature, and Type 1 Myocardial Infarction: An Ecological Time-Series Study. J. Am. Heart Assoc. 2021, 10, e019608. [Google Scholar] [CrossRef]
- McManus, D.D.; Gore, J.; Yarzebski, J.; Spencer, F.; Lessard, D.; Goldberg, R.J. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am. J. Med. 2011, 124, 40–47. [Google Scholar] [CrossRef]
- Krittanawong, C.; Maitra, N.S.; Qadeer, Y.K.; Wang, Z.; Fogg, S.; Storch, E.A.; Celano, C.M.; Huffman, J.C.; Jha, M.; Charney, D.S.; et al. Association of Depression and Cardiovascular Disease. Am. J. Med. 2023, 136, 881–895. [Google Scholar] [CrossRef]
- Saxena, M.; Bloos, S.M.; Graber-Naidich, A.; Sundaram, V.; Pasao, M.; Yiadom, M.Y.A.B. Variation in ACS patient hospital resource utilization: Is it time for advanced NSTEMI risk stratification in the ED? Am. J. Emerg. Med. 2023, 70, 171–174. [Google Scholar] [CrossRef]
- Ma, H.; Wu, S.; Cao, J.; Cai, T. Reassess Hospital Costs and Mortality Between Myocardial Infarction with and Without ST-Segment Elevation in a Modern Context. Ann. Noninvasive Electrocardiol. 2024, 29, e70027. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Consejería de Hacienda, Economía y Empleo. PIB Regional de la UE. Comunidad de Madrid, Madrid, España, 2022. Available online: https://www.comunidad.madrid/sites/default/files/doc/economia/pib_regional_2022_ue27.pdf (accessed on 20 July 2025).
- Memoria del Servicio Madrileño de Salud. 2018. Available online: https://gestiona3.madrid.org/bvirtual/BVCM020283.pdf (accessed on 20 July 2025).
- Instituto Nacional de Estadística. Tasa de Mortalidad Atribuida a las Enfermedades Cardiovasculares, el Cáncer, la Diabetes o las Enfermedades Respiratorias Crónicas por Comunidad Autónoma, Edad, Sexo y Periodo. Available online: https://www.ine.es/jaxi/Tabla.htm?tpx=46687 (accessed on 20 July 2025).
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF). Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction. Circulation 2018, 138, e618–e651, Erratum in Circulation 2018, 138, e652. https://doi.org/10.1161/CIR.0000000000000632. [Google Scholar] [CrossRef]
- Fichas Estadísticas Municipales. Comunidad de Madrid. Madrid, España. Available online: https://gestiona.comunidad.madrid/desvan/almudena/fichasmunicipales.html (accessed on 20 July 2025).
- Duque, I.; Domínguez-Berjón, M.F.; Cebrecos, A.; Prieto-Salceda, M.D.; Esnaola, S.; Calvo Sánchez, M.; Marí-Dell’Olmo, M. Índice de privación en España por sección censal en 2011 [Deprivation index by enumeration district in Spain, 2011]. Gac Sanit. 2021, 35, 113–122. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Dirección General de Salud Pública. IIIrd Atlas of Mortality and Socio-Economic Inequalities in the Madrid Region. Community of Madrid, Madris, Spain, October 2021. Available online: https://www.comunidad.madrid/publicacion/ref/50460 (accessed on 15 October 2025).
- Li, Y.; Cao, G.-Y.; Jing, W.-Z.; Liu, J.; Liu, M. Global trends and regional differences in incidence and mortality of cardiovascular disease, 1990−2019: Findings from 2019 global burden of disease study. Eur. J. Prev. Cardiol. 2022, 30, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Landon, B.E.; Hatfield, L.A.; Bakx, P.; Banerjee, A.; Chen, Y.-C.; Fu, C.; Gordon, M.; Heine, R.; Huang, N.; Ko, D.T.; et al. Differences in Treatment Patterns and Outcomes of Acute Myocardial Infarction for Low- and High-Income Patients in 6 Countries. JAMA 2023, 329, 1088–1097. [Google Scholar] [CrossRef]
- Snowdon, J.L.; Scheufele, E.L.; Pritts, J.; Le, P.-T.; Mensah, G.A.; Zhang, X.; Dankwa-Mullan, I. Evaluating Social Determinants of Health Variables in Advanced Analytic and Artificial Intelligence Models for Cardiovascular Disease Risk and Outcomes: A Targeted Review. Ethn. Dis. 2023, 33, 33–43. [Google Scholar] [CrossRef]
- Ruano-Ravina, A.; Pena-Gil, C.; Abu-Assi, E.; Raposeiras, S.; van’t Hof, A.; Meindersma, E.; Bossano Prescott, E.I.; González-Juanatey, J.R. Participation and adherence to cardiac rehabilitation programs. A systematic review. Int. J. Cardiol. 2016, 223, 436–443. [Google Scholar] [CrossRef]
- de Mestral, C.; Stringhini, S. Socioeconomic Status and Cardiovascular Disease: An Update. Curr. Cardiol. Rep. 2017, 19, 115. [Google Scholar] [CrossRef]
- Rahimi, A.R.; Spertus, J.A.; Reid, K.J.; Bernheim, S.M.; Krumholz, H.M. Financial Barriers to Health Care and Outcomes After Acute Myocardial Infarction. JAMA 2007, 297, 1063–1072. [Google Scholar] [CrossRef][Green Version]
- Castiello, D.S.; Oliva, A.; Andò, G.; Niccoli, G.; Pelliccia, F.; Moscarella, E.; Montone, R.A.; Gragnano, F.; Porto, I.; Calabrò, P.; et al. Antithrombotic therapy in complex percutaneous coronary intervention. EuroIntervention 2025, 21, e1051–e1068. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.J.T.; Mitchell, C.; Hemmelgarn, B.R.; Tonelli, M.; Faris, P.; Zhang, J.; Tsuyuki, R.T.; Fletcher, J.; Au, F.; Klarenbach, S.; et al. Eliminating Medication Copayments for Low-Income Older Adults at High Cardiovascular Risk: A Randomized Controlled Trial. Circulation 2023, 147, 1505–1514. [Google Scholar] [CrossRef]
- Magnani, J.W.; Ning, H.; Wilkins, J.T.; Lloyd-Jones, D.M.; Allen, N.B. Educational Attainment and Lifetime Risk of Cardiovascular Disease. JAMA Cardiol. 2024, 9, 45–54. [Google Scholar] [CrossRef] [PubMed]
- You, Y.; Chen, J.; Wang, K.; Wu, T.; Bai, L.; Li, G.; Wu, S. Impact of Short-Term Exposure to Ozone on Hospital Admissions for Multiple Cardiovascular Diseases: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2025, 14, e037205. [Google Scholar] [CrossRef] [PubMed]
- Campuzano, R.; Núñez, J.; Sánchez, V.; Gómez-Doblas, J.J.; Arrarte, V.; Cequier, Á.; Miranda, B.; Fernández, C.; Prado, N.; Rosillo, N.; et al. Impact of fine particulate matter (PM2.5) pollution on hospital admissions and mortality due to acute myocardial infarction in Spain. Rev. Esp. Cardiol. (Engl. Ed.) 2025. ahead of print. [Google Scholar] [CrossRef]
- Farley, K.L.; Owen, D.; Fitch, A.; Fletcher, D.; Scheffler, J.; Jones, L. A tale of two cities: Contrasting equity of greenspace benefits in relation to PM2.5 exposure. BMC Public Health 2025, 25, 3449. [Google Scholar] [CrossRef]
- Schwartz, S. The fallacy of the ecological fallacy: The potential misuse of a concept and the consequences. Am. J. Public Health 1994, 84, 819–824. [Google Scholar] [CrossRef] [PubMed]
| Mean | Minimum | Maximum | Standard Deviation | |
|---|---|---|---|---|
| Sociodemographic data | ||||
| Mean age | 39.1 | 35.2 | 42.5 | 2.01 |
| Rate of inhabitants older than 65 | 13.6 | 6.2 | 20.9 | 3.51 |
| Rate of female population (%) | 37.2% | 33.8% | 41.2% | 1.74 |
| Public investment parameters | ||||
| Rate of teachers per non-university alumni | 13.11 | 11.57 | 14.39 | 0.74 |
| Public health centers (per 10,000 inhabitants) | 1.13 | 0 | 4.94 | 1.16 |
| Median | Minimum | Maximum | Rank | |
|---|---|---|---|---|
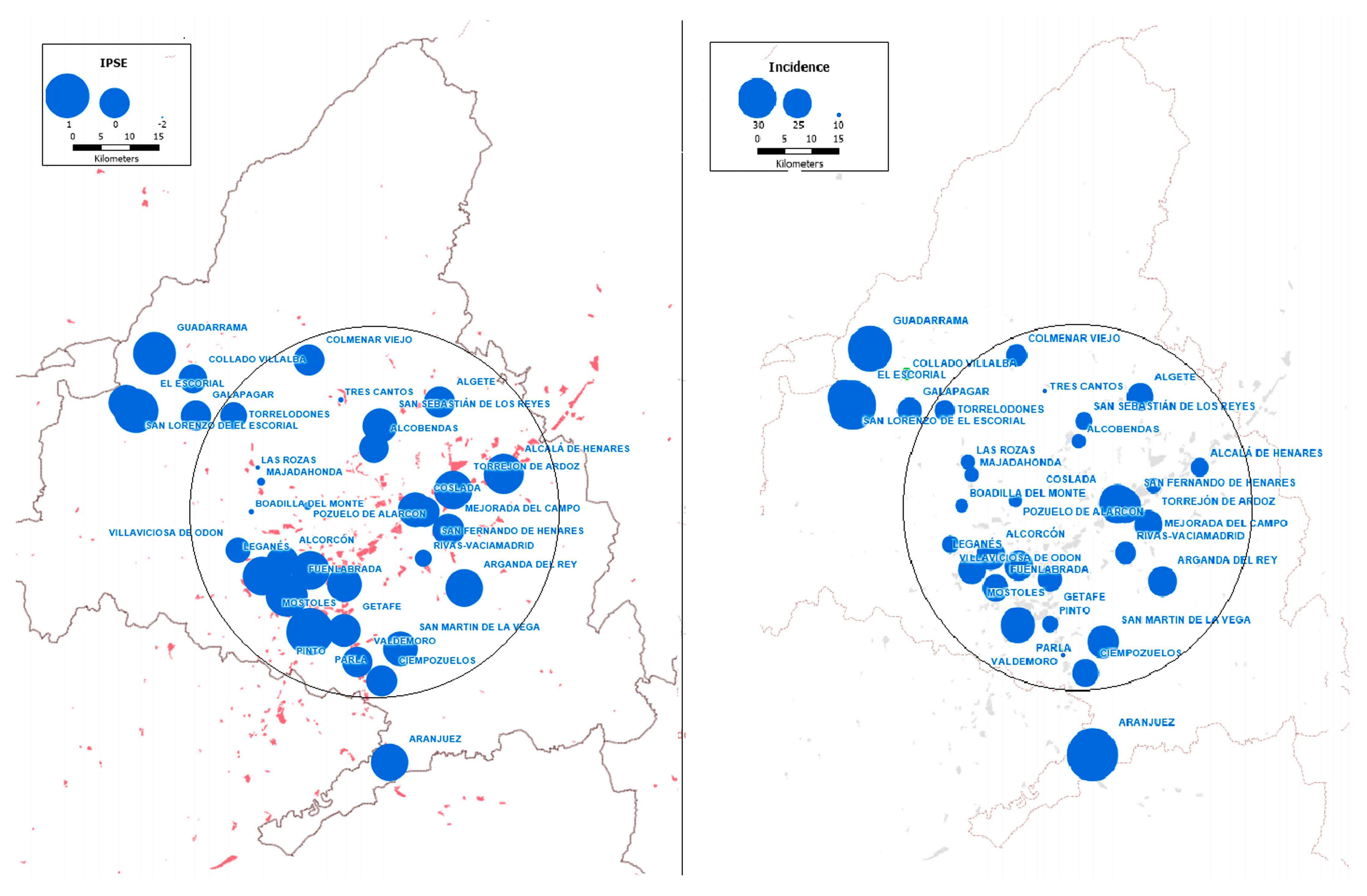
| Incidence of STEMI (per 100.000 inhabitants) | 22.5 | 14.11 | 44.96 | 30.85 |
| Sociodemographic data | ||||
| Inhabitants aged 18 or older | 60,251 | 12,763 | 170,160 | 150,397 |
| Foreign population (per 1000 inhabitants) | 117.78 | 69.1 | 235.2 | 184.1 |
| Wealth and employment data | ||||
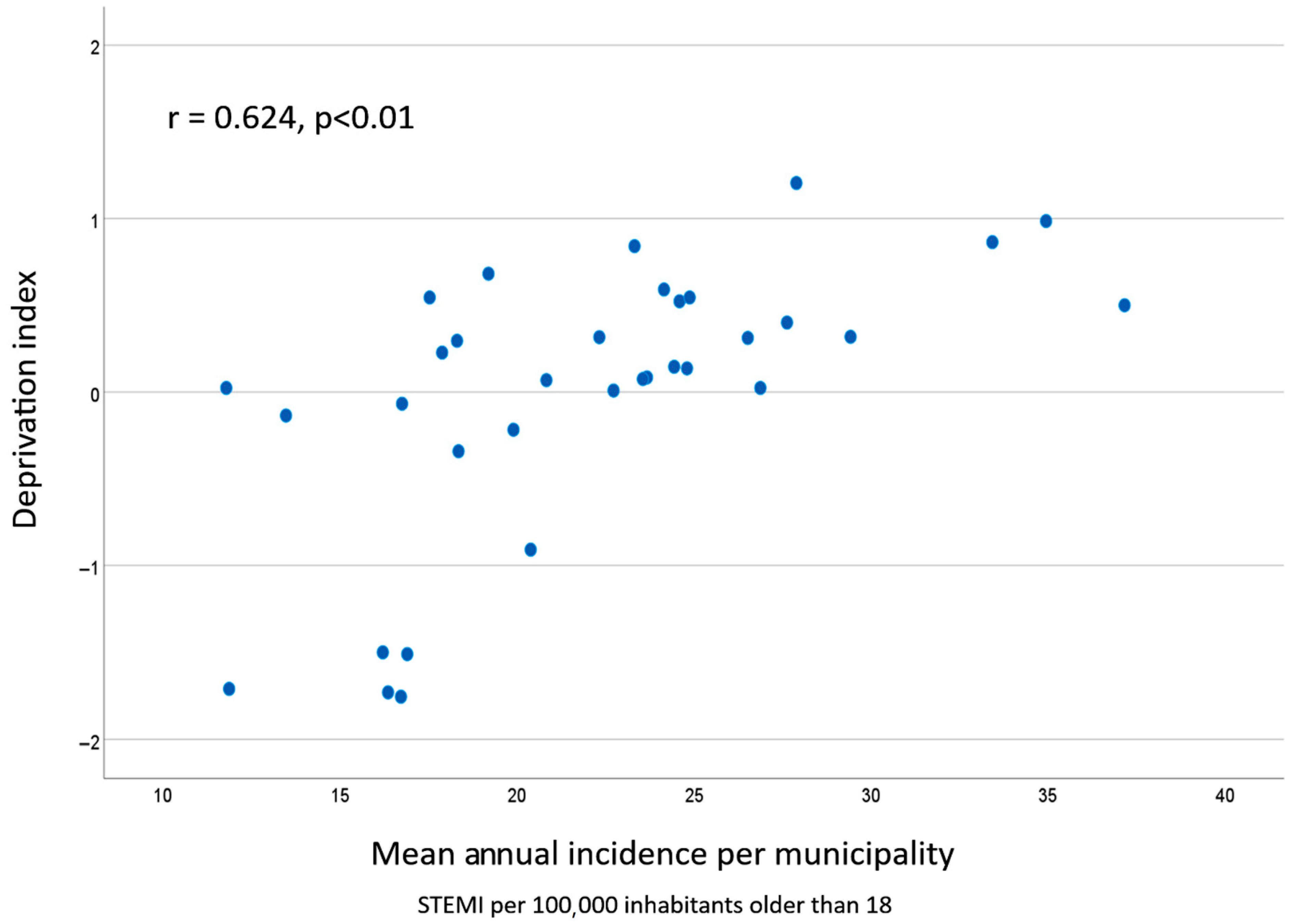
| Deprivation index | 0.20 | −1.98 | 0.62 | 2.60 |
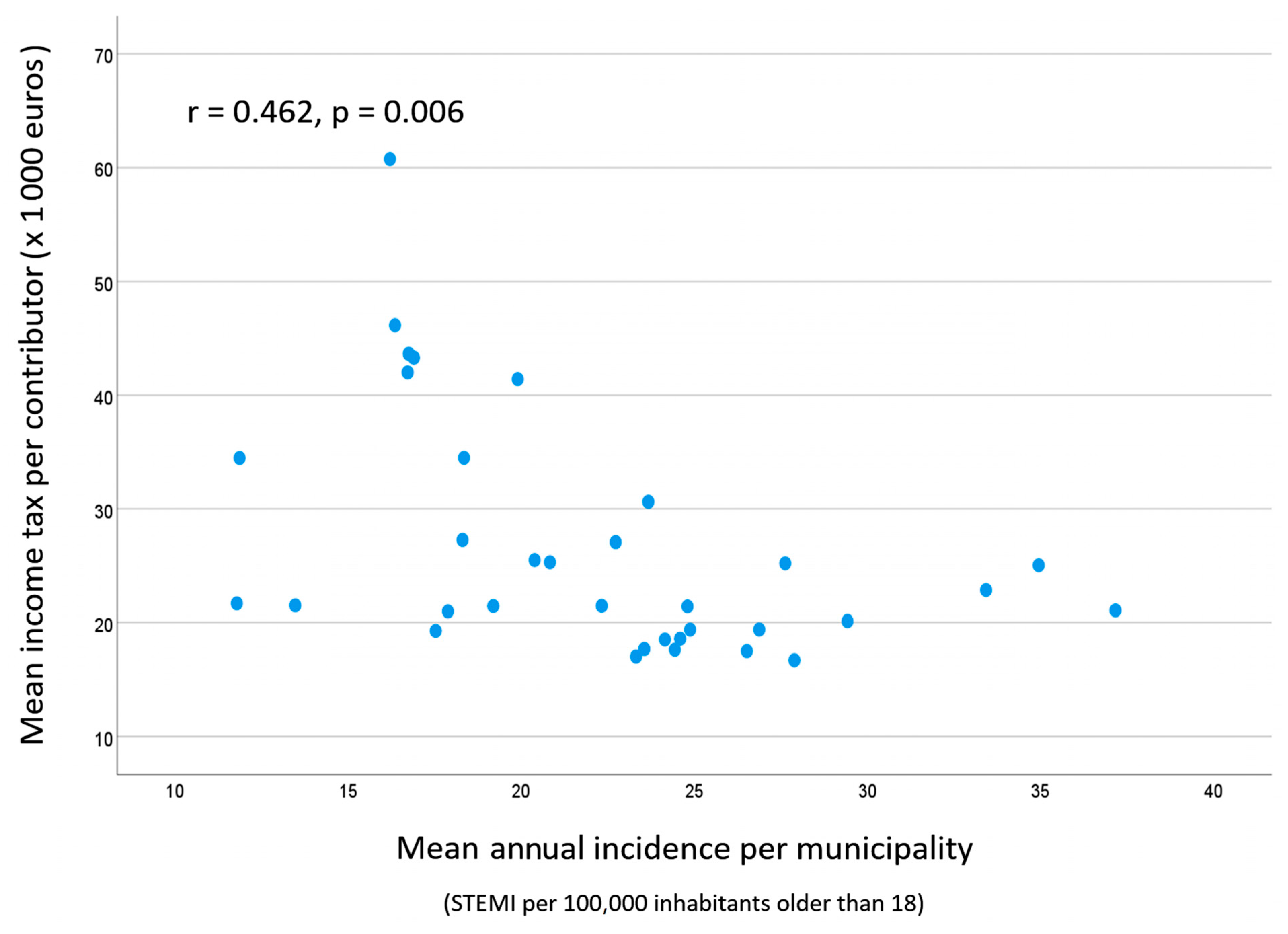
| Mean income tax per taxpayer (×1000 euros) | 21.6 | 16.8 | 62.7 | 51.4 |
| Gross domestic product per capita (×1000 euros) | 22.2 | 10.6 | 68.2 | 57.6 |
| Unemployment rate (%) | 7.7 | 3.45 | 10.40 | 6.95 |
| Financial employees (per 1000 inhabitants) | 16.3 | 9.3 | 52.6 | 42.9 |
| Public investment parameters | ||||
| Libraries per 10,000 inhabitants | 0.37 | 0.14 | 0.87 | 0.73 |
| Demographic Data | |||||
|---|---|---|---|---|---|
| Population older than 18 | Mean age | Older than 65 | Female | Foreign population | |
| r | −0.114 | 0.426 | 0.339 | 0.114 | 0.272 |
| p value | ns | 0.012 | ns | ns | ns |
| Wealth and Employment Data | |||||
| Income taxes | GDP | Unemployment rate | Financial employment | Deprivation index | |
| r | −0.462 | −0.442 | 0.354 | −0.497 | −0.624 |
| p value | 0.006 * | 0.009 * | 0.040 * | 0.003 * | <0.001 * |
| Public Investment Data | |||||
| Rate of alumni per teacher | Libraries per 10.000 inhabitants | Health centers per 10.000 inhabitants | |||
| r | −0.052 | −0.204 | 0.308 | ||
| p value | 0.771 | 0.248 | 0.076 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-de-Santiago, E.; Lozano-Batuecas, M.; García-Pérez-Velasco, J.; Gómez-Delgado, J.; García-Arribas, D.; Herruzo-León, A.; García-Lledó, A. Wealth, Unemployment, Social Investment, and Risk of ST-Segment Elevation Myocardial Infarction—An Ecological Analysis of a Low-Cardiovascular-Risk European Region. J. Clin. Med. 2025, 14, 7707. https://doi.org/10.3390/jcm14217707
García-de-Santiago E, Lozano-Batuecas M, García-Pérez-Velasco J, Gómez-Delgado J, García-Arribas D, Herruzo-León A, García-Lledó A. Wealth, Unemployment, Social Investment, and Risk of ST-Segment Elevation Myocardial Infarction—An Ecological Analysis of a Low-Cardiovascular-Risk European Region. Journal of Clinical Medicine. 2025; 14(21):7707. https://doi.org/10.3390/jcm14217707
Chicago/Turabian StyleGarcía-de-Santiago, Elvira, María Lozano-Batuecas, Javier García-Pérez-Velasco, Jeny Gómez-Delgado, Daniel García-Arribas, Antonio Herruzo-León, and Alberto García-Lledó. 2025. "Wealth, Unemployment, Social Investment, and Risk of ST-Segment Elevation Myocardial Infarction—An Ecological Analysis of a Low-Cardiovascular-Risk European Region" Journal of Clinical Medicine 14, no. 21: 7707. https://doi.org/10.3390/jcm14217707
APA StyleGarcía-de-Santiago, E., Lozano-Batuecas, M., García-Pérez-Velasco, J., Gómez-Delgado, J., García-Arribas, D., Herruzo-León, A., & García-Lledó, A. (2025). Wealth, Unemployment, Social Investment, and Risk of ST-Segment Elevation Myocardial Infarction—An Ecological Analysis of a Low-Cardiovascular-Risk European Region. Journal of Clinical Medicine, 14(21), 7707. https://doi.org/10.3390/jcm14217707






